Summary
The femoral approach has been considered the preferred technique for the endovascular treatment of intracranial aneurysms. Occasionally, aneurysms are not amenable to the standard femoral approach. We describe four cases of basilar artery aneurysm that were treated by the direct vertebral artery access of V1 at the cervical region. The direct vertebral artery access technique can provide an alternative route in selected cases for the treatment of basilar artery aneurysms.
Key words: angiography, basilar artery aneurysm, subarachnoid hemorrhage
Introduction
The femoral approach is the standard technique for the endovascular treatment (EVT) of intracranial aneurysms. Abnormalities in the vascular anatomy may generate technical difficulties for the catheterization of the vertebrobasilar system (VBS). The direct vertebral artery (VA) access has become obsolete since it is relatively difficult to perform and is usually associated with discomfort for the patient. Despite the small role of the direct VA access, the development of the EVT arsenal and the use of better neuroimaging sources could make this technique an alternative in selected cases. We describe four cases of basilar artery aneurysms (BA) treated with direct VA access of V1 segment.
Technique Description
Case 1
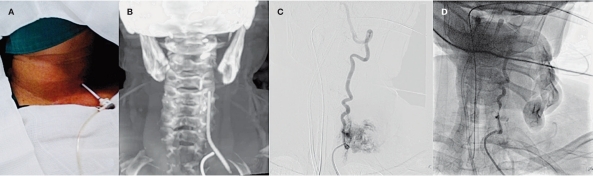
A previously hypertensive 71-year-old woman presented with subarachnoid hemorrhage (SAH), normal computed tomography (CT) scan and a bloodstained cerebrospinal fluid. The Hunt & Hess score (H&H) was 2, and the World Federation of Neurological Surgeons score (WFNS) was 1. Angiography disclosed a loop at the V1 segment of the left VA and a 7.4-mm BA. The right VA had a narrow lumen, thereby could not be used to access the aneurysm. The access through a retrograde catheterization could not be performed due to the angiographically absence of both posterior communicating arteries (PComA). Under general anesthesia a 6F catheter was anchored by the femoral route at the origin of the left VA to provide road map imaging (RMI) during the procedure. The left VA was directly accessed with an 18G catheter-needle mounted in a forceps and RMI guidance. Using a 5F introducer and a hydrophilic guidewire 0.035” the VA was accessed (Figure 1A,B). A microcatheter was introduced directly into the 5F introducer and the aneurysm was catheterized with a microguidewire 0.014”. Throughout the procedure, the patient received continuous heparin anticoagulation. The aneurysm was completely embolized. The 5F introducer was retrieved after complete heparin reversal and simultaneous angiogram VBS, looking for cervical hemorrhage, thrombosis or arterial vasospasm, which were not demonstrated. After eight days of observation the patient was discharged with an uneventful postoperative recovery and Glasgow outcome score (GOS) grade 5.
Figure 1.
A) The position of the introducer in the cervical region to access the left vertebral artery. B) Dyna CT image showing the introducer positioned in the left vertebral artery. C) Bleeding from the left vertebral puncture after removal of the introducer. D) Satisfactory left vertebral artery compression.
Case 2
A 71-year-old woman with systemic hypertension presented with a history of sudden severe headache, stupor and meningeal signs. The H&H and WFNS were both 4. The CT scan disclosed an extensive SAH with blood in the ventricles, and hydrocephalus. The patient was submitted to an external ventricular drainage. A study of VBS showed an 8.5 mm BA, a left VA kinking at the V1 segment and stenosis at the right VA. A non-reversible vasospasm occurred during an attempt to straighten the kinking of the left VA. It was difficult to access the right VA by femoral approach, thus, the brachial catheterization was tried, but failed due to the impossibility to navigate the microcatheter. A retrograde catheterization could not be performed because of the angiographical absence of the right PComA, and the tortuous course of the left PComA. The right V1 segment access was as in the first case. The EVT was performed with seven coils. The 5F introducer was retrieved after complete heparin reversal and simultaneous angiogram, like the first procedure. Complications did not occur during this maneuver. The left vertebral angiogram control was done and the vasospasm disappeared. A VBS disclosed normal vascular flow of the brain stem circulation and absence of vasospasm. The patient died thirty weeks after EVT, secondary to clinical complications.
Case 3
A 62-year-old woman presented with SAH, the Fisher score was 2 and the H&H was 2 and, the WFNS was 1. The angiogram study of VBS showed a loop at the left V1 segment and the right V2 segment which was tortuous and a 7.8 mm BA. Thereby, the left VA access was performed like in the others cases. A severe vasospasm was identified during the control angiogram, which was reversed by the injection of 1 ml of nimodipine. Thereafter, the aneurysm was completely embolized. The 5F introducer was retrieved like in the other cases, and the control angiogram showed a leak of contrast at the point of direct puncture. The activity clotting test (ACT) was 173 seconds and protamine was administrated. A new control angiogram was performed and the bleeding stopped. The patient was submitted to a cervical CT scan which showed no blood in the cervical area and the patient was woken up without any neurological disability or cervical hematoma. After a 14-day observation the patient was discharged with an uneventful postoperative recovery and GOS grade 5.
Case 4
A 75-year-old woman with systemic hypertension presented with SAH, and a CT scan with Fisher IV and hydrocephalus. The H&H was V, and the WFNS was 5. An external ventricular drain was inserted, with neurological improvement. The angiogram study of VBS showed kinking in both VA and a 6 mm BA. Attempts to correct the kinking and navigation through radial arteries were tried, but were unsuccessful. The left V1 segment access was as in the other cases. The aneurysm was completely embolized. The control angiogram showed extravasation of contrast at the point of puncture (Figure 1C), with normal ACT. A compression maneuver was performed on the anterior cervical region to stop the VA bleeding. A control angiogram was done and the extravasation stopped with this maneuver (Figure 1D). There were no complications related with the procedure performed. The patient died five days after EVT secondary to neurological injury.
Discussion
Historically, the vertebral artery approach was first studied by Berczeller and Kugler, in 1937, describing a posterior upper neck dissection to approach the vertebral artery at the sulcus atlantis. Their technique, however, was never applied to living subjects. In 1938, Sjöqvist described a newer method, that consisted in an anterior operative exposure of the V1 segment of the vertebral artery, immediately before its entrance into the transverse foramen of C6. Takahashi, in 1940, was the first to publish a direct puncture of the vertebral artery based on a plotted course of this vessel from its origin in subclavian artery to its entry into the foramen transversarium of C6. In 1950, Lindgren used x rays to identify osteophytes in the cervical spine and to choose the best approach to the vertebral artery into the foramen transversarium. He did not recommend any specific level, but stated that the middle and lower parts of the cervical spine are the worst because the vertebral osteophytes. Jaeger, in 1952, was the first to report the use a polyethylene catheter through the needle, withdrawing the needle before the contrast medium injection. Finally, Maslowski developed a percutaneous lateral atlanto-occipital method for vertebral angiography. The technique was reported in 1955, and described a percutaneous approach to the vertebral artery. The needle is positioned at the tip of mastoid process and advanced medially until contact with the tip of the atlas transverse process, and be adjusted to pass just above it to puncture the artery 4,5,7.
Furthermore, since the technique of direct VA access was first described 4, advances in neuroimaging and interventional neuroradiology have expanded the options to access the vertebrobasilar circulation. Facing these recent advances and relative technical difficulties to perform the technique, direct VA access became a secondary therapeutic alternative in the management of intracranial aneurysms 8. Nowadays, the EVT via femoral approach is considered the standard endovascular access by the majority of interventional neuroradiologists. Nevertheless, an approximate failure rate of 5% is reported due to tortuous access vessels 1. The access with a retrograde approach through the anterior circulation was described by Moret et al. 6 since the traditional endovascular approach to a cerebral aneurysm is anterograde. Unfortunately, this approach may be restrictive, because these catheters cannot always be navigated at an optimal angle into the arterial branches. The alternatives to surpass this inconvenience are the neurosurgical clipping and the EVT via the direct cervical access 2. In all cases we cannot access the aneurysms by anterograde or retrograde approach by femoral puncture. Therefore, considering the patients' age, clinical status and previous reports of direct cervical access, we selected the cervical approach. There are only three cases of direct VA access to treat basilar artery aneurysms reported in the literature 2. Bleeding from the puncture site after sheath removal is the most frequent problem related to the cervical direct access technique. To avoid cervical hematomas and the risk of upper airway obstruction, the use of protamine at the end of the procedure, manual compression, and sometimes, the application of hemostatic closure devices are recommended 3. A proper understanding of the cervical anatomy, the use of digital equipment and fine needle-catheters in a single puncture are essential to prevent puncture-related complications. We observed that the most frequent complication was transient puncture-induced vasospasm in the VA. It is important to stress the effectiveness of manual compression in controlling hemorrhage related to sheath removal at the termination of the endovascular procedure. During the angiographic control we observed the effectiveness of manual compression (Figure 1D). The control CT scan did not show cervical hematoma. Thus, high-quality endovascular materials allied with previously described techniques may overcome difficulties in challenging cases.
Conclusion
The direct VA access technique could provide a practical treatment strategy for the management of basilar artery aneurysms in those patients in whom endovascular coiling is the treatment of choice, and are not amenable to the standard femoral approach. The safety of the procedure, however, cannot be evaluated because of the few cases reported associated with the short-term follow-up of the patients.
References
- 1.Aletich VA, Debrun GM, Misra M, et al. The remodeling technique of balloon-assisted Guglielmi detachable coil placement in wide-necked aneurysms: experience at the University of Illinois at Chicago. J Neurosurg. 2000;93:388–396. doi: 10.3171/jns.2000.93.3.0388. [DOI] [PubMed] [Google Scholar]
- 2.Blanc R, Piotin M, Mounayer C, et al. Direct cervical arterial access for intracranial endovascular treatment. Neuroradiology. 2006;48:925–929. doi: 10.1007/s00234-006-0157-1. [DOI] [PubMed] [Google Scholar]
- 3.Blanc R, Mounayer C, Piotin M, et al. Hemostatic closure device after carotid puncture for stent and coil placement in an intracranial aneurysm: technical note. Am J Neuroradiol. 2002;23:978–981. [PMC free article] [PubMed] [Google Scholar]
- 4.Lindgren E. Percutaneous angiography of the vertebral artery. Acta Radiol. 1950;33:389–404. doi: 10.3109/00016925009133899. [DOI] [PubMed] [Google Scholar]
- 5.Maslowski HA. Vertebral angiography: percutaneous lateral atlanto-occipital method. Br J Surg. 1955;177:1–8. doi: 10.1002/bjs.18004317702. [DOI] [PubMed] [Google Scholar]
- 6.Moret J, Ross IB, Weill A, et al. The retrograde approach: a consideration for the endovascular treatment of aneurysms. Am J Neuroradiol. 2000;21:262–268. [PMC free article] [PubMed] [Google Scholar]
- 7.Schechter MM, de Gutiérrez-Mahoney CG. The evolution of vertebral angiography. Neuroradiology. 1973;5:157–164. doi: 10.1007/BF00341532. [DOI] [PubMed] [Google Scholar]
- 8.Weill A, Cognard C, Spelle L, et al. Endovascular treatment of basilar tip aneurysms after direct puncture of the vertebral artery. Am J Neuroradiol. 1998;19:1554–1556. [PMC free article] [PubMed] [Google Scholar]