Summary
Arterial dissections account for 2% of strokes in all age groups, and up to 25% in patients aged 45 years or younger. The safety of endovascular intervention in this patient population is not well characterized.
We identified all patients in the Merci registry – a prospective, multi-center post-market database enrolling patients treated with the Merci Retriever thrombectomy device – with arterial dissection as the most likely stroke etiology. Stroke presentation and procedural details were obtained prospectively; data regarding procedural complications, intracerebral hemorrhage (ICH), and the use of stenting of the dissected artery were obtained retrospectively.
Of 980 patients in the registry, ten were identified with arterial dissection (8/10 ICA; 2/10 vertebrobasilar). The median age was 48 years with a baseline NIH stroke scale score of 16 and median time to treatment of 4.9 h. The procedure resulted in thrombolysis in cerebral ischemia (TICI) scores of 2a or better in eight out of ten and TICI 2b or better in six out of ten patients. Stenting of the dissection was performed in four of nine (44%). The single complication (1/9; 11%) – extension of a dissected carotid artery – was treated effectively with stenting. No symptomatic ICH or stroke in a previously unaffected territory occurred. A favorable functional outcome was observed in eight out of ten patients.
Despite severe strokes on presentation, high rates of recanalization (8/10) and favorable functional outcomes (8/10) were observed. These results suggest that mechanical thrombectomy in patients with acute stroke resulting from arterial dissection is feasible, safe, and may be associated with favorable functional outcomes.
Key words: stroke, acute stroke, arterial dissection, mechanical thrombectomy, endovascular, carotid dissection, vertebral dissection, stenting, interventional
Introduction
Carotid and vertebral artery dissection account for approximately 2% of strokes in all age groups, and up to 25% in patients aged 45 years or younger 1. Few series have evaluated mechanical endovascular interventions in this clinical context. We therefore reviewed the safety, recanalization rates, and outcomes of patients treated with mechanical thrombectomy for acute stroke due to arterial dissection in the Merci registry.
Methods
The Merci registry is a prospective, multi-center, international, post-market database enrolling acute ischemic stroke patients treated with the Merci Retriever thrombectomy device (Concentric Medical, Mountain View, CA, USA). The database includes the following prospectively collected information: stroke etiology, patient demographics, stroke severity (as determined by the NIH stroke scale score, NIHSSS), location of arterial occlusion, endovascular interventions performed, and 90 day functional outcomes. After identifying all patients with arterial dissection as the stroke etiology in the Merci registry, we then reviewed individual patient charts retrospectively to identify complications (extension of arterial dissection, symptomatic intracerebral hemorrhage (SICH), and stroke in a previously unaffected territory). In addition, we determined retrospectively whether stenting of the dissected vessel was performed.
Results
Of the 980 patients enrolled in the registry, dissection was designated as the probable stroke etiology in ten patients (1.0%) (Table 1).
Table 1.
| Pt | Age | Baseline NIHSSS |
Dissection location |
Clot location |
IV tPA |
Onset to arterial puncture |
Procedure length |
Heparin (U) during procedure |
Number of passes |
IA lytic |
IA GpII b/IIIa |
Stent | Procedural complication |
SICH | TICI Pre |
TICI Post |
Recan (TICI ≥2a) |
Recan (TICI ≥2b) |
90d mRS |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 39 | L ICA | L M1 | Y | 9.4 | 5.3 | 18000 | 5 | N | no | yes | no | NA | 0 | 2b | Y | Y | 3 | |
| 2 | 46 | 14 | L ICA | L M1 | Y | 3.9 | 4.0 | 4500 | 1 | Y | no | yes | no | no | 1 | 2a | Y | N | 1 |
| 3 | 51 | 28 | L ICA | L M2 | N | 2.8 | 3.1 | 3500 | 4 | N | no | no | no | no | 0 | 2b | Y | Y | 3 |
| 4 | 18 | 19 | R ICA | R ICA/M1 | N | 3.1 | 1.6 | None | 1 | N | no | no | no | no | 0 | 3 | Y | Y | 0 |
| 5 | 48 | 11 | R ICA | R M1/M2 | N | 7.4 | 2.2 | None | 2 | N | yes | yes | yes* | no | 0 | 0 | N | N | 2 |
| 6 | 51 | 14 | R ICA | R M1/M2 | N | 3.2 | 1.9 | None | 2 | Y | no | no | no | no | 0 | 3 | Y | Y | 0 |
| 7 | 33 | BA | BA | N | 5.1 | 1.9 | None | 3 | N | no | no | no | no | 0 | 2a | Y | N | 2 | |
| 8 | 47 | 17 | R VERT/BA | R VERT/BA | N | 5.5 | 1.5 | 3000 | 3 | Y | no | yes | no | no | 0 | 3 | Y | Y | 1 |
| 9 | 52 | 1 | L ICA | L ICA/M2 | N | 6.3 | 1.6 | None | 1 | Y | no | no | no | no | 0 | 0 | N | N | 1 |
| 10 | 57 | 23 | L ICA | L M1/M2 | N | 2.7 | 1.4 | None | 2 | Y | no | NA | NA | NA | 0 | 2b | Y | Y | 2 |
| Mean or % Median |
44 48 |
16 |
20% | 4.9h 4.5h |
2.4h 1.9h |
2.4 2.0 |
50% | 10% | 80% | 60% |
1.5 |
||||||||
| *Extension of dissection by microcatheter, treated successfully with stenting. NIHSS: NIH Stroke Scale Score; IV tPA: Intravenous tPA prior to intra-arterial intervention; IA lytic: Intra-arterial thrombolytic administered during intervention; SICH: Symptomatic intracranial hemorrhage; TICI Pre: Thrombolysis in cerebral ischemia score prior to intervention; TICI post: Thrombolysis in cerebral ischemia score after intervention; 90d mRS: 90 day modified Rankin Score; NA: not available. | |||||||||||||||||||
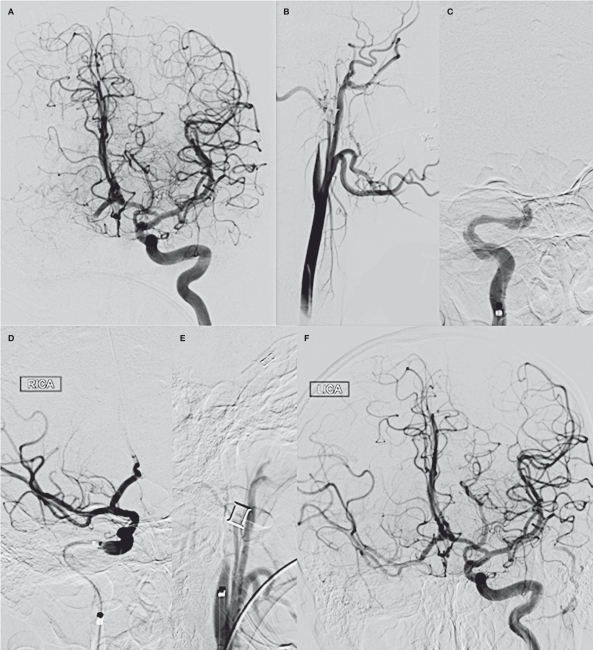
Figure 1.
A representative patient (case 4). An 18-year-old with spontaneous dissection of the right internal carotid artery and carotid-T occlusion. A) Left internal carotid artery injection, AP view, prior to intervention demonstrates no cross-filling of the right anterior circulation with a cutoff of the right A1 anterior cerebral artery consistent with possible carotid-T occlusion. B) Right common carotid injection, lateral view, demonstrates flame-shaped tapering/occlusion of the right ICA consistent with dissection. C) An 035 inch exchange wire was placed in the right external carotid artery and the 5F diagnostic catheter exchanged for a 6F flexor shuttle which was brought into the right carotid bulb proximal to the occlusion. The occlusion was then traversed with a coaxial system consisting of an 18L microcatheter inside an 044 inch Distal Access Catheter; this system was used as a rail allowing the 6F shuttle to be brought up distal to the occlusion. Repeat injection through the Shuttle, AP view, confirms occlusion of the carotid terminus. D) After one pass with the Merci Retriever v2.5 Firm, an injection through the guide catheter, AP view, demonstrates that the carotid terminus is recanalized, with flow re-established through the right M1 and M2 MCA branches and the right A1 ACA. E) After withdrawal of the shuttle proximal to the dissection, repeat injection, lateral view, demonstrates persistent occlusion of the right ICA. F) Repeat angiography of the left internal carotid artery demonstrates excellent cross-filling across the anterior communicating artery to supply the right anterior circulation.
The median age was 48 years (range 18 to 57) and the median baseline NIHSSS was 16 (range 1 to 28). Dissected arteries included the internal carotid artery (ICA) in eight out of ten (80%) and the vertebrobasilar system in 20%. Intracranial arterial occlusions were located in the middle cerebral artery (MCA) alone in seven out of eight patients with carotid dissection and a tandem distal ICA/MCA occlusion was present in one out of eight. Of the two patients with vertebrobasilar dissection, one had thrombus in the basilar artery alone and one had thrombosis of both the right vertebral artery and the basilar artery. The stroke etiology of the patient with isolated basilar artery occlusion was designated by the treating interventionalist as dissection at the time of the procedure, although some uncertainty existed. This patient presented with occlusion extending from the proximal basilar artery to the basilar tip. After recanalization of the basilar artery with the Merci retriever, residual stenosis remained within the proximal basilar which persisted on follow-up imaging nine months after treatment. Because of the absence of significant atherosclerosis in other vascular territories, this case was designated as a possible intracranial dissection.
Intravenous tissue plasminogen activator (IV tPA) was administered prior to intervention in two out of ten patients (20%). The mean time from stroke onset to arterial access was 4.9 h (median 4.5 h; range 2.7 to 9.4 h). Adjunctive intra-arterial thrombolytics (IAT) was given in five out of ten (50%) cases and IV glycoprotein IIb/IIIa inhibitors in one out of ten (10%). TICI 2a or better recanalization was achieved in 80%; TICI 2b or better flow was seen in 60%.
Information regarding the use of stenting during the procedure and procedural complications was available in nine out of ten patients and the presence or absence of symptomatic intracerebral hemorrhage was available for eight out of ten patients. Stenting of the dissected portion of the artery was used in four out of nine (44%). In all of these patients, stenting was performed to restore flow in patients with complete occlusion or near occlusion. The timing of stenting with respect to the procedure was available for three out of four patients in whom stents were used; stents were placed before intracranial mechanical thrombectomy in two out of three patients and afterwards in one. The rationale for stenting prior to thrombectomy was to provide vascular access for the thrombectomy procedure and the rationale for stenting afterward was to preserve vessel patency in the context of high grade stenosis.
The single complication (1/9; 11%) – extension of a dissected carotid artery by a microcatheter – was treated effectively with stenting. Otherwise, there were no complications (including SICH or stroke in a previously unaffected territory). At 90 days, the median mRS was 1.5 (range 0 to 3), with eight out of ten (80%) achieving a good functional outcome at 90 days (mRS≤2).
Discussion
The role for acute interventional treatment of stroke due to arterial dissection has not been fully defined. Because patients with arterial dissection may have abnormal vessels, there has been a concern that endovascular interventions could cause additional dissections in previously unaffected vessels, pseudoaneurysm formation, or vessel rupture. In addition, traversing the dissected artery with a microwire and microcatheter – or in some cases, a guide catheter or shuttle and guidewire – may pose a technical challenge and carries a risk of extending the dissection, with an increase in the degree of arterial stenosis or the formation of a pseudoaneurysm. Our case series documents only one of these complications, suggesting that these concerns may be overstated.
Several investigations describe the results of endovascular interventions for the treatment of stroke due to arterial dissection, although a paucity of data exists on the use of mechanical thrombectomy specifically. Stenting of the dissected portion of the cervical carotid or vertebral artery has been reported in patients with recurrent embolism, hemodynamic stroke, or enlarging pseudoaneurysm despite appropriate medical therapy 2-5. In addition, stenting of the dissection followed by intra-arterial infusion of thrombolytics and stenting of a tandem intracranial arterial occlusion has been reported in a few case reports or small case series in both the anterior 6-10 and posterior 11 circulations.
To our knowledge, only two case reports and one other published case series document the results of endovascular mechanical thrombectomy in patients with stroke due to dissection. Yu et al. described mechanical thrombectomy and stenting in a patient with basilar artery thrombosis due to a vertebral artery dissection 12 and Chen described a case of traumatic cervical carotid dissection leading to carotid-T occlusion which was successfully recanalized with the mechanical thrombectomy 13. Lavalle et al. 6 described six patients treated with stenting of the cervical carotid artery followed by IA thrombolytic therapy (one patient) or mechanical thrombectomy (five patients). A 90 day mRS <=2 was seen in all patients treated endovascularly and appeared to be superior to a comparison group of four patients treated with intravenous tPA alone, in whom an mRS <=2 was found in only one out of four. PH-2 ICH was present in one out of six patients treated interventionally and one out of four administered IV tPA.
Our small case series appears to support the safety and possible efficacy of mechanical thrombectomy for stroke due to arterial dissection. Despite presenting with severe strokes (median NIHSSS 16), three month outcomes were favorable (all mRS≤3; 80% mRS≤2). Recanalization rates were similar to those achieved by endovascular intervention of other etiologies, with TICI 2a or better flow in 80% and TICI 2b or better flow in 60%. Only one procedural complication was observed – extension of a dissection during traversal by a microcatheter – which did not result in additional morbidity. Otherwise, no significant adverse procedural events occurred and, among the patients for whom information was available, none developed symptomatic intracranial hemorrhage. Furthermore, although the sample size is too small to draw firm conclusions, there was no evidence that the use of adjunctive thrombolytic agents (IA tPA and Gp IIb/IIIa inhibitors) resulted in increased risk of extension of intramural thrombus within the dissection or increased the risk of complications associated with mechanical thrombectomy.
Our investigation has both advantages and limitations. To our knowledge, this is the largest series reporting the results of mechanical thrombectomy in the treatment of acute stroke due to arterial dissection. As a subgroup analysis of a large, prospective registry, demographic information, procedural details and outcomes were obtained prospectively with 90 day follow-up available in all patients. On the other hand, data regarding the use of arterial stents and the presence of intracerebral hemorrhage was obtained retrospectively. Furthermore, no control group exists, limiting the ability to establish a true treatment benefit. Finally, given the nature of the registry, it is not possible to determine how patients were selected for intervention or how many patients were eligible for inclusion in the registry but were not enrolled; the potential for bias exists if patients were systematically selected for enrollment into the registry who were expected to have good outcomes and excluded if expected to have a poor outcomes.
In summary, we report the results of mechanical thrombectomy with the Merci retriever in a series of patients with stroke due to carotid or vertebral artery dissection. Despite severe strokes on presentation, functional outcomes at 90 days appeared favorable and the rate of recanalization was reasonably high. These results suggest that mechanical thrombectomy in patients with acute stroke resulting from arterial dissection is feasible. The relatively low rate of complications and relatively high rates of favorable outcomes are promising, although firm conclusions about the use of mechanical thrombectomy in this patient population would require a substantially larger sample size and an appropriate control group.
Acknowledgments
We wish to acknowledge Gary Walker, PhD (Concentric Medical) for his assistance with data management.
References
- 1.Schievink WI. Spontaneous dissection of the carotid and vertebral arteries. N Engl J Med. 2001;344:898–906. doi: 10.1056/NEJM200103223441206. [DOI] [PubMed] [Google Scholar]
- 2.Kadkhodayan Y, Jeck DT, Moran CJ, et al. Angioplasty and stenting in carotid dissection with or without associated pseudoaneurysm. Am J Neuroradiol. 2005;26:2328–2335. [PMC free article] [PubMed] [Google Scholar]
- 3.Fava M, Meneses L, Loyola S, et al. Carotid artery dissection: endovascular treatment. Report of 12 patients. Catheter Cardiovasc Interv. 2008;71:694–700. doi: 10.1002/ccd.21483. [DOI] [PubMed] [Google Scholar]
- 4.Pham MH, Rahme RJ, Arnaout O, et al. Endovascular stenting of extracranial carotid and vertebral artery dissections: a systematic review of the literature. Neurosurgery. 2011;68:856–866. doi: 10.1227/NEU.0b013e318209ce03. discussion 866. [DOI] [PubMed] [Google Scholar]
- 5.Yin Q, Li Y, Fan X, et al. Feasibility and safety of stenting for symptomatic carotid arterial dissection. Cerebrovasc Dis. 2011;32(Suppl 1):11–15. doi: 10.1159/000330315. [DOI] [PubMed] [Google Scholar]
- 6.Lavallee PC, Mazighi M, Saint-Maurice JP, et al. Stent-assisted endovascular thrombolysis versus intravenous thrombolysis in internal carotid artery dissection with tandem internal carotid and middle cerebral artery occlusion. Stroke. 2007;38:2270–2274. doi: 10.1161/STROKEAHA.106.481093. [DOI] [PubMed] [Google Scholar]
- 7.Baumgartner RW, Georgiadis D, Nedeltchev K, et al. Stent-assisted endovascular thrombolysis versus intravenous thrombolysis in internal carotid artery dissection with tandem internal carotid and middle cerebral artery occlusion. Stroke. 2008;39:e27–28. doi: 10.1161/STROKEAHA.107.500959. [DOI] [PubMed] [Google Scholar]
- 8.Mourand I, Brunel H, Vendrell JF, et al. Endovascular stent-assisted thrombolysis in acute occlusive carotid artery dissection. Neuroradiology. 2010;52:135–140. doi: 10.1007/s00234-009-0597-5. [DOI] [PubMed] [Google Scholar]
- 9.Ohta H, Natarajan SK, Hauck EF, et al. Endovascular stent therapy for extracranial and intracranial carotid artery dissection: single-center experience. J Neurosurg. 2011;115:91–100. doi: 10.3171/2011.1.JNS091806. [DOI] [PubMed] [Google Scholar]
- 10.Abboud H, Houdart E, Meseguer E, et al. Stent assisted endovascular thrombolysis of internal carotid artery dissection. J Neurol Neurosurg Psychiatry. 2005;76:292–293. doi: 10.1136/jnnp.2004.041863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cerrato P, Berardino M, Bottacchi E, et al. Vertebral artery dissection complicated by basilar artery occlusion successfully treated with intra-arterial thrombolysis: three case reports. Neurol Sci. 2008;29:51–55. doi: 10.1007/s10072-008-0861-1. [DOI] [PubMed] [Google Scholar]
- 12.Yu W, Binder D, Foster-Barber A, et al. Endovascular embolectomy of acute basilar artery occlusion. Neurology. 2003;61:1421–1423. doi: 10.1212/wnl.61.10.1421. [DOI] [PubMed] [Google Scholar]
- 13.Chen M. Mechanical recanalization of acute carotid terminus occlusion from traumatic arterial dissection. Front Neurol. 2010;1:123. doi: 10.3389/fneur.2010.00123. [DOI] [PMC free article] [PubMed] [Google Scholar]