Abstract
During the last years, multiple methods and a wide set of materials for skull base reconstruction have been described. In our experience, the ideal graft for duraplasty is the iliotibial tract due to its favorable characteristics in terms of thickness, pliability, and strength. In this report, we show the iliotibial tract-harvesting technique under endoscopic guidance with a minimally invasive approach using a cadaveric model. Two longitudinal incisions of 1 cm each were made at 4 cm down a line drawn between the anterior-superior iliac spine and the lateral margin of patella at the extremities of the middle third of the thigh. By using a set of instruments for endoscopic face-lifting, the graft was easily set up and harvested. The endoscopic approach is associated with less visible scars, but longer operative time in comparison with open traditional procedure. The pros and cons in terms of morbidity need to be evaluated by further studies on actual cases.
Keywords: Iliotibial tract, skull base reconstruction, endoscopic harvesting, cadaveric model
One of the major challenges of skull base surgery is reconstruction of dural defects. In recent years, multiple reconstruction methods and a wide range of materials, both homologous and heterologous, have been reported with varying degrees of success.1,2,3 The ideal graft for duraplasty should be easy to harvest, available in adequate quantity, biocompatible with a minimal risk of rejection, and associated with minimal morbidity.4 Although locoregional pedicled flaps represent an ideal option in terms of aesthetic results, morbidity, and complication rates,5 they are not always available for reconstruction after an extended endoscopic resection of a sinonasal malignancy for obvious oncologic needs. In our experience in endoscopic skull base reconstruction, the graft that best fulfills these requirements is the iliotibial tract (ITT), which is the tendinous portion of the fascia lata covering the vastus lateralis muscle on the lateral aspect of the thigh. It extends from the iliac crest to the infracondylar tubercle of the tibia (Gerdy's tubercle), with an average length of 400 mm and average width of 90 mm.6 Because of its features in terms of thickness, pliability, and strength, it is easy to handle during endoscopic procedures and consequently ideal for multilayer reconstruction of skull base defects even extending from frontal sinus to planum sphenoidale, from orbit to orbit.7 The ITT is usually harvested by a longitudinal 10-cm incision of the skin and subcutaneous tissues at the level of middle third of the thigh because of the presence of fascia lata tensor muscle in the upper third and a progressively increasing thickness in its lower third. In this report, we describe the feasibility of an endoscopy-guided ITT-harvesting technique using a cadaveric model.
MATERIALS AND METHODS
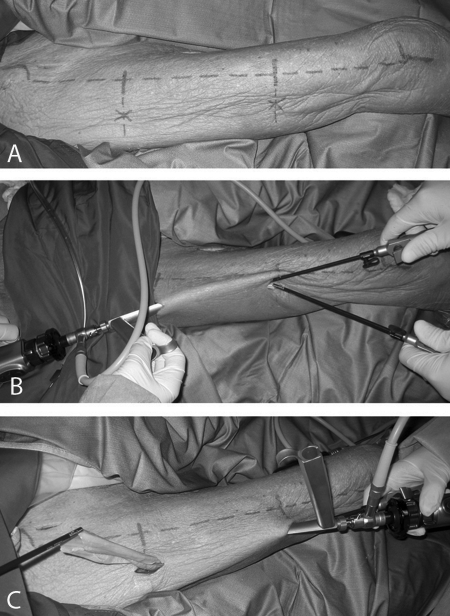
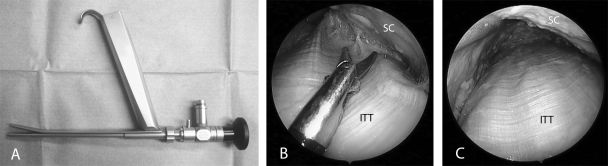
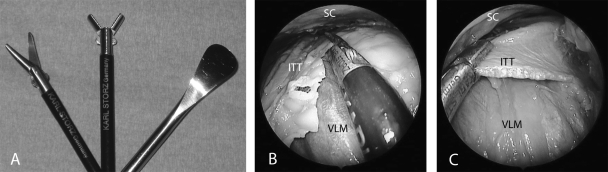
The study was performed on a 72-year-old male cadaver voluntarily donated. Two longitudinal incisions, 1 cm each, were made at 4 cm down a line drawn between the anterior superior iliac spine and the lateral margin of patella at the extremities of the middle third of the thigh (Fig. 1A). The choice of performing two incisions was related to the need of obtaining access to the surgical field upward and downward and also the need for two different operative corridors for the endoscope and instruments originally developed for endoscopic face-lifting (Fig. 1B; Karl Storz, Tuttlingen, Germany). Once the fascial layer was reached, with the assistance of an L-shaped optical retractor and a distal spatula, the subcutaneous tissue was gently dissected from the underlying myofascial compartment (Fig. 2). By elevating the overlying tissues with the optical retractor coupled with a 30-degree endoscope, a large surgical cavity was created (Fig. 2). Once the ITT was adequately exposed as a result of the double access, a graft of the required size was delineated and harvested with the help of a pincer and a scissor (Fig. 3). Finally, the graft was removed through one of the two incisions (Fig. 1C).
Figure 1.
Two incisions of 1 cm each were made at the extremities of the middle third of the thigh (A). The surgical field is controlled by two different operative corridors for the scope and instrumentation (B). The graft is taken out through one of the two incisions (C).
Figure 2.
A 30-degree endoscope is inserted into the optical retractor (A). Dissection of the subcutaneous tissue from the underlying ITT is performed (B) with exposure of the entire surgical field (C). SC, subcutaneous tissue; ITT, iliotibial tract.
Figure 3.
The graft is harvested with the assistance of a malleable dissector (A), scissors (A and B), and pincer (A and C). ITT, iliotibial tract; SC, subcutaneous tissue; VLM, vastus lateralis muscle.
DISCUSSION
In the last two decades, endoscopic and minimally invasive techniques have reduced perioperative morbidity in many fields of surgery with smaller incisions, shorter hospitalization time, and lower morbidity. When endoscopic instruments and experience are available, even a simple procedure such as ITT harvesting may be performed through minimally invasive access. Endoscopic harvesting of fascia lata was first described by Tucker et al in 1997, using three or four working ports for endoscope and instrumentation. They performed this technique for the reconstruction of the abdominal wall in three patients affected by inguinal hernia. The largest graft harvested was 12 × 15 cm, and morbidity was limited to a single seroma at the level of the donor site.8 Moreover, Malhotra et al also tested endoscopic harvesting of fascia lata on three patients, adopting a single small incision in the lateral aspect of the thigh. They reported no postoperative complications, but they harvested only tight linear strips of fascia.9
In the traditional external technique, a 10-cm linear or “S”-shaped incision is performed in contrast with the endoscopic approach described here, in which two smaller and less visible incisions are adopted.7,10 Grafts up to 15 cm in length and 8 cm in width could be required in the multilayer reconstruction of extended skull base defects; a double access is necessary to harvest a large sheet of tissue and to obtain two different corridors for the endoscope and instruments. Although a longer time for endoscopic harvesting has to be considered, a better control of bleeding in view of the meticulous and thorough dissection should also be expected. The placement of drainage, usually required in the external procedure, would be not required in the endoscopic setting, as confirmed by the experience of Malhotra et al.9 Although these authors have not described lateral prolapse of the vastus lateralis muscle in the postoperative course, when an extensive portion of ITT is removed, this possible complication might be encountered and cause deformity of the lateral thigh. In a traditional procedure, the wound is closed with two-layer subcutaneous suture to avoid muscle prolapse, and the endoscopic approach makes this unfeasible. In young female patients, the possibility to have no visible scars on the thigh would be a crucial issue. However, the final aesthetic result and the degree of muscular prolapse after endoscopic harvesting of ITT needs to be carefully considered in living patients.
In conclusion, ITT represents an ideal material in the reconstruction of limited and extended skull base defects and may be harvested by an external or endoscopic procedure. The former is characterized by an easier technique, a larger surgical field, and the possibility to close the wound with a double subcutaneous suture. On the other hand, an endoscopic approach may yield less visible scarring but entail a longer surgical time; moreover, endoscopic capability and experience are required, and a major risk of muscle prolapse is possible when a large amount of tissue is needed.
References
- Prevedello D M, Barges-Coll J, Fernandez-Miranda J C, et al. Middle turbinate flap for skull base reconstruction: cadaveric feasibility study. Laryngoscope. 2009;119:2094–2098. doi: 10.1002/lary.20226. [DOI] [PubMed] [Google Scholar]
- Fortes F SG, Carrau R L, Snyderman C H, et al. The posterior pedicle inferior turbinate flap: a new vascularized flap for skull base reconstruction. Laryngoscope. 2007;117:1329–1332. doi: 10.1097/mlg.0b013e318062111f. [DOI] [PubMed] [Google Scholar]
- Shah R N, Surowitz J B, Patel M R, et al. Endoscopic pedicled nasoseptal flap reconstruction for pediatric skull base defects. Laryngoscope. 2009;119:1067–1075. doi: 10.1002/lary.20216. [DOI] [PubMed] [Google Scholar]
- Tabaee A, Anand V K, Brown S M, Lin J W, Schwartz T H. Algorithm for reconstruction after endoscopic pituitary and skull base surgery. Laryngoscope. 2007;117:1133–1137. doi: 10.1097/MLG.0b013e31805c08c5. [DOI] [PubMed] [Google Scholar]
- Hadad G, Bassagasteguy L, Carrau R L, et al. A novel reconstructive technique after endoscopic expanded endonasal approaches: vascular pedicle nasoseptal flap. Laryngoscope. 2006;116:1882–1886. doi: 10.1097/01.mlg.0000234933.37779.e4. [DOI] [PubMed] [Google Scholar]
- Birnbaum K, Siebert C H, Pandorf T, Schopphoff E, Prescher A, Niethard F U. Anatomical and biomechanical investigations of the iliotibial tract. Surg Radiol Anat. 2004;26:433–446. doi: 10.1007/s00276-004-0265-8. [DOI] [PubMed] [Google Scholar]
- Villaret A B, Yakirevitch A, Bizzoni A, et al. Endoscopic transnasal craniectomy in the management of selected sinonasal malignancies. Am J Rhinol Allergy. 2010;24:60–65. doi: 10.2500/ajra.2010.24.3397. [DOI] [PubMed] [Google Scholar]
- Tucker J G, Choat D, Zubowicz V N. Videoscopically assisted fascia lata harvest for the correction of recurrent ventral hernia. South Med J. 1997;90:399–401. doi: 10.1097/00007611-199704000-00007. [DOI] [PubMed] [Google Scholar]
- Malhotra R, Selva D, Olver J M. Endoscopic harvesting of autogenous fascia lata. Ophthal Plast Reconstr Surg. 2007;23:372–375. doi: 10.1097/IOP.0b013e3181469cbd. [DOI] [PubMed] [Google Scholar]
- Amir A, Gatot A, Zucker G, Sagi A, Fliss D M. Harvesting large fascia lata sheaths: a rational approach. Skull Base Surg. 2000;10:29–34. [PMC free article] [PubMed] [Google Scholar]