Abstract
Appearance of the male genitalia is linked with self-esteem and sexual identity. Aesthetic surgery of the male genitalia serves to correct perceived deficiencies as well as physical deformities, which may cause psychological distress. Attention to patient motivation for surgery and to surgical technique is key to achieving optimal results. In this review, the authors describe aesthetic surgical techniques for treatment of penile and scrotal deficiencies. They also discuss techniques for revision in patients with previous surgery.
Keywords: Penis enlargement, penis lengthening, penis reconstruction, male genital aesthetic surgery, hidden penis, buried penis, scrotum reduction, penoscrotal web
A man's perception of his genitalia has a significant effect on self-esteem and sexual identity. Many cultures associate penile length with virility and sexual prowess. With increased exposure to popular media and pornographic material, men and women may develop a misconception of male genital norms, with the corresponding erroneous belief that genitalia of extreme length and girth is, in fact, commonplace.
Hence, male patients present for aesthetic genital surgery with the aim of altering the external appearance of the penis or scrotum despite the fact that they are often normal in size and shape. Advances in surgical techniques have made possible aesthetic improvement in the male genitalia. However, it is always crucial to examine the patient's underlying motivation for the surgery, as well as to rule out psychiatric problems. Because male genital appearance is often linked to self-confidence and may affect intimate relationships, it is important to address the underlying mental and physical issues before scheduling a patient for aesthetic genital surgery. Patient understanding of realistic expectations will result in greater satisfaction for both the patient and surgeon.
EVALUATION OF THE PATIENT
The goals of the patient should be explored and documented. One of the tools suggested for use in selecting patients for augmentation phalloplasty is a questionnaire, aimed at assessing a patient's willingness to undergo penile augmentation and also to measure postoperative result.1 Evaluation begins with a full history focusing on erectile, orgasmic, and urinary function.
A thorough physical examination of the male genitalia is performed.
Penile curvature or other abnormalities, such as Peyronie's plaques, should be noted on physical exam. It is important to be aware of normal penile dimensions. The length of the fully stretched flaccid penis correlates well with the length of the erect penis.2 The girth of the flaccid and erect penis does not have as reliable a relationship. In a study on 949 men, the average penile length was found to be 12.9 ± 1.9 cm, while girth was found to be 8.9 ± 0.9 cm3. Length measurements are taken from both the pubic bone and from the skin over the pubis to the tip of the glans on full stretch with the penis at 90 degrees perpendicular to the abdomen. Penile girth is measured at the base and at the level of the corona with the penis on full stretch.
The patient is examined both standing and supine to evaluate changes with position and gravity. The penis may appear shorter due to a relative or completely hidden penis, which may be caused by a shortage of penile skin (usually after a circumcision), by a large pubic fat pad, or by descent of the pubic fat pad and skin. The penis may also bury into the scrotum causing partial penile concealment. The ventral surface of the penis should be examined to rule out a penoscrotal web, which may result in an aesthetically or functionally shorter penis.
The patient should ideally also be examined with an erect penis, especially if girth surgery is to be performed. It is sufficient if the patient presents photos showing his erect penis from various angles. Otherwise, an erection can be obtained and then photographed from various angles through patient self-stimulation or intracavernosal injection of prostaglandin E1.
PENILE LENGTHENING
Release of the suspensory ligament of the penis may allow penile lengthening.4 The ligament is released for a width of one fingerbreadth along the length of the pubic symphysis by incising directly on the periosteum in the midline. This is usually achieved through a pubic transverse incision just above the penopubic junction. A V-Y advancement flap based distally at the penopubic junction may give the appearance of increased flaccid penile length. Unfortunately, V-Y flap complications may occur, as the blood supply of the penis may be disrupted, leading to healing problems such as partial flap loss and wound dehiscence. Scarring may result in hairless or depressed pubic areas. In addition, the V-Y advancement flap results in movement of thick, hair-bearing skin onto the penis, which may result in an unnatural humped appearance at the base of the penis. Reattachment of the penis to the pubis may paradoxically result in shortening of the penis, while a change in the angle of erection may also result. A fat flap mobilized from the medial spermatic cord can be transposed in the space between the pubic symphysis and corpora to prevent reattachment and shortening.5 De-epithelialization of the distal part of the V-Y flap and interposition between the base of the penis and pubis has been advocated as a method to minimize losses in penile length gained with suspensory ligament release.6 Use of a scrotal flap or skin graft is an alternative technique to provide coverage of the corporal bodies following release of the suspensory ligament of the penis.7 A rare complication of suspensory ligament release is penile instability, which is invariably caused by an overly aggressive release of the ligament.
The amount of penile length gained with suspensory ligament release is controversial, and may vary. Occasionally flaccid length may increase by a centimeter or more, but often no gain is achieved. The use of penile weights or stretching devices postoperatively potentially allows increase of length gain. The patient commences use of these devices approximately one week after surgery and continues daily for a period of months to years.
Recently, several of these penile stretching devices have been investigated as a noninvasive option to increase penile length. These require the patient to wear the device typically around 4 to 9 hours a day for 3 to 6 months. An increase in flaccid penile length ranging from 2.3 to 2.7 cm was reported for the Andro-Penis®8 and Golden Erect®9 devices. Further studies are required, however, before these devices can be considered an effective treatment for penile lengthening.
PENILE GIRTH ENHANCEMENT
Increase in penile girth as well as length is sought by the majority of men seeking augmentation phalloplasty. Key to a good result is creation of a symmetric cylinder with increased girth at all aspects, but this is very difficult. Girth surgery can often lead to severe deformities and complications.
Autologous fat injections into the dartos fascia are used commonly to increase penile girth. Advantages include lack of rejection and availability of material. However, this method is technique dependent, and results may vary among practitioners. Injecting small amounts of fat using multiple tunnels result in less secondary deformities. If not performed well or if large amounts of fat are injected, complications may result, which include unsightly nodules and irregularities from uneven fat injections and resorption, as well as asymmetry of the penis and loss of penile rigidity due to excess fat (Fig. 1).
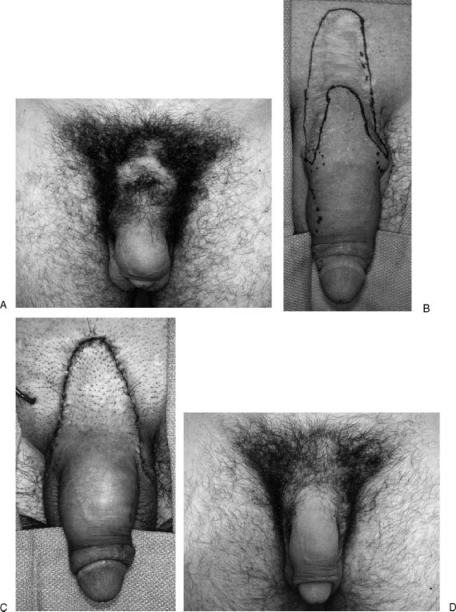
Figure 1.
A 26-year-old man several years after penile enlargement with VY advancement flap and penile fat injections (by other physician). (A) Pre-operation: The patient has a wide, hairless pubic scar, and a low-hanging penis with distortion from fat. (B) Markings for complete reversal of the VY flap and selective fat excision to achieve more normal contour. (C) The appearance after the procedure. Note the small drain. (D) Several months post-operation showing a normal penis with elimination of most of the deformities.
Dermal or dermal fat grafts may also be used to increase penile girth. These are usually placed as strips within the dartos fascia. Alternatively, a sheet graft is inset around the majority of the circumference of the penis, which has the advantage of a smooth texture. A partial circumcision or transverse pubic incision is used. The grafts are secured proximally and distally with sutures to prevent migration. Typically, an increase of girth ranging from 2 to 4 cm is achieved. However, severe complications can occur if the grafts do not survive completely. The resulting scar formation can cause penile shortening or curvature (Fig. 2). Donor site scars can also be very long and unsightly.
Figure 2.
A 28-year-old man with penile curvature resulting from fibrosis of the dermal fat grafts (by other physician).
Problems with dermal fat grafts and unsightly donor sites have led to the alternative use of Alloderm or other allograft dermal matrix grafts for girth enhancement. Alloderm is placed in layers above the Buck's fascia and sutured proximally and distally. Complications may occur, such as visible or palpable deformities as well as asymmetry, penile shortening, and curvature. Infection may also occur leading to skin loss (Fig. 3).
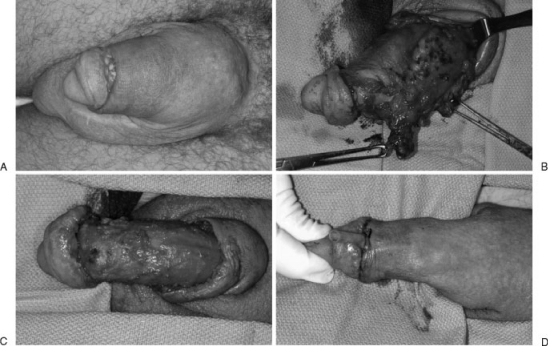
Figure 3.
A 33-year-old man who had previous dermal fat grafts inserted followed by insertion of Alloderm®, which became infected (by other physician). (A) Open wound from chronic drainage and penile distortion from implanted material (B) Allis clamps on Alloderm® and dermal fat grafts. Normal corpora are above. (C) Corpora after removal of material. (D) Penis at the conclusion of the procedure.
Synthetic materials have been used by some practitioners for girth enhancement. Injectable liquid silicone10 may have good short-term appearance, but many long-term penile deformities have been seen due to silicone migration and nodule formation (GJ Alter, personal experience, 2010) Hyaluronic acid11 injected into the glans penis has apparent good results and may be used to treat premature ejaculation, but caution should be used with these materials, which have caused intense foreign body reactions when used in other areas of the body.12 Long-term outcome studies are required before widespread adoption of hyaluronic acids for penile augmentation.
A true increase in the girth of the corporal bodies can be achieved through longitudinal incisions through the tunica albuginea at the 3 and 9 o'clock positions. These can be patched with saphenous vein grafts13 or Alloderm®. Postsurgical increases in erect penile diameter ranging from 1.1 to 2.1 cm were reported. These procedures have the risk of erectile dysfunction if poor healing or infection occurs.
Recent research has described the use of tissue engineering approaches to increase penile girth. Autologous fibroblasts were harvested from scrotal skin and implanted on polylactic-acid-co-glycolide (PLGA) scaffolds.14 These were then implanted under the Buck's fascia of the penile shaft. The authors described a mean increase in flaccid and erect penile girth of 4.01 and 2.92 cm, respectively. Another study using a similar technique described a mean increase in penile girth of 3.15 cm (range 1.9 to 4.1).15 Future research may reveal new techniques for augmentation phalloplasty.
REVISION SURGERY
Unfortunately, patients often present with dissatisfaction following previous penile enlargement surgery. It is crucial to prioritize the patient's reconstructive goals, as it may not be possible or advisable to reverse all the deformities in one surgery. The self-esteem and psychological issues that motivated the patients to seek the initial surgery are exacerbated by the poor result from the initial penile aesthetic surgery. Therefore, these patients are often devastated and more self-conscious. Hence, care must be taken with the reconstruction to aid patients in regaining physical and psychological health.
Reversal of a V-Y advancement flap used to lengthen the penis is the most common revision procedure.16 Patients are often unhappy with a dorsal penile hump, proximal hair-bearing tissue, or other V-Y flap deformity. The amount of penile shaft skin available should be assessed to ensure that complete reversal of the V-Y flap does not shorten the penis or restrict an erection. If there is insufficient skin, partial reversal may be performed, which results in an inverted Y-shaped scar with a shorter vertical limb. Meticulous tension-free skin closure is required to reduce the risk of hypertrophic scarring. A suction drain should be used. Re-release of the penile suspensory ligament should only be performed if there is significant penile shortening, as the risk of injury to dorsal neurovascular structures is increased.
Injection of autologous fat for girth enhancement may result in nodules or penile asymmetry. Resection of nodules may be performed through a limited or complete circumcision incision, median raphe incision, or through a previous V-Y incision. If possible, tailor the fat by removing only small fat amounts. Complete removal of fat with its intertwined dartos fascia may result in lymphedema. In addition, penile skin can attach to Buck's fascia, and the proximal dorsal corpora can attach to the pubic subcutaneous tissue or skin, which may result in penile shortening.
Previous dermal and dermal-fat grafts or Alloderm may result in similar problems, inclusive of penile shortening, induration, and curvature. Removal of grafts may be performed through circumcision, median raphe, or low pubic incisions. Care should be taken to prevent injury to the dorsal neurovascular structures. Dartos fascia should be preserved whenever possible to prevent adhesion of the skin to Buck's fascia. Unilateral or bilateral spermatic cord fat flaps may be used to fill dead space at the penopubic junction to prevent penile shortening.
HIDDEN OR BURIED PENIS
A hidden, buried, or concealed penis refers to a penis in which its appearance is obscured partially or completely within the pubic skin and fat and/or scrotum (Figs. 4 and 5). Most patients have normal corporal length but function and aesthetic appearance are hindered. There are many causes, such as penile skin deficiency from overresection of shaft skin during circumcision or from chronic inflammation, obesity, weight loss with skin excess, aging with skin descent, or congenital buried penis. If the patient has adequate skin, the underlying deformity is characterized by a lack of firm attachments between the Buck's fascia and the dartos fascia and skin. This causes the corporal bodies to remain inside the body, while the skin telescopes on the outside. Treatment of inadequate penile skin is beyond the scope of this chapter.
Figure 4.
(A) 25-year-old man with a relative hidden penis. He has a large pubic fat pad. (B) Two-months postoperation from suprapubic liposuction and dermatolipectomy and pubic and penoscrotal tacking. His penis is much more visible.
Figure 5.
(A,B) A 55-year-old man with completely hidden penis, a large pubic fat pad, and pubic skin descent. (C,D) Six-months postperation from suprapubic liposuction and dermatolipectomy and pubic and penoscrotal tacking. The patient would have a better cosmetic improvement with an abdominoplasty.
A moderate pubic fat pad can be reduced with liposuction if no significant buried penis is present.17 Usually, excess pubic skin is excised; the suprapubic fat pad is removed with liposuction and/or lipectomy; and the pubic escutcheon is elevated.18 The pubic skin and subcutaneous tissue need to be stabilized to the rectus fascia with tacking sutures. The ventral penile skin usually needs to be tacked to the tunica albuginea at the penoscrotal junction to prevent burying into the scrotum.19
If the patient does not have a significant pubic fat pad and skin descent, pubic liposuction with tacking from the skin at the penopubic junction to the corpora cavernosa can be performed in association with the penoscrotal tacking.20
The surgery for hidden penis is very successful and results in improved penile visual and functional length, and often improves the chronic skin inflammation associated with a severe hidden penis.
SCROTAL REDUCTION
Aging, stretching due to a hydrocele or varicocele, or congenital laxity may lead to an enlarged and/ or low-hanging scrotum by patients, leading to concerns with self-image or discomfort from skin irritation. A horizontal excision of the mid to upper scrotum allows removal of excess scrotal skin.21 Asymmetrical excision of the lower scrotal skin may be performed if there is unilateral scrotal enlargement. Skin with underlying dartos fascia is excised. The dartos is reapproximated with resorbable sutures, and the skin is closed with subcuticular resorbable sutures. Care should be taken to preserve the posterior scrotum due to its superior lymphatic drainage. Hemostasis is key, as a hematoma is the most common complication.
PENOSCROTAL WEB CORRECTION
A penoscrotal web is caused by scrotal skin extending onto the ventral surface of the penile shaft. This results in a loss of definition of the penoscrotal angle and may also cause problems with sexual intercourse. Penoscrotal webbing may be congenital, but may also occur following overresection of the ventral penile skin from circumcision. One technique is to incise the web transversely and close the resultant defect vertically,22 but dog-ears must be excised to prevent unsightly deformities. Mild webbing may be treated with a single or double Z-plasty, with the vertical limb aligned along the median raphe at the penoscrotal junction.23 For more severe webbing, excess skin can be resected along the median raphe, with a Z-plasty at the penoscrotal junction to prevent recurrent scar contracture (Fig. 6). An artificial erection induced by intracavernosal injection of prostaglandin E1 should be used to determine the maximal amount of skin that can be removed without causing penile constriction during erection. Another technique described is the use of one or two V-Y advancement flaps at the area of the penoscrotal web to recreate the penoscrotal border24
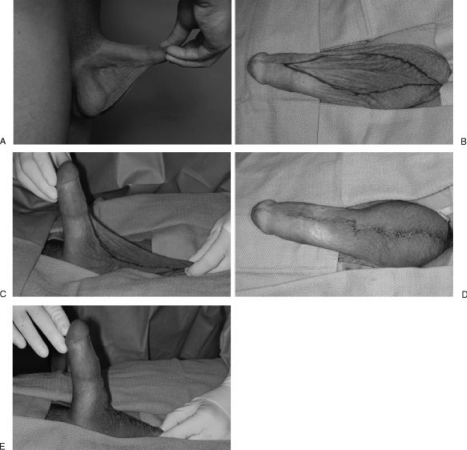
Figure 6.
(A) A 28-year-old man with severe penoscrotal web extending to the distal penis. (B,C) Marking for skin excision, which is performed with a pharmacologic erection. Notice the proximal circumcision scar, which contributed to the web by overresection of ventral penile skin. (D,E) Closure with z-plasty at the penoscrotal junction to prevent web recurrence from scar contraction.
CONCLUSION
Aesthetic surgery of the male genitalia represents both treatment for physical deformities and penile dysmorphophobia, or perceived “small penis.” Care should be taken to address both physical and psychological aspects of the problem. Meticulous surgical technique and realistic expectations are essential for favorable surgical and psychological results.
References
- Spyropoulos E, Galanakis I, Dellis A. Augmentation Phalloplasty Patient Selection and Satisfaction Inventory: a novel questionnaire to evaluate patients considered for augmentation phalloplasty surgery because of penile dysmorphophobia. Urology. 2007;70(2):221–226. doi: 10.1016/j.urology.2007.03.053. [DOI] [PubMed] [Google Scholar]
- Schonfeld W A, Beebe G W. Normal growth and variation in the male genitalia from birth to maturity. J Urol. 1942;48:759–779. [Google Scholar]
- Kamel I, Gadalla A, Ghanem H, Oraby M. Comparing penile measurements in normal and erectile dysfunction subjects. J Sex Med. 2009;6(8):2305–2310. doi: 10.1111/j.1743-6109.2009.01305.x. [DOI] [PubMed] [Google Scholar]
- Alter G J. Augmentation phalloplasty. Urol Clin North Am. 1995;22(4):887–902. [PubMed] [Google Scholar]
- Alter G J. Penile enlargement surgery. Tech Urol. 1998;4(2):70–76. [PubMed] [Google Scholar]
- Shaeer O, Shaeer K, el-Sebaie A. Minimizing the losses in penile lengthening: “V-Y half-skin half-fat advancement flap” and “T-closure” combined with severing the suspensory ligament. J Sex Med. 2006;3(1):155–160. doi: 10.1111/j.1743-6109.2005.00105.x. [DOI] [PubMed] [Google Scholar]
- Shirong L, Xuan Z, Zhengxiang W, Dongli F, Julong W, Dongyun Y. Modified penis lengthening surgery: review of 52 cases. Plast Reconstr Surg. 2000;105(2):596–599. doi: 10.1097/00006534-200002000-00018. [DOI] [PubMed] [Google Scholar]
- Gontero P, Di Marco M, Giubilei G, et al. A pilot phase-II prospective study to test the ‘efficacy’ and tolerability of a penile-extender device in the treatment of ‘short penis’. BJU Int. 2009;103(6):793–797. doi: 10.1111/j.1464-410X.2008.08083.x. [DOI] [PubMed] [Google Scholar]
- Nikoobakht M, Shahnazari A, Rezaeidanesh M, Mehrsai A, Pourmand G. Effect of penile-extender device in increasing penile size in men with shortened penis: preliminary results. [Epub ahead of print] J Sex Med. 2010;January:19. doi: 10.1111/j.1743-6109.2009.01662.x. [DOI] [PubMed] [Google Scholar]
- Yacobi Y, Tsivian A, Grinberg R, Kessler O. Short-term results of incremental penile girth enhancement using liquid injectable silicone: words of praise for a change. Asian J Androl. 2007;9(3):408–413. doi: 10.1111/j.1745-7262.2007.00262.x. [DOI] [PubMed] [Google Scholar]
- Kim J J, Kwak T I, Jeon B G, Cheon J, Moon D G. Human glans penis augmentation using injectable hyaluronic acid gel. Int J Impot Res. 2003;15(6):439–443. doi: 10.1038/sj.ijir.3901044. [DOI] [PubMed] [Google Scholar]
- Christensen L, Breiting V, Janssen M, Vuust J, Hogdall E. Adverse reactions to injectable soft tissue permanent fillers. Aesthetic Plast Surg. 2005;29(1):34–48. doi: 10.1007/s00266-004-0113-6. [DOI] [PubMed] [Google Scholar]
- Austoni E, Guarneri A, Cazzaniga A. A new technique for augmentation phalloplasty: albugineal surgery with bilateral saphenous grafts—three years of experience. Eur Urol. 2002;42(3):245–253. discussion 252–253. doi: 10.1016/s0302-2838(02)00264-6. [DOI] [PubMed] [Google Scholar]
- Jin Z, Wu Y G, Yuan Y M, et al. Tissue engineering penoplasty with biodegradable scaffold Maxpol-T co-grafted autologous fibroblasts for small penis syndrome. December 16 (Epub ahead of print) J Androl. 2010 doi: 10.2164/jandrol.110.011247. [DOI] [PubMed] [Google Scholar]
- Perovic S V, Byun J S, Scheplev P, Djordjevic M L, Kim J H, Bubanj T. New perspectives of penile enhancement surgery: tissue engineering with biodegradable scaffolds. Eur Urol. 2006;49(1):139–147. doi: 10.1016/j.eururo.2005.08.016. [DOI] [PubMed] [Google Scholar]
- Alter G J. Reconstruction of deformities resulting from penile enlargement surgery. J Urol. 1997;158(6):2153–2157. doi: 10.1016/s0022-5347(01)68185-0. [DOI] [PubMed] [Google Scholar]
- Adham M N, Teimourian B, Mosca P. Buried penis release in adults with suction lipectomy and abdominoplasty. Plast Reconstr Surg. 2000;106(4):840–844. doi: 10.1097/00006534-200009040-00014. [DOI] [PubMed] [Google Scholar]
- Alter G J. Surgical techniques: surgery to correct hidden penis. J Sex Med. 2006;3(5):939–942. doi: 10.1111/j.1743-6109.2006.00298.x. [DOI] [PubMed] [Google Scholar]
- Alter G J, Ehrlich R M. A new technique for correction of the hidden penis in children and adults. J Urol. 1999;161(2):455–459. [PubMed] [Google Scholar]
- Firlit C F, Hirhlji D, Palafiri A V. Penile concealment: a successful approach to correction. Dialogues Ped Urol. 2006;28(2):4–5. [Google Scholar]
- Alter G J. Aesthetic genital surgery. In: Mathes S J, Hentz V R, editors. Plastic Surgery. 2nd ed. Vol. VI. Philadelphia: WB Saunders and Co; 2000. pp. 389–410. [Google Scholar]
- Walsh P C. Campbell's Urology. 8th ed. Philadelphia, PA: Saunders; 2002. p. 2339. [Google Scholar]
- Alter G J. Correction of penoscrotal web. J Sex Med. 2007;4(4 Pt 1):844–847. doi: 10.1111/j.1743-6109.2007.00512.x. [DOI] [PubMed] [Google Scholar]
- Chang S J, Liu S P, Hsieh J T. Correcting penoscrotal web with the V-Y advancement technique. J Sex Med. 2008;5(1):249–250. doi: 10.1111/j.1743-6109.2007.00647.x. [DOI] [PubMed] [Google Scholar]