Abstract
The vascularized nasoseptal flap has become a principal reconstructive technique for the closure of endonasal skull base surgery defects. Despite its potential utility, there has been no report describing the use of the modern nasoseptal flap to repair traumatic cerebrospinal fluid (CSF) leaks and documenting the outcomes of this application. Specific concerns in skull base trauma include septal trauma with disruption of the flap pedicle, multiple leak sites, and issues surrounding persistent leaks after traumatic craniotomy. We performed a retrospective case series review of 14 patients who underwent nasoseptal flap closure of traumatic CSF leaks in a tertiary academic hospital. Main outcome measures include analysis of clinical outcome data. Defect etiology was motor vehicle collision in eight patients (57%), prior sinus surgery in four (29%), and assault in two (14%). At the time of nasoseptal flap repair, four patients had failed prior avascular grafts and two had previously undergone craniotomies for repair. Follow-up data were available for all patients (mean, 10 months). The overall success rate was 100% (no leaks), with 100% defect coverage. The nasoseptal flap is a versatile and reliable local reconstructive technique for ventral base traumatic defects, with a 100% CSF leak repair rate in this series.
Keywords: Cranial base, nasoseptal flap, cerebrospinal fluid leak, reconstructive techniques, endoscopy
Traumatic injury to the ventral skull base carries a high risk of developing cerebrospinal fluid (CSF) leak. Ascending infection and meningitis are thought to occur in 8.6 to 41% of these cases.1 Hence, the primary goal of treatment is to recreate the watertight barrier between the arachnoid space and the sinonasal tract. Secondary goals include eliminating dead space and preserving neurovascular and ocular function. A variety of techniques, utilizing multiple repair materials, have been proposed for leak repair2,3; however, no standardized algorithm exists and methods vary widely between surgeons. Specific concerns in skull base trauma include septal damage, multiple leak sites, and issues surrounding persistent leaks after craniotomy.
One reconstructive technique that has gained great popularity among surgeons performing skull base tumor surgery via the expanded endoscopic approach is the pedicled nasoseptal flap. This vascular flap, based on the nasoseptal artery, is composed of tissue from the nasal septum mucoperiosteum and mucoperichondrium. Known benefits of this procedure in reconstructing skull base surgical defects include expedited healing, low incidences of infection and wound complications, and a low rate of postoperative CSF leaks.4 Yet, despite its potential utility, there has been no report describing the use of the nasoseptal flap to repair traumatic CSF leaks and documenting the outcomes of this application. We report a technical description, advantages, and limitations of the nasoseptal flap for the repair of traumatic CSF leaks in a series of 14 patients.
METHODS
Patient Population
A retrospective chart review was performed on all patients who underwent nasoseptal flap closure of traumatic CSF leaks by the primary author (A.Z.) at the University of North Carolina at Chapel Hill and University of Pittsburgh Medical Center between August 2007 and October 2009.
Operative Technique
The technical details of harvesting the nasoseptal flap have been previously described.5 This section provides a brief technical description of our most current nasoseptal flap reconstructive technique for high-flow defect reconstruction. Two parallel incisions are made following the sagittal plane of the nasal septum. The inferior incision is made along the maxillary crest or onto the nasal floor. The superior incision is made 1 to 2 cm below the most superior aspect of the septum to preserve the olfactory epithelium. A vertical incision joins these two incisions anteriorly, close to the mucocutaneous junction. Posteriorly, the superior incision is extended laterally along the inferior aspect of the sphenoid os, and the inferior incision is extended along the posterior border of the nasal septum and then curved laterally along the choanal arch. These lateral extensions of the incisions allow a larger arc of rotation about the pedicle, and the adequate height of the flap at the sphenoid rostrum ensures the preservation of the vascular pedicle. The flap is elevated in an anterior-to-posterior fashion in a submucoperichondrial plane and is stored in the nasopharynx or the antrum during the skull base portion of the procedure.
Once the skull base portion of the case is complete, we then use a dural substitute such as Dura Matrix Onlay (Stryker, Kalamazoo, MI) or DuraGen (Integra, Plainsboro, NJ) to cover the exposed intracranial structures reconstructing the arachnoid. This is preferentially placed as an inlay graft. The nasoseptal flap is then rotated over the defect and overlaps over the bony boundaries of the defect. All mucosa is drilled away over the boney areas of the nasoseptal flap onlay to ensure healing. If the defect is too large for complete coverage with the nasoseptal flap, the uncovered areas are reinforced with fat or Alloderm (LifeCell, Branchburg, NJ). Once the flap completely covers the defect, Surgicel (Ethicon, Cornelia, GA) is placed around the edges to hold the flap in place. Then DuraSeal (Confluent Surgical, Waltham, MA) is sprayed over the entire surface of the flap overlapping the edges, making sure not to infiltrate DuraSeal under the flap, which will impede healing. Next, Gelfoam (Pfizer, New York, NY) is placed over the entire surface in two layers to prevent the Foley balloon or tampon sponge packing from sticking to the flap reconstruction. If the defect is primarily sellar or parasellar, then a 10-mL Foley balloon is used as the bolster. If the defect is cribriform or clival, then usually tampon sponges are used. For high-flow leaks, these stay in place for 5 to 7 days. Antibiotic coverage is required while the tampon sponges are in place. Silastic splints are placed over the nasoseptal flap donor site and left in place for 3 weeks. The patient is instructed to use nasal saline sprays four times per day for 4 weeks and then at 4 weeks a twice-daily sinus rinse or irrigation is started. The patient is seen at 3, 6, and 12 weeks for debridement if needed.
Outcomes
Outcome data were obtained from review of clinical variables from Dr. Zanation's prospective skull base reconstruction database. Specific postoperative complications of interest included recurrent CSF leak, meningitis, abscess formation, and the necessity of further revision surgery. Additional information recorded included success of repair, percent coverage of defect, relative mucosalization, and any other complication.
RESULTS
Fourteen (eight male and six female) patients with traumatic CSF leaks were repaired with the nasoseptal flap during the study period. The mean age was 49 years (range, 15 to 80 years). The etiology of the defect was motor vehicle collision in 8 patients (57%), prior sinus surgery in 4 (29%), and assault in 2 (14%). Defect size varied from 4 mm to 3.4 cm (longest axis). All areas of the ventral skull base (cribriform, sphenoid, and clivus) were represented, and three patients had two leak sites. At the time of nasoseptal flap repair, four patients had failed prior avascular grafts and two had previously undergone craniotomies for repair. The clinical case of one patient with multiple leak sites is presented in Fig. 1. Follow-up data, including postoperative endoscopy, were available for all patients (mean 10 months).
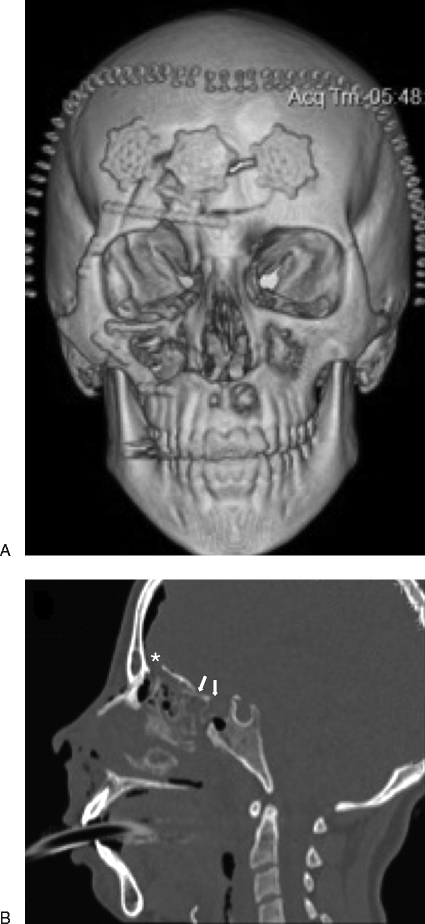
Figure 1.
Clinical case of a 15-year-old female patient involved in a motor vehicle accident. Prior to arriving at our center, the patient underwent facial reconstruction and two craniotomies. (A) 3-D reconstruction shows the extent of these repairs. (B) Despite these repair attempts, the patient developed persistent high-flow cerebrospinal fluid (CSF) leaks in the sphenoid and posterior ethmoids. The nasoseptal flap provided 100% coverage of all leaks, with no further leaking at 18 months postoperatively. In this figure, arrows indicate persistent CSF leaks and the asterisk, a leak repaired via craniotomy.
In all cases, a viable flap was observed without necrosis and with rapid mucosalization. The overall success rate was 100% (no leaks), with 100% coverage, including three patients with multiple leak sites. We encountered no infectious or wound complications; however, one patient developed persistent headaches and elevated intracranial pressures, requiring placement of a ventriculoperitoneal shunt within 6 months postoperatively.
Postoperative healing was complete, with no crusting and 100% mucosalization, by 10 weeks in all patients (range, 4 to 10 weeks). Patients had a mean of 2.5 debridements during the healing process, performed routine nasal irrigation three times per day until complete mucosalization occurred, and performed twice-daily nasal irrigation for 6 months postoperatively.
DISCUSSION
In 1952, Hirsch6 first described the use of a nasoseptal flap for the repair of CSF leaks. Others subsequently developed modifications, with good results;7,8,9,10 however, the utility of these techniques was limited by their random blood supply and the fact that torsional forces caused many flaps to pull apart from the defect.4 Advances in the field of endoscopic endonasal surgery, including multilayer reconstruction, dural suturing techniques, and intranasal balloon catheters,11 as well as the popularity of a refined nasoseptal flap for reconstruction of defects after skull base surgery, have made it necessary to revisit the issue of nasoseptal flap repair of CSF leaks.
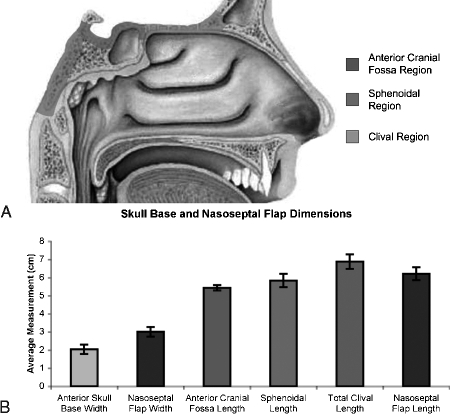
Endoscopic endonasal repair of traumatic CSF leaks has a success rate of ~95%.12 Experience with reconstruction after skull base surgery has shown that small defects can be reliably reconstructed using a variety of techniques while maintaining a high degree of success (90 to 97%).13,14 Sherman et al15 reported 100% successful closure rate using expanded polytetrafluoroethylene dural substitute. Germani et al16 described similar results (97% leak-free closure) in a series of 55 patients undergoing leak repair with acellular dermal allograft, and the work of Shah et al17 suggested that the use of fibrin adhesive in conjunction with acellular dermal grafts may provide even lower incidence of CSF leak. Snyderman et al11 outlined a technique using both dural graft matrix and two layers of acellular dermal allograft. As many of the acellular reconstruction techniques demonstrate similar incidence of CSF leaks, some have postulated that for minor defects, success does not depend on the type of reconstructive material, repair technique, or use of lumbar spinal drainage.18 Of the options available, the nasoseptal flap has been favored by many because the use of vascular tissue has the added benefit of efficient wound healing. The modern nasoseptal flap is supported by a rich vascular pedicle, perfused by the nasoseptal arteries; it is this vascular supply that is responsible for the flap's versatility, reliability, and arc of rotation. Because the flap is fully vascularized via the pedicle, healing must only occur at the edges of the defect—a clear advantage over free grafts, in which the entire defect bed must heal over the free graft site.5 This property allows most reconstructions to heal and mucosalize within 12 weeks5,19—an accelerated postoperative recovery period thought to decrease the risk of CSF leaks and ascending meningitis.20 In addition, the nasoseptal flap has a long reach with a total surface area enough to reconstruct any part of the cranial base (Fig. 2).19,21 Finally, visualization of the nasoseptal flap postoperatively allows the physician to characterize the reconstruction for potential flap failure.22
Figure 2.
Skull base and nasoseptal flap dimensions. (A) Illustration depicting the three modules of the ventral skull base. (B) Data obtained from radioanatomic analyses comparing the relative lengths and widths of the skull base modules and the nasoseptal flap show that the flap has ample size and width to cover any single module of the cranial base. (Series presented in Shah RN, Surowitz JB, Patel MR, et al. Endoscopic pedicled nasoseptal flap reconstruction for pediatric skull base defects. Laryngoscope 2009;119:1067–1075.)
The introduction of the nasoseptal flap reduced the postoperative CSF rate incidence after endonasal skull base surgery to 5%, comparable to that of traditional approaches.4 However, recent unpublished data from this institution examining results from 225 skull base tumor patients reconstructed with the nasoseptal flap demonstrated improved results, following a technical learning curve. Overall leak rate in this cohort was 6.2%, where the first 25 patients had a 24% leak rate and the last 200 had only 4% incidence of postoperative CSF leaks (Patel, unpublished data). Recent estimates of delayed leak rate and bacterial meningitis after endonasal closure were ~1.9%23 and 2%,11 following endoscopic skull base surgery. These results are echoed in our data of traumatic CSF leak repairs with 100% closure and no instances of delayed leak or infectious complications.
The chief limitation in nasoseptal flap reconstruction is that the decision to save this flap must be made preoperatively or there is a risk of injuring this tissue. Another concern of importance in traumatic CSF leaks is that septal trauma may damage the pedicle, rendering the flap nonviable. The same may be said of patients with prior posterior septectomy or large sphenoidotomies—these procedures interrupt blood supply to the flap, precluding its use.5,20
CONCLUSION
Ultimately, skull base defect location, size, and type of CSF leak should guide reconstruction efforts; however, nasoseptal flap closure should be considered in traumatic CSF leaks, especially patients with multiple leak sites or prior craniotomy for repair. With a large flap that can cover the entire ventral skull base, low patient morbidity, and exceptional overall leak repair rate (100% in this series), the nasoseptal flap is a versatile and reliable local reconstructive technique for ventral base traumatic defects.
ACKNOWLEDGMENTS
This work was supported by a grant from the Doris Duke Charitable Foundation funding Clinical Research Fellow Stephen A. Wheless.
References
- Costa H, Cerejo A, Baptista A, et al. The galea frontalis myofascial flap in anterior fossa CSF leaks. Br J Plast Surg. 1993;46:503–507. doi: 10.1016/0007-1226(93)90225-z. [DOI] [PubMed] [Google Scholar]
- Platt M P, Parnes S M. Management of unexpected cerebrospinal fluid leak during endoscopic sinus surgery. Curr Opin Otolaryngol Head Neck Surg. 2009;17:28–32. doi: 10.1097/MOO.0b013e32831fb593. [DOI] [PubMed] [Google Scholar]
- Moyer J S, Chepeha D B, Teknos T N. Contemporary skull base reconstruction. Curr Opin Otolaryngol Head Neck Surg. 2004;12:294–299. doi: 10.1097/01.moo.0000131445.27574.be. [DOI] [PubMed] [Google Scholar]
- Hadad G, Bassagasteguy L, Carrau R L, et al. A novel reconstructive technique after endoscopic expanded endonasal approaches: vascular pedicle nasoseptal flap. Laryngoscope. 2006;116:1882–1886. doi: 10.1097/01.mlg.0000234933.37779.e4. [DOI] [PubMed] [Google Scholar]
- Zanation A M, Carrau R L, Snyderman C H, et al. Nasoseptal flap reconstruction of high flow intraoperative cerebral spinal fluid leaks during endoscopic skull base surgery. Am J Rhinol Allergy. 2009;23:518–521. doi: 10.2500/ajra.2009.23.3378. [DOI] [PubMed] [Google Scholar]
- Hirsch O. Successful closure of cerebrospinal fluid rhinorrhea by endonasal surgery. AMA Arch Otolaryngol. 1952;56:1–12. doi: 10.1001/archotol.1952.00710020018001. [DOI] [PubMed] [Google Scholar]
- Vrabec D P, Hallberg O E. Cerebrospinal fluid rhinorrhea. Intranasal approach, review of the literature, and report of a case. Arch Otolaryngol. 1964;80:218–229. doi: 10.1001/archotol.1964.00750040224022. [DOI] [PubMed] [Google Scholar]
- Montgomery W W. Cerebrospinal fluid rhinorrhea. Otolaryngol Clin North Am. 1973;6:757–771. [PubMed] [Google Scholar]
- McCabe B F. The osteo-mucoperiosteal flap in repair of cerebrospinal fluid rhinorrhea. Laryngoscope. 1976;86:537–539. doi: 10.1288/00005537-197604000-00009. [DOI] [PubMed] [Google Scholar]
- Yessenow R S, McCabe B F. The osteo-mucoperiosteal flap in repair of cerebrospinal fluid rhinorrhea: a 20-year experience. Otolaryngol Head Neck Surg. 1989;101:555–558. doi: 10.1177/019459988910100507. [DOI] [PubMed] [Google Scholar]
- Snyderman C H, Carrau R L, Kassam A B, et al. Endoscopic skull base surgery: principles of endonasal oncological surgery. J Surg Oncol. 2008;97:658–664. doi: 10.1002/jso.21020. [DOI] [PubMed] [Google Scholar]
- Snyderman C H, Kassam A B, Carrau R, Mintz A. Endoscopic reconstruction of cranial base defects following endonasal skull base surgery. Skull Base. 2007;17:73–78. doi: 10.1055/s-2006-959337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hegazy H M, Carrau R L, Snyderman C H, Kassam A, Zweig J. Transnasal endoscopic repair of cerebrospinal fluid rhinorrhea: a meta-analysis. Laryngoscope. 2000;110:1166–1172. doi: 10.1097/00005537-200007000-00019. [DOI] [PubMed] [Google Scholar]
- Senior B A, Jafri K, Benninger M. Safety and efficacy of endoscopic repair of CSF leaks and encephaloceles: a survey of the members of the American Rhinologic Society. Am J Rhinol. 2001;15:21–25. doi: 10.2500/105065801781329356. [DOI] [PubMed] [Google Scholar]
- Sherman J H, Pouratian N, Okonkwo D O, Jane J A, Jr, Laws E R. Reconstruction of the sellar dura in transsphenoidal surgery using an expanded polytetrafluoroethylene dural substitute. Surg Neurol. 2008;69:73–76. discussion 76. doi: 10.1016/j.surneu.2007.07.069. [DOI] [PubMed] [Google Scholar]
- Germani R M, Vivero R, Herzallah I R, Casiano R R. Endoscopic reconstruction of large anterior skull base defects using acellular dermal allograft. Am J Rhinol. 2007;21:615–618. doi: 10.2500/ajr.2007.21.3080. [DOI] [PubMed] [Google Scholar]
- Shah A R, Pearlman A N, O'Grady K M, Bhattacharyya T K, Toriumi D M. Combined use of fibrin tissue adhesive and acellular dermis in dural repair. Am J Rhinol. 2007;21:619–621. doi: 10.2500/ajr.2007.21.3078. [DOI] [PubMed] [Google Scholar]
- Zweig J L, Carrau R L, Celin S E, et al. Endoscopic repair of cerebrospinal fluid leaks to the sinonasal tract: predictors of success. Otolaryngol Head Neck Surg. 2000;123:195–201. doi: 10.1067/mhn.2000.107452. [DOI] [PubMed] [Google Scholar]
- Kassam A B, Thomas A, Carrau R L, et al. Endoscopic reconstruction of the cranial base using a pedicled nasoseptal flap. Neurosurgery. 2008;(1 Suppl 1):ONS44–ONS52. discussion ONS52–ONS43. doi: 10.1227/01.neu.0000297074.13423.f5. [DOI] [PubMed] [Google Scholar]
- Fortes F S, Carrau R L, Snyderman C H, et al. The posterior pedicle inferior turbinate flap: a new vascularized flap for skull base reconstruction. Laryngoscope. 2007;117:1329–1332. doi: 10.1097/mlg.0b013e318062111f. [DOI] [PubMed] [Google Scholar]
- Shah R N, Surowitz J B, Patel M R, et al. Endoscopic pedicled nasoseptal flap reconstruction for pediatric skull base defects. Laryngoscope. 2009;119:1067–1075. doi: 10.1002/lary.20216. [DOI] [PubMed] [Google Scholar]
- Kang M D, Escott E, Thomas A J, et al. The MR imaging appearance of the vascular pedicle nasoseptal flap. AJNR Am J Neuroradiol. 2009;30:781–786. doi: 10.3174/ajnr.A1453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey R J, Smith J E, Wise S K, Patel S J, Frankel B M, Schlosser R J. Intracranial complications before and after endoscopic skull base reconstruction. Am J Rhinol. 2008;22:516–521. doi: 10.2500/ajr.2008.22.3223. [DOI] [PubMed] [Google Scholar]