Abstract
The role of robotic surgery in the skull base is evolving and represents the natural progression toward maximizing surgical resections in confined spaces without compromising oncological principles. In this study, we describe the novel application of robotic surgery to the repair of dural defects in the skull base. A transmaxillary-transantral approach to the nasal cavity was performed bilaterally in a cadaveric model. Repair of the skull base defect was undertaken robotically. In this technical report, we demonstrate the feasibility of a suture-based technique for surgical reconstruction of the skull base with robotic assistance in a cadaveric model. In all cases, suture repair of dural defects was successfully performed with robotic-assisted technique. Although preliminary in nature, this study suggests that traditional suture techniques can be implemented in a confined surgical site with the use of robotic technology.
Keywords: Robotic surgery, anterior skull base, reconstruction, dura
Minimally invasive surgery of the skull base continues to evolve and plays an increasingly important role in the management of skull base malignancies.1 This shift toward utilization of the transnasal corridor exclusively for cranial base malignancies is limited primarily by the ability of the surgeon to reconstruct large defects in the central skull base. This limitation is made more complex by the frequent need for adjuvant irradiation in these patients, necessitating a watertight closure of dural defects to prevent potentially life-threatening cerebrospinal fluid (CSF) leaks and meningitis.
Options for repair of the skull base include free mucosal grafts, fascia lata grafts, pedicled mucosal grafts, and biological materials.2 Although each has advantages and disadvantages, only the pedicled mucoperiosteal grafts are vascularized,3 a necessary component of any reconstruction in patients undergoing postoperative irradiation or in previously irradiated patients. One of the major drawbacks of the endoscopic approach is the inability to perform a suture-based reconstruction of the dura using currently available technology, an approach that is easily undertaken with a pericranial flap through the transcranial approach.
The role of robotic surgery in the skull base is evolving and represents the natural progression toward maximizing surgical resections in confined spaces without compromising oncological principles. We have previously reported on the feasibility of robotic surgical techniques for the resection of anterior skull base4 and central skull base/sellar tumors.5 In this study, we describe the novel application of robotic surgery to the repair of dural defects in the skull base.
METHODS
Four fresh frozen cadaveric heads were utilized for this study. Human cadaveric heads were used in conjunction with the University of Texas Health Science Center Department of Anatomy with institutional approval for anatomic specimen use. The surgical approach has been previously described.4,5 Briefly, a transmaxillary-transantral approach to the nasal cavity was performed bilaterally. A septal mucoperichondrial flap was harvested, and the DaVinci surgical robot (Intuitive Surgical Inc., Sunnyvale, CA) was then docked. Resection of the nasal septum and cribriform plate was performed, and dural defects were created either by incising the dura or by resecting a central area of the anterior cranial fossa dura (Fig. 1).
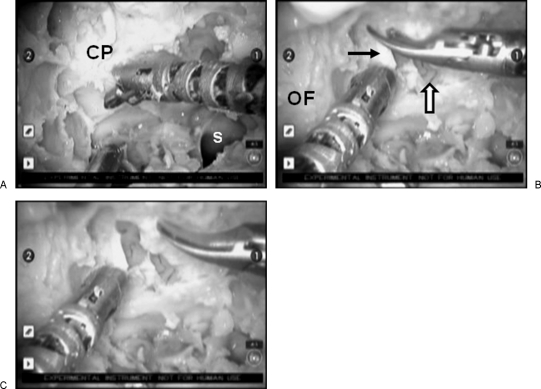
Figure 1.
(A–C) Resection of the cribriform plate (CP) and incision of the dura (black arrow) with the robotic instrumentation after complete exposure of medial orbital walls and sphenoid sinus (S). The frontal lobe is visible (white arrow). OF, orbital fat.
Repair of the skull base defect was undertaken robotically with two distinct techniques. First, repair of the dura was approached via primary reconstruction with both continuous and interrupted suture technique. Next, the harvested mucoperiosteal graft was trimmed to size and sutured into the dural defect with both running and interrupted suture techniques.
DISCUSSION
Technically successful reconstruction of the skull base via the transnasal route remains a complex clinical challenge. Multilayered closures are necessary to separate the intracranial space from the sinonasal cavity to prevent CSF leakage and meningitis. The major limitation of the multitudinous vascularized and nonvascularized approaches is lack of a true “watertight” seal. Rather, these approaches rely upon the layering of various substances and tissue adhesives to achieve nasocranial separation. As robotic-assisted surgical approaches to the anterior cranial fossa are evolving, repairing iatrogenic defects will be necessary. In this technical report, we demonstrate the feasibility of a suture-based technique for surgical reconstruction of the skull base with robotic assistance in a cadaveric model.
The integrity and durability of cranial base reconstruction become acutely critical for patients who have undergone resections for malignancies. Although patients with benign pathologies or low-grade malignancies are often treated with surgery alone, those with aggressive malignancies require adjuvant external beam radiotherapy (EBRT) with or without chemotherapy.6,7 Postoperative CSF leaks can lead to delays in the initiation of EBRT and allow for tumor regrowth. Alternatively, patients may develop delayed CSF leaks in an incompletely healed surgical bed, which could necessitate treatment breaks to manage them. Additionally, patients who have undergone preoperative radiotherapy are at an increased risk of postoperative CSF leakage.8 These potential sequelae can lead to significant morbidity and adverse oncological outcomes. A suture-based approach for immediate watertight reconstruction can help overcome some of these limitations.
A variety of suture materials were utilized, as were differing suture techniques. Due to its innate tensile properties and memory, monofilament was the most challenging to utilize, and a continuous technique appeared to provide the most stable reconstruction. Although the use of self-tightening surgical sutures for skull base reconstruction has been previously reported,9,10 our experience suggested that this approach was of limited value and was not effective in providing a safe dural closure. Attempts to robotically repair the dura with U-clips (Medtronic, Minneapolis, MN) were unsuccessful (data not shown), although this may have been related to the limited tension that can be exerted by the robotic arms.
The major limitations of this described approach are (1) clinical applicability; (2) suture materials; (3) biological materials; and (4) current robotic instrumentation. Although the DaVinci surgical robot has recently achieved Food and Drug Administration approval for applications in the head and neck, its utility in the skull base and sinonasal cavity remains off-label. Additionally, the current surgical instrumentation has not been optimized for bone resection, which can shorten the life span of the robotic articulating dissectors. Conceptually, this approach offers the opportunity to utilize fascia lata or other biological matrices (e.g., Alloderm, LifeCell Corporation, Branchburg, NJ; Duragen, Integra Neurosciences, Plainsboro, NJ) as a sutured graft, as opposed to overlay or underlay grafts.
RESULTS
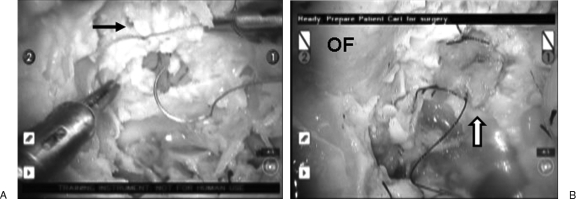
In all cases, suture repair of dural defects were successfully performed with robotic-assisted technique (Fig. 2; Video 1). Within the restricted confines of the endonasal resection bed, the robotic system greatly facilitated suturing of the dura with minimal trauma to surrounding critical neurovascular structures, including the orbits, carotid arteries, and frontal lobes. Further, tension-free reconstruction of moderately sized dural defects with mucoperiosteal grafts was technically feasible.
Figure 2.
Reconstruction of the dura. (A) primary repair of a dural defect (arrow) with polyglactin suture (Ethicon, Johnson & Johnson, New Brunswick, NJ). (B) Repair of a large dural defect with a mucosal graft (white arrow).
Video 1.
Video demonstrating intranasal suture repair of various dural defects and reconstruction with a mucosal graft.
CONCLUSION
In conclusion, we present a novel approach to reconstruction of the anterior cranial base in a preclinical cadaveric model. Although preliminary in nature, this study suggests that traditional suture techniques can be implemented in a confined surgical site with the use of robotic technology. Further optimization of both the technology and the technique is necessary to maximize use in human patients suffering from skull base malignancies.
NOTES
This work was presented at the Annual Meeting of the American Head and Neck Society, 2008.
ACKNOWLEDGMENTS
Dr. Hanna has received an educational grant from Intuitive Surgical for the training residents and fellows in robotic surgery.
References
- Hanna E, DeMonte F, Ibrahim S, Roberts D, Levine N, Kupferman M. Endoscopic resection of sinonasal cancers with and without craniotomy: oncologic results. Arch Otolaryngol Head Neck Surg. 2009;135:1219–1224. doi: 10.1001/archoto.2009.173. [DOI] [PubMed] [Google Scholar]
- Banks C A, Palmer J N, Chiu A G, O'Malley B W, Jr, Woodworth B A, Kennedy D W. Endoscopic closure of CSF rhinorrhea: 193 cases over 21 years. Otolaryngol Head Neck Surg. 2009;140:826–833. doi: 10.1016/j.otohns.2008.12.060. [DOI] [PubMed] [Google Scholar]
- Kassam A B, Thomas A, Carrau R L, Snyderman C H, et al. Endoscopic reconstruction of the cranial base using a pedicled nasoseptal flap. Neurosurgery. 2008;63:ONS44–ONS52. discussion ONS52–ONS3. doi: 10.1227/01.neu.0000297074.13423.f5. [DOI] [PubMed] [Google Scholar]
- Hanna E Y, Holsinger C, DeMonte F, Kupferman M. Robotic endoscopic surgery of the skull base: a novel surgical approach. Arch Otolaryngol Head Neck Surg. 2007;133:1209–1214. doi: 10.1001/archotol.133.12.1209. [DOI] [PubMed] [Google Scholar]
- Kupferman M, Demonte F, Holsinger F C, Hanna E. Transantral robotic access to the pituitary gland. Otolaryngol Head Neck Surg. 2009;141:413–415. doi: 10.1016/j.otohns.2009.05.028. [DOI] [PubMed] [Google Scholar]
- Diaz E M, Jr, Johnigan R H, III, Pero C, et al. Olfactory neuroblastoma: the 22-year experience at one comprehensive cancer center. Head Neck. 2005;27:138–149. doi: 10.1002/hed.20127. [DOI] [PubMed] [Google Scholar]
- Hoppe B S, Stegman L D, Zelefsky M J, et al. Treatment of nasal cavity and paranasal sinus cancer with modern radiotherapy techniques in the postoperative setting—the MSKCC experience. Int J Radiat Oncol Biol Phys. 2007;67:691–702. doi: 10.1016/j.ijrobp.2006.09.023. [DOI] [PubMed] [Google Scholar]
- Nishioka H, Haraoka J, Ikeda Y. Risk factors of cerebrospinal fluid rhinorrhea following transsphenoidal surgery. Acta Neurochir (Wien) 2005;147:1163–1166. discussion 1166. doi: 10.1007/s00701-005-0586-3. [DOI] [PubMed] [Google Scholar]
- Eloy J A, Carai A, Patel A B, Genden E M, Bederson J B. Combined endoscope-assisted transclival clipping and endovascular stenting of a basilar trunk aneurysm: case report. Neurosurgery. 2008;62(3 Suppl 1):142–143. discussion 143–144. doi: 10.1227/01.neu.0000317385.91432.df. [DOI] [PubMed] [Google Scholar]
- Gardner P, Kassam A, Snyderman C, Mintz A, Carrau R, Moossy J J. Endoscopic endonasal suturing of dural reconstruction grafts: a novel application of the U-Clip technology. Technical note. J Neurosurg. 2008;108:395–400. doi: 10.3171/JNS/2008/108/2/0395. [DOI] [PubMed] [Google Scholar]