Abstract
Maytenus heterophylla (Eckl. and Zeyh.) N.K.B. Robson and Maytenus senegalensis (Lam.) Exell are two African shrubs or trees that go under the common name of spike thorn, which belong to the Celastraceae family. Different plant parts of this species are largely used in traditional medicine for infectious and inflammatory diseases treatment. Several studies have been reported for both these species, but there are no recent review articles focusing microscopic, phytochemistry and pharmacological studies. The aim of this review is to summarize the information about these two African traditional medicines. Such kind of data can be applied in future experimental work and may guide future studies, namely in the field of validation of traditional medicine.
Keywords: African traditional knowledge, ethnopharmacology, Maytenus heterophylla, Maytenus senegalensis, microscopy, phytochemistry
INTRODUCTION
African traditional medicine is one of the oldest and perhaps the most diverse of all medicine systems. Africa is considered to be the cradle of mankind, with a rich biological and cultural diversity, and there are marked differences between different regions of this continent when it comes to healing practices.[1]
Maytenus heterophylla (Eckl. and Zeyh.) N.K.B. Robson and Maytenus senegalensis (Lam.) Exell are African shrubs or trees that go under the common name of spike thorn, which belong to the Celastraceae family. According to Neuwinger, M. heterophylla and M. senegalensis are two of the most frequently used species of the Maytenus Molina genus in the African traditional medicine (along with M. acuminata, M. buchananii, M. mossambicensis, M. obscura, M. peduncularis, M. putterlickioides, M. serrata and M. undata).[2]
In this paper, we will summarize and review the information about these important African traditional medicines that are currently of particular interest in new product development.
Most of the African cultures have a verbal tradition and, therefore, written information on cultural features in the past are not so readily available from Africa as from many other parts of the world.[3] The ethnobotanical information on the uses of these plants was sometimes documented on herbarium labels and, in this way, ethnobotanical information on a number of plants began to accumulate.[3] Systematic accounts in written form dealing with medicinal plants in Africa are of a fairly recent date, while reports dealing with ethnopharmacological aspects are more recent. A number of traditional national pharmacopeias have appeared, starting with the Madagascar Pharmacopeia in 1957, and research in the field of ethnobotany and ethnopharmacology has developed rapidly in many African countries.[3] The African Pharmacopoeia, covering traditional medicine of many African countries, has been published by the Scientific Technical Research Commission of the Organization of African Unity, starting with volume 1 in 1985 (African Pharmacopoeia, Vol. 1, 1985). Recently, the Association for African Medicinal Plants Standards, from Mauritius, started the publication of Medicinal Plants Monographs, providing botanical, phytochemical, pharmacological and commercial information on the most important medicinal plants used in Africa.[4]
In Africa, the ethnopharmacological and botanical knowledge on the uses of medicinal plants is often orally passed down from generation to generation.[5] Although traditional medicine has been recognized as a part of primary health care programs in many African countries,[6] there is a need to evaluate scientifically the crude extracts of plants for their medicinal and pharmacodynamic properties, clinical usefulness and toxicological potential.[7]
Higher plants are still poorly explored as sources of new drugs.[8] There are several ways in selecting plant materials when searching for new medicinal plants/active compounds. Ethnopharmacological information on medicinal plants is often of substantial importance for the finding of new potential medicinal plants/new ways of using an already known plant. It has been estimated that 74% of the pharmacologically active plant-derived components were discovered after the ethnomedical uses of the plants started to be investigated.[9–10] Another important way of discovering new medicinal plants and lead compounds is the phylogenetic approach, in which a number of closely related species of plants, assumed to contain related chemical compounds (chemotaxonomy), are screened for their biological effects.[11–12] Random sampling, i.e. collecting plant samples from certain habitats with high-species diversity (e.g., tropical rainforests), can be beneficial for finding novel chemical entities, but is somewhat time-consuming and requires hard work.[12] This kind of sampling is likely to be the industrial approach and most likely to be used for evaluating plants for bioactive compounds.[13]
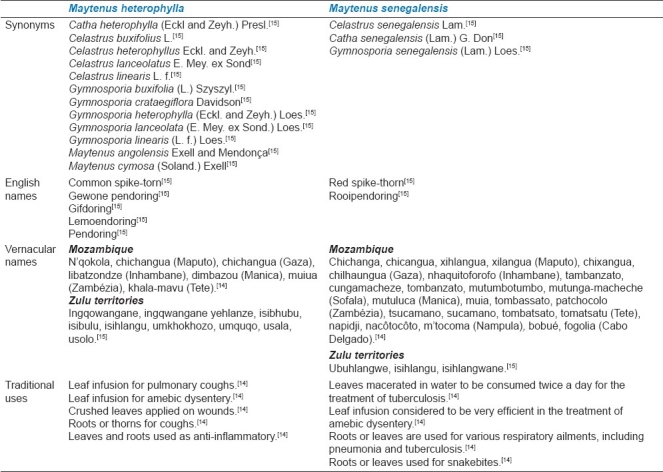
Both species mentioned above are traditionally used as antimicrobial and anti-inflammatory agents. More specifically, M. heterophylla and M. senegalensis are used to treat respiratory ailments and inflammation.[14–15] Table 1 compares M. heterophylla and M. senegalensis, referring the respective synonyms (the most common ones appear in bold), the English names, the local vernacular names (in Mozambique and in the Zulu territories) as well as the most common traditional uses. The use of these plants as anti-inflammatory herbal drugs is also common in other African countries like Benin, Kenya, Zambia, Tanzania, Senegal and Zimbabwe. In Tropical and Southwestern Africa, M. heterophylla leaves are also employed in the treatment of dysmenorrhoea and M. senegalensis leaves are used to treat toothaches, in India.[14–17]
Table 1.
Comparasion betwen the synonyms, common names and the ethnopharmacological uses of M. heterophylla and M. senegalensis
Botanical description
The Celastraceae classification at the generic level has undergone changes. As currently circumscribed, the genus Maytenus Molina, even after the reinstatement of Gumnosporia, is still clearly a heterogeneous group of species, a view also supported by others authors.[18–22]
M. heterophylla [Figure 1] has Gymnosporia heterophylla (Eckl. and Zeyh.) Loes. as synonym homotypic, and is an evergreen shrub, tree or, more rarely, a shrublet, often spreading or straggling, which grows up to 9 m high, unarmed or with green to brown spines up to 24 cm long (axillary spines or terminating short axillary branches), glabrous or very rarely with young branches lined or angular. The leaves are petiolated, alternated or often fascicled. The lamina of M. heterophylla is pale to deep green (or rarely glaucous above, concolorous or often grey–green below), often with a pale midrib, petiole up to 10 mm long. Spathulated, oblanceolated to ovated or elliptic margins, up to 9.5 cm × 5 cm, irregularly serrulated to entire. Dichasial cymes, located on solitary and axillary shoots or in axillary panicles. The flowers are dioecious, unscented, with peduncle 1–30 mm long, pedicels up to 7 mm, circular to triangular–lanceolate sepals 5(6) up to 1.5 mm long, white elliptic–oblong to oblong–spathulate petals 5(6) up to 3.5 mm long (with margin finely ciliolate to entire). The flowers bloom in dense, short racemes between the leaves (May/June), sometimes not until December. Yellow to red obovoid or subpyriform to subglobosoid capsule, 3–10 mm long, ovary 2–3 locular, coriaceous or succulent, smooth or rugulose. Reddish-brown 1–3(4) seeds, glossy, with a thin yellowish aril obliquely covering the lower 1/2–2/3.[14,23]
Figure 1.

General aspect of Maytenus heterophylla in the natural habitat. Reproduction size: column width
M. senegalensis [Figure 2] has Gymnosporia senegalensis (Lam.) Loes. as synonym homotypic, and is a shrub, tree or, more rarely, a shrublet, which grows up to 15 m high, unarmed or with spines up to 7 cm long (axillary or terminating short axillary branches), glabrous, without latex, young branches almost unlined, often glaucous.
Figure 2.

General aspect of Maytenus senegalensis in the natural habitat. Reproduction size: column width
Leaves are petiolated, alternated or fascicled, usually glaucous, and coriaceous (with lateral nerves and relatively lax reticulate venation slightly prominent or not prominent). The lamina of M. senegalensis is pale green pale, petiole up to 20 mm (9) long. Margins are spathulated, ovated to oblong–elliptic, up to 13 cm × 6 cm, often densely serrulated. Dichasial cymes located on short axillary shoots (or occasionally in axillary panicles). The flowers are dioecious (or rarely monoecious), scented peduncle 1–16 mm long, pedicels up to 6 mm long, oblong–lanceolate to ovate-triangular sepals (5) up to 1.2 mm long, pale yellow elliptic or oblanceolate petals 1–3.5 mm long (with margin finely ciliolate). The capsule is reddish, globosoid or pyriform, 2–6 mm long, ovary 2–3 locular, smooth. Reddish–brown 1–2 seeds, glossy, with a fleshy smooth rose–pink in yellowish aril obliquely covering the lower 1/2–2/3.[14,23]
Geographic distribution
Celastraceae is a large family comprising trees, shrubs and woody lianas with a Gondwanan distribution.[24]
Geographically, M. heterophylla is mainly distributed in the east coast of Africa, whereas M. senegalensis has a wider distribution, concerning Arabia, Afghanistan and India as well.[14] Therefore, the distribution of M. heterophylla is apparently confined from Ethiopia, the Sudan and East Congo southward to the Cape and westward to Angola and Southwestern Africa (Matobo and Bulalima-Mangwe districts of Zimbabwe), whereas M. senegalensis is widespread in the Savannah regions of tropical Africa.[23]
The habitat of these species is also different. M. heterophylla grows in forest, fringing forest margins, thickets and woodland or on termite mounds or sand dunes, whereas M. senegalensis occupies a wide variety of habitats, from deciduous woodland, thickets, scrub and wooded grassland and also on river banks and swamp margins.[23]
MICROSCOPIC STUDIES
Establishment of the quality control parameters necessary to profit herbal materials as raw materials for the manufacture of herbal medicines is one of the goals of our research team. Microscopy is one of the recognized techniques of identification of herbal raw materials and a mandatory technique for identification of herbal drugs according to official pharmacopoeias.
Some South American species of the genus Maytenus (M. ardisiaefolia, M. brasiliensis, M. cestrifolia, M. communis, M. ilicifolia and M. obtusifolia) were already microscopically characterized by other authors.[25–26] However, no studies were found to be related to the botanical identification of M. heterophylla and M. senegalensis leaves as herbal drugs and, in sequence, these kind of studies were conducted by our research team. The methodology includes the analysis of the whole, fragmentized and powdered plant material (M. heterophylla and M. senegalensis leaves) by light and scanning electron microscopy techniques.
For M. heterophylla, among the identified characters, the most useful for leaf identification of M. heterophylla includes the typical leaf bilateral organization; the presence of anomocytic stomata, more frequent in lower epidermis, and surrounded by a ring of four to six subsidiary cells appear with an irregular distribution; papillate cells on the surface of epidermal cells; multicelled uniseriate covering trichomes (rare). Calcium oxalate cluster crystals are present frequently in the palisade parenchyma, near the phloem cells of the midrib and occasionally occur on the epidermis.[27]
For M. senegalensis leaf identification, the most useful characteristics are the isobilateral organization of the parenchyma, with palisade parenchyma on both epidermises; the presence of calcium oxalate cluster crystals, isolated or inserted into the palisade parenchyma; and the characteristic epidermal cells with sinuous walls, a smooth cuticle and paracytic stomata more frequent in the lower epidermis.[28]
CHEMICAL CONSTITUENTS
The Celastraceae family is a source of important bioactive secondary metabolites. Alkaloid amines such as cathine often occur in this botanical family as also, rarely, benzylisoquinolide alkaloids.[15] Celastraceae members are commonly tanniferous, containing anthocyanins, sometimes saponiferous, only rarely cyanogenic and without iridoid compounds.[15] Among the compounds isolated from their species, triterpenes and triterpenoid quinonemethides are of great interest due to their wide range of biological activities.[17] Constituents as β-amyrin, lupane derivatives and quinoid pigments are considered typical of the Celastraceae family members.[15]
Compounds isolated from the Maytenus genus include the ansa macrolide, maytansine, and related macrolides such as normaytansine, maytanprine and maytanbutine.[15] Other isolated compounds include spermidine alkaloids (celacinnine and celallocinine) and nicotinoyl sesquiterpene alkaloids (maytoline and maytolidine) as well as catechin, procyanidins and phenoldienone triterpenoids.[16]
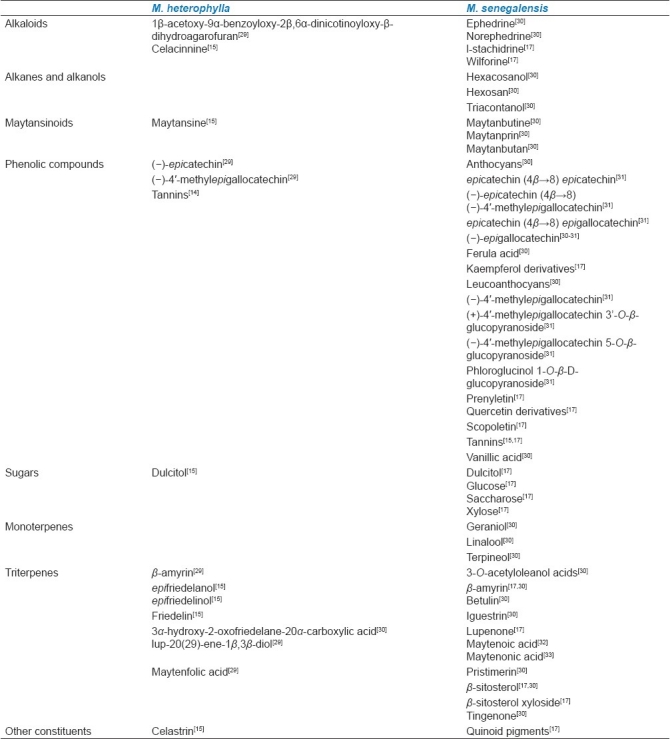
Table 2 summarizes the chemical compounds identified in M. heterophylla and M. senegalensis.
Table 2.
Chemical constituents of M. heterophylla and M. senegalensis
BIOLOGICAL ACTIVITY
Previous biological studies were reported in both species. The in vivo antiplasmodial activity of M. heterophylla and M. senegalensis root-bark extracts against resistant strains of P. berghei was determined.[34] M. senegalensis root and stem extracts demonstrated in vitro antiplasmodial activity against a cloroquine-sensitive strain of P. falciparum (D10).[35] Another study evaluated the in vitro activity of M. senegalensis leaf and stem-bark extracts against two strains of P. falciparum (cloroquine and pyrimethamine sensitive 3D7 strain; cloroquine-resistant and pyrimethamine-sensitive Dd2 strain).[36] An extract of the stem-bark of M. senegalensis demonstrated in vitro antileishmanial activity against promastigotes of Leishmania major reference vaccine strain (5AKSH).[37] Pristimerin was identified as the antileishmanial agent of M. senegalensis and proved to be active against resistant strains of P. falciparum.[38]
Stem-bark and root-bark extracts of M. senegalensis were tested against Bacillus subtilus, Micrococcus luteus and Staphylococcus aureus.[39] Maytenonic acid-isolated root-bark has a proven antibacterial activity against B. subtilus, Escherichia coli, Klebsiella pneumoniae and S. aureus.[33] An acetone extract of the aerial parts of this species has been revealed to be active against a sensitive strain of Mycobacterium tuberculosis (H37Rv strain, 0.5 mg/mL).[40]
Despite the use of different species of the genus Maytenus in African traditional medicine to prepare infusions or decoctions as anti-inflammatory and analgesic remedies for oral and/or topical administration,[41] biological studies concerning the evaluation of the anti-inflammatory activity of the African Maytenus species are scarce. However, the anti-inflammatory activity of the South American species of this genus was already performed, and the activity of M. ilicifolia,[41] M. aquifolium,[42] M. boaria[43] and M. rigida[44] was already verified. This kind of activity could be justified by the presence of phenol and triterpen metabolites.[41]
Recently, the anti-inflammatory activities of M. heterophylla and M. senegalensis ethanol extracts (70%) were determined in Wistar albino rats by the carrageenan-induced paw edema method. These extracts exhibited significant anti-inflammatory activity (120 mg/kg, per os), reducing edema by 51% and 35%, respectively.[45]
TOXICITY
Toxicity studies are particularly relevant because the risks differ from the type of extract and depend on the route and form of administration. Tradition and the knowledge accumulated over generations are commonly evoked to justify the activity and harmlessness of herbal products. Therefore, pharmacological and toxicological assays are essential to substantiate this knowledge and to guarantee that these extracts are devoid of toxicity (the difference between medicine and toxin is the dose).
Acute and sub-acute toxicity screening of M. heterophylla and M. senegalensis ethanol extracts (70%) was evaluated in adult male CD-6 mice. While M. heterophylla extract at 1200 mg/kg is shown to be non-toxic, M. senegalensis extract indicated some toxicity.[45]
CONCLUSION
It can be concluded that M. heterophylla and M. senegalensis have been used in African traditional medicine for the treatment of numerous ailments, including respiratory diseases, inflammation, microbial affections and topical application for healing wounds.
Biological activity studies confirm most of the traditional uses of these herbal drugs and toxicity studies meet the safe use of M. heterophylla. However, further detailed in vivo studies are needed to investigate this possibility. Most of the active compounds have not yet been isolated. There are still many constituents of M. heterophylla and M. senegalensis, with potential pharmacological activity, which have never been investigated. It is very likely that both species contain many beneficial pharmacological properties due to their wide spectrum of uses in the African traditional medicine. Therefore, in vivo and clinical investigations regarding their pharmacological effects could provide valuable evidence and insights into their potential benefits for future clinical management of many human diseases.
There is also a great deal of research pertaining to the discovery and characterization of new active therapeutic agents for several diseases such as tuberculosis and cancer. Academic institutions should invest more in ethnopharmacological researches and, thus, contribute to a wider benefit of the populations where this kind of medicine is essential to a better healthcare system.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Gurib-Fakim A. Medicinal plants: Traditions of yesterday and drugs of tomorrow. Mol Aspect Med. 2006;27:1–93. doi: 10.1016/j.mam.2005.07.008. [DOI] [PubMed] [Google Scholar]
- 2.Neuwinger HD. African traditional medicine: A dictionary of plant use and applications. Stuttgart: Medpharm Scientific Publishers; 2000. [Google Scholar]
- 3.Hedberg I, Staugard F. Traditional medicine in Botswana. Gaborone: Ipeleng Publishers; 1989. [Google Scholar]
- 4.Port Lewis:Association for African Medicinal Plants Standards, Ltd. 2000-2010. [cited 2010 Jun 15]. Available from: http://www.aamps.org/en/
- 5.Kokwaro O. Medicinal Plants of East Africa. Nairobi: East African Literature; 1976. [Google Scholar]
- 6.The promotion and development of traditional medicine. Geneva (Switzerland): WHO Press; 1978. World Health Organization. [Google Scholar]
- 7.Kyerematen GA, Ogunlana EO. An integrated approach to the pharmacological evaluation of traditional materia medica. J Ethnopharmacol. 1987;20:191–207. doi: 10.1016/0378-8741(87)90048-1. [DOI] [PubMed] [Google Scholar]
- 8.Hostettman K, Terreaux C. Search for new lead compounds from higher plants. Chimia. 2000;54:652–7. [Google Scholar]
- 9.Farnsworth NR, Soejarto DD. Global importance of medicinal plants. In: Akerele O, Heywood V, Synge H, editors. Conservation of Medicinal Plants. Cambridge: Cambridge University Press; 1991. [Google Scholar]
- 10.Wood-Sheldon J, Balick MJ, Laird SA. Medicinal plants: Can utilization and conservation coexist? Bronx: The New York Botanical Garden; 1997. [Google Scholar]
- 11.Cotton CM. Ethnobotany - Principles and Applications. Chisester: John Wiley and Sons; 1996. [Google Scholar]
- 12.Vuorelaa P, Leinonenb M, Saikkuc P, Tammelaa P, Rauhad JP, Wennberge T, et al. Natural products in the process of finding new drug candidates. Curr Med Chem. 2004;11:1375–89. doi: 10.2174/0929867043365116. [DOI] [PubMed] [Google Scholar]
- 13.Fabricant DS, Farnsworth NR. The value of plants used in traditional medicine for drug discovery. EHP. 2001;109:69–75. doi: 10.1289/ehp.01109s169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jansen PC, Mendes O. Plantas medicinais: Seu Uso Tradicional em Moçambique. Maputo: Imprensa do Partido; 1991. [Google Scholar]
- 15.Hutchings A, Scott A, Lewis G, Cunningham A. Zulu medicinal plants: An inventory. Pinetown: University of Natal Press; 1996. [Google Scholar]
- 16.Hedberg I, Hedberg O, Madati PJ, Mshigeni KE, Mshiu EN, Samuelsson G. Inventory of plants used in traditional medicine in Tanzania. I. Plants of the families Acanthaceae-Cucurbitaceae. J Ethnopharmacol. 1982;6:29–60. doi: 10.1016/0378-8741(82)90070-8. [DOI] [PubMed] [Google Scholar]
- 17.Mueller M, Mechler E. Medicinal plants in tropical countries: Traditional use - experience - facts. Stuttgart: Thieme; 2005. [Google Scholar]
- 18.Rogers CB, Abbot ATD, van Wyk AE. A convenient thin layer chromatographic technique for chemotaxonomic application in Maytenus (Celastraceae) S Afr J Bot. 1999;65:174–6. [Google Scholar]
- 19.Simmons MP, Hedin JP. Relationships and morphological character change among genera of Celastraceae sensu lato (including Hippocrateaceae) Ann Missouri Bot Gard. 1999;86:723–57. [Google Scholar]
- 20.Simmons MP, Clevinger CC, Savolainen V, Archer RH, Mathews S, Doyle JJ. Phylogeny of the Celastraceae inferred from phytochrome B gene sequence and morphology. Am J Bot. 2001;88:313–25. [PubMed] [Google Scholar]
- 21.Simmons MP, Savolainen V, Clevinger CC, Archer RH, Davis JI. Phylogeny of the Celastraceae inferred from 26S nrDNA, phytochrome B, atpB, rbcL, and morphology. Molec Phylog Evol. 2001;19:353–66. doi: 10.1006/mpev.2001.0937. [DOI] [PubMed] [Google Scholar]
- 22.Jordaan M, van Wyk AE. Sectional classification of Gymnosporia (Celastraceae), with notes on the nomenclatural and taxonomic history of the genus. Taxon. 2006;55:515–25. [Google Scholar]
- 23.New York: ITHAKA; © 2000-2010. [cited 2010 Jun 15]. Available from: http://www.aluka.com . [Google Scholar]
- 24.Alvarenga N, Ferro EA. Bioactive triterpenes and related compounds from Celastraceae. In: Atta-ur-Rahman, editor. Studies in Natural Products Chemistry Volume 33, Part 13. Amsterdam: Elsevier Science Publishers; 2006. pp. 239–307. [Google Scholar]
- 25.Joffily A, Vieira RC. Anatomia foliar de Maytenus Mol. Emend Mol. (Celastraceae), ocorrente no Estado do Rio de Janeiro, Brasil. Acta Bot Bras. 2005;19:549–61. [Google Scholar]
- 26.Duarte MR, Debur MC. Stem and leaf morphoanatomy of Maytenus ilicifolia. Fitoterapia. 2005;76:41–9. doi: 10.1016/j.fitote.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 27.da Silva G, Taniça M, Gomes ET, Serrano R, Silva O. Morphoanatomy and histochemistry of Maytenus heterophylla leaf, an African medicine. Planta Med. 2009;75:994. [Google Scholar]
- 28.Serrano R, Gomes ET, Silva O. Botanical characterization of Maytenus senegalensis leaf an African medicinal plant. Planta Med. 2008;74:1131. [Google Scholar]
- 29.Orabi KY, Al-Qasoumi SI, El-Olemy MM, Mossa JS, Muhammad I. Dihydroagarofuran alkaloid and triterpenes from Maytenus heterophylla and Maytenus arbutifolia. Phytochemistry. 2001;58:475–80. doi: 10.1016/s0031-9422(01)00277-1. [DOI] [PubMed] [Google Scholar]
- 30.Pistelli L, Venturi R, Marsili A, Morelli I. Alkaloids and coumarins from Gymnosporia senegalensis var. spinosa (Celastraceae) Biochem Syst Ecol. 1998;26:677–9. [Google Scholar]
- 31.Hussein G, Nakamura N, Meselhy MR, Hattori M. Phenolics from Maytenus senegalensis. Phytochemistry. 1999;50:689–94. [Google Scholar]
- 32.Sosa S, Morelli CF, Tubaro A, Cairoli P, Speranza G, Manitto P. Anti-inflammatory activity of Maytenus senegalensis root extracts and of maytenoic acid. Phytomedicine. 2007;14:109–14. doi: 10.1016/j.phymed.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 33.Lindsey KL, Budesinsky M, Kohout L, van Staden J. Antibacterial activity of maytenonic acid isolated from the root-bark of Maytenus senegalensis. S Afr J Bot. 2006;72:473–7. [Google Scholar]
- 34.Muregi FW, Ishih A, Suzuki T, Kino H, Amano T, Mkoji GM, et al. In vivo antimalarial activity of aqueous extracts from Kenyan medicinal plants and their chloroquine (CQ) potentiation effects against a blood-induced CQ-resistant rodent parasite in mice. Phytother Res. 2007;21:337–43. doi: 10.1002/ptr.2067. [DOI] [PubMed] [Google Scholar]
- 35.Clarkson C, Maharaj VJ, Crouch NR, Grace OM, Pillay P, Matsabisa MG, et al. In vitro antiplasmodial activity of medicinal plants native to or naturalized in South Africa. J Ethnopharmacol. 2004;92:177–91. doi: 10.1016/j.jep.2004.02.011. [DOI] [PubMed] [Google Scholar]
- 36.El Tahir A, Satti GMH, Khalid SA. Antiplasmodial activity of selected Sudanese medicinal plants with emphasis on Maytenus senegalensis (Lam.) Exell J Ethnopharmacol. 1999;64:227–33. doi: 10.1016/s0378-8741(98)00129-9. [DOI] [PubMed] [Google Scholar]
- 37.El Tahir A, Ibrahim AM, Satti GM, Theander TG, Kharazmi A, Khalid SA. The potential antileishmanial activity of some Sudanese medicinal plants. Phytother Res. 1998;12:576–9. [Google Scholar]
- 38.Matu EN, van Staden J. Antibacterial and anti-inflammatory activities of some plants used for medicinal purposes in Kenya. J Ethnopharmacol. 2003;87:35–41. doi: 10.1016/s0378-8741(03)00107-7. [DOI] [PubMed] [Google Scholar]
- 39.Khalid SA, Friedrichsen GM, Christensen SB, El Tahir A, Satti GM. Isolation and characterization of pristimerin as the antiplasmodial and antileishmanial agent of Maytenus senegalensis (Lam.) Exell Arkivoc. 2007;9:129–34. [Google Scholar]
- 40.Lall N, Meyer JJM. In vitro inhibition of drug-resistant and drugsensitive strains of Mycobacterium tuberculosis by ethnobotanically selected South African plants. J Ethnopharmacol. 1999;66:347–54. doi: 10.1016/s0378-8741(98)00185-8. [DOI] [PubMed] [Google Scholar]
- 41.Jorge RM, Leite JP, Oliveira AB, Tagliati CA. Evaluation of antinociceptive, anti-inflammatory and ulcerogenic activities of Maytenus ilicifolia. J Ethnopharmacol. 2004;94:93–100. doi: 10.1016/j.jep.2004.04.019. [DOI] [PubMed] [Google Scholar]
- 42.Kimura E, Albiero AL, Cuman RK, Caparroz-Assef SM, Oga S, Bersani-Amado CA. Effect of Maytenus aquifolium extract on the pharmacokinetic and anti-inflammatory effectiveness of piroxicam in rats. Phytomedicine. 2000;7:117–21. doi: 10.1016/S0944-7113(00)80083-5. [DOI] [PubMed] [Google Scholar]
- 43.Backhouse N, Delporte C, Negrete R, Munoz O, Ruiz R. Antiinflammatory and antipyretic activities of Maytenus boaria. Pharmaceut Biol. 1994;32:239–44. [Google Scholar]
- 44.dos Santos VL, Costa VB, Agra MF, Silva BA, Batista LM. Pharmacological studies of ethanolic extracts of Maytenus rigida Mart (Celastraceae) in animal models. Rev Bras Farmacogn. 2007;17:336–42. [Google Scholar]
- 45.da Silva G, Taniça M, Rocha J, Serrano R, Gomes ET, Sepodes B, et al. In vivo anti-inflammatory effect and toxicological screening of Maytenus heterophylla and Maytenus senegalensis extracts. Hum Exp Toxicol [Internet] 2000. Jul 29, [cited 2011 May 10]. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20670987 . [DOI] [PubMed]


