Abstract
Hip fracture incidence appears to be declining in the United States, but changes in bone mineral density (BMD) of the population have not been evaluated. We used femur BMD data from the National Health and Nutrition Examination Survey (NHANES) 2005–2006 to estimate the prevalence of low femoral BMD in adults age 50 years and older and compared it with estimates from NHANES III (1988–1994). Dual-energy X-ray absorptiometry systems (pencil-beam geometry in NHANES III, fan-beam geometry in NHANES 2005–2006) were used to measure femur BMD, and World Health Organization (WHO) definitions of low BMD were used to categorize skeletal status. In 2005–2006, 49% of older US women had osteopenia and 10% had osteoporosis at the femur neck. In men, 30% had femur neck osteopenia and 2% had femur neck osteoporosis. An estimated 5.3 million older men and women had osteoporosis at the femur neck, and 34.5 million more had osteopenia in 2005–2006. When compared with NHANES III, the age-adjusted prevalence of femur neck osteoporosis in NHANES 2005–2006 was lower in men (by 3 percentage units) and women (by 7 percentage units) overall and among non-Hispanic whites. Changes in body mass index or osteoporosis medication use between surveys did not fully explain the decline in osteoporosis. Owing to the increase in the number of older adults in the US population, however, more older adults had low femur neck BMD (osteoporosis + osteopenia) in 2005–2006 than in 1988–1994. Thus, despite the decline in prevalence, the estimated number of affected older adults in 2005–2006 remained high.
Keywords: FEMORAL NECK, OSTEOPOROSIS, TOTAL HIP, RACE; ETHNICITY, GENDER, SECULAR TRENDS
Introduction
Recent fracture incidence data suggest that hip fracture rates may be declining in the United States,(1,2) but whether this decline is associated with improvements in bone mineral density (BMD) or due to other factors is unknown. The most recent nationally representative estimates of osteoporosis prevalence, based on femur BMD data from the third National Health and Nutrition Examination Survey (NHANES III, 1988–1994), were published a decade ago.(3) Total-body and regional BMD data from NHANES 1999–2004 have been published,(4) but these cannot provide osteoporosis estimates for the femur neck, which has been proposed by the World Health Organization (WHO)(5) as the skeletal site that should be used for the description of osteoporosis in populations. To address these data gaps, proximal femur bone density measurements by dual-energy X-ray absorptiometry (DXA) were included in the continuous NHANES beginning in 2005. Not only can these data can provide more recent estimates of the prevalence of osteoporosis based on the recommended femur neck skeletal site, but they also can provide estimates of osteoporosis prevalence at the total hip, the skeletal site on which the osteoporosis objective in Healthy People 2010 is based.(6) Finally, these data allow a comparison of osteoporosis prevalence in representative samples of the noninstitutionalized US population that were assessed at two different time points so that changes in bone status over time can be examined. The specific objectives of this study are to (1) assess the prevalence of low bone density at the femur neck and total hip in US adults aged 50 years and older in 2005–2006, (2) compare the prevalence of low total hip BMD in 2005–2006 with target prevalence goals identified for the population in Healthy People 2010, and (3) contrast the prevalence of low bone density at the femur neck and total hip in 2005–2006 with those observed in NHANES III.
Methods
Sample
The NHANES are conducted by the National Center for Health Statistics (NCHS), Centers for Disease Control and Prevention, to assess the health and nutritional status of large representative cross-sectional samples of the noninstitutionalized civilian US population. In NHANES III, a nationally representative sample was obtained in two 3-year cycles between 1988 and 1994. Starting in 1999, data from a nationally representative sample have been collected each year, but data are released for 2-year periods to protect confidentiality and increase statistical reliability. The present study was based on data collected in NHANES 2005–2006. In each NHANES, data were collected via household interviews and direct standardized physical examinations conducted in specially equipped mobile examination centers.(7,8) All procedures in both surveys were approved by the NCHS Institutional Review Board, and written informed consent was obtained from all subjects.
NHANES III and NHANES 2005–2006 were designed to provide reliable estimates for three race/ethnic groups: non-Hispanic whites, non-Hispanic blacks, and Mexican Americans. Race and ethnicity were self-reported by the participants. A total of 10,995 adults age 50 years and older were eligible to participate in NHANES III. Of the eligible sample, 8654 (79%) were interviewed, and 7155 (65%) were examined. The present study uses data for 6401 adults age 50 years and older with valid nonmissing femur BMD data from NHANES III, which represents 58% of the sample in this age range who were originally selected for NHANES III, 74% of the participants in this age range who were interviewed, and 89% of those who received physical examinations. A total of 3157 adults age 50 years and older were eligible to participate in NHANES 2005–2006. Of these, 2214 (70%) were interviewed, and 2119 (68%) were examined. The analytic sample from NHANES 2005–2006 was limited to 1614 adults age 50 years and older with valid, nonmissing femur BMD data, which represents 51% of the participants in this age range who were eligible to participate in the survey, 73% of the interviewed participants, and 76% of those who received physical examinations.
Variables
As described elsewhere,(9) femur BMD was measured in NHANES 2005–2006 with Hologic QDR 4500A fan-beam densitometers (Hologic, Inc., Bedford, MA, USA) using Discovery version 12.4 software. Scanning was done in the fast mode. In NHANES III, femur BMD was measured with Hologic QDR 1000 pencil-beam densitometers.(10) Rigorous quality-control (QC) programs were employed in both surveys, which included use of anthropomorphic phantoms and review of each QC and respondent scan at a central site (Department of Radiology, University of California San Francisco in NHANES 2005–2006 and Department of Diagnostic Radiology, Mayo Clinic in NHANES III).(9,10) In both surveys, the left hip was scanned unless there was a history of previous fracture or surgery.
To address the potential impact of the change in DXA methodology between surveys, a literature search was performed to identify the magnitude of the difference that might be expected when the same individuals were measured on both scanner types.(18–21) The largest discrepancy between the two scanners found in published studies was a difference of ± 3% at either the femur neck or total hip.(18,21) Accordingly, the BMD values of each respondent from NHANES 2005–2006 were raised or lowered by 3%. Estimates of osteoporosis, as defined below, that were based on the adjusted BMD values from NHANES 2005–2006 then were calculated and compared with the prevalence estimates from NHANES III (data not shown). Although the magnitude of the prevalence estimates was altered by this adjustment, conclusions regarding the differences in prevalence between surveys were the same as when based on the observed BMD values except in one case (when BMD was lowered by 3% in men). As a result, the observed BMD values from both surveys were used in the present study without adjustment for the difference in DXA methods.
In the present study, BMD data at the femur neck and total hip were analyzed. The femur neck was chosen because it has been proposed as the reference skeletal site for defining osteoporosis in epidemiologic studies.(5) The total hip was included because it is the skeletal site used in the Healthy People 2010 objective related to osteoporosis.(6) Definitions of osteopenia and osteoporosis were based on criteria outlined by WHO in 1994(11):
Osteopenia: BMD between 1 standard deviation (SD) and 2.5 SD below the mean of the young reference group.
Osteoporosis: BMD 2.5 SD or more below the mean of the young reference group.
As recommended more recently by the WHO,(5) 20- to 29-year-old non-Hispanic white women from NHANES III(3) were used as the reference group to derive these cutoff values for men and women in both surveys. The specific NHANES III cutoff values used to define osteopenia were 0.561 to 0.74 g/cm2 and 0.641 to 0.82 g/cm2 for the femur neck and total hip, respectively.(3) The thresholds for osteoporosis were 0.56 g/ cm2 or less and 0.64 g/cm2 or less for the femur neck and total hip, respectively.(3)
Two potential explanatory factors related to secular trends in BMD were examined in the present study: body mass index (BMI) and use of osteoporosis medications. These variables were chosen because they have been shown to be strongly related to BMD,(12,13) and there is also evidence that changes have occurred in the population since NHANES III.(14–16) BMI was calculated as body weight (kilograms) divided by height (meters squared). In both surveys, body weight was measured to the nearest 0.01 kg using an electronic load-cell scale, and standing height was measured with a fixed stadiometer.
Osteoporosis medication users were defined as those who self-reported having been treated for osteoporosis and/or were currently taking the prescription medications described below. Data to define users of osteoporosis medications were collected in a comparable manner in both surveys. Respondents who self-reported having been diagnosed with osteoporosis by a physician were asked if they had been treated for it. In addition, all respondents, regardless of whether they had self-reported having been diagnosed with osteoporosis, showed the containers for all current prescription medications to the interviewer, who recorded the name of the product. Medications were assigned standard generic names and four-digit generic codes using the Physicians’ GenRx(17) in NHANES III. The December 2007 Multum Lexicon Drug Database (Cerner Multum, Inc., Denver CO; www.multum.com/Lexicon.htm) was used to assign generic drug names and codes in NHANES 2005–2006.
Osteoporosis medications were defined as medications included in a recent systematic review of the comparative effectiveness of treatments to prevent osteoporotic fractures.(13) In NHANES III, these included calcitonin, calcitriol, ergocalciferol, etidronate, sodium fluoride, tamoxifen, calcium acetate, and sex hormones (i.e., estrogen and testosterone, as defined below). In NHANES 2005–2006, they included bisphosphonates (e.g., alendronate, risedronate, etidronate, pamidronate, tiludronate, ibandronate, and zolendronate), calcitonin, calcitriol, fluoride, raloxifene, tamoxifen, tibolone, strontium ranelate, parathyroid hormone, teriparatide, and sex hormones (i.e., estrogen and testosterone). The Multum drug therapeutic category codes for estrogen and testosterone were used to identify the relevant sex hormone treatments in NHANES 2005–2006. Generic drugs corresponding to these Multum drug therapeutic codes were considered to be in these categories in NHANES III as well. “Estrogens” included estradiol, estradiol valerate, estrogenic substances, conjugated estrogens, esterified estrogens (alone and with methyltestosterone), estropipate, ethinyl estradiol (alone or with ethynodiol diacetate, levonorgestrel, norethindrone, norethindrone acetate, or desogestrel), diethylstilbesterol (alone or with disphosphate), fluoxymesterone, and quinestrol. “Testosterones” included testosterone, testosterone cypionate, stanozolol, and nandrolone decanoate.
Education was included as a variable in order to make comparisons with subgroups identified in the osteoporosis objective in Healthy People 2010.(6) Education was defined as numbers of years of schooling completed and was categorized as less than high school, high school, and more than high school to be consistent with categories used in the Healthy People 2010 osteoporosis objective.
Statistical analysis
Analyses were conducted with PC-SAS (version 9.1, SAS Institute, Cary, NC, USA) and SUDAAN (version 9.03, Research Triangle Institute, NC, USA). All analyses used sample weights and took into account the complex design of the survey. When multiple comparisons of estimates between groups were made, a Bonferoni correction was used.
BMD means by age and race/ethnicity were calculated for NHANES 2005–2006 using linear regression and adjusting for the other characteristic in the model. The prevalence of low BMD at the femur neck and total hip in 2005–2006 was calculated by sex and age group, and differences by age and sex were tested using logistic regression. Prevalence estimates for the total population and by race/ethnicity were age standardized to the US Census 2000 population estimates when not provided by detailed age groups. Estimates of the number of older US adults with poor skeletal status were calculated by multiplying the unadjusted prevalences for age 50+ by Census Current Population Survey estimates of the noninstitutionalized US population for 2005–2006 (www.cdc.gov/nchs/about/major/nhanes/nhanes_cps_totals.htm).
Changes in the prevalence of low femur BMD between NHANES III and NHANES 2005–2006 were examined by calculating the age-standardized prevalence in each survey for the total population age 50 years and older and by sex and race/ ethnicity. Differences between age-standardized prevalences were tested using a t test. Differences between the two surveys also were tested using logistic regression models that included age and the survey time period.
Secondary analyses were done to assess the potential impact of changes in BMI and osteoporosis medications on the observed difference in prevalence of femur neck osteoporosis. These analyses were stratified by race/ethnicity in order to avoid potential confounding by this variable in the relationships. The analyses were limited to non-Hispanic whites owing to statistically unreliable prevalence estimates of osteoporosis and/ or medication use in the other groups. To assess the potential impact of differences in BMI and medication use, the prevalences before and after adjusting for those two factors were calculated using logistic regression models that also included age and the survey time period as variables.
Results
Mean femur neck and total hip BMD by age, sex, and race/ ethnicity are shown in Table 1 for adults age 50 years and older after adjusting for the other variables shown in the table. Age was significantly negatively related to BMD overall at the femur neck (beta = −0.0032 and −0.0050 for men and women, respectively, p <.001) and total hip (beta = −0.0027 and −0.0056 for men and women, respectively, p <.001). However, the sexes differed in regard to the specific pattern of differences between successive decades. In women, mean BMD was significantly lower in each successive age decade at both skeletal sites. In men, however, only the difference between 60 to 69 years and 70 to 79 years reached statistical significance at either skeletal site. Race/ethnicity also was related significantly to BMD at both femur sites. Non-Hispanic blacks had a significantly higher age-adjusted mean BMD than whites at both skeletal sites in both sexes (see Table 1). Age-adjusted mean femur neck BMD was significantly higher in Mexican-American women than non-Hispanic white women, but age-adjusted mean total hip BMD did not differ significantly between these two groups of women. Among men, non-Hispanic whites and Mexican Americans had similar age-adjusted mean BMDs at both skeletal sites.
Table 1.
Adjusted Mean Femur Neck and Total Hip BMD1 by Age and Race/Ethnicity Among Men and Women: NHANES 2005–2006
| Femur neck | Total hip | ||||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| n | Mean2 | SEM | p Value* | Mean2 | SEM | p Value* | |
| Women | |||||||
| Age (years) | .001 | .001 | |||||
| 50–59 | 235 | 0.763a | 0.012 | 0.895a | 0.012 | ||
| 60–69 | 241 | 0.729ab | 0.007 | 0.858ab | 0.009 | ||
| 70–79 | 157 | 0.664bc | 0.006 | 0.786bc | 0.009 | ||
| 80+ | 107 | 0.623c | 0.010 | 0.728c | 0.012 | ||
| Race/ethnicity | .001 | .02 | |||||
| Non-Hispanic white | 437 | 0.714ab | 0.005 | 0.843a | 0.006 | ||
| Non-Hispanic black | 146 | 0.786a | 0.012 | 0.894a | 0.014 | ||
| Mexican American | 120 | 0.761b | 0.015 | 0.880 | 0.022 | ||
| Men | |||||||
| Age (years) | .001 | .004 | |||||
| 50–59 | 271 | 0.833 | 0.009 | 1.010 | 0.009 | ||
| 60–69 | 273 | 0.813a | 0.009 | 1.000a | 0.008 | ||
| 70–79 | 203 | 0.768a | 0.015 | 0.954a | 0.015 | ||
| 80+ | 127 | 0.733 | 0.013 | 0.922 | 0.015 | ||
| Race/ethnicity | .001 | .001 | |||||
| Non-Hispanic white | 530 | 0.803a | 0.004 | 0.986a | 0.005 | ||
| Non-Hispanic black | 179 | 0.889ab | 0.013 | 1.072ab | 0.007 | ||
| Mexican American | 130 | 0.807b | 0.011 | 0.984b | 0.006 | ||
Means for each characteristic have been adjusted for the other characteristic shown in the table.
Means sharing common superscripts within sex group differ significantly, p <.05.
p value for overall F test for this variable from linear regression.
The crude, or unadjusted, prevalence and estimated millions of older adults (all races combined) with osteoporosis and osteopenia at both femur sites in 2005–2006 by sex are shown in Table 2. Forty-nine percent of older women and 30% of older men had osteopenia at the femur neck, whereas 10% of women and 2% of men had osteoporosis at this site. The prevalence of low BMD was lower at the total hip; for example, among older women, 36% had osteopenia, and 7 percent had osteoporosis. Multiplying these prevalences by 2005–2006 Census Current Population Survey estimates revealed that roughly 40 million older adults had low BMD at the femur neck (34.5 million with osteopenia + 5.3 million with osteoporosis). Comparable estimates for women at the total hip are 0.3 million with osteoporosis and 8.3 million with osteopenia. The number of older men with total hip osteoporosis could not be reliably estimated, but 1.4 million were estimated to have osteopenia at the total hip.
Table 2.
Crude Prevalence of Low Femur Neck and Total Hip BMD by Sex Among Adults Age 50+ Years: NHANES 2005–2006
| Osteopenia | Osteoporosis | ||||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| n | % | SE | Millions | % | SE | Millions | |
| Femur neck | |||||||
| Women | 740 | 49 | 2.3 | 22.7 | 10 | 0.9 | 4.5 |
| Men | 874 | 30 | 1.4 | 11.8 | 2 | 0.3 | 0.8 |
| Total hip | |||||||
| Women | 740 | 36 | 2.1 | 8.3 | 7 | 1.1 | 0.3 |
| Men | 874 | 12 | 1.0 | 1.4 | –a | –a | –a |
Unreliable; standard error/mean > 40% or estimate was zero.
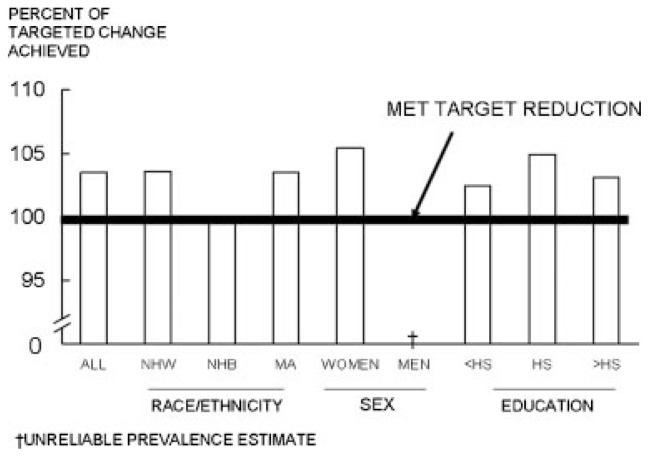
Estimates of total hip osteoporosis in 2005–2006 are compared with targets set by the osteoporosis objective in Healthy People 2010 in Fig. 1. The observed prevalences achieved 100% to 105% of the target reduction set for this objective depending on the demographic category considered.
Fig. 1.
Percent of reduction in osteoporosis prevalence targeted by Healthy People 2010 that was achieved by US adults aged 50 years and older in 2005–2006.
Age-adjusted estimates of osteoporosis and osteopenia prevalence at both femur sites are compared between NHANES 2005–2006 and NHANES III by age, sex, and race/ethnicity in Table 3. The prevalence of osteoporosis declined between surveys in both sexes overall, as well as among non-Hispanic white men and women. The decline was larger among women than men; for example, the prevalence of femur neck osteoporosis was 7 percentage units lower in NHANES 2005–2006 than in NHANES III among women versus 3 percentage units lower in men. However, the prevalence of osteoporosis was similar in the two surveys in non-Hispanic black women and also did not differ significantly between surveys among Mexican-American women, although the estimates tended to be lower in 2005–2006 (see Table 3). Estimates could not be compared between surveys among non-Hispanic black or Mexican-American men owing to a lack of statistically reliable estimates for 2005–2006.
Table 3.
Age-Adjusteda Prevalence of Low Femur Neck or Total Hip BMD of Adults Age 50+ Years by Sex and Race/Ethnicity: NHANES III Compared with NHANES 2005–2006
| Femur neck | Total hip | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||
| Sample size | NHANES III | NHANES 2005–2006 | NHANES III | NHANES 2005–2006 | ||||||
|
|
|
|
|
|
||||||
| NHANES III | NHANES 2005–2006 | % | SE | % | SE | % | SE | % | SE | |
| Osteopenia | ||||||||||
| Women | ||||||||||
| Total | 3311 | 740 | 49 | 1.2 | 50 | 2.2 | 39 | 0.8 | 37 | 2 |
| Non-Hispanic white | 1880 | 437 | 51 | 1.3 | 52 | 2.6 | 41 | 0.9 | 39 | 2.7 |
| Non-Hispanic black | 695 | 146 | 36 | 2.1 | 36 | 4.1 | 28 | 1.4 | 25 | 2.4 |
| Mexican American | 600 | 120 | 47 | 1.6 | 38 | 3.4 | 38 | 2.1 | 22* | 3.8 |
| Men | ||||||||||
| Total | 3090 | 874 | 34 | 1.2 | 32 | 1.4 | 17 | 1.1 | 13 | 1.1 |
| Non-Hispanic white | 1723 | 530 | 35 | 1.3 | 33 | 1.8 | 18 | 1.4 | 14 | 1.5 |
| Non-Hispanic black | 647 | 179 | 20 | 1.9 | 22 | 3.6 | 12 | 1.2 | 7 | 1.8 |
| Mexican American | 625 | 130 | 27 | 1.6 | 34 | 5.2 | 13 | 1.4 | 12 | 3.0 |
| Osteoporosis | ||||||||||
| Women | ||||||||||
| Total | 3311 | 740 | 18 | 0.9 | 11* | 0.7 | 16 | 0.7 | 8* | 1.0 |
| Non-Hispanic white | 1880 | 437 | 19 | 1.0 | 11* | 1.0 | 16 | 0.9 | 8* | 1.0 |
| Non-Hispanic black | 695 | 146 | 7 | 1.4 | 7 | 2.3 | 10 | 1.4 | 8 | 2.3 |
| Mexican American | 600 | 120 | 16 | 2.1 | 10 | 2.6 | 18 | 2.7 | 8 | 2.5 |
| Men | ||||||||||
| Total | 3090 | 874 | 5 | 0.6 | 2* | 0.3 | 3 | 0.3 | –c | –c |
| Non-Hispanic white | 1723 | 530 | 5 | 0.7 | 2* | 0.3 | 3 | 0.4 | –c | –c |
| Non-Hispanic black | 647 | 179 | 3b | 1.0 | –c | –c | 2 | 0.7 | –c | –c |
| Mexican American | 625 | 130 | 2 | 0.3 | –c | –c | 2 | 0.4 | –c | –c |
Age standardized by the direct method to the 2000 Census.
May be unreliable; standard error/mean >30% and <40%.
Unreliable; standard error/mean >40% or estimate was zero.
p <.05 comparing NHANES III with NHANES 2005–2006 within sex and race/ethnic group with Bonferroni adjustment.
In contrast, the prevalence of osteopenia did not differ between surveys in any group except Mexican-American women, in whom the prevalence in 2005–2006 was significantly lower at the total hip (see Table 3). The lack of difference in osteopenia between surveys despite a decline in osteoporosis may be due to the location of the osteoporosis and osteopenia cutoff values in the BMD distribution coupled with differences in the shape of the BMD distributions between the two surveys. The cutoff values for osteoporosis fall in the tail region of the BMD distribution, where differences in the BMD distribution between the surveys were more pronounced. The cutoff values for osteopenia fall more in the center of the BMD distribution, where differences between surveys were less pronounced.
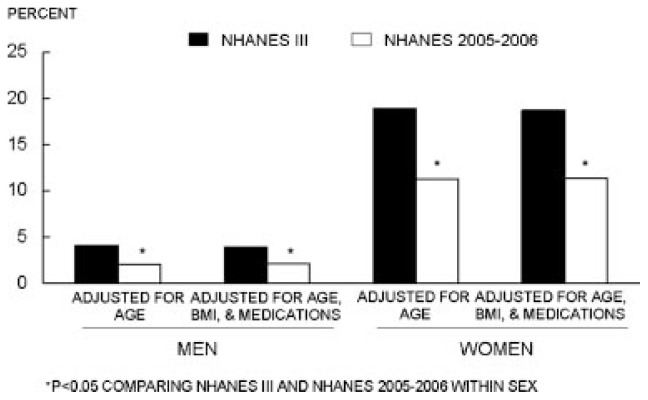
Secondary analyses were performed to assess the impact of changes in BMI and medication use that might underlie the observed difference in osteoporosis between NHANES III and NHANES 2005–2006. Figure 2 provides a comparison of femur neck osteoporosis prevalence between NHANES III and NHANES 2005–2006 before and after adjusting for BMI and medication use differences in the two surveys. Adjusting for these two factors had almost no impact on prevalence estimates, which remained significantly lower in 2005–2006.
Fig. 2.
Femur neck osteoporosis in non-Hispanic white adults aged 50 years and older, before and after adjusting for body mass index.
Discussion
The prevalence of osteoporosis, whether defined by femur neck or total hip BMD, appears to have declined between 1988–1994 and 2005–2006 in older US adults. The overall decline is consistent with the decline in hip fracture incidence that has been observed in other national and community-based studies in this country over the same time period.(1,2) This decline results in reduced prevalence estimates that meet or exceed the reductions set as the target in Healthy People 2010.(6) The decline is most evident among non-Hispanic whites. Smaller changes were observed among non-Hispanic blacks and Mexican Americans that did not reach statistical significance possibly owing to their smaller sample sizes in NHANES 2005–2006. Nonetheless, the estimated reduction in osteoporosis prevalence observed among non-Hispanic blacks and Mexican Americans in 2005–2006 met the targets set for these groups in Healthy People 2010.
Despite the apparent decline in low femur BMD between NHANES III and NHANES 2005–2006, the estimated number of affected older adults remains high. For example, an estimated 5.3 million older men and women had osteoporosis at the femur neck, and 34.5 million had osteopenia in 2005–2006. Comparable figures for 1988–1994 from NHANES III were 7.3 million with femur neck osteoporosis and 26.3 million with femur neck osteopenia.(3) Thus the increase in the number of older adults in the US population led to more older adults having low femur neck BMD (osteoporosis + osteopenia) in 2005–2006 (39.8 million) than in 1988–1994 (33.6 million) despite the decline in osteoporosis prevalence.
The decline in femoral osteoporosis did not appear to be strongly associated with two bone-related factors known to have changed in the population between the two time periods examined: an increase in BMI(14,15) and approval of new medications (e.g., several bisphosphonates and teriparatide) to prevent and treat osteoporosis.(13,16) We had previously projected that the increase in BMI was unlikely to significantly reduce the prevalence of osteoporosis in older women despite its strong relationship with BMD(12) because the increase in overweight was confined to a fairly small proportion of the total population of older women.(22) The present results support our earlier projections. The lack of impact of medication use in the present study also may stem in part from the small increase in use: 10% of our NHANES III sample compared with 16% of our NHANES 2005–2006 sample were currently taking prescription osteoporosis medications or reported ever receiving treatment for osteoporosis. Not unexpectedly, the type of medications differed between surveys, being almost exclusively estrogen in the NHANES III and almost exclusively bisphosphonates in the NHANES 2005–2006. Whether these two drug classes have similar effects on femur BMD is not certain because, to our knowledge, head-to-head randomized clinical trials have not been conducted. Meta-analyses of randomized trials of each class separately have been performed, however. Between-trial comparisons must be interpreted with caution owing to the potential impact of variability in study designs, but the meta-analysis results suggest that these two drug classes may have similar effects on femur BMD.(23) Furthermore, six head-to-head randomized clinical trials found no difference in fracture incidence in patients using these two drug classes.(13)
Differences in the DXA technology used in the two surveys also may have contributed to the observed decline in prevalence. Devices from the same manufacturer were used in both surveys, but NHANES III used first-generation pencil-beam instruments (QDR 1000), whereas NHANES 2005–2006 used third-generation fan-beam instruments (QDR 4500a/Discovery). The DXA manufacturer performed calibration studies between sequential generations of DXA instruments so that the old and new systems would provide equivalent BMD values within the average accepted level of agreement between any two DXA systems of roughly ±2%. However, a direct in vivo comparison between the QDR 1000 and QDR 4500a/Discovery was not made (Thomas Kelly, personal communication, Hologic, Inc.). We found only a small number of published studies with in vivo results for the QDR 1000 compared directly with any version of the QDR 4500a,(18–21) and they differed somewhat in the estimated magnitude and direction of the BMD difference for a particular femur region of interest. Some studies found that the difference between DXA systems depended on the subject’s BMD value,(18) whereas others did not.(20,21) This lack of consistency prevented us from developing a robust statistical adjustment to remove the effects of the DXA system change from the NHANES data set. Instead, we performed a sensitivity analysis in which we raised or lowered each NHANES 2005–2006 respondent’s BMD value by 3% and reexamined differences in prevalence between NHANES 2005–2006 and NHANES III. Conclusions were unchanged for women regardless of how BMD was adjusted and changed for men only when BMD values were adjusted by −3%. This suggests, but cannot establish, that differences in DXA technology are unlikely to fully explain the apparent decline seen between surveys, at least in women. Interpretation of the change in prevalence among men is complicated by the low prevalence estimates observed in both surveys.
Race/ethnic differences in femur BMD were similar to those seen in NHANES III,(24) with non-Hispanic blacks having the highest BMD values and non-Hispanic whites having the lowest values. Mexican Americans had BMD values that generally fell between those of non-Hispanic blacks and whites, although not all the differences were statistically different. Interestingly, Mexican Americans had lower BMD values than non-Hispanic whites for the total body and at several large skeletal subregions when total-body BMD values from NHANES 1999–2004 were examined.(4) The use of different population samples in NHANES 1999–2004 versus 2005–2006 could have contributed to this discrepancy, but a similar discrepancy in ranking of Hispanics versus whites also has been observed in other studies in which both the femur and total-body measurements were made on the same individuals.(25,26) The basis for this discrepancy is unclear. Differences in femur shape between ethnic groups could be a contributing factor. For example, differences in anteroposterior diameter and platymeria, or flattening, of the proximal femur have been noted between whites and Native Americans.(27) Mexican Americans vary in their degree of Native American ancestry, but Klimenditis et al.(28) found that self-identified Mexican Americans in New Mexico had 39% Native American genetic admixture.
This study has limitations beyond the inability to directly address the difference in DXA methods used in the two surveys. The sample from NHANES 2005–2006, although nationally representative, is smaller than the sample from NHANES III and was drawn from fewer locations in the United States, so prevalence estimates from NHANES 2005–2006 may be less stable than those from NHANES III. Nonresponse bias may be present in the estimates from both surveys. Nonresponse bias owing to refusal to participate in the physical examinations in NHANES is reduced by a nonresponse adjustment factor included in the calculation of the sample weights for use with examinee data. Approximately 11% and 24%, respectively, of the NHANES III and NHANES 2005–2006 respondents age 50 years and older who came to the examination centers lacked usable proximal femur DXA data, and this nonresponse is not addressed by the sample weight adjustments. However, results from a detailed nonresponse bias analysis conducted by NCHS prior to public release of the NHANES 2005–2006 femur data suggested that additional adjustments for nonresponse (beyond those performed in the construction of the original examination weights) were not necessary. Finally, institutionalized people, an important at-risk group for osteoporosis,(29) are excluded from the NHANES sampling frame by design.
In summary, the prevalence of osteoporosis, as defined by low femur BMD, appears to have declined among older adults in the United States since the mid-1990s so that osteoporosis reduction targets identified for the population in Healthy People 2010 have been met. The observed decrease in femoral osteoporosis seen between 1988–1994 and 2005–2006 is encouraging, but the number of older US adults with low femur BMDs remains substantial, and annual costs associated with osteoporotic fractures are projected to rise by almost 50%, from $17 billion to $25 billion, between the years 2005 and 2025 owing to the aging of the population.(30) Although it is reasonable to assume that the decline in the prevalence of low femur BMD underlies the fall in hip fracture incidence that has been reported in other studies,(1,2) this could not be addressed directly in the present study owing to a lack of incident fracture data for this sample and thus requires further investigation. Finally, more research is needed to identify factors that underlie the decline in low BMD, which does not appear to be explained by the increase in average BMI of the population or by the introduction of new pharmaceutical treatments for osteoporosis prevention and treatment.
Acknowledgments
The findings and conclusions in this article are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention, the National Institutes of Health, or the Department of Health and Human Services.
Footnotes
Disclosures
All the authors state that they have no conflicts of interest.
References
- 1.Melton LJ, Kearns AE, Atkinson EJ, et al. Secular trends in hip fracture incidence and recurrence. Osteoporos Int. 2009;20:687–694. doi: 10.1007/s00198-008-0742-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gehlbach SH, Avrunin JS, Puleo E. Trends in hospital care for hip fractures. Osteoporos Int. 2007;18:585–591. doi: 10.1007/s00198-006-0281-0. [DOI] [PubMed] [Google Scholar]
- 3.Looker AC, Orwoll ES, Johnston CC, et al. Prevlance of low femoral bone density in older US adults from NHANES III. J Bone Miner Res. 1997;12:1761–1768. doi: 10.1359/jbmr.1997.12.11.1761. [DOI] [PubMed] [Google Scholar]
- 4.Looker AC, Melton LJ, Harris T, Borrud L, Shepherd J, McGowan J. Age, gender, and race/ethnic differences in total body and subregional bone density. Osteoporos Int. 2009;20:1141–1149. doi: 10.1007/s00198-008-0809-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kanis JA, McCloskey EV, Johansson H, Oden A, Melton LJ, Khaltaev N. A reference standard for the description of osteoporosis. Bone. 2008;42:467–75. doi: 10.1016/j.bone.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 6.US Department Health and Human Services. Healthy People 2010. 2nd ed. Washington: US Government Printing Office; 2000. Arthritis, osteoporosis and back conditions; pp. 17–18. [Google Scholar]
- 7.Centers for Disease Control and Prevention, National Center for Health Statistics. Current National Health and Nutrition Examination Survey (NHANES), 1999. [Accessed February 2, 2009]. Available at: www.cdc.gov/nchs/about/major/nhanes/currentnhanes.htm.
- 8.National Center for Health Statistics. Plan and operation of the third National Health and Nutrition Examination Survey, 1988–1994. DHHS Publ No. (PHS) 94-1308. [Accessed February 2, 2009];Vital Health Stat. 1994 1(32) Available at: www.cdc.gov/nchs/data/nhanes/nhanes3. [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention, National Center for Health Statistics. Documentation, codebook and frequencies: dual-energy x-ray absorptiometry—bone measurements, survey years 2005 to 2006, January 2009. [Accessed February 2, 2009]. Available at: www.cdc.gov/nchs/data/nhanes/nhanes_05_06/dxxfem_d.pdf.
- 10.Wahner HW, Looker AC, Dunn WL, Walters LC, Hauser MF, Novak C. Quality control of bone densitometry in a national health survey (NHANES III) using three mobile examination centers. J Bone Miner Res. 1994;9:951–960. doi: 10.1002/jbmr.5650090621. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization. Technical Report Series No. 843. Geneva, Switzerland: WHO; 1994. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. [PubMed] [Google Scholar]
- 12.Reid IR. Relationships between fat and bone. Osteoporos Int. 2008;19:595–606. doi: 10.1007/s00198-007-0492-z. [DOI] [PubMed] [Google Scholar]
- 13.MacLean C, Alexander A, Carter J, et al. Comparative Effectiveness Review No. 12. Rockville, MD: Agency for Healthcare Research and Quality; Dec, 2007. Comparative effectiveness of treatments to prevent fractures in men and women with low bone density or osteoporosis. [PubMed] [Google Scholar]
- 14.Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults. 1999–2000. JAMA. 2002;288:1723–1727. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- 15.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States. 1999–2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 16.Stafford RS, Drieling RL, Hersh AL. National trends in osteoporosis visits and osteoporosis treatment, 1988–2003. Arch Intern Med. 2004;164:1525–1530. doi: 10.1001/archinte.164.14.1525. [DOI] [PubMed] [Google Scholar]
- 17.Denniston PL, Epner JA, editors. 1993 Physicians’ GenRx, 1994: The Official Drug Reference. Smithtown, NY: Data Pharmaceutica, Inc; 1993. [Google Scholar]
- 18.Bouyoucef SE, Cullum ID, Ell PJ. Cross-calibration of a fan-beam X-ray densitometer with a pencil-beam system. Br J Radiol. 1996;69:522–531. doi: 10.1259/0007-1285-69-822-522. [DOI] [PubMed] [Google Scholar]
- 19.Barthe N, Braillon P, Ducassou D, Basse-Cathalinat B. Comparison of two Hologic DXA systems (QDR 1000 and QDR 4500/A) Br J Radiol. 1997;70:728–739. doi: 10.1259/bjr.70.835.9245885. [DOI] [PubMed] [Google Scholar]
- 20.Kolta S, Ravaud P, Fechtenbaum J, Dougados M, Roux C. Follow-up of individual patients on two DXA scanners of the same manufacturer. Osteoporos Int. 2000;11:709–713. doi: 10.1007/s001980070070. [DOI] [PubMed] [Google Scholar]
- 21.Henzell S, Dhaliwal SS, Price RI, et al. Comparison of pencil-beam and fan-beam DXA systems. J Clin Densitometr. 2003;6:205–210. doi: 10.1385/jcd:6:3:205. [DOI] [PubMed] [Google Scholar]
- 22.Looker AC, Flegal KM, Melton LJ. Impact of increased overweight on the projected prevalence of osteoporosis in older women. Osteoporos Int. 2007;18:307–313. doi: 10.1007/s00198-006-0241-8. [DOI] [PubMed] [Google Scholar]
- 23.Cranney A, Guyatt G, Griffith L, et al. and the Osteoporosis Methodology Group and the Osteoporosis Research Advisory Group. Summary of meta-analyses of therapies for postmenopausal osteoporosis, IX. Endocrine Rev. 2002;23:570–578. doi: 10.1210/er.2001-9002. [DOI] [PubMed] [Google Scholar]
- 24.Looker AC, Wahner HW, Dunn WL, et al. Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int. 1998;8:468–489. doi: 10.1007/s001980050093. [DOI] [PubMed] [Google Scholar]
- 25.Araujo AB, Travison TG, Harris SS, Holick MF, Turner AK, McKinlay JB. Race/ethnic differences in bone mineral density in men. Osteoporos Int. 2007;18:943–953. doi: 10.1007/s00198-006-0321-9. [DOI] [PubMed] [Google Scholar]
- 26.Morton DJ, Barrett-Connor E, Kritz-Silverstein D, Wingard DL, Schneider DL. Bone mineral density in postmenopausal Caucasian, Filipina, and Hispanic women. Int J Epidemiol. 2003;32:150–156. doi: 10.1093/ije/dyg024. [DOI] [PubMed] [Google Scholar]
- 27.Gill GW. Racial variation in the proximal and distal femur: heritability and forensic utility. J Forens Sci. 2001;46:791–799. [PubMed] [Google Scholar]
- 28.Klimentidis YC, Miller GF, Shriver MD. Genetic admixture, self-reported ethnicity, self-estimated admixture, and skin pigmentation among Hispanic and Native Americans. Am J Phys Anthropol. 2009;138:375–383. doi: 10.1002/ajpa.20945. [DOI] [PubMed] [Google Scholar]
- 29.Zimmerman SI, Girman CJ, Buie VC, et al. The prevalence of osteoporosis in nursing home residents. Osteoporos Int. 1999;9:151–157. doi: 10.1007/s001980050129. [DOI] [PubMed] [Google Scholar]
- 30.Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States. 2005–2025. J Bone Miner Res. 2007;22:465–475. doi: 10.1359/jbmr.061113. [DOI] [PubMed] [Google Scholar]