Abstract
DENV1-E106 is a monoclonal antibody (MAb) with strong neutralizing activity against all five DENV-1 genotypes and therapeutic activity in mice. Here, we evaluated the potential for DENV-1 to escape neutralization by DENV1-E106. A single mutation in domain III of the envelope protein (T329A) emerged, which conferred resistance to DENV1-E106. However, the T329A variant virus had differing phenotypes in vitro and in vivo with attenuation in cell culture yet increased infectivity in Aedes aegypti mosquitoes. Mice infected with this T329A variant still were protected against lethal infection by DENV1-E106 even though much of the neutralizing activity was lost. This study reveals the complex dynamics of neutralization escape of an inhibitory MAb against DENV, and suggests that evaluation of therapeutic MAbs requires detailed investigation in relevant hosts.
INTRODUCTION
Dengue virus (DENV) infection after mosquito inoculation causes clinical disease ranging from a self-limiting febrile illness (Dengue Fever, DF) to a life threatening hemorrhagic and capillary leak syndrome (Dengue Hemorrhagic Fever (DHF)/Dengue Shock Syndrome (DSS)). DENV is the most prevalent mosquito-transmitted viral disease and causes an estimated 50 to 100 million infections and 250,000 cases of DHF/DSS per year worldwide, with 2.5 billion people at risk (Halstead, 1988; Monath, 1994). Globally, there is significant diversity among DENV strains, including four serotypes (DENV-1, DENV-2, DENV-3, and DENV-4) that differ at the amino acid level by 25 to 40 percent and multiple genotypes within a serotype that vary by up to ~6% (Holmes and Twiddy, 2003; Rico-Hesse, 1990). At present, no approved antiviral treatment or vaccine is available, and therapy remains supportive.
The potential of passive immunotherapy for flavivirus infection has prompted the development and evaluation of several neutralizing human or humanized monoclonal antibodies (MAbs) against West Nile, Japanese encephalitis, and Dengue viruses (Balsitis et al., 2009; Beltramello et al., 2010; Goncalvez et al., 2008; Gould et al., 2005; Schieffelin et al., 2010; Sultana et al., 2009; Throsby et al., 2006). Recently, we described a panel of inhibitory DENV-1-specific MAbs, of which only four were highly protective in an IFNαβR−/− × IFNγR−/− AG129 mouse model of DENV-1 infection (Shrestha et al., 2010). One of these MAbs, DENV1-E106, strongly neutralized all five DENV-1 genotypes in cell culture and was active therapeutically even when administered as a single dose four days after infection in mice. Mapping studies by yeast display suggested that DENV1-E106 recognizes a composite epitope on the A-strand and lateral ridge of domain III (DIII) of the envelope (E) protein. As flaviviruses have an error-prone RNA polymerase, replication can result in rapid viral evolution. Thus, the potential for emergence of resistant variants is a significant concern for antibody-based therapeutics, especially for DENV, in which humans play a requisite role in the natural transmission cycle.
In this study, we selected for neutralization escape mutations of DENV1-E106. A single mutation in DIII of the E protein (T329A) was identified that conferred resistance to DENV1-E106. This T329A variant virus had differing phenotypes in vitro and in vivo with attenuation in cell culture yet paradoxically enhanced infectivity in mosquitoes. Moreover, mice infected with this T329A variant nonetheless were protected against lethality by DENV1-E106. This study reveals the complex dynamics of escape of a strongly neutralizing MAb against DENV in mice and mosquitoes.
RESULTS
Selection of a neutralization escape variant in cell culture
DENV1-E106 is a inhibitory sub-complex specific MAb that neutralized infection of strains corresponding to all five DENV-1 genotypes and improved clinical outcome in mice when administered as a single dose four days after infection with the West-Pac-74 (genotype 4) strain of DENV-1 (Shrestha et al., 2010). Given its broad-spectrum antiviral activity against all DENV-1 genotypes and possible therapeutic potential, we questioned whether resistance would occur under selective pressure during the course of treatment. Prior mapping studies identified putative recognition sites for DENV1-E106 MAb in the A-strand (K310) and lateral ridge of DIII (G328, T329, D330, P325, K361, E362, P364, and K385), as mutations in these residues reduced binding to DIII when expressed on the surface of yeast (Shrestha et al., 2010). To begin to identify key functional residues on DIII that engaged DENV1-E106, we selected for neutralization escape mutants in cell culture. We used DENV-1 West-Pac-74, a genotype 4 strain, since it was more resistant (12-fold, P < 0.01, Fig 1A) to DENV1-E106 compared to the genotype 2 strain 16007, and thus might be easier to recover escape variants. After three sequential passages of DENV-1 strain West-Pac-74 in BHK21-15 cells in the presence of 10 µg/ml of MAb, a resistant virus emerged that no longer was efficiently neutralized (EC50 of 7,860 ng/ml of escape variant versus 16 ng/ml of wild type, P = 0.005, Fig 1A); nonetheless, as high concentrations of MAb did inhibit infection, the escape mutant must still bind DENV1-E106, albeit with markedly reduced affinity.
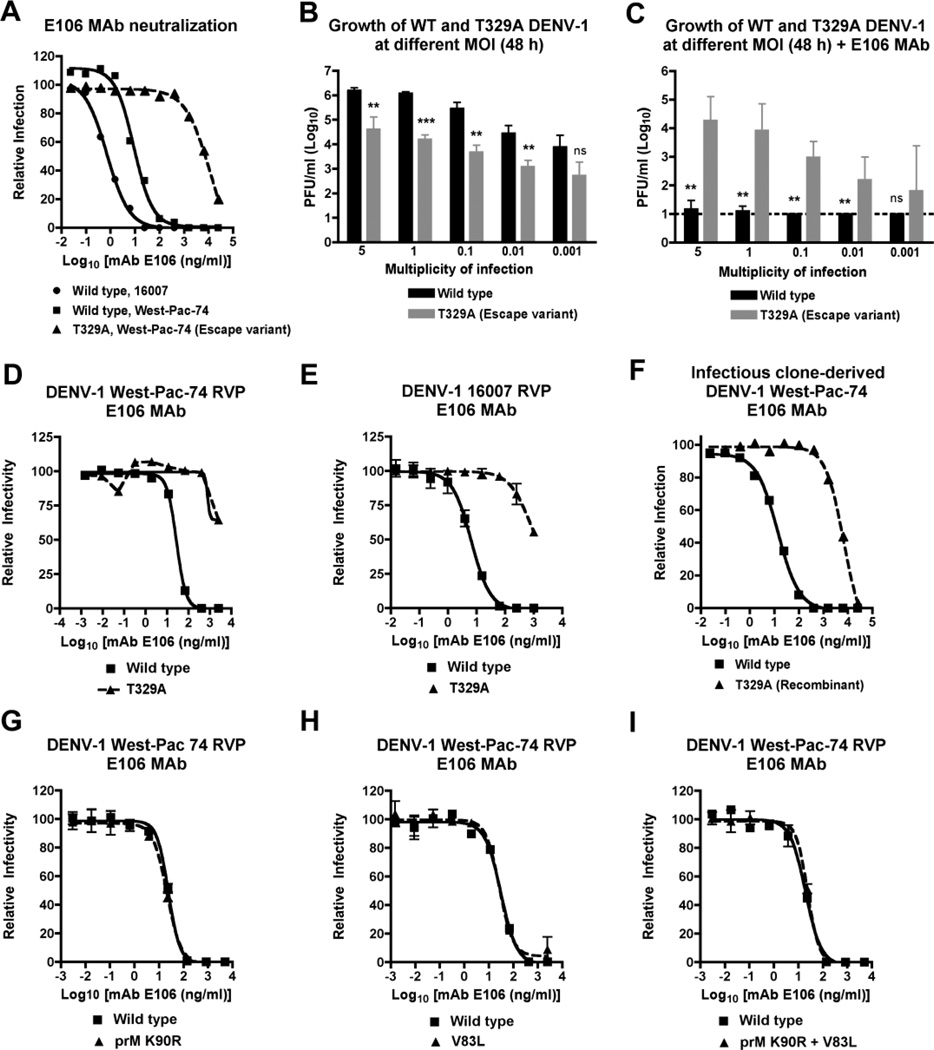
Figure 1. Phenotype of the DENV-1 T329A neutralization escape variant.
A. Neutralization curves with DENV1-E106 and the parent 16007 DENV-1 strain (genotype 2), the heterologous West-Pac-74 DENV-1 strain (genotype 4), and the T329A West-Pac-74 DENV-1 strain derived directly from passage in cell culture. The data are representative of three independent experiments performed in duplicate on BHK21-15 cells. B–C. Yield of wild type and T329A West-Pac-74 DENV-1 from supernatants of BHK21-15 cells after infection at different input MOI in the (B) absence or (C) presence of DENV1-E106. The data are the average of three independent experiments performed in duplicate and asterisks indicate differences that are statistically significant. Dashed lines indicate the limit of detection of the assay. D–E. Confirmation of resistant phenotype with wild type and mutant DENV-1 RVP. Genetically engineered DENV-1 RVP displaying the structural proteins of (D) West-Pac-74 or (E) 16007 with or without a single amino acid substitution (T329A) were incubated with increasing concentrations of DENV1-E106. F. Neutralization curves of DENV1-E106 with wild type or T329A West-Pac-74 DENV-1 strains derived by site-directed substitution into an infectious cDNA clone. The data are representative of two independent experiments performed in duplicate on BHK21-15 cells. G–I. Genetically engineered DENV-1 RVP (strain West-Pac-74) with single mutations (G) K90R in prM or (H) V83L in E or both mutations (I) K90R + V83L were incubated with increasing concentrations of DENV1-E106 and analyzed by flow cytometry. For D, E, and G–I, representative data of experiments performed on Raji-DCSIGNR cells is shown. Error bars represent the standard error of the mean of duplicate infections.
To determine the mutations that conferred the neutralization escape phenotype, viral RNA sequences were obtained from 30 independent plaque-purified escape variants and compared to the wild type DENV-1 sequence derived from virus propagated in parallel in the absence of MAb selection. All (30 of 30) escape variants contained only a single-nucleotide change (T to A) encoding a T329A mutation in the E protein, as no other changes were identified. To understand the significance of the T329A change, we assessed the growth kinetics of wild type and escape variant (T329A) viruses in the absence or presence of 10 µg/ml DENV1-E106 MAb in BHK21-15 cells. Notably, in the absence of antibody, T329A DENV-1 grew less well as evidenced by a reduced percentage of infected cells and lower (up to 70-fold, P < 0.001) viral titers at 48 hours over a broad range (0.01 to 5) of multiplicities of infection (MOI) (Fig 1B, and data not shown). However, in the presence of MAb, while virtually no virus was recovered in the supernatants of cells infected with wild type virus at 48 hours, T329A virus was obtained at several different MOI (Fig 1C). As additional confirmation, we generated a T329A mutant virus using two different reverse-genetic strategies. First, DENV-1 RVP (Ansarah-Sobrinho et al., 2008; Dowd et al., 2011) corresponding to West-Pac-74 or 16007 strains were engineered with or without a single amino acid mutation at T329A, produced in HEK293T cells, and analyzed for MAb neutralization. Whereas DENV1-E99 MAb (which maps to residues E309, K310, and E311 on the A-strand of DIII (Shrestha et al., 2010)) neutralized both wild-type and T329A RVP equivalently (data not shown), DENV1-E106 failed to efficiently neutralize the T329A mutant in either the West-Pac-74 or 16007 backgrounds (Fig 1D and E). As a final confirmation, we introduced the T329A substitution into an infectious cDNA clone of DENV-1 West-Pac-74 (Whitehead et al., 2003). As expected, the EC50 of the fully infectious T329A variant generated by reverse genetics showed similar resistance to DENV1-E106 MAb (Fig 1F) but retained sensitivity to neutralization by DENV1-E99 (data not shown). Overall, our results suggest that while the infectivity of wild type DENV-1 was strongly inhibited by DENV1-E106 MAb, similar viral titers were observed for the T329A escape variant in the presence or absence of antibody. However, the T329A mutant virus still was attenuated in BHK21-15 cells compared to wild type virus.
Stability of T329A DENV-1 variant in cell culture and mosquitoes
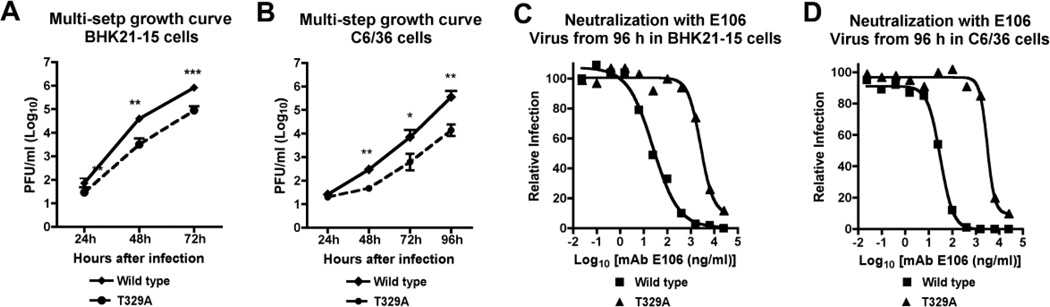
To further characterize the attenuated phenotype of the T329A DENV-1 variant in cell culture, we performed multi-step growth kinetics in mammalian (BHK21-15) and insect (C6/36) cells. Notably, in both cell types a 9 to 26-fold reduction in viral yield compared to wild type virus was observed after infection over a period of 72 to 96 hours (Fig 2A and B). To assess whether the T329A mutation was stable in BHK21-15 and C6/36 cells, virus was harvested from the supernatant of the respective cell types at the end of the time course and used for PRNT assays with DENV1-E106 MAb. No evidence of functional reversion was observed, as virus harvested from BHK21-15 or C6/36 cells infected with the T329A variant retained its resistant phenotype (Fig 2C and D). Consistent with this, sequencing of RNA from virus-containing supernatants at 96 hours revealed no reversion at amino acid position 329 of the E protein (data not shown).
Figure 2.
Growth analysis and stability of DENV-1 T329A neutralization escape variant. A–B. Multi-step growth curves of wild type or T329A West-Pac-74 DENV-1 in (A) BHK21-15 or (B) C6/36 cells. Cells were infected at an MOI of 0.01 and supernatants were harvested at 24-hour intervals for titration by plaque assay. The data are the average of three independent experiments performed in duplicate and asterisks indicate differences that are statistically significant. C–D. Supernatants were harvested at 96 hours from wild type or T329A DENV-1 infected (C) BHK21-15 or (D) C6/36 cells and used for PRNT analysis to assess stability of the escape mutation in cell culture. The data are representative of two independent experiments performed in duplicate on BHK21-15 cells.
Given the growth defect of T329A DENV-1 in C6/36 Aedes albopictus cells, we assessed its infectivity and stability in Aedes aegypti mosquitoes. Initially, we confirmed the presence of DENV-1 RNA in the midgut after blood meal infection with 3 × 106 PFU of wild type or T329A DENV-1 (West-Pac-74 strain) by harvesting at mosquitoes at one hour after feeding, homogenizing tissues, and analyzing viral RNA by RT-PCR; notably, no difference in initial infection with wild type or T329A DENV-1 was observed (Table 1, and data not shown). Remarkably, the T329A virus showed greater infectivity (22% for T329A and 0% for wild-type) of mosquitoes after a 14-day extrinsic incubation period. Sequencing of viral RNA recovered from the whole body of infected mosquitoes at 14 days post-infection revealed a low (7%) rate of reversion to wild type virus. Thus, the T329A DENV-1 neutralization escape variant efficiently infected the relevant arthropod vector and did not rapidly revert to the wild type sequence during a typical (14 day) period of replication in mosquitoes.
Table 1.
Infection and reversion of DENV-1 T329A in Aedes aegypti
| 0 to 1 hour post infection |
14 days post infection |
14 days post infection |
|
|---|---|---|---|
| Virus | Number positive (%) |
Number infected (%) |
Number revertants (%) |
| T329A | 10/10 (100) | 15/69 (22) | 1/15 (7) |
| Wild type | 10/10 (100) | 0/47 (0) | ND |
| P-value | NS | 0.0003 | ND |
Aedes aegypti mosquitoes were fed orally wild type (3.1 × 106 PFU/ml) or T329A (2.6 × 106 PFU/ml) DENV-1 in a 1:1 blood to virus ratio. Engorged mosquitoes were harvested immediately (within one hour) after feeding and screened for presence of DENV RNA or held for a 14-day extrinsic incubation period, after which bodies were harvested for viral RNA sequencing as described in the Methods. The results are pooled from independent experiments, and the proportions infected were compared by Fisher’s exact test. ND indicates not determined, as mosquitoes were not infected with the wild type parent DENV-1 West-Pac-74 strain under these conditions. NS indicates no significant difference.
Phenotype of T329A DENV-1 in mice
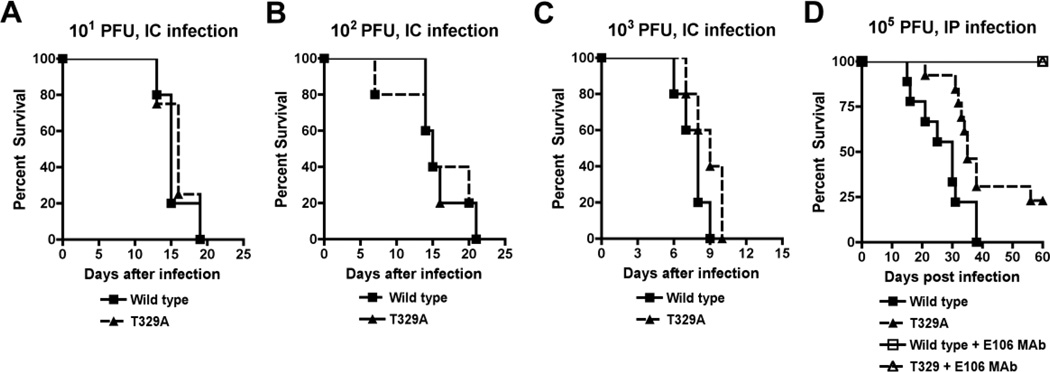
Given that the growth defect of T329A DENV-1 in C6/36 cells did not correlate with the phenotype in mosquitoes, we hypothesized that although it was attenuated in BHK21-15 cells, it nonetheless might still retain virulence in mice; this would suggest that replication dynamics in some tissue culture cell lines might not reliably predict phenotypes in animals. To test this, we performed a dose-response analysis using a stringent intracranial challenge model of DENV-1 West-Pac-74 in AG129 mice; this model was used because previously we had observed a dose-dependent change in the mean survival time of infected mice (Shrestha et al., 2010). Somewhat surprisingly, no difference in overall survival rate or average survival time was detected between wild type and T329A DENV-1 (West-Pac-74 strain) after intracranial infection with 101, 102, or 103 PFU of virus (Fig 3A, B, and C, P > 0.5). Because the intracranial challenge route bypasses infectivity requirements in peripheral organs, we also tested for attenuation after intraperitoneal challenge. Using a higher 105 PFU dose, which is required to achieve 100% lethality of the parent DENV-1 West-Pac-74 strain over the course of 3 to 5 weeks (Shrestha et al., 2010), we now observed mild attenuation of T329A DENV-1 (Fig 3D) as reflected by a decreased lethality rate (77% versus 100%, P < 0.02) and increased mean survival time (27.1 ± 2.8 versus 35.3 ± 2.8 days, P < 0.05).
Figure 3.
Phenotype of T329A DENV-1 in AG129 mice. A–C. AG129 mice were infected via an intracranial route with (A) 101, (B) 102, or (C) 103 PFU of wild type or T329A West-Pac-74 DENV-1 and followed for survival. The number of animals for each dose ranged from 5 to 6 per group. No differences were statistically significant. D. AG129 mice were untreated or pre-treated with 500 µg of DENV1-E106 prior to infection with wild type or T329A West-Pac-74 DENV-1. The number of animals for each antibody ranged from 10 to 18 per group. Statistically significant differences are described in the text.
Because of the shift of the survival curve, we speculated that in the absence of DENV1-E106 MAb pressure, within a few days, T329A DENV-1 might revert to the more virulent A329T parent virus. To evaluate this, we repeated the intraperitoneal challenge experiments with the wild type and T329A DENV-1 in the presence of 500 µg of DENV1-E106 that was administered one day prior to infection. As anticipated, the wild type DENV-1 showed no virulence in the presence of DENV1-E106 MAb. However, and somewhat unexpectedly, the T329A DENV-1 variant also showed no virulence when DENV1-E106 MAb was administered (Fig 3D), suggesting that either reversion of the escape virus occurred (and this revertant was blocked by DENV1-E106) or that the low-level of neutralizing activity of the DENV1-E106 MAb against the T329A virus (EC50 of 7,860 ng/ml, see Fig 1A) was sufficient to limit virulence in this model. To address this, we recovered infectious virus from the brains of moribund mice infected with T329A DENV-1 and obtained viral RNA sequences directly after RT-PCR amplification of viral RNA of brain homogenates or after plaque purification. Remarkably, all viral RNA sequences retained the T329A mutation in the E protein, with no other specific changes in the E protein identified. Consistent with this, 12 independent plaque-purified viruses from brain homogenates retained resistance to DENV1-E106 by plaque reduction neutralization assay (data not shown). Thus, although the T329A virus was attenuated and relatively resistant to DENV1-E106 MAb in mice, in vivo reversion did not occur frequently and DENV1-E106 MAb could still inhibit the virulence of the escape virus.
Selection of DENV1-E106 MAb escape virus in vivo
As the T329A DENV-1 cell culture derived escape variant retained sensitivity to DENV1-E106 MAb in vivo, we subsequently assessed the potential for emergence of resistant variants directly by recovering viruses from mice infected with wild type virus during MAb treatment. Ten AG129 mice were infected with 105 PFU of wild type DENV-1 West-Pac-74 and treated with a single 500 µg dose of DENV1-E106 MAb on day two post-infection. Whereas 8 of 10 mice showed complete protection with no evidence of clinical disease, two mice developed signs of infection by day 21 including lethargy and weight loss. Brain homogenates were recovered from these animals as well as control mice infected with wild type or T329A mutant DENV-1 West-Pac-74 in the absence of DENV1-E106 treatment. Viral RNA was obtained from plaque picks from brain homogenates corresponding to the mice receiving wild type virus + DENV1-E106 MAb, or receiving wild type or T329A mutant virus without MAb treatment, and the structural genes were sequenced in their entirety (Table 2). Notably, none of the plaque isolates from DENV1-E106-treated ill mice contained the T329A escape mutation. Instead, 22 of the 24 plaque picks isolated from mice receiving DENV1-E106 treatment had viral RNA sequences containing conservative mutations in prM (K90R) and DII of the E protein (V83L); despite the presence of these mutations, bulk brain tissue homogenates and all plaque isolates remained sensitive to neutralization by DENV1-E106, and substitution of the V83L, K90R, or V83L + K90R mutations into DENV-1 West-Pac RVP also failed to confer resistance (Fig 1G–I). Thus, while treatment failure with DENV1-E106 MAb was possible and resulted in mutation from the wild type virus, surprisingly, this was not associated with neutralization escape.
Table 2.
Virus mutations isolated from in vivo passage in AG129 mice.
| Wild type virus, No MAb |
T329A virus, No MAb |
Wild type virus DENV1-E106 MAb |
|
|---|---|---|---|
| K90R (prM) | 0/8a (0)b | 0/8 (0) | 22/24 (92) |
| V83L (Envelope) | 0/8 (0) | 0/8 (0) | 23/24 (96) |
| E202K (Envelope) | 4/8 (50) | 8/8 (100) | 12/24 (50) |
| T329A (Envelope) | 0/8 (0) | 8/8 (100) | 0/24 (0) |
indicates # isolates with mutation/total # of isolates
indicates the mutation frequency
AG129 mice were infected with 105 PFU of wild type DENV-1 West-Pac-74 or T329A mutant virus by an intraperitoneal route. Two days later, some of the mice receiving wild type viruses were administered a single 500 µg dose of DENV1-E106 by an intraperitoneal route. Brain homogenates were collected from all mice at 21 days and processed for viral RNA sequencing (see Methods).
DISCUSSION
Antibody-based therapy is currently being explored as a platform for pre- and/or post-exposure treatment of flavivirus infections (Diamond, 2009). For DENV in particular, theoretical concerns regarding exacerbation of acute disease and increasing the likelihood of DHF/DSS through the induction of antibody-dependent enhancement of infection (ADE) have been minimized by modification of sequences in the Fc region to eliminate binding to Fc-γ and complement receptors (Balsitis et al., 2010; Beltramello et al., 2010). Nonetheless, for DENV, where humans are an integral part of the natural cycle, the emergence of resistance and transmission of variants to mosquitoes could rapidly render costly therapeutic antibodies ineffective. To explore this question, we evaluated the potential for resistance of our most potently and broadly neutralizing MAb against DENV-1.
Although selection of neutralization escape variants in cell culture occurred, we recovered only one mutant (T329A) from 30 different plaque-purified viruses in the course of two independent experiments. Resistance can occur via selection of a preexisting mutant subpopulation or through the emergence of variant viruses during prolonged treatment (Margeridon-Thermet and Shafer, 2010). Given that a single mutation with the same nucleotide change was observed in all independent plaque variants, it seems likely that the T329A variant existed as a small subpopulation within the original viral stock. The T329A variant was attenuated in culture in BHK21-15 mammalian and C6/36 insect cells, with decreased replication in single- and multi-step growth analyses. Somewhat surprisingly, this attenuated phenotype was not observed in Aedes aegypti mosquitoes after feeding by blood meal; instead, and for reasons that remain unclear, the T329A variant showed a higher level of infectivity compared to the neutralization sensitive parent strain. We confirmed that feeding mosquitoes ingested the wild type and T329A mutant virus equivalently by harvesting tissues immediately after blood meal, and assaying viral RNA by RT-PCR. A related disparity between infectivity in C6/36 cells and Aedes aegypti mosquitoes was recently described with DENV-2 engineered with mutations in the adjacent FG loop (residues 382 to 385) on DIII (Erb et al., 2010); in that study, however, an opposing phenotype was described, as mutant DENV-2 replicated efficiently in insect cells but were compromised in mosquitoes fed blood meals or inoculated by intrathoracic injection. The low-level (in our case, 0%) infectivity rate with DENV-1 West-Pac-74 wild type virus after oral feeding of a blood meal has been reported previously in Aedes aegypti mosquitoes (Whitehead et al., 2003). The virus-host cell interactions that mediate midgut infection of Aedes aegypti by DENV remain poorly understood, and wide variation in infectivity has been observed among DENV serotypes (Gubler et al., 1979) and genotypes within a given serotype (Armstrong and Rico-Hesse, 2001, 2003). Since the T329A mutation was selected based on its ability to escape MAb neutralization and maps to a region of DIII that has been postulated to participate in virus attachment to host cells (Bhardwaj et al., 2001; Chu et al., 2005; Lee et al., 2006; Zhang et al., 2010), this residue could have functional significance in mediating midgut infection of mosquitoes. Although this particular observation was unexpected, it was reproducible, consistent with known variation in DENV strain infectivity of mosquitoes, and warrants further investigation.
The central finding derived from the mosquito experiments, however, is that in most insects the T329A mutation was not purified during the extrinsic phase of replication. Analogously, T329A DENV-1 showed no change in virulence after intracranial infection of mice and only a modest attenuation after intraperitoneal infection, without evidence of reversion. Thus, and somewhat surprisingly, analysis of attenuation of variant viruses in cell culture did not directly predict their behavior in insects or animals. In addition to understanding the significance of cell culture selected escape mutants of therapeutic antibodies, this finding may be relevant for characterization of live flavivirus vaccines that contain attenuating mutations, whose phenotype is initially selected based on altered replication in cell culture.
Prior experiments with WNV and the highly therapeutic MAb E16 identified an escape mutant (K307E) that was completely resistant to neutralization in vitro even at high MAb concentrations, and this correlated with a failure to protect in vivo after passive antibody transfer and infection with an in vitro-derived escape variant (Zhang et al., 2009). In comparison, even though the T329A variant was ~500-fold less sensitive to the neutralizing activity of DENV1-E106 MAb in cell culture and could cause lethal infection in AG129 mice in the absence of antibody without reversion, its pathogenesis still was inhibited when mice were pretreated with DENV1-E106 MAb. Although further study is warranted, this could reflect the residual neutralizing activity that DENV1-E106 MAb has for DENV-1 T329A (EC50 of ~8 µg/ml) or an enhanced protection that is conferred by the effector functions of the Fc region of antibodies. We also were unable to select for a bona fide escape mutation in vivo in the presence of DENV1-E106 MAb, even though treatment failure occurred; these results are analogous to studies with WNV E16 MAb in which escape mutants in vivo were not identified during the acute course of infection; rather sustained treatment over months was required before emergence of an escape variant was observed (Zhang et al., 2009). Binding of the complement component C1q can reduce the stoichiometric threshold for antibody-mediated neutralization and improve the potency of antibodies 5 to 20-fold, depending on the isotype (Mehlhop et al., 2009), and activating Fc-γ receptors can enhance protection against flaviviruses in vivo (Chung et al., 2006; Chung et al., 2007; Oliphant et al., 2005; Schlesinger et al., 1993; Vogt et al., 2011) through enhanced phagocytosis or antibody-dependent cellular cytotoxicity. Future testing of agylcosyl variants of DENV1-E106 MAb that lack the ability to bind C1q or Fc-γ receptors (Tao and Morrison, 1989) with wild type and T329A West-Pac-74 viruses will help to define whether antibody effector functions explains the residual protective activity in vivo against the T329A escape variant and the failure to select treatment-resistant variants.
In summary, whereas a single neutralization escape variant was selected rapidly in cell culture, distinct phenotypes with this virus were observed in vivo in mosquitoes and mice. Emergence of resistant variants could occur with single MAb therapeutics against DENV during an epidemic if introduction into the mosquito vector does not purify the mutation. Alternatively, the use of combinations of neutralizing MAbs that recognize distinct epitopes could limit the rapid development of resistance.
MATERIALS AND METHODS
Cells, virus and mice
The Dengue virus type-1 strain (West-Pac-74, genotype 4) was obtained from Dr. Stephen Whitehead (NIAID, NIH, Bethesda, MD) and amplified in C6/36 Aedes albopictus cells according to previously described protocols (Shrestha et al., 2010). BHK21-15 cells were cultured in Dulbecco's Modified Eagle Medium (DMEM) supplemented with 10% fetal bovine serum (FBS) (Omega Scientific) and antibiotics (penicillin G and streptomycin) at 37°C in a humidified 5% CO2 incubator. BHK21-15 cells were used to determine DENV-1 West-Pac-74 stock titer by standard plaque assay (Shrestha et al., 2010). IFNαβR−/− × IFNγR−/− mice on the 129 Sv background (AG129 mice) were a gift from Dr. Skip Virgin (Washington University School of Medicine) and bred in a pathogen-free barrier facility. All mouse studies were carried out in strict accordance with the recommendations in the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health. The protocol was approved by the Institutional Animal Care and Use Committee at the Washington University School of Medicine (Assurance Number: A3381-01).
Selection of the T329A neutralization escape mutant in cell culture
To select a variant that escaped neutralization by DENV1-E106 MAb, the genotype 4 DENV-1 strain West-Pac-74 (4 × 105 PFU) was incubated with 10 µg/ml of DENV1-E106 for one hour at room temperature in DMEM supplemented with 10% FBS. The mixture was added to BHK21-15 cells in a six-well plate and incubated for two hours at 37°C. Wells were washed three times, fresh DMEM medium containing 10 µg/ml of DENV1-E106 MAb was added, and cells were incubated at 37°C for 96 hours. Supernatant was harvested, mixed with 20 µg/ml of fresh DENV1-E106 mAb, and the selection process was repeated for two additional passages. After the third passage under MAb selection, supernatants were titrated for resistant viruses by performing a plaque reduction neutralization test (PRNT)50 assay in BHK21-15 cells in the presence of DENV1-E106 MAb. After confirmation of an escape phenotype, plaques formed under DENV1-E106 MAb selection were visualized using a neutral red overlay. Plaque-purified virus was recovered, amplified under MAb selection (10 µg/ml) in BHK21-15 cells for three days at 37°C, and supernatants were stored aliquotted at −80°C. Infected BHK21-15 cells were trypsinized from wells, washed, and total cellular RNA was isolated using an RNeasy kit (Qiagen). The E gene was amplified by reverse-transcription of the viral RNA and cDNA synthesis using the Superscript III One-Step RT-PCR System (Invitrogen) with the following DENV-1 forward and reverse primers: 840F: 5'-TGCCATAGGAACATCCATCA-3' or 850F: 5'-ACATCCATCACCCAGAAAGG-3'; 1436F: 5'-TGACCGACTACGGAGCTCTT-3'; 1655R: 3'-TGCTTCTTTGCATGAGCTGT-5'; 2416R: 3'-TGACAAAAATGCCACTTCCA-5', and 2519R: 3'-CTCTTTGGGGAGTCAGCTTG-5'. Direct sequencing of the gel-purified PCR products was compared to the sequence of the laboratory stock DENV-1 West-Pac-74 strain that was passaged and plaque-purified in parallel in the absence of MAb selection.
In vivo selection of escape mutant
In an attempt to generate a neutralization escape virus in vivo, AG129 mice were infected with 105 PFU of wild type DENV-1 West-Pac-74 by an intraperitoneal route. Two days later, mice were administered a single dose of 500 µg of DENV1-E106 by an intraperitoneal route and monitored for morbidity for 60 days. Ill-appearing mice were euthanized, and brain tissues were divided for virus titration in the presence or absence of DENV1-E106 and extraction of total RNA. To isolate potential escape mutants, virus from brain homogenates was plaque purified as described previously (Sukupolvi-Petty et al., 2010). Viral RNA was extracted from brain tissue by using an RNeasy mini kit (Qiagen) and sequenced as described above along with an additional forward primer in the capsid gene: 69F: 5’AGGGTCGACCGTCTTTCAAT-3’ to obtain complete structural gene sequences. Viral RNA was extracted from viral supernatants of plaque-purified isolates using the QIAamp Viral RNA kit (Qiagen) and sequenced.
DENV-1 infectious cDNA clone and mutant generation
The DENV-1 West-Pac-74 infectious cDNA clone pRS424DEN1WP (Puri et al., 2000; Whitehead et al., 2003) (gift of S. Whitehead, Bethesda. MD) was used to create wild type and mutant infectious DENV-1. The T329A single amino acid substitution was introduced into pRS424DEN1WP by site directed mutagenesis. Wild type and mutant plasmids were grown in competent BD1528 bacteria at room temperature and recovered using standard molecular biology techniques. Plasmids were linearized, treated with proteinase K, extracted twice with phenol and chloroform, and precipitated with ethanol at −20°C overnight. DNA was used as a template for in vitro DNA-dependent RNA transcription with the AmpliScribe T7 kit (Epicentre) with the addition of m7G(5')ppp(5')A cap analog (New England BioLabs). Transcription reactions were run at 37°C for 5 hours and the reaction was then electroporated (3 pulses at 850V, 25µF, ∞Ω) into BHK21-15 cells. Cells were added to a T75 tissue culture flask in DMEM with 10% FBS and observed for the onset of cytopathic effects (CPE). Once CPE were observed, virus-containing supernatant was collected, cellular debris pelleted, and supernatant aliquots frozen at −80°C. The cells remaining in the T75 flask were harvested and used as a source of viral RNA to confirm that the desired sequence was retained.
DENV-1 neutralization assay with reporter virus particles
DENV-1 reporter virus particles (RVP) are pseudo-infectious virions produced by genetic complementation of a WNV sub-genomic replicon with the DENV structural genes in trans. Wild type and mutant (T329A (E gene), K90R (prM gene), and V83L (E gene)) DENV-1 RVP were generated as described previously (Ansarah-Sobrinho et al., 2008; Dowd et al., 2011); a plasmid expressing the wild type or mutant C-prM-E genes of DENV-1 (strains West-Pac-74 or 16007) was cotransfected into 293T cells with a plasmid encoding a WNV replicon expressing GFP. The C-prM-E plasmid of DENV-1 West-Pac-74 or 16007 was mutated using the QuikChange site directed mutagenesis kit (Stratagene) to introduce amino acid substitutions. Supernatants containing RVP were harvested 72 hours after transfection, filtered through a 0.2 µm filter, and stored aliquotted at −80°C. RVP were incubated with serial dilutions of MAb under conditions of antibody excess at 37°C for one hour. Subsequently, MAb-RVP mixtures were added to Raji-DCSIGNR cells, which stably express the DC-SIGNR attachment factor (Davis et al., 2006), and were incubated at 37°C for 48 hours. Infected cells were assayed for GFP expression using a FACSCalibur flow cytometer (Becton Dickinson).
Phenotype of neutralization escape mutant viruses
(a) Cell culture. The neutralizing activity of DENV1-E106 was determined by using a plaque reduction neutralization test in BHK21-15 cells as described previously (Shrestha et al., 2010). Additionally, single- and multi-step growth curve analysis was performed in BHK21-15 or C6/36 cells with wild type and mutant DENV-1 at different MOI (5, 1, 0.1, 0.01, or 0.001) in the presence or absence of 25 µg/ml DENV1-E106 MAb. Two hours later, free virus was removed and cells were grown in the presence or absence of 25 µg/ml DENV1-E106 MAb at 37°C. Two days later, supernatants were harvested, and virus production was determined by plaque assay in BHK21-15 cells. (b) Mice. To determine the virulence of T329A escape viruses, AG129 mice were infected with wild type or mutant virus at 101, 102 or 103 PFU by intracranial infection or 105 PFU by intraperitoneal infection. Mice were monitored for morbidity and mortality for 60 days. Brain tissues were harvested when mice were moribund and stored at −80°C. To assess whether DENV1-E106 MAb could protect mice after infection with the T329A escape virus, AG129 mice were administered single dose of 500 µg/mouse antibody one day before intraperitoneal infection with 105 PFU of wild type and mutant virus.
Mosquito infection
Aedes aegypti mosquitoes (Rexville D strain) were provided by Dr. Ken Olson (Colorado State University) and reared according to standard procedures. Adult females were fed a mixture of defibrinated goose blood and either wild type or T329A DENV-1 in a 1:1 blood:virus ratio. ATP was added to the bloodmeal at a final concentration of 2 mM. Undiluted titers of the wild type and mutant viruses were 3.1 × 106 PFU/ml and 2.6 × 106 PFU/ml, respectively. After feeding, mosquitoes were anesthetized, and engorged females separated into cartons and held for a 14-day extrinsic incubation period (EIP) at 28°C, 70 to 80% relative humidity, and a 16:8 photoperiod. In separate experiments, mosquitoes were fed a blood meal using the same virus stocks, and harvested within one hour of feeding.
Viral RNA sequencing from mosquitoes
Whole mosquito bodies were collected, homogenized in RLT lysis buffer, and RNA was extracted using RNeasy kits (Qiagen, Valencia CA). Samples were screened for DENV-1 infection using a OneStep RT-PCR Kit (Qiagen, Valencia CA) and primers that amplified a 500 nucleotide region in domain III of the envelope (E) gene (1546F: 5’-ATCATGGCTCGTCCACAAAC-3’ and 2045R: 5’-GCTCCGCTTCAATGTTGACT-3’). This region contains the single nucleotide polymorphism that differentiates the wild type and mutant viruses. RT-PCR reactions from positive mosquitoes were purified using either QIAquick PCR purification kits (Qiagen, Valencia CA) or StrataPrep PCR purification kits (Stratagene, La Jolla CA). Amplicons were sequenced using a primer annealing 149 bases upstream (1771F: 5’-TGCAGGACACCTGAAATGCAG-3’) of the single nucleotide polymorphism (Genewiz, South Plainsfield NJ). Sequence chromatograms were analyzed to assess reversion to the wild type sequence using the PERL script PolySNP (Hall and Little, 2007).
Statistical analysis
All data were analyzed using Prism software (GraphPad software). For survival analysis, Kaplan-Meier survival curves were analyzed by log-rank test. For growth kinetics and neutralizing titers an unpaired T-test or analysis of variance was used to determine significance.
HIGHLIGHTS.
A single mutation confers neutralization escape against a therapeutic anti-DENV MAb
Replication of escape mutant virus in cell culture did not predict activity in vivo
Escape mutant virus was not purified in Aedes aegypti vector
Mice treated with MAb and infected with escape mutant virus were still protected
ACKNOWLEDGEMENTS
The authors thank R. Rico-Hesse, A. de Silva, and R. Tesh for providing DENV-1 strains, S. Whitehead for the infectious cDNA clone of West-Pac-74 and the BD1528 bacteria, and J. Roehrig for critical comments on the manuscript. This work was supported by the Burroughs Wellcome Fund, the intramural program of NIAID, and NIH grants R01-AI077955, U01-AI061373, and U54 AI057160 (Midwest Regional Center of Excellence for Biodefense and Emerging Infectious Diseases Research).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Ansarah-Sobrinho C, Nelson S, Jost CA, Whitehead SS, Pierson TC. Temperature-dependent production of pseudoinfectious dengue reporter virus particles by complementation. Virology. 2008;381:67–74. doi: 10.1016/j.virol.2008.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong PM, Rico-Hesse R. Differential susceptibility of Aedes aegypti to infection by the American and Southeast Asian genotypes of dengue type 2 virus. Vector Borne Zoonotic Dis. 2001;1:159–168. doi: 10.1089/153036601316977769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong PM, Rico-Hesse R. Efficiency of dengue serotype 2 virus strains to infect and disseminate in Aedes aegypti. Am J Trop Med Hyg. 2003;68:539–544. doi: 10.4269/ajtmh.2003.68.539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balsitis SJ, Coloma J, Castro G, Alava A, Flores D, McKerrow JH, Beatty PR, Harris E. Tropism of dengue virus in mice and humans defined by viral nonstructural protein 3-specific immunostaining. Am J Trop Med Hyg. 2009;80:416–424. [PubMed] [Google Scholar]
- Balsitis SJ, Williams KL, Lachica R, Flores D, Kyle JL, Mehlhop E, Johnson S, Diamond MS, Beatty PR, Harris E. Lethal antibody enhancement of dengue disease in mice is prevented by Fc modification. PLoS Pathog. 2010 doi: 10.1371/journal.ppat.1000790. e1000790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beltramello M, Williams KL, Simmons CP, Macagno A, Simonelli L, Quyen NT, Sukupolvi-Petty S, Navarro-Sanchez E, Young PR, de Silva AM, Rey FA, Varani L, Whitehead SS, Diamond MS, Harris E, Lanzavecchia A, Sallusto F. The human immune response to Dengue virus is dominated by highly cross-reactive antibodies endowed with neutralizing and enhancing activity. Cell Host Microbe. 2010;8:271–283. doi: 10.1016/j.chom.2010.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhardwaj S, Holbrook M, Shope RE, Barrett AD, Watowich SJ. Biophysical characterization and vector-specific antagonist activity of domain III of the tick-borne flavivirus envelope protein. J Virol. 2001;75:4002–4007. doi: 10.1128/JVI.75.8.4002-4007.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu JJ, Rajamanonmani R, Li J, Bhuvanakantham R, Lescar J, Ng ML. Inhibition of West Nile virus entry by using a recombinant domain III from the envelope glycoprotein. J Gen Virol. 2005;86:405–412. doi: 10.1099/vir.0.80411-0. [DOI] [PubMed] [Google Scholar]
- Chung KM, Nybakken GE, Thompson BS, Engle MJ, Marri A, Fremont DH, Diamond MS. Antibodies against West Nile virus non-structural (NS)-1 protein prevent lethal infection through Fc gamma receptor-dependent and independent mechanisms. J Virol. 2006;80:1340–1351. doi: 10.1128/JVI.80.3.1340-1351.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung KM, Thompson BS, Fremont DH, Diamond MS. Antibody recognition of cell surface-associated NS1 triggers Fc-g receptor mediated phagocytosis and clearance of WNV infected cells. J Virol. 2007;81:9551–9555. doi: 10.1128/JVI.00879-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis CW, Nguyen HY, Hanna SL, Sanchez MD, Doms RW, Pierson TC. West Nile virus discriminates between DC-SIGN and DC-SIGNR for cellular attachment and infection. J Virol. 2006;80:1290–1301. doi: 10.1128/JVI.80.3.1290-1301.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diamond MS. Progress on the development of therapeutics against West Nile virus. Antiviral Res. 2009;83:214–227. doi: 10.1016/j.antiviral.2009.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowd KA, Jost CA, Durbin AP, Whitehead SS, Pierson TC. A dynamic landscape for antibody binding modulates antibody-mediated neutralization of West Nile virus. PLoS Pathog. 2011;7 doi: 10.1371/journal.ppat.1002111. e1002111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erb SM, Butrapet S, Moss KJ, Luy BE, Childers T, Calvert AE, Silengo SJ, Roehrig JT, Huang CY, Blair CD. Domain-III FG loop of the dengue virus type 2 envelope protein is important for infection of mammalian cells and Aedes aegypti mosquitoes. Virology. 2010;406:328–335. doi: 10.1016/j.virol.2010.07.024. [DOI] [PubMed] [Google Scholar]
- Goncalvez AP, Chien CH, Tubthong K, Gorshkova I, Roll C, Donau O, Schuck P, Yoksan S, Wang SD, Purcell RH, Lai CJ. Humanized monoclonal antibodies derived from chimpanzee Fabs protect against Japanese encephalitis virus in vitro and in vivo. J Virol. 2008;82:7009–7021. doi: 10.1128/JVI.00291-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gould LH, Sui J, Foellmer H, Oliphant T, Wang T, Ledizet M, Murakami A, Noonan K, Lambeth C, Kar K, Anderson JF, de Silva AM, Diamond MS, Koski RA, Marasco WA, Fikrig E. Protective and therapeutic capacity of human single chain Fv-Fc fusion proteins against West Nile virus. J Virol. 2005;79:14606–14613. doi: 10.1128/JVI.79.23.14606-14613.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gubler DJ, Nalim S, Tan R, Saipan H, Sulianti Saroso J. Variation in susceptibility to oral infection with dengue viruses among geographic strains of Aedes aegypti. Am J Trop Med Hyg. 1979;28:1045–1052. doi: 10.4269/ajtmh.1979.28.1045. [DOI] [PubMed] [Google Scholar]
- Hall GS, Little DP. Relative quantitation of virus population size in mixed genotype infections using sequencing chromatograms. J Virol Methods. 2007;146:22–28. doi: 10.1016/j.jviromet.2007.05.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halstead SB. Pathogenesis of dengue: challenges to molecular biology. Science. 1988;239:476–481. doi: 10.1126/science.3277268. [DOI] [PubMed] [Google Scholar]
- Holmes EC, Twiddy SS. The origin, emergence and evolutionary genetics of dengue virus. Infect Genet Evol. 2003;3:19–28. doi: 10.1016/s1567-1348(03)00004-2. [DOI] [PubMed] [Google Scholar]
- Lee JW, Chu JJ, Ng ML. Quantifying the specific binding between West Nile virus envelope domain III protein and the cellular receptor alphaVbeta3 integrin. J Biol Chem. 2006;281:1352–1360. doi: 10.1074/jbc.M506614200. [DOI] [PubMed] [Google Scholar]
- Margeridon-Thermet S, Shafer RW. Comparison of the Mechanisms of Drug Resistance among HIV, Hepatitis B, Hepatitis C. Viruses. 2010;2:2696–2739. doi: 10.3390/v2122696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehlhop E, Nelson S, Jost CA, Gorlatov S, Johnson S, Fremont DH, Diamond MS, Pierson TC. Complement protein C1q reduces the stoichiometric threshold for antibody-mediated neutralization of West Nile virus. Cell Host Microbe. 2009;6:381–391. doi: 10.1016/j.chom.2009.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monath TP. Dengue: the risk to developed and developing countries. Proc Natl Acad Sci U S A. 1994;91:2395–2400. doi: 10.1073/pnas.91.7.2395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliphant T, Engle M, Nybakken G, Doane C, Johnson S, Huang L, Gorlatov S, Mehlhop E, Marri A, Chung KM, Ebel GD, Kramer LD, Fremont DH, Diamond MS. Development of a humanized monoclonal antibody with therapeutic potential against West Nile virus. Nature Medicine. 2005;11:522–530. doi: 10.1038/nm1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puri B, Polo S, Hayes CG, Falgout B. Construction of a full length infectious clone for dengue-1 virus Western Pacific,74 strain. Virus Genes. 2000;20:57–63. doi: 10.1023/a:1008160123754. [DOI] [PubMed] [Google Scholar]
- Rico-Hesse R. Molecular evolution and distribution of dengue viruses type 1 and 2 in nature. Virology. 1990;174:479–493. doi: 10.1016/0042-6822(90)90102-w. [DOI] [PubMed] [Google Scholar]
- Schieffelin JS, Costin JM, Nicholson CO, Orgeron NM, Fontaine KA, Isern S, Michael SF, Robinson JE. Neutralizing and non-neutralizing monoclonal antibodies against dengue virus E protein derived from a naturally infected patient. Virol J. 2010;7:28. doi: 10.1186/1743-422X-7-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlesinger JJ, Foltzer M, Chapman S. The Fc portion of antibody to yellow fever virus NS1 is a determinant of protection against YF encephalitis in mice. Virology. 1993;192:132–141. doi: 10.1006/viro.1993.1015. [DOI] [PubMed] [Google Scholar]
- Shrestha B, Brien JD, Sukupolvi-Petty S, Austin SK, Edeling MA, Kim T, O'Brien KM, Nelson CA, Johnson S, Fremont DH, Diamond MS. The Development of Therapeutic Antibodies that Neutralize Homologous and Heterologous Genotypes of Dengue Virus Type 1. PLoS Pathog. 2010;6 doi: 10.1371/journal.ppat.1000823. e1000823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sukupolvi-Petty S, Austin SK, Engle M, Brien JD, Dowd KA, Williams KL, Johnson S, Rico-Hesse R, Harris E, Pierson TC, Fremont DH, Diamond MS. Structure and Function Analysis of Therapeutic Monoclonal Antibodies against Dengue Virus Type 2. J Virol. 2010;84:9227–9239. doi: 10.1128/JVI.01087-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sultana H, Foellmer HG, Neelakanta G, Oliphant T, Engle M, Ledizet M, Krishnan MN, Bonafe N, Anthony KG, Marasco WA, Kaplan P, Montgomery RR, Diamond MS, Koski RA, Fikrig E. Fusion loop peptide of the West Nile virus envelope protein is essential for pathogenesis and is recognized by a therapeutic cross-reactive human monoclonal antibody. J Immunol. 2009;183:650–660. doi: 10.4049/jimmunol.0900093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tao MH, Morrison SL. Studies of aglycosylated chimeric mouse-human IgG. Role of carbohydrate in the structure and effector functions mediated by the human IgG constant region. J Immunol. 1989;143:2595–2601. [PubMed] [Google Scholar]
- Throsby M, Geuijen C, Goudsmit J, Bakker AQ, Korimbocus J, Kramer RA, Clijsters-van der Horst M, de Jong M, Jongeneelen M, Thijsse S, Smit R, Visser TJ, Bijl N, Marissen WE, Loeb M, Kelvin DJ, Preiser W, ter Meulen J, de Kruif J. Isolation and characterization of human monoclonal antibodies from individuals infected with West Nile Virus. J Virol. 2006;80:6982–6992. doi: 10.1128/JVI.00551-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogt MR, Dowd KA, Engle M, Tesh RB, Johnson S, Pierson TC, Diamond MS. Poorly neutralizing cross-reactive antibodies against the fusion loop of West Nile virus envelope protein protect in vivo via Fc-{gamma} receptor and complement-dependent effector mechanisms. J Virol. 2011;22:11567–11580. doi: 10.1128/JVI.05859-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitehead SS, Falgout B, Hanley KA, Blaney JE, Jr, Markoff L, Murphy BR. A live, attenuated dengue virus type 1 vaccine candidate with a 30-nucleotide deletion in the 3' untranslated region is highly attenuated and immunogenic in monkeys. J Virol. 2003;77:1653–1657. doi: 10.1128/JVI.77.2.1653-1657.2003. Jr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang S, Bovshik EI, Maillard R, Gromowski GD, Volk DE, Schein CH, Huang CY, Gorenstein DG, Lee JC, Barrett AD, Beasley DW. Role of BC loop residues in structure, function and antigenicity of the West Nile virus envelope protein receptor-binding domain III. Virology. 2010;403:85–91. doi: 10.1016/j.virol.2010.03.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang S, Vogt MR, Oliphant T, Engle M, Bovshik EI, Diamond MS, Beasley DW. The development of resistance to passive therapy by a potently neutralizing humanized West Nile virus monoclonal antibody. J Infect Dis. 2009;200:202–205. doi: 10.1086/599794. [DOI] [PMC free article] [PubMed] [Google Scholar]