Abstract
Previous research has found concurrent and prospective associations between negative mood and body dissatisfaction; however, only experimental research can establish causal relationships. This study utilized an experimental design to examine the influence of negative mood on body dissatisfaction. Undergraduate women were randomly assigned to an experimental or control condition. Participants in the experimental condition (n = 21) completed a negative mood induction procedure. Participants in the control condition (n = 24) completed a neutral mood procedure. All participants completed visual analogue scales regarding their mood and satisfaction with weight and shape before and after each manipulation. Body dissatisfaction increased following the procedure for experimental but not control participants, suggesting that negative mood caused increased body dissatisfaction. In cultures that idealize thinness, body dissatisfaction may arise from funneling general feelings of dysphoria into more concrete and culturally meaningful negative feelings about the body.
Keywords: body image, experiment, negative affect, undergraduate women
Negative affect is a prospective risk factor for the development of eating disorders (Stice, 2002). Further, acute increases in negative affect appear to be a trigger for binge eating among women with bulimia nervosa and binge eating disorder (Haedt-Matt & Keel, 2011). Thus, negative mood has both distal and proximal significance in disordered eating. Similarly, body dissatisfaction predicts the development of a variety of negative consequences, particularly eating pathology (Johnson & Wardle, 2005; Stice, 2002). However, little is known about the causal relationship between these two risk factors. The purpose of this study was to examine the influence of negative mood on body dissatisfaction.
Body dissatisfaction and negative mood consistently show positive associations in clinical (e.g., Dunkley, Masheb, & Grilo, 2010) and non-clinical samples of women (e.g., Johnson & Wardle, 2005; Santos, Richards, & Bleckley, 2007). Although a large body of research suggests that body dissatisfaction contributes to negative mood, depression also has been supported as a prospective risk and maintenance factor for body dissatisfaction in longitudinal studies (Bearman, Presnell, Martinez, & Stice, 2006; Keel, Mitchell, Davis, & Crow, 2001). Thus, some researchers have proposed a model in which negative mood increases body dissatisfaction (Griffiths & McCabe, 2000; Keel et al., 2001; Tylka & Subich, 2004). Keel and colleagues (2001) theorized that depression may cause body dissatisfaction because general negative feelings are funneled into negative feelings about body shape and weight in cultures that idealize thinness. Expanding on earlier theoretical models, Tylka and Subich (2004) posited that negative affect contributes to body image disturbance because women who experience negative affect are more likely to internalize the thin ideal and generalize negative feelings toward their bodies. Supporting these proposals, research has found that negative affect and self-esteem are unique predictors of variance in body image (Griffiths & McCabe, 2000; Tylka & Subich, 2004). If negative mood increases body dissatisfaction, we would expect changes in negative mood to precede changes in body dissatisfaction. However, correlational and longitudinal findings cannot establish whether acute changes in mood cause acute changes in body dissatisfaction.
Previous research has used experimental methods to successfully manipulate mood and body satisfaction in non-clinical samples of women. Negative mood inductions led to increases in body dissatisfaction in some (Baker, Williamson, & Sylve, 1995; Cohen-Tovée, 1993; M. J. Taylor & Cooper, 1992) but not all studies (Carter, Bulik, Lawson, Sullivan, & Wilson, 1996). Conflicting results may be due to limitations of this literature, including small sample size (N = 15; Carter et al., 1996), no control condition for comparison (Cohen-Tovée, 1993), and lack of an immediate pre-induction assessment of mood and body dissatisfaction (Baker et al., 1995). Thus, methodological limitations constrain the conclusions that can be drawn from existing experimental studies. The present study sought to examine causal relationships between mood and body dissatisfaction in a non-clinical sample utilizing a controlled experimental design with repeated assessments to evaluate changes in mood and body dissatisfaction as a consequence of negative mood induction procedures. We hypothesized that experimentally-induced increases in negative mood would cause increases in body dissatisfaction.
Method
Participants
Participants were 45 female undergraduates recruited through campus advertisements. Eligible participants were between 18 and 25 years old, had a body mass index (BMI) in the normal range (19 – 24 kg/m2), and reported no prior or current eating disorder during a screening interview that covered lifetime history of eating disorder symptoms. Mean (SD) age and BMI were 20.03 (1.78) years and 21.68 (1.71) kg/m2, respectively. The sample was predominantly Caucasian (90.5%). Participants were paid $10 for their participation. This research was reviewed and approved by an institutional review board.
Measures
Participants completed demographic and self-report questionnaires on a separate day as part of a larger study examining factors that influence body image. Measures included global ratings of depression, body dissatisfaction, and eating pathology and were completed within one week of their participation in the current study. In addition, participants completed assessments of their current mood, body shape satisfaction, and weight satisfaction immediately before and after experimental procedures using three visual analogue scales.
Beck Depression Inventory (BDI)
This 21-item scale is a widely-used measure of depressive symptoms (Beck, Ward, Mendelson, Mock, & Erbaugh, 1961). Cronbach’s alpha in this study was .92.
Eating Attitudes Test-26 (EAT-26)
This 26-item measure assesses features commonly present in individuals with anorexia nervosa (Garner, Olmsted, Bohr, & Garfinkel, 1982). Using a scale that ranges from 1 (never) to 6 (always), participants rate how often they engage in certain thoughts and behaviors such as, “I like my stomach to be empty” and “I am terrified about being overweight.” Although Garner and colleagues (1982) recommended recoding items into a 0–3 rating system, item values in the current study were summed using a continuous 1–6 rating system to counter lower variability in a non-clinical sample. Cronbach’s alpha for the current sample was .92.
Body Dissatisfaction subscale of the EDI (EDI-BD)
This 9-item scale measures the belief that certain body parts are too large (Garner, Olmstead, & Polivy, 1983). Because of greater sensitivity in a nonclinical population, original item values ranging from 1 to 6 (rather than recoded items) were summed to calculate a score on this measure. Cronbach’s alpha for the current sample was .92.
Bulimia Test-Revised (BULIT-R)
This 36-item scale assesses bulimic symptoms. The BULIT-R has demonstrated good predictive ability for bulimia nervosa (Thelen, Farmer, Wonderlich, & Smith, 1991). Cronbach’s alpha for the current sample was .96.
Visual Analogue Scales (VAS)
Participants’ current mood, body shape satisfaction, and weight satisfaction were evaluated immediately before and after the experimental/control procedure using three VAS. To assess mood, participants were asked, “How are you feeling right now?” with response anchors of “Extremely Unhappy” on the left end versus “Extremely Happy” on the right end. To assess weight and body shape satisfaction, participants were asked, “How do you feel about your weight right now?” and “How do you feel about your body shape right now?” with response anchors of “Extremely Unsatisfied” at the left end and “Extremely Satisfied” at the right end. These horizontal scales were 100 millimeters long, and participants were instructed to make one vertical mark on each line to indicate their current state. Scores were calculated by measuring the distance in millimeters from the left end of the scale to the participant’s mark. Changes in VAS scores were used to evaluate changes in mood, body shape satisfaction, and weight satisfaction. VAS scores measuring satisfaction with body weight and appearance have correlated highly with the EDI-BD, demonstrating good construct validity (Heinberg & Thompson, 1995).
Procedure
Participants were told that the purpose of this study was to investigate body image. After providing informed consent, participants were randomly assigned by a coin toss into either the experimental (n = 21) or control condition (n = 24).
Similar to methods successfully implemented by Cohen-Tovée (1993), the current study used Clark’s (1983) musical mood induction method to induce a temporary increase in negative affect in the experimental group and no mood change in the control group. After completing the pre-induction VAS, participants in the experimental group received the following written instructions: “Please try to get into a sad mood. Both the statements on the cards and the music are designed to help you get into that mood. Read the statements to yourself and try to think that they are true for you.” Participants then listened to an excerpt from Gabriel Faur Fauré’s “Requiem” (Op. 48, part one, “Introit et Kyrie”) while viewing ten printed self-statements with negative connotations, such as “I have been dishonest” and “I do not have any true friends.” Importantly, none of the negative self-statements were related to body shape or weight.
Participants in the control group completed the pre-induction VAS and then received the following written instructions: “Please read the following statements and think about a time when you’ve observed or experienced the events described in the statements.” Control participants viewed cards with neutral statements, such as “In the mountains, the air is fresh” and “Leaves change color in the fall,” while listening to an excerpt from Antonín Dvorák's “Slavonic Dances” (Op. 46, No. 1 in C major & Op. 72, No. 7 in C major). None of the neutral statements were self-statements.
Musical excerpts for both control and experimental groups were approximately 10 minutes long. After the music was finished, the study administrator turned off the tape and participants completed the post-induction VAS without discussion. For both conditions, the study administrator maintained a neutral affect so as not to influence participants’ responses.
Data Analyses
Independent samples t-tests were used to compare experimental and control participants on demographic characteristics and baseline depression, body dissatisfaction, and eating pathology. Repeated measures ANOVAs were used to examine effects of Group (experimental vs. control), Time (pre- vs. post-induction), and their interaction for influence on mood and body dissatisfaction. For each significant interaction, the simple effects of group within time and time within group were examined using a corrected p-value to control for multiple comparisons.
Results
There were no differences between experimental and control participants on demographic characteristics or baseline measures of global eating pathology, body dissatisfaction, or depression (see Table 1), supporting the success of randomization.
Table 1.
Comparison of Groups on Demographics and Measures of Related Pathology
| Control (n = 24) | Experimental (n = 21) | |||||
|---|---|---|---|---|---|---|
| Variable | M | SD | M | SD | t(39 to 42) | p |
| Age | 20.44 | 2.12 | 19.56 | 1.21 | 1.51 | .142 |
| BMI | 21.79 | 1.63 | 21.56 | 1.83 | 0.39 | .698 |
| BDI | 4.4 | 4.0 | 7.6 | 8.9 | −1.54 | .132 |
| BULIT-R | 57.3 | 20.5 | 64.9 | 27.1 | −1.06 | .297 |
| EAT-26 | 6.9 | 10.4 | 10.7 | 12.1 | −1.13 | .264 |
| EDI-BD | 5.7 | 6.1 | 6.8 | 7.4 | −0.53 | .602 |
Note. BDI = Beck Depression Inventory; BMI = body mass index; BULIT-R = Bulimia Test-Revised; EAT-26 = Eating Attitudes Test-26; EDI-BD = Body Dissatisfaction subscale of the Eating Disorder Inventory.
Effects on Mood
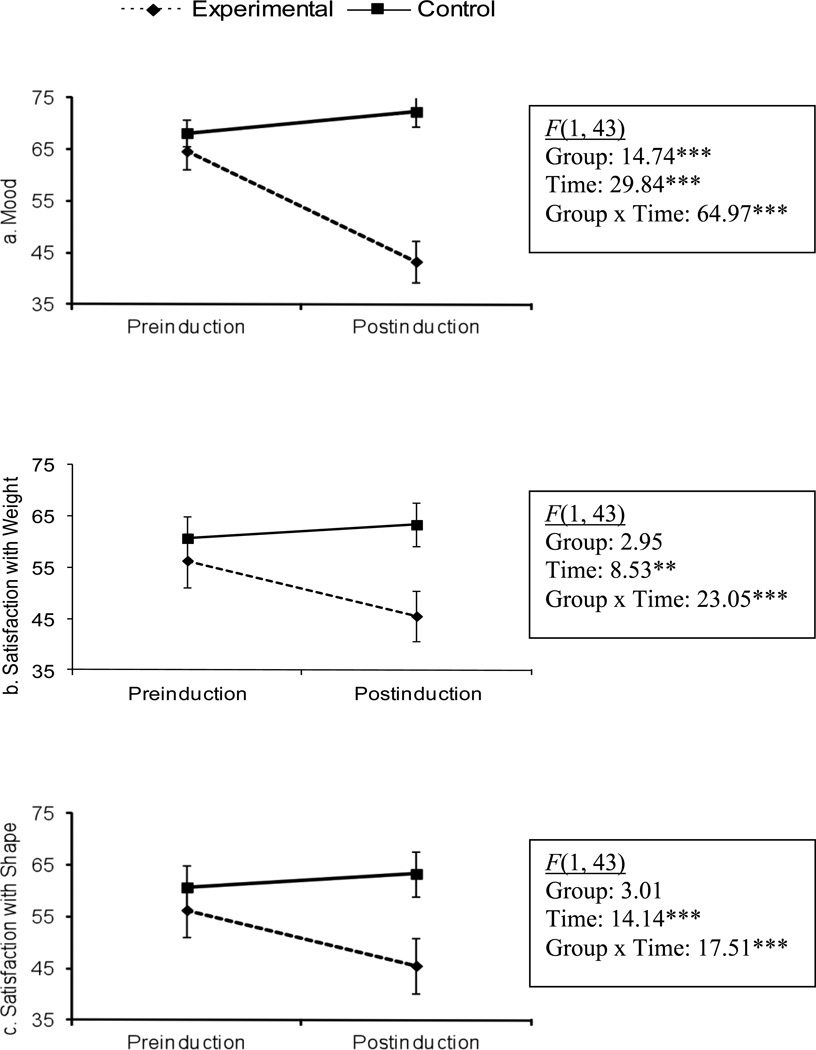
A repeated measures ANOVA revealed significant main effects of Group (experimental vs. control) and Time (pre-induction to post-induction) on mood. However, these main effects are qualified by a significant Group X Time interaction (Figure 1a). Both groups reported a moderately positive mood before induction procedures and did not differ from each other in the simple effects analysis (p = .41). Control participants’ mood remained relatively stable over time (p = .06), whereas experimental participants experienced a worsening of mood following the negative mood induction procedure (p < .001). Thus, results suggested that the experimental procedure was successful in inducing a negative mood.
Figure 1.
Repeated measures ANOVA for VAS scores before and after mood induction procedure. *p < .05, **p < .01, ***p < .001
Effects on Body Dissatisfaction
In addition to changes in mood, we hypothesized that experimentally induced changes in mood would cause changes in body satisfaction. There was a significant effect of Time and a significant Group × Time interaction for VAS ratings of satisfaction with weight and body shape (Figures 1b and 1c). Simple effects analyses revealed that experimental and control participants did not differ in levels of satisfaction with body shape or weight prior to induction procedures (ps > .35). Mirroring results for mood, satisfaction with body shape and weight decreased significantly in experimental participants (ps < .001) and did not change in control participants over time (ps > .17). Consistent with study hypotheses, results indicated that the negative mood induction procedure caused decreased satisfaction with body weight and shape among experimental participants.
Discussion
We employed a rigorous experimental design to examine causal relationships between mood and body dissatisfaction. A negative mood induction caused increased negative mood and increased body dissatisfaction, providing strong support for a causal model in which depressed mood contributes to body dissatisfaction. All participants were in a healthy weight range and, therefore, had no objective reason to experience body dissatisfaction during this study. In cultures which idealize thinness, body dissatisfaction may arise from funnelling general feelings of dysphoria into more concrete and culturally meaningful negative feelings about the body (Keel et al., 2001). Increases in body dissatisfaction may then lead to disordered eating behaviors, such as dieting and binge eating, that contribute to the development of eating disorders. These findings may explain why negative affect is a prospective risk factor for bulimia nervosa (Stice, 2002) and how negative affect could be a proximal trigger for disordered eating behaviors (Haedt-Matt & Keel, 2011).
However, current results do not rule out the possibility that body dissatisfaction also causes increased negative mood. Indeed, previous research has found that body dissatisfaction prospectively predicts greater negative affect (e.g., Paxton et al., 2006), and there are likely reciprocal relationships in which body dissatisfaction and negative mood contribute to each other. Further, negative mood may contribute to increased body dissatisfaction, which then causes even greater negative mood, resulting in a downward spiral similar to recent research on body checking and weight/shape concerns among Caucasian women (Fitzsimmons & Bardone-Cone, 2011). Future research is needed to examine potential reciprocal relations between mood and body satisfaction.
Limitations of this study included a predominantly Caucasian sample. In addition, participants were drawn from a non-clinical sample of undergraduate students, and causal relationships between mood and body dissatisfaction may differ in women with clinical eating disorders. However, depression is a significant longitudinal predictor of body dissatisfaction among women with bulimia nervosa (Keel et al., 2001). Thus, it appears that depression plays a role in the development of body dissatisfaction among a clinical sample. Future research is needed to further investigate the generalizability of these results. Participants were aware of the purpose of this study, and experimental participants were instructed to get into a sad mood. Thus, demand characteristics may have influenced who chose to participate and current findings. Future research is needed to examine the effects of a negative mood induction using more deceptive techniques, such as a back story or “filler” questionnaires. The current study compared a negative versus neutral mood induction condition and did not include a positive mood induction control. Future studies could investigate the impact of a positive mood induction on body satisfaction. In addition, future studies are needed to examine whether some individuals are predisposed to experiencing body dissatisfaction as a consequence of negative mood. We were precluded from examining potential moderators in the current study due to small sample size and a resulting lack of statistical power. However, trait personality characteristics and internalization of the thin ideal represent prime candidates to examine as moderators in future studies. Finally, the effects of changes in negative mood may not be specific to changes in body dissatisfaction. Increased negative mood could cause increased negative evaluations across multiple domains (e.g., feeling fat and feeling stupid). However, funnelling general negative emotions into body dissatisfaction may be specific to cultures where body shape and weight are used to evaluate one’s self-worth.
In conclusion, findings supported negative mood as a causal risk factor for body dissatisfaction. This research has important implications for the prevention of body dissatisfaction and, potentially, disordered eating. Most prevention programs employ a disease-specific pathway model that focuses specifically on body image, such as Student Bodies (C. B. Taylor et al., 2006) and Reflections: Body Image Program (Becker, Bull, Schaumberg, Cauble, & Franco, 2008). However, current results suggest that a non-specific vulnerability stressor model (Levine & Smolak, 2006), which focuses more on general mood states and sources of negative affect, such as stressful life events, lack of social support, and teasing, may also represent an effective prevention strategy. Supporting this assertion, intervention efforts targeted towards reducing depressive symptoms have been effective in reducing bulimic symptoms (Burton, Stice, Bearman, & Rohde, 2007). Importantly, current findings cannot establish whether increases in negative mood are the sole, or even primary, cause of body dissatisfaction. Thus, future studies are needed to compare the effects of programs based on a disease-specific pathway versus a non-specific vulnerability stress model on changes in body image, disordered eating, and related mood disturbances.
Highlights.
We examined the causal relationship between negative mood and body dissatisfaction.
We randomly assigned participants to either a negative mood or a neutral mood induction procedure.
Negative mood induction caused increased body dissatisfaction.
Findings support negative mood as a causal risk factor for body dissatisfaction.
Acknowledgements
This work was supported by grants F31 MH085456 (PI: Alissa Haedt-Matt) and R01 MH63758 (PI: Pamela Keel) from the National Institute of Mental Health. The authors would like to acknowledge Yvonne Garcia, Julie Gravener, Brooke Palmer, Erin Valenti, and Andrea Volfova for their assistance with data collection and data entry.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Portions of this research were presented at the 2007 International Conference on Eating Disorders in Baltimore, Maryland and the 21st Annual Meeting for the Society for Research in Psychopathology in Iowa City, Iowa.
References
- Baker JD, Williamson DA, Sylve C. Body image disturbance, memory bias, and body dysphoria: Effects of negative mood induction. Behavior Therapy. 1995;26:747–759. [Google Scholar]
- Bearman SK, Presnell K, Martinez E, Stice E. The skinny on body dissatisfaction: A longitudinal study of adolescent girls and boys. Journal of Youth and Adolescence. 2006;35:229–241. doi: 10.1007/s10964-005-9010-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Becker CB, Bull S, Schaumberg KF, Cauble A, Franco A. Effectiveness of peer-led eating disorders prevention: A replication trial. Journal of Consulting and Clinical Psychology. 2008;76:347–354. doi: 10.1037/0022-006X.76.2.347. [DOI] [PubMed] [Google Scholar]
- Burton E, Stice E, Bearman SK, Rohde P. Experimental test of the affect-regulation theory of bulimic symptoms and substance use: A randomized trial. International Journal of Eating Disorders. 2007;40:27–36. doi: 10.1002/eat.20292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter FA, Bulik CM, Lawson RH, Sullivan PF, Wilson JS. Effect of mood and food cues on body image in women with bulimia and controls. International Journal of Eating Disorders. 1996;20:65–76. doi: 10.1002/(SICI)1098-108X(199607)20:1<65::AID-EAT8>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- Clark DM. On the induction of depressed mood in the laboratory: Evaluation and comparison of the Velten and musical procedures. Advances in Behaviour Research & Therapy. 1983;5:27–49. [Google Scholar]
- Cohen-Tovée EM. Depressed mood and concern with weight and shape in normal young women. International Journal of Eating Disorders. 1993;14:223–227. doi: 10.1002/1098-108x(199309)14:2<223::aid-eat2260140213>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- Dunkley DM, Masheb RM, Grilo CM. Childhood maltreatment, depressive symptoms, and body dissatisfaction in patients with binge eating disorder: The mediating role of self-criticism. International Journal of Eating Disorders. 2010;43:274–281. doi: 10.1002/eat.20796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzsimmons EE, Bardone-Cone AM. Downward spirals of body surveillance and weight/shape concern among African American and Caucasian college women. Body Image. 2011;8:216–223. doi: 10.1016/j.bodyim.2011.04.003. [DOI] [PubMed] [Google Scholar]
- Garner DM, Olmstead MP, Polivy J. Development and validation of a multidimensional eating disorder inventory for anorexia nervosa and bulimia. International Journal of Eating Disorders. 1983;2:15–34. [Google Scholar]
- Garner DM, Olmsted MP, Bohr Y, Garfinkel PE. The Eating Attitudes Test: Psychometric features and clinical correlates. Psychological Medicine: A Journal of Research in Psychiatry and the Allied Sciences. 1982;12:871–878. doi: 10.1017/s0033291700049163. [DOI] [PubMed] [Google Scholar]
- Griffiths JA, McCabe MP. The influence of significant others on disordered eating and body dissatisfaction among early adolescent girls. European Eating Disorders Review. 2000;8:301–314. [Google Scholar]
- Haedt-Matt A, Keel PK. Revisiting the affect regulation model of binge eating: A meta-analysis of studies using ecological momentary assessment. Psychological Bulletin. 2011;137:660–681. doi: 10.1037/a0023660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinberg LJ, Thompson JK. Body image and televised images of thinnes and attractiveness: A controlled laboratory investigation. Journal of Social and Clinical Psychology. 1995;14:325–338. [Google Scholar]
- Johnson F, Wardle J. Dietary restraint, body dissatisfaction, and psychological distress: A prospective analysis. Journal of Abnormal Psychology. 2005;114:119–125. doi: 10.1037/0021-843X.114.1.119. [DOI] [PubMed] [Google Scholar]
- Keel PK, Mitchell JE, Davis TL, Crow SJ. Relationship between depression and body dissatisfaction in women diagnosed with bulimia nervosa. International Journal of Eating Disorders. 2001;30:48–56. doi: 10.1002/eat.1053. [DOI] [PubMed] [Google Scholar]
- Levine MP, Smolak L. The prevention of eating problems and eating disorders: Theory, research, and practice. Mahwah, NJ: Lawrence Erlbaum Associates Publishers; 2006. [Google Scholar]
- Paxton SJ, Neumark-Sztainer D, Hannan PJ, Eisenberg ME. Body dissatisfaction prospectively predicts depressive mood and low self-esteem in adolescent girls and boys. Journal of Clinical Child and Adolescent Psychology. 2006;35:539–549. doi: 10.1207/s15374424jccp3504_5. [DOI] [PubMed] [Google Scholar]
- Santos M, Richards CS, Bleckley MK. Comorbidity between depression and disordered eating in adolescents. Eating Behaviors. 2007;8:440–449. doi: 10.1016/j.eatbeh.2007.03.005. [DOI] [PubMed] [Google Scholar]
- Stice E. Risk and maintenance factors for eating pathology: A meta-analytic review. Psychological Bulletin. 2002;128:825–848. doi: 10.1037/0033-2909.128.5.825. [DOI] [PubMed] [Google Scholar]
- Taylor CB, Bryson S, Luce KH, Cunning D, Doyle AC, Abascal LB, Wilfley DE. Prevention of eating disorders in at-risk college-age women. Archives of General Psychiatry. 2006;63:881–888. doi: 10.1001/archpsyc.63.8.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor MJ, Cooper PJ. An experimental study of the effect of mood on body size perception. Behaviour Research and Therapy. 1992;30:53–58. doi: 10.1016/0005-7967(92)90096-y. [DOI] [PubMed] [Google Scholar]
- Thelen MH, Farmer J, Wonderlich S, Smith M. A revision of the Bulimia Test: The BULIT—R. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1991;3:119–124. [Google Scholar]
- Tylka TL, Subich LM. Examining a multidimensional model of eating disorder symptomatology among college women. Journal of Counseling Psychology. 2004;51:314–328. [Google Scholar]