Abstract
Purpose
To report changes in health-related quality of life (HRQOL) 1 year following strabismus surgery.
Design
Retrospective cohort study
Methods
73 adults undergoing strabismus surgery in a single clinical practice completed the Adult Strabismus-20 (AS-20) HRQOL questionnaire pre-operatively and at 6 weeks and 1 year post-operatively. All included adults were successfully aligned at 6 weeks post-operatively. Success was defined based on clinical criteria. Change in AS-20 psychosocial and function scores was evaluated as: 1) difference in scores between 6 weeks and 1 year post-operatively and 2) proportions exceeding previously published limits of agreement at 6 weeks and 1 year.
Results
For patients successfully aligned at both 6 weeks and 1 year (n=51), further improvement in median scores was seen from 6 weeks to 1 year for both the psychosocial scale (83.8 vs 93.8; P<0.0001) and the function scale (72.5 vs 77.5; P=0.007). Also, a greater proportion exceeded limits of agreement at 1 year than at 6 weeks (psychosocial: 48% vs 30%; P=0.007, function: 67% vs 51%; P=0.01). For patients who became partial success (n=18) or failure (n=4) at 1 year there was a numerical decrease in scores at 1 year.
Conclusions
Adult strabismus patients who remain successfully aligned, show continued improvement in both psychosocial and function scores from 6 weeks to 1 year post-operatively, indicating that improvement in HRQOL is long-lasting. Evaluation of HRQOL should be considered when reporting strabismus surgery outcomes in clinical trials, and may prove helpful in assessing outcomes in clinical practice.
Introduction
We have previously reported the development and validation of the Adult Strabismus-20 (AS-20), a health-related quality of life (HRQOL) questionnaire for adults with strabismus.1–3 Using this questionnaire, we found initial (6 week) post-operative improvement in HRQOL following successful strabismus surgery, and also found that the AS-20 discriminated well between patients classified as surgical success, partial success or failure.3 Nevertheless, it is unknown how strabismus surgery may affect HRQOL over a longer period of post-operative follow-up. In this present study, we evaluated changes in HRQOL 1 year following strabismus surgery, in patients successfully aligned at 6 weeks.
Methods
Patients
Seventy-three adult strabismus patients were prospectively recruited. Because we were interested in evaluating long-term change in HRQOL scores in patients who were initially successfully aligned post-operatively (Table 1), we included only patients designated as surgical “success” at their 6-week outcome exam. All included patients completed the AS-20 pre-operatively, at 6 weeks (median 7, range 4 to 14 weeks) and at 1 year (median 12, range 5 to 22 months) post-operatively. Fifty-six (77%) of 73 had strabismus with binocular diplopia and evidence of fusion potential and 17 (23%) had strabismus without diplopia. One (1%) of the 56 diplopia patients had visual confusion, but was grouped with diplopia patients, because the aim of surgery was to relieve symptoms of visual confusion. Patients were not recruited if they could not read or understand English or if they had severe cognitive impairment and we excluded patients with ocular myasthenia gravis because the condition may vary from day to day. Median age of our included patients was 53 (range 18 to 88) years; 50 (68%) were female and 69 (95%) self-reported their race as ‘White.’ Thirty-four (47%) had undergone previous surgery in a separate episode of care. Fifty-one of 73 patients underwent uniplanar surgery: 41 (56%) horizontal, 7 (10%) vertical and 3 (4%) torsional. Twenty-two of 73 patients underwent multi-planar surgery: 10 (14%) horizontal and vertical, 7 (10%) vertical and torsional, 4 (5%) horizontal and torsional and 1 (1%) underwent combined horizontal, vertical and torsional surgery. Median visual acuity was 20/20 (range 20/15 to 20/40) in the better eye and 20/25 (range 20/15 to Count Fingers) in the worse eye. Overall, 1 (1%) was in prism correction at their 6 week assessment and 10 (14%) at their 1-year outcome assessment. Pre-operative AS-20 data have been reported on 54 (74%) of 73 patients in previous analyses.2–4 Six-week post-operative AS-20 data have been previously reported on 53 (73%) of 73 patients.3 One-year data have not been previously reported.
Table 1.
Criteria used to define post-operative clinical outcomes as success, partial success or failure 1 year postoperatively in adults undergoing strabismus surgery.
| Success (All criteria must be met) | Partial success (All criteria must be met) | Failure (If any one criterion met) | |
|---|---|---|---|
| Angle of deviation by SPCT* | < 10 prism diopters straight ahead distance and near | ≤ 15 prism diopters straight ahead distance and near (without prism) | > 15 prism diopters straight ahead distance or near (without prism) |
| Diplopia / Visual confusion | None or “rare” straight ahead distance and reading | None, “rare” or “sometimes” straight ahead distance and reading. | “Always” or “often” straight ahead distance or reading |
| Prism | Not allowed | Allowed | Allowed |
| Bangerter foil / occlusion | Not allowed | Not allowed | Allowed |
For classification as success or partial success, all listed criteria had to be met, for classification as failure only one criterion had to be met. If the criteria for more than one outcome group was met, the patient was allocated to the group with the better outcome.
SPCT = simultaneous prism cover test.
Clinical assessment and questionnaire administration
Angle of deviation was measured pre- and post-operatively, at distance and near, using simultaneous prism and cover test (SPCT) and prism and alternate cover test (PACT). For 3 of 17 non-diplopic patients, Krimsky measurements were used as visual acuity did not allow accurate cover testing. Patients completed the AS-20 questionnaire at pre- and post-operative assessments. Questionnaires were self-administered, without supervision, following simple verbal and written instructions and were typically completed before any clinical examination procedures had been performed. Patients were instructed to respond as when wearing any habitual refractive correction, including prism if prescribed.
The AS-20 consists of 20 items in 2 subscales, 10 in a psychosocial subscale and 10 in a function subscale (full questionnaire with user instructions available at: http://public.pedig.jaeb.org/, accessed September 30, 2011). For each question a 5-point Likert type scale is used for responses: ‘never’ (score 100), ‘rarely’ (score 75), ‘sometimes’ (score 50), ‘often’ (score 25), and ‘always’ (score 0).1 A psychosocial score (10 items), and function score (10 items) is calculated as a mean of all answered items and ranges from 0 to 100 (worst to best HRQOL).1 One patient overlooked the psychosocial subscale questions at their pre-operative examination and one overlooked the psychosocial subscale at their 6-week postoperative examination; therefore pre- to post-operative differences on the psychosocial scale could not be calculated for these 2 patients (total 71 patients for analyses of psychosocial subscale).
Classification of post-operative outcomes
We defined post-operative outcome groups a priori, based on clinical criteria alone (Table 1). Three post-operative outcome categories were created: success, partial success and failure (Table 1). If patients met the criteria for more than one group, they were allocated to the group with the better outcome. Classification as success required no diplopia / visual confusion (or only “rare”) straight ahead distance and for reading, with less than 10 pd heterotropia in primary position at distance and near by SPCT (Table 1). Classification as partial success required, diplopia / visual confusion present “sometimes” or less straight ahead distance and for reading (with or without prism), and no more than 15 pd heterotropia (Table 1). Classification as surgical failure was assigned if either diplopia / visual confusion was “often” or “always” straight ahead distance or for reading, or if there was more than 15 pd heterotropia at distance or near, or the patient was using a Bangerter foil / occlusion (Table 1). Patients classified as failure at 1 year continued under clinical care for further management, but additional treatment and outcome data are not reported in the present study.
For assessment of diplopia frequency, we have increasingly utilized a revised diplopia questionnaire (Smith SJ, Liebermann L, Hatt SR, Leske DA, Holmes JM. Quantifying diplopia using a patient-reported outcome questionnaire. Invest Ophthalmol Vis Sci 2011;52:ARVO E-Abstract 6361), completed by the patient. Revised diplopia questionnaire data were available, and used for classification of outcomes, in 9 (12%) of 73 at 6 weeks and 43 (59%) of 73 at 1 year. If revised diplopia questionnaire data were not available, frequency of diplopia was ascertained using the medical history.
Analyses
AS-20 psychosocial and function scores1 were calculated for each patient at the pre-operative assessment and at 6-weeks and 1-year post-operatively, as the mean of all answered items. Pre-operative, 6-week post-operative and 1-year post-operative AS-20 psychosocial and function scores were analyzed in two ways: 1) Difference between scores from pre-operatively to 6 weeks post-operatively and from 6 weeks to 1 year post-operatively, compared using signed rank tests, reporting medians and quartiles of the scores; 2) Comparison of proportions exceeding previously published 95% limits of agreement (LOA) (psychosocial scale 17.7 points; function scale 19.5 points2), using McNemar’s tests. Analyses were performed across all patients, and separately for diplopic and non-diplopic patients, without regard to success status at 1 year. A secondary analysis was performed for sub-groups according to success status at 1 year: 1) success at both 6 weeks and 1 year; 2) success at 6 weeks, partial success at 1 year; 3) success at 6 weeks, failure at 1 year. All statistical analyses were performed using SAS computer software version 9.1.3.
Results
Post-operative outcomes
By study design, all included patients were classified as success at 6 weeks. Overall, 51 (70%) were successfully aligned at both 6 weeks and 1 year postoperatively, 18 (25%) become partial successes at 1 year (17 diplopic, 1 non-diplopic) and 4 (5%) became failures at 1 year (3 diplopic, 1 non-diplopic). For diplopia patients, 36 (64%) of 56 were a success at both 6 weeks and 1 year. For non-diplopic patients, 15 (88%) of 17 were a success at both 6 weeks and 1 year.
Median change
AS-20 psychosocial score
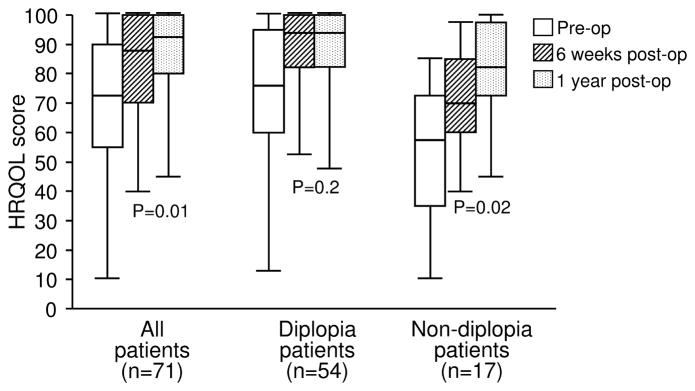
Across all patients (n=71 with pre- and post-operative psychosocial scores), median AS-20 psychosocial score improved from 72.5 (quartiles 55.0, 90.0) pre-operatively to 87.5 (70.0, 100.0; P <0.0001) 6 weeks post-operatively (Figure 1). There was further improvement in psychosocial scores at 1 year post-operatively (92.5 [80.0, 100.0]; P=0.01). For non-diplopic patients, median psychosocial score improved from 57.5 (35.0, 72.5) pre-operatively to 70.0 (60.0, 85.0; P=0.0006) 6 weeks postoperatively, with further improvement at 1 year post-operatively (82.5 [72.5, 97.5] P=0.02) (Figure 1). For diplopic patients, median psychosocial scores improved from 76.3 (60.0, 95.0) pre-operatively to (93.8 [82.5, 100.0]; P<0.0001) at 6 weeks postoperatively, however there was no further improvement in scores at 1 year (93.8 [82.5, 100.0]; P=0.2) (Figure 1).
Figure 1.
Psychosocial Adult Strabismus-20 (AS-20) scores pre-operatively, 6 weeks post-operatively and 1 year post-operatively in 71 adult strabismus patients successfully aligned at 6 weeks (overall, without regard to success status at 1 year). Scores improved further at 1 year, across all patients and for non-diplopic patients. Boxes represent 1st quartile, median and 3rd quartile values; whiskers represent extreme values. P value represents difference between 6 weeks and 1 year.
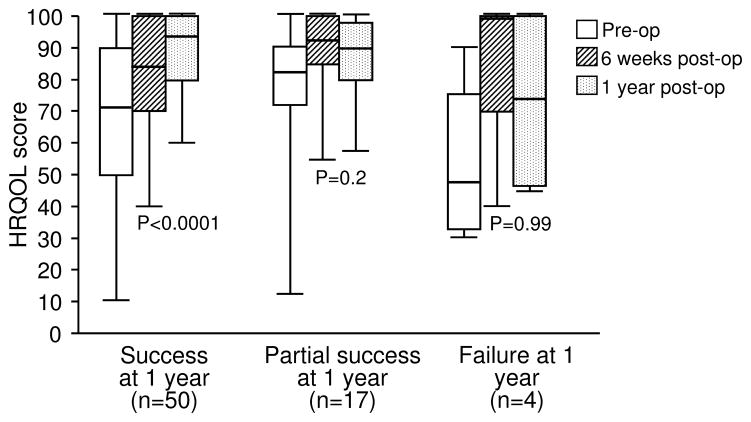
For the 50 patients classified as success at both 6 weeks and 1 year (with pre- and post-operative psychosocial scores), median psychosocial score improved from 71.3 (50.0, 90.0) pre-operatively to 83.8 (70.0, 100.0; P<0.0001) at 6 weeks postoperatively (Figure 2). There was further improvement in psychosocial scores at 1 year post-operatively (93.8 [80.0, 100.0]; P<0.0001) (Figure 2). Both diplopia patients (n=35) and non-diplopia patients (n=15) who were a success at both 6 weeks and 1 year, showed further improvement in scores at 1 year (P<0.03 for each comparison). For the 17 patients who became a partial success at 1 year, median psychosocial score improved from 82.5 (72.5, 90.0) pre-operatively to 92.5 (85.0, 100; P=0.002) 6 weeks post-operatively, but there was no further improvement in scores at 1 year (90.0 [80.0, 97.5]; P=0.2) (Figure 2). For the 4 patients who became failures at 1 year, there was a large numerical improvement from pre-operatively (47.5 [32.5, 75.0]) to 6 weeks postoperatively (100.0 [70.0, 100.0]; P=0.1), but this did not reach statistical significance due to small sample size. For these 4 failures at 1 year, there was a numerical decrease in 1-year psychosocial score (73.8 [46.3, 100.0]; P=0.99) (Figure 2).
Figure 2.
Psychosocial Adult Strabismus-20 (AS-20) scores pre-operatively, 6 weeks post-operatively and 1 year post-operatively in 71 adult strabismus patients successfully aligned at 6 weeks and sub-classified as success, partial success and failure at 1 year. For patients who remained successfully aligned at 1 year psychosocial scores improved further at 1 year. Boxes represent 1st quartile, median and 3rd quartile values; whiskers represent extreme values. P value represents difference between 6 weeks and 1 year.
AS-20 function score
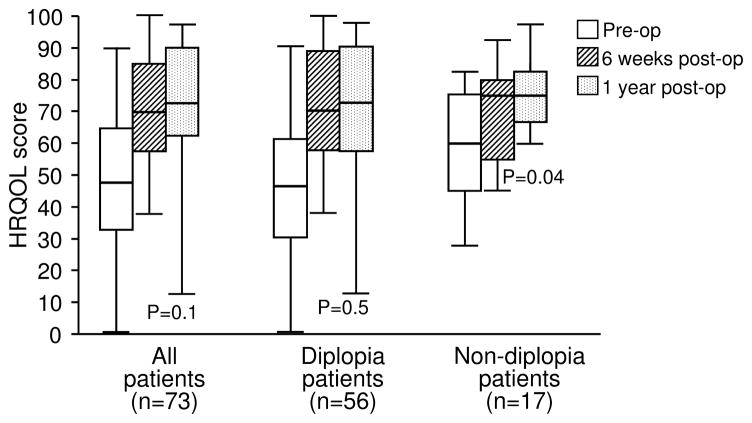
Across all patients, median AS-20 function score improved from 47.5 (quartiles 32.5, 65.0) pre-operatively to 70.0 (57.5, 85.0; P<0.0001) at 6 weeks post-operatively. There was no further improvement in median function score at 1 year post-operatively (72.5 [62.5, 90.0]; P=0.1) (Figure 3). For diplopic patients median function score improved from 46.3 (30.0, 61.3) pre-operatively to 70.0 (57.5, 88.8; P<0.0001) 6 weeks post-operatively, but there was no further improvement in scores at 1 year (72.5 [57.5, 90.0]; P=0.5) (Figure 3). For non-diplopic patients, median function score improved from 60.0 (45.0, 75.0) pre-operatively to 75.0 (55.0, 80.0; P=0.04) at 6 weeks postoperatively, with further improvement in scores at 1 year post-operatively (75.0 [66.7, 82.5]; P=0.04) (Figure 3).
Figure 3.
Function Adult Strabismus-20 (AS-20) scores pre-operatively, 6 weeks postoperatively and 1 year post-operatively in 73 adult strabismus patients successfully aligned at 6 weeks (overall, without regard to success status at 1 year). Scores improved further at 1 year in non-diplopic patients. Boxes represent 1st quartile, median and 3rd quartile values; whiskers represent extreme values. P value represents difference between 6 weeks and 1 year.
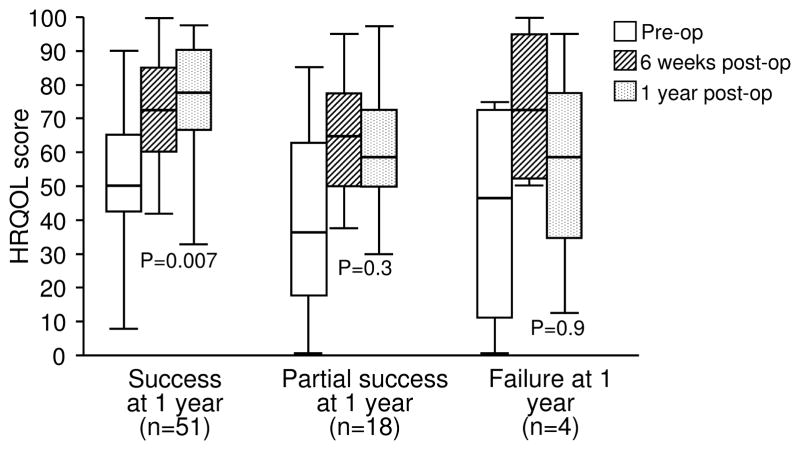
For the 51 patients classified as success at both 6 weeks and 1 year (with pre- and post-operative function scores), median function scores improved from 50.0 (42.5, 65.0) pre-operatively to 72.5 (60.0, 85.0; P<0.0001) at 6 weeks post-operatively (Figure 4). There was further improvement in function scores at 1 year post-operatively (77.5 [66.7, 90.0]; P=0.007) (Figure 4). Diplopia patients (n=36) who were a success at both 6 weeks and 1 year showed further improvement in scores at 1 year (P=0.04), but non-diplopic patients (n=15) showed no further improvement in scores at 1 year (P=0.08). For the 18 patients who became a partial success at 1 year, median function scores improved from 36.3 (17.5, 62.5) pre-operatively to 65.0 (50.0, 77.5); P<0.0001) 6 weeks post-operatively, but there was no further improvement in scores at 1 year (58.8 [50.0, 72.5]; P=0.3) (Figure 4). For the 4 patients who became failures at 1 year, there was a large numerical improvement from pre-operatively (46.3 [11.3, 72.5]) to 6 weeks postoperatively (72.5 [52.5, 95.0]; P=0.4) but this did not reach statistical significance due to small sample size. For these 4 failures there was a numerical decrease in function score from 6 weeks to 1 year (58.8 [35.0, 77.5]; P=0.9) (Figure 4).
Figure 4.
Function Adult Strabismus-20 (AS-20) scores pre-operatively, 6 weeks postoperatively and 1 year post-operatively in 73 adult strabismus patients successfully aligned at 6 weeks and sub-classified as success, partial success and failure at 1 year. For patients who remained successfully aligned at 1 year, function scores improved further. Boxes represent 1st quartile, median and 3rd quartile values; whiskers represent extreme values. P value represents difference between 6 weeks and 1 year.
Proportions exceeding 95% limits of agreement
AS-20 psychosocial score
Across all patients (n=71 with pre- and post-operative psychosocial scores), the proportion who exceeded 95% LOAs on the psychosocial scale was greater at 1 year than at 6 weeks post-operatively (41% vs 28%; P=0.01) (Table 2). This improvement in scores at 1 year was apparent in diplopic patients (39% vs 24%; P=0.02), but not in non-diplopic patients (47% vs 41%; P=0.3) (Table 2).
Table 2.
Proportion of adult strabismus patients (overall, diplopia patients, no diplopia patients) showing pre- to postoperative change in Adult Strabismus-20 health-related quality of life psychosocial and function scores exceeding 95% limits of agreement (psychosocial scale 17.7 points; function scale 19.5 points2), 1 year post-operatively.
| Proportion exceeding limits of agreement | Overall (n=73) | Diplopia (n=56) | No diplopia (n=17) | |||
|---|---|---|---|---|---|---|
| 6 weeks post- operatively | 1 year post- operatively | 6 weeks post- operatively | 1 year post- operatively | 6 weeks post- operatively | 1 year post- operatively | |
| AS-20 Psychosocial | 20/71* (28%) | 29/71* (41%) | 13/54 (24%) | 21/54 (39%) | 7/17 (41%) | 8/17 (47%) |
| AS-20 Function | 38/73 (52%) | 43/73 (59%) | 34/56 (61%) | 36/56 (64%) | 4/17 (24%) | 7/17 (41%) |
Significantly greater proportion of patients exceeded 95% LOA at 1 year than at 6 weeks (P=0.02)
For the 50 patients classified as success at both 6 weeks and 1 year, a greater proportion exceeded limits of agreement at 1 year (48%) compared with 6 weeks (30%; P=0.007) (Table 3). For the 17 patients classified as success at 6 weeks and partial success at 1 year, proportions were similar at 1 year and 6 weeks (24% vs 18%; P=0.3). For the 4 patients classified as success at 6 weeks and failure at 1 year, proportions were also similar, although the comparison was limited by small sample size (25% vs 50%; P= 0.3) (Table 3).
Table 3.
Proportion of adult strabismus patients showing pre- to post-operative change in Adult Strabismus-20 psychosocial (n=71) and function (n=73) scores exceeding 95% limits of agreement (psychosocial scale 17.7 points; function scale 19.5 points2), grouped according to alignment 1 year post-operatively (success, partial success, failure)
| Proportion exceeding limits of agreement | Success 6 weeks, success 1 year | Success 6 weeks, partial success 1 year | Success 6 weeks, failure 1 year | |||
|---|---|---|---|---|---|---|
| 6 weeks post- operatively | 1 year post- operatively | 6 weeks post- operatively | 1 year post-operatively | 6 weeks post- operatively | 1 year post- operatively | |
| AS-20 Psychosocial | 15/50* (30%) | 24/50* (48%) | 3/17 (18%) | 4/17 (24%) | 2/4 (50%) | 1/4 (25%) |
| AS-20 Function | 26/51* (51%) | 34/51* (67%) | 9/18 (50%) | 7/18 (39%) | 3/4 (75%) | 2/4 (50%) |
Significantly greater proportion of patients exceeded 95% LOA at 1 year than at 6 weeks (P<0.01 for each comparison)
AS-20 function score
For the function scale, the proportion who exceeded 95% LOAs was similar at 1 year compared with 6 weeks, across all patients (59% vs 52%; P=0.2), for diplopia patients (64% vs 61%; P=0.5), and for non-diplopic patients (41% vs 24%; P=0.08) (Table 2).
For the 51 patients classified as success at both 6 weeks and 1 year, a greater proportion exceeded LOAs at 1 year compared to 6 weeks (67% vs 51%; P=0.01) (Table 3). Proportions were similar at 1 year and 6 weeks for those classified as success at 6 weeks and partial success at 1 year (n=18) (39% at 1 year vs 50% at weeks; P=0.2) and for those classified as success at 6 weeks and failure at 1 year (n=4), (50% at 1 year vs 75% at 6 weeks; P=0.3) (Table 3).
Discussion
Adult strabismus patients who remain successfully aligned, show further improvements in HRQOL from 6 weeks to 1 year following strabismus surgery. Improvements in HRQOL affect both psychosocial and function domains and occur in both diplopic and non-diplopic types of strabismus. For patients whose clinical status changes from success at 6 weeks to partial success or failure at 1 year, no additional improvements in HRQOL are seen.
There are few previous studies reporting prospectively evaluated changes in HRQOL in adult strabismus patients undergoing surgery. There are also few data on how HRQOL may change immediately following surgery compared with longer-term post-operative follow-up. Jackson et al5 prospectively studied pre- and post-operative HRQOL scores in 46 strabismic adults, using generic HRQOL instruments. In the Jackson et al5 study, post-operative outcomes were assessed once, an average of 3 months following surgery, and showed overall improvements in psychosocial adjustment, but outcomes were not interpreted in the context of clinical success or failure. Assessing changes in HRQOL over a longer period of follow-up enables evaluation of the lasting benefits of strabismus surgery. We previously reported improvements in HRQOL in successfully aligned patients at 6-weeks post-operatively,3 but in the present study we found that improvements in HRQOL increased 1 year following successful surgery. These data indicate that successful strabismus surgery has a long-lasting, positive impact on the patient’s HRQOL.
We analyzed our 1-year data firstly overall (without regard to success status at 1 year) and secondly by success status at 1 year. Both approaches have potential biases; for the first approach, if a large proportion of patients became clinical failures at 1 year it would be difficult to find an overall effect. Whereas for the second approach, limiting the cohort to 1-year successes might introduce selection bias. Nevertheless, both approaches indicated improvement in HRQOL from 6 weeks to 1 year. Including all patients seen 1-year post-operatively (regardless of success status at 1 year), continued improvement was seen mainly in psychosocial scores. The lack of further improvement in function scores at 1 year was likely due to inclusion of partial successes and failures in this initial analysis, most of whom were classified as not successful due to recurrent diplopia. In our secondary analysis, limited to patients who remained successfully aligned at 1 year, diplopic patients did in fact show further improvement in function scores at 1 year. These data provide further evidence of the comprehensive HRQOL benefits of strabismus surgery when patients remain well aligned and diplopia free.
In this study, we confirmed with 1-year follow-up data, our previous 6-week finding,3 that the AS-20 questionnaire is responsive and discriminates well between surgical success, partial success and failures. Patients classified as partial success or failure at 1 year (and therefore by definition having recurrent strabismus) showed no further improvement in scores whereas patients classified as success showed further improvement in scores. These qualities of responsiveness and discrimination are important in a HRQOL questionnaire, especially when interpreting change in HRQOL scores over time, and allow average change in scores to be attributed to real change in underlying conditions, rather than other potential sources of variability.
Continued improvements in HRQOL over a longer period of post-operative follow-up, may be explained in part by physical phenomena such as resolved redness and improved ocular comfort. In addition, the impact of improved alignment may become more evident to the patient with increased exposure to social situations and with more extended experience of visually demanding tasks. Our definition of success was such that it is unlikely that further improvements in HRQOL were due to further changes in underlying alignment. It is possible that the patient’s personality may influence perceived improvement, or that there may be a placebo effect from surgery, but we attempted to avoid such potential biases by carefully defining a cohort of successfully aligned patients, using clinical criteria alone. We therefore feel it is reasonable to interpret our data as showing real, long-lasting improvements in HRQOL following strabismus surgery.
We utilized two methods to analyze pre- to post-operative change in HRQOL scores. For change across a population we analyzed median scores and found significant improvements from pre-operatively to 6 weeks and 1 year post-operatively. Our alternative method involved analyzing change at the individual patient level, using previously derived 95% LOAs2 as the threshold for real change. We found that a greater proportion of patients exceeded these thresholds at 1 year than at 6 weeks postoperatively, when analysis was limited to patients who remained successfully aligned at 1 year. Nevertheless, not all successfully aligned patients exceeded the LOAs (highest proportion 67% on function scale at 1 year, Table 3). It is possible that due to individual patient variability, the derived 95% LOA values present somewhat unrealistic thresholds for individual patients to exceed. Despite this limitation, there may still be value in using 95% LOAs for auditing clinical outcomes and for evaluating treatment effectiveness in clinical trials.
There are some limitations to our study. In selecting only patients with 1-year post-operative follow-up, we recognize there may be some selection bias. Patients often attend our practice from a considerable geographical distance and therefore may only return 1 year following surgery if there are ongoing problems or concerns. Such self-selection would bias towards finding no further improvement in HRQOL at 1 year, while we found further improvement. Our finding of further improved psychosocial scores at 1 year when analyzing all patients (including partial successes and failures at 1 year) may appear suggestive of a possible placebo effect from surgery. Nevertheless, when analyzed separately, patients who worsened to partial success or failure at 1 year showed a numerical decrease in scores from 6 weeks to 1 year (statistical analysis limited by small sample size). We aimed to avoid any influence of the clinical examination findings on the patient’s perception of their HRQOL, by having patients complete the AS-20 before their clinical examination commenced. In the few cases where this was not achieved (due to the demands of busy clinics) and the AS-20 was completed during the examination, the clinical findings may have influenced the patient’s responses. However it is unlikely that this would cause any systematic bias towards better or worse HRQOL scores.
In diplopic and non-diplopic adult strabismus patients, HRQOL continues to improve from 6 weeks to one year following successful strabismus surgery, in both psychosocial and function domains, confirming the lasting benefits of strabismus surgery in such populations. The AS-20 provides a useful tool for assessing HRQOL in cohorts of adult strabismus patients, both for evaluating outcomes in clinical practice and in clinical trials.
Acknowledgments
Funding / Support: Supported by National Institutes of Health Grants EY015799 and EY018810 (JMH), Research to Prevent Blindness, New York, NY (JMH as Olga Keith Weiss Scholar and an unrestricted grant to the Department of Ophthalmology, Mayo Clinic), and Mayo Foundation, Rochester, MN.
Other Acknowledgments: None
Footnotes
Conflict of interest: No conflicting relationship exists for any author
Contributions to Authors: design and conduct of the study (SRH, LL, DAL, JMH); collection of data (SRH, LL, JMH), management, analysis, and interpretation of the data (SRH, DAL,LL, JMH); preparation, review and approval of the manuscript (SRH, DAL, LL, JMH).
Statement about Conformity with Author Information: Institutional Review Board/Ethics Committee Mayo Clinic, Rochester MN prospectively approved this study. All experiments and data collection were conducted in a manner compliant with the Health Insurance Portability and Accountability Act. Informed consent was obtained from all participants. All research procedures adhered to the tenets of the Declaration of Helsinki.
Financial Disclosures: Grant support by National Institutes of Health Grants EY015799 and EY018810 (JMH), and Research to Prevent Blindness, New York, NY (JMH as Olga Keith Weiss Scholar and an unrestricted grant to the Department of Ophthalmology, Mayo Clinic)
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Hatt SR, Leske DA, Bradley EA, Cole SR, Holmes JM. Development of a Quality-of-Life Questionnaire for Adults with Strabismus. Ophthalmology. 2009;116(1):139–144. doi: 10.1016/j.ophtha.2008.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Leske DA, Hatt SR, Holmes JM. Test-retest reliability of health-related quality of life questionnaires in adults with strabismus. Am J Ophthalmol. 2010;149(4):672–676. doi: 10.1016/j.ajo.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hatt SR, Leske DA, Holmes JM. Responsiveness of health-related quality of life questionnaires in adults undergoing strabismus surgery. Ophthalmology. 2010;117(12):2322–2328. doi: 10.1016/j.ophtha.2010.03.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hatt SR, Leske DA, Bradley EA, Cole SR, Holmes JM. Comparison of quality of life instruments in adults with strabismus. Am J Ophthalmol. 2009;148(4):558–562. doi: 10.1016/j.ajo.2009.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jackson S, Harrad RA, Morris M, Rumsey N. The psychosocial benefits of corrective surgery for adults with strabismus. Br J Ophthalmol. 2006;90(7):883–888. doi: 10.1136/bjo.2005.089516. [DOI] [PMC free article] [PubMed] [Google Scholar]