Abstract
OBJECTIVE:
To identify whether a health-related quality of life (HRQoL) instrument intended to capture reproductive concerns is sensitive and appropriate for adolescent patients with cancer.
METHODS:
Pilot testing was completed by administering a 10-item instrument designed to identify reproductive concerns of female adolescent patients with cancer aged 12–18. Parents were also asked to predict their daughters’ responses. Fourteen patients and parents participated. The main outcome measures were language, relevance, accuracy, sensitivity, and missing content regarding the HRQoL instrument. Two pediatric hospitals and 1 local support group for patients and survivors served as the setting for this study.
RESULTS:
The majority of parents provided inaccurate predictions of their daughters’ responses regarding their reproductive concerns. Overall, parents underestimated their daughters’ concerns because the majority of adolescents reported a strong desire for future parenthood whereas parents expected their daughters to be satisfied with survivorship.
CONCLUSIONS:
Adolescent patients with cancer have strong reproductive concerns; however, this may not be captured on current HRQoL instruments and may be further neglected due to parents’ unawareness. Discussions should be encouraged with adolescent patients before beginning treatment regarding their concerns and values about parenting in the future and cannot rely on parent-proxy reports.
KEY WORDS: adolescent, cancer, congruence, fertility, reproduction
What’s Known on This Subject:
Survival takes precedence for adolescent patients with cancer and their families. Patients may not discuss their treatments’ potential to damage their reproductive capacity, which has significant psychological late effects in survivorship.
What This Study Adds:
Strong reproductive concerns of adolescents with cancer may not be captured on current health-related quality of life instruments and may be neglected by parents’ unawareness. Parent-proxy reports of adolescent reproductive concerns are not suitable for capturing specific emotions and feelings.
Advances in technology, pharmaceuticals, and screening over the past 40 years have dramatically improved rates of survival for what was once thought to be a rarely curable disease: childhood cancer. Between the years 2003 and 2008, more than 36 000 new cases of childhood cancer were reported.1 These new clinical advances are steadily increasing rates of successful treatment, and pediatric patients today have an 80% chance of survival.2
Survival often takes immediate precedence in the minds of patients and families after a diagnosis. Yet, soon thereafter, they may begin to consider and experience a variety of late effects from the treatment received. Infertility is a potential late effect from treatment of cancer. Infertility may be reversible after some cancer treatments, although sustained infertility develops in 50% to 95% of adult cancer survivors.3–5 The US-based organizations the American Society of Clinical Oncology and the American Academy of Pediatrics have recommended that all patients with cancer of childbearing age be informed about the potential for infertility due to cancer treatments and be referred to a reproductive endocrinologist.6,7
Studies examining patient and survivor perspectives on fertility show evidence of remorse and regret among those who felt uninformed.8,9 However, few studies have systematically assessed the reproductive concerns and preferences of patients with cancer themselves, and only a few studies have focused on adolescents.8,10 Adolescents in particular are an important group to study because they represent ∼4 to 6 times the number of childhood patients with cancer.11
Health-related quality of life (HRQoL) assessment tools are commonly used in the adolescent cancer population to measure physical, psychological, social, and cognitive domains which can predict and track outcomes in clinical trials and research and evaluation purposes as well as highlight needs for a variety of healthcare services.12 Some studies have used HRQoL measurements with pediatric populations that are designed for and by adults, limiting the accuracy of the results.13,14 Although HRQoL assessments are intended to be completed by the patients themselves, there are times, particularly in pediatrics, that patients cannot complete these assessments because of illness, age, cognitive impairments, or extreme fatigue.15 In these cases parents may serve as the proxy patient; however, parent reports of their child’s HRQoL should be noted as secondary information and not be misconstrued as the patient’s own words because of the discrepancies of many parent-proxy reports.12,16
Only considering the parents’ concerns about the adolescents’ health may lead to underreporting or overreporting of HRQoL and may result in inefficient resource use as healthcare workers attempt to meet the needs of the adolescent. It was once believed that parents should be the only reporters of their children’s HRQoL,17 but more recently, adolescents’ unique health perceptions are being recognized.16,18
Current HRQoL instruments for both adult and adolescent patients with cancer lack comprehensive assessments of reproductive concerns. Wenzel et al19 developed a stand-alone 14-item Reproductive Concerns Scale in 2005 to assess a variety of reproductive concerns of adult female cancer survivors. The Reproductive Concerns Scale was validated by using adult female healthy controls with a high internal consistency among survivors (Cronbach’s α coefficient = 0.91).19 No parallel measure currently exists for adolescent oncology patients.
To expand on the existing literature, we conducted a study to pilot test a 10-item reproductive concerns scale adapted for adolescent patients with cancer. Adolescent patients with cancer and their parents were administered the instrument in separate interviews; in this article we report only the findings on the large amount of incongruent responses between parents and adolescents. On the basis of the existing literature,16,20–24 it was hypothesized that adolescents will have fewer reproductive concerns than their parents or that adolescents will not view their concerns as drastically and negatively as parents. This hypothesis was supported by the belief that adolescents would struggle to actualize the long-term effects of potentially losing the ability to have biological children, whereas parents have already experienced and been impacted by parenthood. We also hypothesized that congruence between parent and adolescent would vary by age. Older adolescents may be more likely to have considered parenthood and have a better understanding of reproduction. As a result, older adolescents may tend to share similar reproductive concerns with their parents, thus resulting in higher congruence as compared with younger adolescents.
Methods
Participants
Participants in this study were adolescents aged 12 to 18 and their parents. Eligibility criteria included the following: (1) must have had cancer diagnosis; (2) currently undergoing treatment or had undergone treatment within the past 6 months of recruitment; (3) ability to speak and comprehend questions in English; and (4) willingness to provide assent from adolescents and written consent from parents. This was a multicenter study including adolescents who received treatment at 2 pediatric oncology centers: All Children’s Hospital in St. Petersburg, Florida, and Children’s Hospital of Orange County in Orange County, California, as well as additional recruitment from a nonprofit organization in Tampa, Florida, providing support to adolescent oncology patients and their families. The University of South Florida and Children’s Hospital of Orange County Institutional Review Boards approved this study.
Survey Instrument
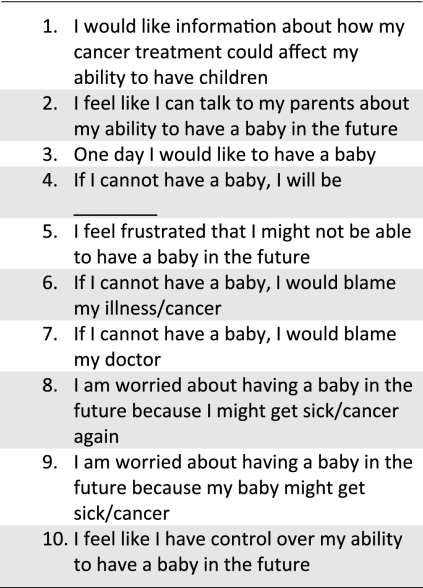
On the basis of a review of the existing literature, the research team determined that there were no validated survey instruments that captured the reproductive concerns of adolescents with cancer. Wenzel et al’s19 reproductive concerns instrument was developed for adult women with cancer, and it was determined that to administer this instrument to adolescents, adaptations must be made. Preliminary adaptations were made to the Wenzel et al19 items, resulting in a 10-item instrument applicable to adolescents aged 12 to 18 (Fig 1). The adapted reproductive concerns scale assessed adolescents’ concerns with potential effects of treatment on fertility, assigning blame for potential infertility, and feelings associated with potential infertility. In separate interviews, adolescents and their parents were read each item and were then asked to answer the item and also describe how they felt about the statement itself. This process, called cognitive debriefing, is a key component to ensuring that future adaptations were age and cognitively appropriate. Cognitive debriefing solicits direct input from participants on the item content, format, and presentation and the level at which the item or statement is understood.25,26 Parents were asked to also predict their child’s response to each of the original items (shown in Table 1). The accuracy of these predictions is detailed below.
FIGURE 1.
Ten-item reproductive concerns adapted from Wenzel et al19 (adapted assessment).
TABLE 1.
Suggested Changes to the Original Items by Respondents and Congruence Between Parent and Child Responses to the Original Items
| Parent Prediction of Child Response, (%) | Child Response, (%) | |
|---|---|---|
| Do you understand fertility?a | 86 | 100 |
| One day I would like to have a baby.b | 71 | 93 |
| If I cannot have a baby in the future, I will be sad.b | 50 | 29 |
| Disappointeda | 7 | 36 |
| Open-endeda | 43 | 29 |
| I feel frustrated that I might not be able to have a baby in the future.b | 21 | 7 |
| Sada | 29 | 7 |
| Disappointeda | 14 | 50 |
| Open-endeda | 14 | 7 |
| Othera | 14 | 29 |
| I feel like I have control over my fertility.b | 21 | 29 |
| I feel like I can talk to my parents about fertility.b | 100 | 64 |
| I have talked to my parents about fertility.a | 86 | 71 |
| If I cannot have a baby, I would blame the illness/cancer.b | 79 | 43 |
| If I cannot have a baby, I would blame the doctor.b | none | none |
| I am satisfied with the information I received about my future fertility.b | 79 | 42 |
| Do you want to know the impacts of your treatment on your fertility?a | 71 | 79 |
| I am worried about having a baby in the future because I might get cancer again.b | 29 | 57 |
| I am worried about having a baby in the future because my baby might get cancer.b | 43 | 71 |
| Worried baby will have treatment defects?a | 4 | 11 |
| Would you consider adoption?a | 14 | 21 |
Represent participants’ suggested changes to the items.
Represent the original 10 HRQoL items.
Interview
After informed consent was obtained from both parent and adolescent, interviews were conducted separately (by Devin Murphy). The ability to conduct the interviews separately is germane to this study to ensure that parents did not prompt adolescent answers or prevent adolescents from expressing their feelings since parental presence may cause them to feel embarrassed or self-conscious. Each interview was tape recorded and subsequently transcribed verbatim. The interviews lasted between 30 and 40 minutes, with both adolescents and parents being given an incentive of $25 at the completion of each interview. Interviews were conducted between July 2009 and November 2010.
Analysis
Once all the audiotapes were transcribed, data analysis was based on the constant comparative method and the grounded theory approach. Adolescent and parent interviews were analyzed separately, and then familial dyads were analyzed for congruence. Codes were created to categorize responses and were then aggregated into themes. Similar qualitative themes were grouped together,27 and the research team identified subcategories that emerged through several rounds of thematic validation.28 Each code was dichotomized (response yes or no) and input into SPSS software (SPSS Inc, Chicago, IL) to calculate frequencies and cross tabulations.
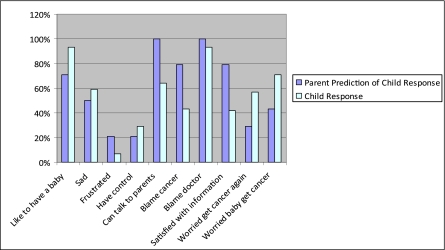
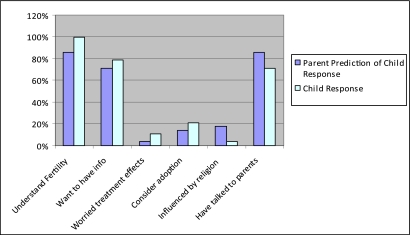
Results
In total, 14 parent-child pairs were interviewed (n = 28). In all but 1 case the mother was the parent who participated in the study. Mean age of the adolescent was 15.67, whereas mean age of the parent was 42.30. Seventy-one percent (10) of parents were married, 57% (8) were white, 79% (11) were Christian, 64% (9) had an associate’s degree or higher, and 50% (7) had a child with leukemia. Overall, incongruence was found among all parent-child pairs (Figs 2 and 3, Table 1).
FIGURE 2.
Comparison of parent-child responses to 10-item HRQoL instrument.
FIGURE 3.
Additional feedback not included on the HRQoL instrument.
Sixty-four percent (9 out of 14) of parents provided incongruent predictions on half or more of the 10 statements. Table 2 shows the characteristics of all parents. The largest difference between parents who were congruent versus incongruent was found in education, wherein the majority of parents (60% [8]) who were mostly congruent with their child’s responses had a bachelor’s degree, compared with 22% (3) who held a bachelor’s degree in the mostly incongruent group.
TABLE 2.
Characteristics of Parents With High Versus Low Incongruence
| Incongruent on 5 or More Predictions | Congruent on 5 or More Predictions | |
|---|---|---|
| Total parents, % | 64 (9/14) | 36 (5/14) |
| Female, % | 78 | 100 |
| Race | ||
| White, % | 67 | 60 |
| Hispanic, % | 11 | 20 |
| Other, % | 22 | 20 |
| Age (parent) | ||
| Mean ± SD | 47.56 ± 5.15 | 47.2 ± 5.76 |
| Range | 42–55 | 41–53 |
| Age (child) | ||
| Mean ± SD, y | 15.44 ± 1.7 | 15.80 ± 2.59 |
| Range, y | 12–18 | 13–18 |
| Insurance | ||
| Private, % | 78 | 80 |
| Public, % | 23 | 20 |
| Education | ||
| ≥Associate’s degree, % | 56 | 80 |
| Marital status | ||
| Married, % | 78 | 60 |
| Single/divorced, % | 22 | 0 |
| Widowed, % | 0 | 40 |
| Religion | ||
| Christian, % | 78 | 80 |
| Child’s diagnosis | ||
| Leukemia, % | 44 | 60 |
| Hodgkin’s lymphoma, % | 33 | 0 |
| Rhabdomyosarcoma, % | 11 | 20 |
| Brain tumor, % | 0 | 20 |
| Child on treatment, % | 67 | 80 |
| Treatment type | ||
| Chemotherapy, % | 100 | 100 |
| Radiation, % | 67 | 60 |
| Surgery, % | 11 | 20 |
| Child-reported health | ||
| Excellent or very good, % | 33 | 40 |
| Good, % | 56 | 40 |
| Fair, % | 11 | 20 |
This study was not powered to conduct multivariate analyses; therefore, the associations between parent and adolescent demographic characteristics and parent incongruence of half or more responses could not be reliably estimated. Cross tabulation was used to examine the interrelation between parents who were incongruent on half or more of the items and specific item responses.
Half of the parents who said their daughter did not want to know the risks to fertility from her cancer treatment were also incongruent on 5 or more statements. Seventy percent of parents (10) who believe that their daughter does not worry about having a baby in the future because she might get cancer again were also incongruent on 5 or more questions. Seventy-five percent of parents (11) who said their daughter does not worry about having a baby in the future because her baby might get cancer were incongruent on more than 5 questions. Seventy-five percent of parents (11) say they have talked to their daughter about fertility and she is satisfied with the information, whereas 40% (6) of adolescents say they have talked to their parent and they are satisfied. Of the sample, only 2 parents indicated they have not talked to their daughter about fertility, and these parents were also incongruent on 5 or more questions.
One statement (“I’ll be frustrated if I can’t have a baby”) showed a 64% (9) incongruence between parents’ predictions and adolescents’ responses. Here, approximately 30% (4) of parents said that their daughter would say she would be sad, not frustrated; however, 50% (7) of adolescents said they would be disappointed, not frustrated. The majority of parents who were incongruent on this question held an associate’s degree or higher, were Christian, had a child with leukemia, had a child that self-reported her health as good, and say they have talked with their daughter about fertility.
Two other statements showed a 57% (8) incongruence between parents’ predictions and adolescents’ responses. One statement was “If I cannot have a baby, I would blame my cancer,” wherein the majority of parents are married, are less than 50 years old, and have an associate’s degree or higher. The second statement was “I am worried about having a baby in the future because I might get cancer again,” wherein the majority of parents are divorced or single, are less than 50 years old, and have an associate’s degree or higher.
We accept the null hypothesis that adolescents have more reproductive concerns than their parents. We also accept the null hypothesis that congruence between parent and adolescent did not vary by age because there was found to be no difference between age groups.
Discussion
This study highlights the inaccuracies in parent-predicted responses of their daughters’ reproductive concerns. Two key issues regarding the reproductive concerns of adolescents and their parents’ perceptions and how this may impact HRQoL reporting are identified. First, creating, validating, and administering pediatric instruments must be done with pediatric patients for accuracy. Second, parents often underestimate their daughters’ concerns about future reproduction when impacted by a cancer diagnosis.
Some HRQoL instruments designed for and by adults are used in the pediatric and adolescent cancer setting.29–31 The large differences between children, adolescents, middle-aged adults, and older adults likely make the use of these instruments inappropriate and unreliable. Furthermore, in 2004 Pickard et al32 identified 16 quality of life and HRQoL instruments for pediatric oncology. In practice settings, it is not known how often parent proxies are used for HRQoL assessments of adolescent patients with cancer and especially not their reproductive concerns. Some studies exist that examine adolescents’ and their parents’ general fertility concerns and fertility preservation options; however, there is a large heterogeneity of results. For example, Burns et al33 found that the majority of adolescent patients with cancer and their parents thought about parenthood in the future and had a strong desire to know about fertility preservation options before beginning treatment. No statistical differences were found between groups.33 Alternatively, Oosterhuis et al24 assessed agreement within familial dyads regarding infertility risks of adolescent patients with cancer. Seven out of 12 questionnaire items showed a 10% or larger difference in responses between parents and adolescent.24 Last, Eiser and Morse34 conducted a meta-analysis and found congruence between parent and child reports on HRQoL physical domains but large incongruence for parent and child reports on HRQoL emotional and social domains.34 However there are occasions when parent-proxy reports of HRQoL domains are required because of young age, feeling too ill, known cognitive impairments, and refusal, among other factors.15 Child self-report should be sought whenever possible, and practitioners should document when a parent-proxy response has been made. Children as young as 5 have been shown to reliably report their HRQoL on assessments.35
Another key issue highlighted from the results is that parents often underestimated their daughters’ concerns about future reproduction when impacted by a cancer diagnosis. The few studies examining attitudes of adolescent patients with cancer toward fertility support this conclusion. Crawshaw and Sloper8 found that the majority of adolescents surveyed aged 13 to 21 who were receiving treatment of cancer reported having a strong desire to know immediately after diagnosis how their cancer treatment would impact their fertility. The majority of adolescents who had a known impairment to their fertility were most concerned about future partnering.8 Similar results have also indicated high informational needs of this population regarding treatment’s impact on fertility.9,24,36
There are various reasons why parents underestimated their daughter’s concerns about future reproduction. A focus on survival could overshadow the normative developmental experiences that adolescents with cancer still face. Chronically ill adolescents experience similar desires as their healthy peers and have been shown to deny their cancer diagnosis as an attempt to regain normalcy.37,38 However, this may not be recognized during a cancer crisis. Additionally, as seen in this study, there are discrepancies between parent and child reports on discussions about fertility. Many parents indicated they have talked to their daughter about fertility, whereas a smaller percentage of adolescents said they have spoken to their parents. This may be due to communication patterns regarding sex and reproduction, which may account for the underestimation. Adolescent females have been found to more frequently discuss physical aspects of puberty such as the menstrual cycle with their mothers, discuss refraining from sexual activity with their fathers, and discuss sexual intercourse with their friends.39 Race can also play a role because Hispanic and Asian mothers have been found to less likely talk with their daughters about sex.40 The high reproductive concerns of adolescent patients with cancer highlight the need for these items on HRQoL tools.
This study does have limitations. The small sample size and locations of recruitment reduce generalizability. Also, the population was quite homogenous because no non–English speaking families were included; the majority were white Christians with parents who held a bachelor’s degree. Only 29% (4) of adolescents were in the younger age range, which may also affect generalizability. The pilot nature of this study also requires that further testing be conducted with larger sample sizes before making recommendations. Additionally, further research is needed to explore the congruence of parent-proxy and adolescent reproductive concerns, particularly in ethnically, religiously, educationally, and age-diverse populations.
Conclusions
The use of this form of cognitive debriefing appears effective and useful for developing instruments within this population. Adolescent patients with cancer have strong reproductive concerns; however, this may not be captured on current HRQoL instruments and may be further neglected because of parents’ unawareness. Parent-proxy reports of adolescent reproductive concerns are not suitable for capturing specific emotions and feelings that are impacted by normative development, acceptance of a life-threatening illness, and long-term goals. Discussions should be encouraged with adolescent patients before beginning treatment regarding their concerns and values about parenting in the future. Additional discussions throughout the course of treatment and follow-up may be warranted to assess if concerns or values have changed.
Glossary
- HRQoL
health-related quality of life
Footnotes
Drs Quinn and Knapp, Ms Murphy, and Drs Sawczyn and Sender substantially contributed to the conception, design, acquisition of data, data analysis, and interpretation of results; drafted the article and revised it critically at all stages for important intellectual content; and approved this final version to be uploaded.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by the Oncofertility Consortium, funded by the National Institutes of Health through the NIH Roadmap for Medical Research, grants UL1DE19587 and UL1DE019587.Funded by the National Institutes of Health (NIH).
References
- 1.Li J, Thompson TD, Miller JW, Pollack LA, Stewart SL. Cancer incidence among children and adolescents in the United States, 2001-2003. Pediatrics 2008;121(6). Available at: www.pediatrics.org/cgi/content/full/121/6/e1470 [DOI] [PubMed]
- 2.International Classification of Childhood Cancer United States SEER Cancer Statistics Review 1975-2002. Bethesda, MD: National Cancer Institute; 2002 [Google Scholar]
- 3.Bahadur G. Fertility issues for cancer patients. Mol Cell Endocrinol. 2000;169(1-2):117–122 [DOI] [PubMed] [Google Scholar]
- 4.Padron OF, Sharma RK, Thomas AJ, Jr, Agarwal A. Effects of cancer on spermatozoa quality after cryopreservation: a 12-year experience. Fertil Steril. 1997;67(2):326–331 [DOI] [PubMed] [Google Scholar]
- 5.Drasga R, Einhorn L, Williams S, Patel D, Stevens E. Fertility after chemotherapy for testicular cancer. J Clin Oncol. 1983;1(3):179–183 [DOI] [PubMed] [Google Scholar]
- 6.Lee SJ, Schover LR, Partridge AH, et al. American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J Clin Oncol. 2006;24(18):2917–2931 [DOI] [PubMed] [Google Scholar]
- 7.Fallat ME, Hutter J; American Academy of Pediatrics Committee on Bioethics; American Academy of Pediatrics Section on Hematology/Oncology; American Academy of Pediatrics Section on Surgery. Preservation of fertility in pediatric and adolescent patients with cancer. Pediatrics 2008;121(5). Available at: www.pediatrics.org/cgi/content/full/121/5/e1461 [DOI] [PubMed]
- 8.Crawshaw M, Sloper P. A Qualitative Study of the Experiences of Teenagers and Young Adults When Faced With Possible or Actual Fertility Impairment Following Cancer Treatment. Executive Summary. York, UK: University of York; 2006 [Google Scholar]
- 9.Chapple A, Salinas M, Ziebland S, McPherson A, Macfarlane A. Fertility issues: the perceptions and experiences of young men recently diagnosed and treated for cancer. J Adolesc Health. 2007;40(1):69–75 [DOI] [PubMed] [Google Scholar]
- 10.Crawshaw MA, Glaser AW, Hale JP, Sloper P. Male and female experiences of having fertility matters raised alongside a cancer diagnosis during the teenage and young adult years. Eur J Cancer Care (Engl). 2009;18(4):381–390 [DOI] [PubMed] [Google Scholar]
- 11.Bleyer A, Albritton KH, Barr RD, Lewis IJ, Sender LS. Trailblazers in adolescent and young adult oncology. J Adolesc Young Adult Oncol. 2011;1(1):13–18 [DOI] [PubMed] [Google Scholar]
- 12.Varni JW, Burwinkle TM, Lane M. Health-related quality of life measurement in pediatric clinical practice: an appraisal and precept for future research and application. Health Qual Life Outcomes. 2005;3(34):1–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lewandowski AS, Toliver-Sokol M, Palermo TM. Evidence-based review of subjective pediatric sleep measures. J Pediatr Psychol. 2011;36(7):780–793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vitale MG, Levy DE, Johnson MG, et al. Assessment of quality of life in adolescent patients with orthopaedic problems: are adult measures appropriate? J Pediatr Orthop. 2001;21(5):622–628 [PubMed] [Google Scholar]
- 15.Palmer SN, Meeske KA, Katz ER, Burwinkle TM, Varni JW. The PedsQL Brain Tumor Module: initial reliability and validity. Pediatr Blood Cancer. 2007;49(3):287–293 [DOI] [PubMed] [Google Scholar]
- 16.Levi RB, Drotar D. Health-related quality of life in childhood cancer: discrepancy in parent-child reports. Int J Cancer Suppl. 1999;12:58–64 [DOI] [PubMed] [Google Scholar]
- 17.Strong P. The Ceremonial Order of the Clinic. London, UK: Routledge and Kegan Paul; 1979 [Google Scholar]
- 18.Perrin JM, MacLean WE, Perrin EC. Parental perceptions of health status and psychologic adjustment of children with asthma. Pediatrics. 1989;83(1):26–30 [PubMed] [Google Scholar]
- 19.Wenzel L, Dogan-Ates A, Habbal R, et al. Defining and measuring reproductive concerns of female cancer survivors. J Natl Cancer Inst Monogr. 2005;(34):94–98 [DOI] [PMC free article] [PubMed]
- 20.Jozefiak T, Larsson B, Wichstrøm L, Wallander J, Mattejat F. Quality of life as reported by children and parents: a comparison between students and child psychiatric outpatients. Health Qual Life Outcomes. 2010;8(1):136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Davis E, Davies B, Waters E, Priest N. The relationship between proxy reported health-related quality of life and parental distress: gender differences. Child Care Health Dev. 2008;34(6):830–837 [DOI] [PubMed] [Google Scholar]
- 22.Steinsbekk S, Jozefiak T, Ødegård R, Wichstrøm L. Impaired parent-reported quality of life in treatment-seeking children with obesity is mediated by high levels of psychopathology. Qual Life Res. 2009;18(9):1159–1167 [DOI] [PubMed] [Google Scholar]
- 23.Varni JW, Limbers CA, Burwinkle TM. Parent proxy-report of their children’s health-related quality of life: an analysis of 13,878 parents’ reliability and validity across age subgroups using the PedsQL 4.0 Generic Core Scales. Health Qual Life Outcomes. 2007;5(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Oosterhuis BE, Goodwin T, Kiernan M, Hudson MM, Dahl GV. Concerns about infertility risks among pediatric oncology patients and their parents. Pediatr Blood Cancer. 2008;50(1):85–89 [DOI] [PubMed] [Google Scholar]
- 25.Varni JW, Seid M, Rode CA. The PedsQL: measurement model for the pediatric quality of life inventory. Med Care. 1999;37(2):126–139 [DOI] [PubMed] [Google Scholar]
- 26.Woolley ME, Bowen GL, Bowen NK. The development and evaluation of procedures to assess child self-report item validity educational and psychological measurement. Educ Psychol Meas. 2006;66(4):687–700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dye JF, Schatz IM, Rosenberg BA, Coleman S. Constant comparison method: a kaleidoscope of data. Qual Rep. 2000;4(1/2):1–2 [Google Scholar]
- 28.Patton MQ. Qualitative Research and Evaluation Methods. Thousand Oaks, CA: Sage Publications; 2002 [Google Scholar]
- 29.Bradlyn AS, Harris CV, Warner JE, Ritchey AK, Zaboy K. An investigation of the validity of the quality of Well-Being Scale with pediatric oncology patients. Health Psychol. 1993;12(3):246–250 [DOI] [PubMed] [Google Scholar]
- 30.Sung L, Greenberg ML, Doyle JJ, et al. Construct validation of the Health Utilities Index and the Child Health Questionnaire in children undergoing cancer chemotherapy. Br J Cancer. 2003;88(8):1185–1190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fonseca M, Missotten P, Etienne A, Dupuis G, Lemetayer F, Spitz E. The impact of children’s illness perceptions on paediatric cancer patients’ quality of life. Psychooncology. 2010;19(suppl 2):126 [Google Scholar]
- 32.Pickard S, Topfer L-A, Feeny DH. A structured review of studies on health-related quality of life and economic evaluation in pediatric acute lymphoblastic leukemia. J Natl Cancer Inst Monogr. 2004;33:102–125 [DOI] [PubMed] [Google Scholar]
- 33.Burns KC, Boudreau C, Panepinto JA. Attitudes regarding fertility preservation in female adolescent cancer patients. J Pediatr Hematol Oncol. 2006;28(6):350–354 [DOI] [PubMed] [Google Scholar]
- 34.Eiser C, Morse R. Can parents rate their child’s health-related quality of life? Results of a systematic review. Qual Life Res. 2001;10(4):347–357 [DOI] [PubMed] [Google Scholar]
- 35.Varni JW, Limbers CA, Burwinkle TM. How young can children reliably and validly self-report their health-related quality of life? An analysis of 8,591 children across age subgroups with the PedsQL 4.0 Generic Core Scales. Health Qual Life Outcomes. 2007;5(1):1–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Edge B, Holmes D, Makin G. Sperm banking in adolescent cancer patients. Arch Dis Child. 2006;91(2):149–152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Butow P, Palmer S, Pai A, Goodenough B, Luckett T, King M. Review of adherence-related issues in adolescents and young adults with cancer. J Clin Oncol. 2010;28(32):4800–4809 [DOI] [PubMed] [Google Scholar]
- 38.Cavallo J. A conversation with Brad Zebrack, PhD, MSW, MPH: how to help young adults cope with cancer. ASCO Post. 2011;2(9). Available at: www.ascopost.com/articles/june-15-2011/a-conversation-withbrad-zebrack,-phd,-msw,-mph/. Accessed February 7, 2012 [Google Scholar]
- 39.DiIorio C, Kelley M, Hockenberry-Eaton M. Communication about sexual issues: mothers, fathers, and friends. J Adolesc Health. 1999;24(3):181–189 [DOI] [PubMed] [Google Scholar]
- 40.Meneses LM, Orrell-Valente JK, Guendelman SR, Oman D, Irwin CE, Jr. Racial/ethnic differences in mother-daughter communication about sex. J Adolesc Health. 2006;39(1):128–131 [DOI] [PubMed] [Google Scholar]