Abstract
OBJECTIVES:
To evaluate shifts across BMI categories and associated changes in cardiometabolic risk factors over 2.5 years in an ethnically diverse middle school sample.
METHODS:
As part of HEALTHY, a multisite school-based study designed to mitigate risk for type 2 diabetes, 3993 children participated in health screenings at the start of sixth and end of eighth grades. Assessments included anthropometric measures, blood pressure, and glucose, insulin, and lipids. Students were classified as underweight, healthy weight, overweight, obese, or severely obese. Mixed models controlling for school intervention status and covariates were used to evaluate shifts in BMI category over time and the relation between these shifts and changes in risk factors.
RESULTS:
At baseline, students averaged 11.3 (±0.6) years; 47.6% were boys, 59.6% were Hispanic, and 49.8% were overweight or obese. Shifts in BMI category over time were common. For example, 35.7% of youth who were overweight moved to the healthy weight range, but 13% in the healthy weight range became overweight. BMI shifts were not associated with school intervention condition, household education, or youth gender, race/ethnicity, pubertal status, or changes in height. Increases in BMI category were associated with worsening of cardiometabolic risk factors, and decreases were associated with improvements. Boys who increased BMI category were more vulnerable to negative risk factor changes than girls.
CONCLUSIONS:
There are substantial shifts across BMI categories during middle school that are associated with clinically meaningful changes in cardiometabolic risk factors. Programs to promote decreases in BMI and prevent increases are clearly warranted.
KEY WORDS: obesity, overweight, obesity trends, BMI, glucose, insulin, blood pressure, lipids
What’s Known on This Subject:
Changes in BMI category appear to be common in young children and are associated with cardiometabolic risk in cross-sectional studies. However, there are few longitudinal studies and little information from multiethnic samples of US middle school children.
What This Study Adds:
Findings demonstrate that shifts in BMI category are common in middle-school-aged children and associated with clinically meaningful changes in cardiometabolic risk factors. Programs to promote decreases in BMI, prevent increases, and moderate risk are indicated.
Childhood overweight and obesity have increased dramatically, with associated increases in morbidity, in particular, metabolic and cardiovascular risk factors. Thus, programs to prevent or moderate the development of obesity and minimize risk are a public health priority. HEALTHY1 was a 3-year school-based program designed to reduce risk factors for type 2 diabetes in middle-school youth. Results indicated that there were no differences between intervention and control schools in the primary outcome, the combined prevalence of child overweight and obesity, with overall decreases in prevalence of ∼4%. Intervention schools, however, had larger reductions in the prevalence of obesity, BMI z score, waist circumference, and fasting insulin levels.
The HEALTHY cohort provides a unique opportunity to examine longitudinal patterns of changes in category of BMI in a multiethnic, high-risk sample of US children and to examine the health consequences of these shifts in youth reaching puberty when risk increases. Results from longitudinal studies conducted in other countries generally have suggested moderate2 to strong3,4 stability of BMI and obesity during childhood, but these studies have focused on elementary school children, and there are few prospective studies of US middle school samples. Data from the National Heart, Lung, and Blood Institute Growth and Health Study of Black and White Girls5 documented an increase in the onset of overweight and obesity in girls from ages 9 to 12 years followed by stabilization. However, the data were collected in the 1990s, and boys were not included. In a more recent 2-year longitudinal study of 451 youth in the grades 4 through 6, children in the healthy weight range tended to gain weight, whereas obese youth tended to lose weight, although there were stable rates of overweight and obesity overall.6
With regard to changes in health risk, there are compelling cross-sectional data documenting an association between increased BMI and cardiometabolic risk factors,7–9 as well as findings that pediatric obesity intervention is associated with decreases in BMI and reductions in risk.10,11 Recent prospective findings from the Avon Longitudinal Study of Parents and Children (ALSPAC) in the United Kingdom12 have shown that BMI assessed in 9- to 12-year-old children (N = 5235) was significantly associated with cardiometabolic risk factors at 15 to 16 years, but few minority children were included.13 There is little information from community samples in the United States about changes in BMI category and accompanying health risks over time. Thus, herein we examine patterns of change in BMI categories and their impact on cardiometabolic risk factors in a large, ethnically diverse cohort.
Methods
Study Design
HEALTHY was a 3-year cluster-randomized, controlled primary prevention trial. Details of the HEALTHY protocol have been described.14 In brief, 42 US middle schools with at least 50% of students eligible for free or reduced-price lunch or belonging to a minority group were recruited by the 7 participating centers. The study was approved by the site institutional review boards, and parent consent and child assent were obtained. Schools were randomized by site to intervention or control conditions. All students were invited to participate in a health screening in fall 2006, and 57.6% of students agreed. Intervention schools were provided 2.5 years of a comprehensive program, which included changes to the school food environment and physical education classes and classroom-based education that incorporated behavior change activities. Activities were complemented by communication and social marketing strategies. Participation of control schools was limited to recruitment and data collection.
Data Collection
Methods for data collection were reported previously,14 and additional details are available as a supplement to the main outcome report.1 Students participated in standardized assessments at baseline (grade 6) and end of study (grade 8). Blood was drawn from fasted students to measure glucose, insulin, and lipids. Assays were conducted by the Northwest Lipid Metabolism and Diabetes Research Laboratories, University of Washington, Seattle.14 Height and weight were measured by trained, certified study staff by using the Prospective Enterprises PE-AIM-101 stadiometer and the SECA Corporation α 882 electronic scale. A Gulick tape was used measure waist circumference just above the iliac crest. Blood pressure was recorded 3 times by using an automated blood pressure monitor (Omron HEM-907 or HEM-907Xl, Vernon Hills, IL), and the mean of the second and third recordings was used for analysis. Pubertal status was self-reported by using the Pubertal Development Scale15 and converted to the pubertal stage groups outlined by Tanner.16 The scale was administered to boys and girls separately by trained study staff in a private area, with oral instructions provided from a written script.
Ethnicity and race were self-reported by students. Because participants frequently misunderstood the distinction between ethnicity and race, the information from the separate items was combined: anyone checking “Hispanic or Latino” ethnicity was classified as Hispanic; non-Hispanics choosing only “black or African American” race were classified as black; non-Hispanics choosing only “white” race were white; all other response categories were combined into “other.” A parent or guardian reported the highest level of household education and history of diabetes in first-degree blood relatives.
Statistical Methods
BMI percentile for age and gender was calculated by using Centers for Disease Control reference charts.17 Students with a BMI ≥5th percentile and <85th percentile were classified as healthy weight; the healthy weight range was then subdivided into 2 groups, BMI ≥5th percentile and <50th percentile and BMI ≥50th percentile and <85th percentile. Youth with BMI ≥85th but <95th percentile were classified as overweight, and those ≥95th but <99th percentile as obese. Students with BMI <5th percentile were classified as underweight, and those with BMI ≥99th percentile as severely obese.
We created 7 categories to examine BMI shifts from grades 6 through 8 (categories with small numbers were collapsed): (1) overweight to obese or severely obese; (2) healthy weight to overweight, obese, or severely obese; (3) stayed obese or severely obese; (4) stayed overweight; (5) stayed healthy weight; (6) overweight to healthy weight; and (7) obese or severely obese to overweight or healthy weight. Categories were collapsed further for modeling because of small cell sizes; specifically, the first 2 BMI categories collapsed into an “increased BMI” category, and the last 2 categories into a “decreased BMI” category. Finally, underweight students (n = 82; 2%) were excluded from modeling as shifting to the healthy weight range was not expected to be associated with increased risk.
Descriptive statistics including means, standard deviations, and percents were calculated for all variables. Next, we evaluated whether longitudinal shifts in BMI category differed by school intervention status, gender, race/ethnicity, sixth- and eighth-grade pubertal stage, and head-of-household education level by using separate generalized linear mixed models that took into account sources of variability within and between schools and controlled for baseline BMI percentiles. Change in height from grades 6 through 8 was evaluated as a potential confounder in all models that examined longitudinal changes in BMI category. Separate mixed models were also used to analyze associations between shifts in BMI and changes in cardiometabolic parameters. Baseline values of the risk factors of interest, school intervention status, gender, race/ethnicity, sixth- and eighth-grade pubertal stage, and head-of-household education level were included as covariates. All models tested for BMI shifts and covariates as main effects and for the interaction between BMI shifts and covariates when covariates were significant. Because gender was significant as a main effect across models, subgroup analysis was performed by gender. To evaluate the impact of specific shifts in BMI category, we conducted pairwise comparisons between each of the BMI shift categories. We considered P values ≤.001 to be statistically significant due to multiple comparisons. SAS 9.2 statistical software (SAS Institute Inc, Cary, NC) was used for analyses.
Results
Of the 4603 students in the HEALTHY cohort, 4363 (95%) completed assessments at baseline and end of study. Of these, 370 children from the heterogeneous “other” race/ethnicity category were excluded; they did not differ from those included on school any measured parameter (data not shown). Baseline characteristics for the study sample (n = 3993) are presented in Table 1. Students averaged 11.3 years, and 47.6% were boys. More than half the sample was Hispanic (59.6%), and head-of-household level of education was high school graduate or less in 53.6% of families. Nearly half of the youth (49.8%) were overweight or obese.
TABLE 1.
Sixth-Grade Student Characteristics
| Overalla (n = 3993) | Boys (n = 1902) | Girls (n = 2091) | |
|---|---|---|---|
| Age, y, mean (SD) | 11.3 (0.6) | 11.3 (0.6) | 11.3 (0.5) |
| Race/ethnicity, % | |||
| Hispanic | 59.6 | 59.1 | 60.0 |
| Non-Hispanic black | 19.3 | 18.3 | 20.1 |
| Non-Hispanic white | 21.2 | 22.6 | 19.9 |
| Family history of diabetes, %b | 17.5 | 16.9 | 18.2 |
| Pubertal stage, %c | |||
| Stage 1 | 11.0 | 16.8 | 5.9 |
| Stage 2 | 26.5 | 41.1 | 13.4 |
| Stage 3 | 40.4 | 37.4 | 43.1 |
| Stage 4 | 20.8 | 4.5 | 35.3 |
| Stage 5 | 1.3 | 0.2 | 2.3 |
| Highest education level attained by head of household, % | |||
| Less than high school | 13.0 | 12.7 | 13.4 |
| Some high school | 15.0 | 14.6 | 15.3 |
| High school graduate | 25.6 | 24.8 | 26.4 |
| Some college or specialized training | 27.8 | 27.7 | 27.8 |
| College or university graduate | 12.9 | 14.3 | 11.6 |
| Postgraduate training or degree | 5.7 | 5.9 | 5.6 |
| BMI, mean (SD) | 22.3 (5.4) | 22.4 (5.5) | 22.2 (5.3) |
| BMI percentile ≥85th, % | 49.8 | 52.9 | 46.9 |
| Glucose, mg/dL, mean (SD) | 93.6 (6.5) | 94.5 (6.5) | 92.8 (6.4) |
| Insulin, U/mL, mean (SD) | 13.2 (11.5) | 12.2 (12.2) | 14.2 (10.8) |
| SBP, mm Hg, mean (SD) | 107.4 (10.1) | 108.1 (10.2) | 106.8 (9.9) |
| DBP, mm Hg, mean (SD) | 63.7 (8.6) | 63.7 (8.7) | 63.8 (8.6) |
| HDL, mg/dL, mean (SD) | 52.4 (12.2) | 52.9 (12.4) | 52.0 (12.1) |
| LDL, mg/dL, mean (SD) | 87.0 (23.2) | 89.0 (23.9) | 85.3 (22.5) |
| Cholesterol, mg/dL, mean (SD) | 157.3 (27.5) | 159.4 (28.4) | 155.4 (26.5) |
| Triglycerides, mg/dL, mean (SD) | 89.5 (53.2) | 88.1 (51.9) | 90.8 (54.3) |
| Waist circumference, cm, mean (SD) | 75.9 (14.5) | 76.2 (15.4) | 75.7 (13.7) |
All P values for the comparisons between intervention and control schools at baseline (sixth grade) were >.20.14
A parent or guardian reported history of type 2 diabetes in first-degree blood relatives.
Based on 3712 (n = 1747 boys; n = 1965 girls) self-reports.
Longitudinal Shifts in BMI Category
Longitudinal changes in BMI categories are shown in Table 2. Of the 1.55% (n = 62) of sixth-graders who were underweight, only 0.6% (n = 23) remained underweight at the end of eighth grade. Most sixth-grade youth in the healthy range (n = 1943) remained there at the end of eighth grade (n = 1770; 91.1%). However, when the healthy range was divided into 2 groups, patterns of change emerged. Virtually none of the youth (n = 3; 0.0008%) who started with a BMI ≥5th to <50th percentile became overweight or obese during the study, but 27.8% shifted to the upper half of the healthy weight range. Of sixth graders with a BMI percentile in the upper range of healthy (≥50th to <85th), 13.0% (n = 150) became overweight or obese. There was a notable amount of shifting among students who were overweight or obese in sixth grade. Among overweight sixth-grade youth (n = 778), 35.7% (n = 278) moved to the healthy range, 12.7% (n = 99) became obese or severely obese, and 51.5% (n = 401) remained overweight. Among the 947 youth who were obese, 31.9% (n = 303) improved BMI category, whereas 61.9% (n = 586) remained obese and 6.1% (n = 58) became severely obese. Of the 263 sixth-grade youth who were severely obese, 76.1% (n = 200) stayed severely obese, but 23.9% (n = 63) moved to the obese or overweight category. BMI shifts were not associated with school intervention status or any of the included covariates (data not shown). Furthermore, BMI shifts were not explained by differential increases in height across categories (overall mean height change from sixth to eighth grade was +11.3 ± 5.8 cm).
TABLE 2.
Categories of BMI Percentile (Frequency and Percent) in Sixth and Eighth Grades
| Sixth Grade | Eighth Grade | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Underweight | Healthy (Lower Range) | Healthy (Upper Range) | Overweight | Obese | Severely Obese | Total | |||
| <5 (%) | 5–49 (%) | 50–84 (%) | 85–94 (%) | 95–98 (%) | 99+ (%) | ||||
| Underweight | <5 | 23 (37.1) | 39 (62.9) | 0 (—) | 0 (—) | 0 (—) | 0 (—) | 62 | |
| Healthy (lower range) | 5–49 | 19 (2.4) | 553 (69.4) | 222 (27.8) | 3 (0.4) | 0 (—) | 0 (—) | 797 | |
| Healthy (upper range) | 50–84 | 1 (0.1) | 179 (15.6) | 816 (71.2) | 137 (11.9) | 13 (1.1) | 0 (—) | 1146 | |
| Overweight | 85–94 | 0 (—) | 10 (1.3) | 268 (34.4) | 401 (51.5) | 98 (12.6) | 1 (0.1) | 778 | |
| Obese | 95–98 | 0 (—) | 3 (0.3) | 43 (4.5) | 257 (27.1) | 586 (61.9) | 58 (6.1) | 947 | |
| Severely Obese | 99+ | 0 (—) | 0 (—) | 0 (—) | 5 (1.9) | 58 (22.0) | 200 (76.1) | 263 | |
| Total | 43 | 784 | 1349 | 803 | 755 | 259 | 3993 | ||
Shifts in BMI and Changes in Risk Factors
Table 3 presents longitudinal changes in risk factors across BMI categories. Results of the mixed models that included school intervention status and all covariates documented an overall association between shift in BMI and changes in glucose, insulin, systolic (SBP) and diastolic blood pressure (DBP), high-density lipoprotein (HDL), low-density lipoprotein (LDL), total cholesterol, triglycerides, and waist circumference (all Ps < .001). Most pairwise comparisons documented that increasing BMI category was associated with increases in insulin, SBP, DBP, triglycerides and waist circumference; decreases in HDL; and smaller decreases in LDL and total cholesterol compared with staying in the same or decreasing BMI category. Conversely, most pairwise comparisons documented that decreasing BMI category was associated with improvements in risk factors in comparison with staying the same or increasing BMI category. Staying obese or severely obese was associated with unfavorable changes in virtually all health measures relative to staying in the healthy range or decreasing BMI category. Staying overweight was associated with unfavorable changes relative to staying healthy weight or decreasing BMI category for insulin, SBP, HDL, LDL, triglycerides, and waist circumference.
TABLE 3.
Mean (SD) for Sixth Grade, Eighth Grade, and Change (Δ) in Cardiometabolic Outcomes by Shift in BMI Categorya
| Overweight to Obese+ (N = 99) | Healthy to Overweight/ Obese+ (N = 153) | Stayed Obese+ (N = 902) | Stayed Overweight (N = 401) | Stayed Healthy (N = 1770) | Overweight to Healthy (N = 278) | Obese+ to Overweight/Healthy (N = 308) | Pairwise Comparisonsb of Δc in Cardiometabolic Outcomes | |
|---|---|---|---|---|---|---|---|---|
| Increased Group (I) | OB | OV | HY | Decreased Group (D) | ||||
| Glucose, mg/dL | ||||||||
| 6th | 92.7 (6.4) | 92.3 (5.7) | 94.5 (6.8) | 93.4 (6.2) | 93.1 (6.5) | 93.7 (6.7) | 94.6 (5.9) | OB vs HY; OB vs D; |
| 8th | 95.1 (8.4) | 93.0 (8.2) | 95.8 (8.3) | 93.7 (7.6) | 93.4 (8.7) | 92.4 (7.9) | 93.5 (7.7) | |
| Δ | 2.4 (8.6) | 0.7 (7.2) | 1.3 (7.4) | 0.2 (7.9) | 0.2 (8.9) | –1.3 (7.6) | –1.2 (7.8) | |
| Insulin, µU/mL | ||||||||
| 6th | 12.8 (6.7) | 9.9 (4.4) | 23.2 (16.9) | 12.9 (7.5) | 8.3 (5.3) | 12.6 (8.7) | 17.3 (9.8) | I vs OB; I vs HY; I vs D; OB vs OV; OB vs HY; OB vs D; OV vs HY; OV vs D |
| 8th | 22.3 (12.1) | 17.4 (8.6) | 29.7 (21.7) | 17.3 (8.7) | 12.0 (8.2) | 12.8 (6.0) | 14.9 (9.3) | |
| Δ | 9.5 (10.9) | 7.5 (8.8) | 6.5 (21.6) | 4.4 (9.2) | 3.6 (9.0) | 0.2 (9.7) | –2.3 (11.1) | |
| SBP, mm Hg | ||||||||
| 6th | 106.7 (10.2) | 106.2 (9.2) | 110.8 (10.6) | 106.2 (9.3) | 105.8 (9.8) | 106.6 (9.2) | 111.3 (9.3) | I vs HY; I vs D; OB vs HY; OB vs D; OV vs HY; OV vs D |
| 8th | 115.1 (11.8) | 111.9 (10.3) | 115.0 (11.3) | 112.3 (9.5) | 108.4 (9.6) | 110.1 (10.0) | 113.6 (10.4) | |
| Δ | 8.4 (12.0) | 5.7 (10.1) | 4.2 (11.9) | 6.1 (10.2) | 2.6 (10.7) | 3.5 (10.8) | 2.3 (9.3) | |
| DBP, mm Hg | ||||||||
| 6th | 64.6 (8.1) | 62.5 (8.4) | 67.9 (8.5) | 63.4 (7.6) | 61.5 (8.4) | 63.1 (7.6) | 66.6 (7.8) | I vs HY; I vs D; OB vs OV; OB vs HY; OB vs D; OV vs HY |
| 8th | 68.3 (8.4) | 64.7 (6.9) | 68.5 (8.3) | 64.9 (7.5) | 62.8 (7.2) | 63.1 (7.5) | 64.4 (7.5) | |
| Δ | 3.7 (10.1) | 2.3 (9.1) | 0.6 (9.7) | 1.5 (8.5) | 1.3 (9.4) | –0.0 (9.1) | –2.2 (7.9) | |
| HDL, mg/dL | ||||||||
| 6th | 50.5 (10.8) | 53.7 (13.2) | 45.4 (9.9) | 50.7 (11.0) | 57.0 (11.9) | 51.8 (11.0) | 47.0 (9.4) | I vs OV; I vs HY; I vs D; OB vs HY; OB vs D; OV vs D; HY vs D |
| 8th | 46.2 (9.4) | 49.7 (13.6) | 44.4 (10.4) | 49.8 (10.8) | 55.0 (12.1) | 54.5 (11.7) | 50.9 (10.9) | |
| Δ | –4.3 (8.7) | –4.0 (9.4) | –1.0 (8.0) | –0.9 (9.0) | –2.0 (9.5) | 2.7 (9.5) | 3.8 (8.3) | |
| LDL, mg/dL | ||||||||
| 6th | 88.5 (23.1) | 87.4 (25.1) | 92.6 (25.1) | 89.1 (23.4) | 82.6 (20.7) | 89.9 (25.2) | 91.1 (23.3) | I vs HY; I vs D; OB vs HY; OB vs D; OV vs D; HY vs D |
| 8th | 85.9 (24.3) | 85.7 (25.7) | 87.1 (24.2) | 82.6 (21.2) | 76.1 (20.2) | 78.4 (24.6) | 76.8 (20.6) | |
| Δ | –2.6 (18.0) | –1.7 (17.6) | –5.5 (18.3) | –6.5 (18.4) | –6.5 (15.2) | –11.5 (19.1) | –14.2 (17.5) | |
| Chol, mg/dL | ||||||||
| 6th | 156.6 (27.9) | 157.8 (31.6) | 161.5 (30.0) | 158.3 (28.1) | 153.9 (24.7) | 161.0 (28.8) | 159.5 (28.6) | I vs D; OB vs D; OV vs D; HY vs D |
| 8th | 150.9 (30.6) | 154.2 (30.8) | 153.0 (28.7) | 149.8 (25.5) | 145.3 (24.8) | 147.5 (28.5) | 142.3 (24.9) | |
| Δ | –5.6 (22.1) | –3.6 (22.7) | –8.5 (22.5) | –8.5(22.3) | –8.6 (19.3) | –13.5 (23.5) | –17.2 (22.1) | |
| Trig, mg/dL | ||||||||
| 6th | 87.7 (46.2) | 83.5 (39.8) | 118.5 (65.5) | 93.7 (66.9) | 71.4 (32.0) | 96.1 (51.9) | 107.3 (58.9) | I vs HY; I vs D; OB vs HY; OB vs D; OV vs D; HY vs D |
| 8th | 94.0 (49.9) | 94.0 (55.0) | 108.2 (66.2) | 87.2 (45.3) | 71.2 (30.7) | 72.9 (31.3) | 72.9 (34.5) | |
| Δ | 6.3 (40.4) | 10.4 (50.2) | –10.3 (60.6) | –6.4 (61.7) | –0.2 (32.8) | –23.2 (44.6) | –34.3 (49.8) | |
| Waist, cm | ||||||||
| 6th | 79.1 (5.5) | 69.9 (5.6) | 95.6 (10.6) | 77.4 (5.6) | 64.8 (5.6) | 76.7 (5.6) | 87.1 (7.0) | I vs OV; I vs HY; I vs D; OB vs OV; OB vs HY; OB vs D; OV vs HY; OV vs D; HY vs D |
| 8th | 91.3 (6.3) | 81.7 (6.4) | 101.9 (11.6) | 82.6 (5.9) | 70.3 (5.3) | 75.6 (4.9) | 82.9 (6.1) | |
| Δ | 12.2 (6.0) | 11.8 (5.7) | 6.3 (7.3) | 5.2 (4.9) | 5.5 (4.4) | –1.1 (4.7) | –4.2 (7.0) | |
Chol, cholesterol; Trig, triglycerides.
Underweight youth in sixth or eighth grade were excluded (N = 82); Obese+ includes obese and severely obese youth.
We conducted 10 pairwise comparisons across BMI categories: 1. Increased versus Stayed Obese+ (I versus OB); 2. Increased versus Stayed Overweight (I versus OV); 3. Increased versus Stayed Healthy (I versus HY); 4. Increased versus Decreased (I versus D); 5. Stayed Obese+ versus Stayed Overweight (OB versus OV); 6. Stayed Obese+ versus Stayed Healthy (OB versus HY); 7. Stayed Obese+ versus Decreased (OB versus D); 8. Stayed Overweight versus Stayed Healthy (OV versus HY); 9. Stayed Overweight versus Decreased (OV versus D); and, 10. Stayed Healthy versus Decreased (HY versus D).
Statistical significance is P < .001 in a model that adjusts for the sixth-grade value of the cardiometabolic parameter, school intervention status, gender, race/ethnicity, sixth-grade pubertal stage, eighth-grade pubertal stage, and highest level of household education at baseline.
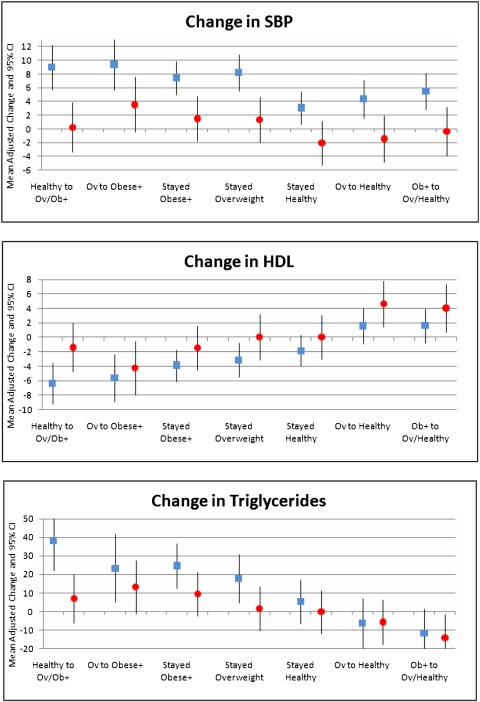
Change in BMI Category and Risk Factors by Gender
Changes in cardiometabolic parameters varied significantly by gender for all parameters except DBP (P = .0067); changes in insulin were borderline significant (P = .001). However, differences were small, and no meaningful patterns were identified except for changes in SBP, HDL, and triglycerides (Ps ≤ .0001), as shown in Fig 1. Boys had greater increases in SBP across BMI categories and greater decreases in HDL than girls, and there was an interaction between BMI shift and gender with triglyceride change (P < .0001). Gender differences in lipids over time were not explained by differential changes in waist circumference. Specifically, waist circumference increased by 4.59 cm (SD = 6.7) in boys and 5.13 cm (SD = 6.5) in girls, P = .0049.
FIGURE 1.
Changes (95% CI) in SBP, HDL, and triglycerides in boys and girls as a function of BMI category shifts from sixth grade to eighth grade. Boys are denoted by squares in figures and girls by circles. Ov, overweight; Ob+ or Obese +, obese and severely obese.
Discussion
There was a striking amount of shifting across BMI categories during the middle school years. Shifts in BMI category were not related to school intervention status, gender, race/ethnicity, baseline or end of study pubertal status, or head-of-household education. Furthermore, shifts in BMI were not explained by changes in height in this group of children studied during the pubertal transition. Of particular interest, more than one-third of overweight sixth-graders shifted to the healthy weight range, and nearly one-third of obese sixth-graders shifted to a lower BMI category by the end of eighth grade. Conversely, of youth who were in the lower end of the healthy range in sixth grade, more than one-quarter moved to the upper end of the healthy range. Similarly, of youth who were in the upper end of the healthy range or in the overweight category in the sixth grade, more than one-quarter increased BMI category.
Sizeable shifts in BMI category in children during childhood have been noted in studies of younger children and those outside the United States.2–4 The ALSPAC2 followed more than 6000 children in the United Kingdom from ages 7 to 11 years and documented shifts in this younger cohort that were similar to those observed in the current study. In a U.S. study of 451 African American and white rural children who were in the fourth through sixth grade at baseline and followed over 28 months,6 rates of overweight and obesity were stable, but rates of incidence and remission of obesity and overweight were approximately equal. Findings from the current investigation, however, significantly extend those of previous studies. Given the substantial racial/ethnic disparities in US rates of pediatric obesity,18 it is crucial to determine whether shifts in BMI are seen across ethnic minority groups. The HEALTHY sample includes large numbers of Hispanic as well as African American and white youth, and thus the current study provides evidence that shifts in BMI category occur across racial/ethnic groups.
The present investigation also documents that BMI shifts are associated with significant changes in cardiometabolic risk factors after adjustment for school intervention status, race/ethnicity, pubertal stage in sixth and eighth grade, and household education. The magnitude of observed changes is similar to those reported in pediatric weight management programs. For example, Savoye et al11 followed an ethnically diverse inner-city group of 209 obese children and adolescents who participated in a yearlong family-based weight control program or a usual care control group and were evaluated 1 year later. Intervention leading to modest weight decreases −2.8 kg/m2) was associated with decreases in total cholesterol, LDL cholesterol, and fasting insulin of −8.0 mg/dL, −4.4 mg/DL, and −4.7 uIU/mL, respectively. Changes of comparable magnitude were observed as a function of decreasing BMI category in HEALTHY youth (−17.2 mg/dL, −14.2 mg/dL, and −2.3 uU/mL for total cholesterol, LDL, and fasting insulin, respectively).
Other research suggests that the observed changes are clinically meaningful. Cross-sectional studies in youth9,19 have documented a strong relation between BMI and cardiometabolic risk. For example, Weiss et al9 documented that each element of the metabolic syndrome is exacerbated with increasing obesity. Similarly, prospective studies have documented a strong linear relationship between BMI and metabolic risk factors in childhood and adverse adult outcomes, including metabolic syndrome20 and coronary heart disease.21,22 In summary, available research findings, although not directly comparable to current data, suggest that the observed shifts in cardiometabolic risk are clinically significant.
Consistent with previous findings,12 the current results also demonstrate convincingly that staying obese or severely obese is associated with significant risk. For example, youth who remained obese or severely obese had significant increases in fasting insulin, with eighth-grade levels of 29.7 uU/mL (insulin levels of ≥30 uU/mL have been used to define elevated risk23), whereas obese or severely obese youth who decreased BMI had significant decreases in fasting insulin in comparison with those who remained obese or severely obese (average eighth-grade fasting insulin was 14.0 uU/mL). Similarly, youth with stable obesity had increases in waist circumference of 5.5 cm compared with decreases of 4.2 cm for youth who were obese or severely obese in the sixth grade but decreased to the healthy weight range. Finally, staying in the healthy weight range over time was associated with the most favorable levels across risk factors.
Changes in risk factors varied as a function of gender such that boys had greater increases in SBP and greater decreases in HDL than girls. Furthermore, boys and girls had different patterns of triglyceride changes, with boys tending to have more unfavorable changes in response to increases in BMI and girls benefitting more from decreases in BMI. These findings echo those observed in ALSPAC,12 which also documented that BMI changes were associated with more adverse risk factor changes in boys than in girls. Thus, boys may be particularly vulnerable to the negative cardiometabolic consequences of obesity.
The current study has significant strengths including the large, multiethnic sample from across the United States and assessments collected by trained, certified staff by using standardized procedures. Nevertheless, there also are limitations. All children participated in a study designed to mitigate risk for type 2 diabetes. Thus, the schools and youth who participated may not be representative of all high-risk US schools or students. All youth participated in health screenings and parents were given reports about child health. Consequently, observed decreases in BMI category may reflect greater awareness of the importance of health behavior among overweight or obese participants and their family members. Next, we used BMI as a proxy for adiposity. However, other research has shown that the association between BMI and cardiovascular risk factors is similar to that between directly assessed fat mass and risk factors,12 indicating the validity of BMI as an index of body fat.
In summary, results document considerable mutability in BMI categories during the middle school years, with clinically meaningful changes in cardiometabolic risk. The shifts in BMI and associated changes in risk were not associated with school intervention status and were robust to adjustment for salient demographic parameters and potential confounders. Thus, there is compelling evidence for the relevance of universal obesity prevention efforts that target middle-school-aged children across all BMI categories to enhance downward shifts in BMI category for overweight and obese children and mitigate increases in BMI category among children in the healthy weight range.
Acknowledgments
The following individuals and institutions constitute the HEALTHY Study Group (* indicates principal investigator or director). Study Chair: Children’s Hospital Los Angeles: F.R. Kaufman. Field Centers: Baylor College of Medicine: T. Baranowski,* L. Adams, J. Baranowski, A. Canada, K.T. Carter, K.W. Cullen, M.H. Dobbins, R. Jago, A. Oceguera, A.X. Rodriguez, C. Speich, L.T. Tatum, D. Thompson, M.A. White, C.G. Williams; Oregon Health & Science University: L. Goldberg,* D. Cusimano, L. DeBar, D. Elliot, H.M. Grund, S. McCormick, E. Moe, J.B. Roullet, D. Stadler; Temple University: G. Foster* (Steering Committee Chair), J. Brown, B. Creighton, M. Faith, E.G. Ford, H. Glick, S. Kumanyika, J. Nachmani, L. Rosen, S. Sherman, S. Solomon, A. Virus, S. Volpe, S. Willi; University of California at Irvine: D. Cooper,* S. Bassin, S. Bruecker, D. Ford, P. Galassetti, S. Greenfield, J. Hartstein, M. Krause, N. Opgrand, Y. Rodriguez, M. Schneider; University of North Carolina at Chapel Hill: J. Harrell,* A. Anderson, T. Blackshear, J. Buse, J. Caveness, A. Gerstel, C. Giles, W. Hall, A. Jessup, P. Kennel, R. McMurray, A-M. Siega-Riz, M. Smith, A. Steckler, A. Zeveloff; University of Pittsburgh: M.D. Marcus,* M. Carter, S. Clayton, B. Gillis, K. Hindes, J. Jakicic, R. Meehan, R. Noll, J. Vanucci, E. Venditti; University of Texas Health Science Center at San Antonio: R. Treviño,* A. Garcia, D. Hale, A. Hernandez, I. Hernandez, C. Mobley, T. Murray, J. Stavinoha, K. Surapiboonchai, Z. Yin. Coordinating Center: George Washington University: K. Hirst,* K. Drews, S. Edelstein, L. El ghormli, S. Firrell, M. Huang, P. Kolinjivadi, S. Mazzuto, T. Pham, A. Wheeler. Project Office: National Institute of Diabetes and Digestive and Kidney Diseases: B. Linder,* C. Hunter, M. Staten. Central Biochemistry Laboratory: University of Washington Northwest Lipid Metabolism and Diabetes Research Laboratories: S.M. Marcovina.*
HEALTHY intervention materials are available for download at http://www.healthystudy.org. We thank the administration, faculty, staff, students, and their families at the middle schools and school districts that participated in the HEALTHY study.
Glossary
- ALSPAC
Avon Longitudinal Study of Parents and Children
- DBP
diastolic blood pressure
- HDL
high-density lipoprotein
- LDL
low-density lipoprotein
- SBP
systolic blood pressure
Footnotes
All authors meet the 3 authorship criteria: all have contributed substantially to the conception and design, acquisition of data, or analysis and interpretation of data; all have critically revised the article for important intellectual content; and all have approved the final version to be published.
This trial has been registered at www.clinicaltrials.gov (identifier NCT00458029).
FINANCIAL DISCLOSURE: Dr Marcus is on the Scientific Advisory Board for United Health Group; Dr Foster is on the Scientific Advisory Boards for United Health Group, NutriSystem, and Con Agra Foods; the other authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: This work was completed with funding from National Institute of Diabetes and Digestive and Kidney Diseases/National Institutes of Health grants U01-DK61230, U01-DK61249, U01-DK61231, and U01-DK61223, with additional support from the American Diabetes Association. Funded by the National Institutes of Health (NIH).
References
- 1.Foster GD, Linder B, Baranowski T, et al. HEALTHY Study Group . A school-based intervention for diabetes risk reduction. N Engl J Med. 2010;363(5):443–453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wright CM, Emmett PM, Ness AR, Reilly JJ, Sherriff A. Tracking of obesity and body fatness through mid-childhood. Arch Dis Child. 2010;95(8):612–617 [DOI] [PubMed] [Google Scholar]
- 3.Hesketh K, Wake M, Waters E, Carlin J, Crawford D. Stability of body mass index in Australian children: a prospective cohort study across the middle childhood years. Public Health Nutr. 2004;7(2):303–309 [DOI] [PubMed] [Google Scholar]
- 4.Wardle J, Brodersen NH, Cole TJ, Jarvis MJ, Boniface DR. Development of adiposity in adolescence: five year longitudinal study of an ethnically and socioeconomically diverse sample of young people in Britain. BMJ. 2006;332(7550):1130–1135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kimm SY, Barton BA, Obarzanek E, et al. NHLBI Growth and Health Study . Obesity development during adolescence in a biracial cohort: the NHLBI Growth and Health Study. Pediatrics. 2002;110(5). Available at: www.pediatrics.org/cgi/content/full/110/5/e54 [DOI] [PubMed] [Google Scholar]
- 6.Williamson DA, Han H, Johnson WD, Stewart TM, Harsha DW. Longitudinal study of body weight changes in children: who is gaining and who is losing weight. Obesity (Silver Spring). 2011;19(3):667–670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marcus MD, Baranowski T, DeBar LL, et al. Severe obesity and selected risk factors in a sixth grade multiracial cohort: the HEALTHY study. J Adolesc Health. 2010;47(6):604–607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baranowski T, Cooper DM, Harrell J, et al. STOPP-T2D Prevention Study Group . Presence of diabetes risk factors in a large U.S. eighth-grade cohort. Diabetes Care. 2006;29(2):212–217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weiss R, Dziura J, Burgert TS, et al. Obesity and the metabolic syndrome in children and adolescents. N Engl J Med. 2004;350(23):2362–2374 [DOI] [PubMed] [Google Scholar]
- 10.Reinehr T, de Sousa G, Toschke AM, Andler W. Long-term follow-up of cardiovascular disease risk factors in children after an obesity intervention. Am J Clin Nutr. 2006;84(3):490–496 [DOI] [PubMed] [Google Scholar]
- 11.Savoye M, Nowicka P, Shaw M, et al. Long-term results of an obesity program in an ethnically diverse pediatric population. Pediatrics. 2011;127(3):402–410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lawlor DA, Benfield L, Logue J, et al. Association between general and central adiposity in childhood, and change in these, with cardiovascular risk factors in adolescence: prospective cohort study. BMJ. 2010;341:c6224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Golding J, Pembrey M, Jones R, ALSPAC Study Team . ALSPAC—the Avon Longitudinal Study of Parents and Children. I. Study methodology. Paediatr Perinat Epidemiol. 2001;15(1):74–87 [DOI] [PubMed] [Google Scholar]
- 14.Hirst K, Baranowski T, DeBar L, et al. HEALTHY Study Group . HEALTHY study rationale, design and methods: moderating risk of type 2 diabetes in multi-ethnic middle school students. Int J Obes (Lond). 2009;33(suppl 4):S4–S20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Robertson EB, Skinner ML, Love MM, et al. The Pubertal Development Scale: a rural and suburban comparison. J Early Adolesc. 1992;12(2):174–186 [Google Scholar]
- 16.Carskadon MA, Acebo C. A self-administered rating scale for pubertal development. J Adolesc Health. 1993;14(3):190–195 [DOI] [PubMed] [Google Scholar]
- 17.Centers for Disease Control National Center for Health Statistics. 2000 CDC growth charts for the United States. Available at: www.cdc.gov/growthcharts. Accessed February 17, 2004
- 18.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA. 2010;303(3):242–249 [DOI] [PubMed] [Google Scholar]
- 19.Freedman DS, Katzmarzyk PT, Dietz WH, Srinivasan SR, Berenson GS. Relation of body mass index and skinfold thicknesses to cardiovascular disease risk factors in children: the Bogalusa Heart Study. Am J Clin Nutr. 2009;90(1):210–216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sun SS, Liang R, Huang TT, et al. Childhood obesity predicts adult metabolic syndrome: the Fels Longitudinal Study. J Pediatr. 2008;152(2):191–200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baker JL, Olsen LW, Sørensen TI. Childhood body-mass index and the risk of coronary heart disease in adulthood. N Engl J Med. 2007;357(23):2329–2337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Freedman DS, Khan LK, Dietz WH, Srinivasan SR, Berenson GS. Relationship of childhood obesity to coronary heart disease risk factors in adulthood: the Bogalusa Heart Study. Pediatrics. 2001;108(3):712–718 [DOI] [PubMed] [Google Scholar]
- 23.Viner RM, Segal TY, Lichtarowicz-Krynska E, Hindmarsh P. Prevalence of the insulin resistance syndrome in obesity. Arch Dis Child. 2005;90(1):10–14 [DOI] [PMC free article] [PubMed] [Google Scholar]