Abstract
OBJECTIVE:
To test the effect on diabetes management outcomes of a low-intensity, clinic-integrated behavioral intervention for families of youth with type 1 diabetes.
METHODS:
Families (n = 390) obtaining care for type 1 diabetes participated in a 2-year randomized clinical trial of a clinic-integrated behavioral intervention designed to improve family diabetes management practices. Measurement of hemoglobin A1c, the primary outcome, was obtained at each clinic visit and analyzed centrally. Blood glucose meter data were downloaded at each visit. Adherence was assessed by using a semistructured interview at baseline, mid-study, and follow-up. Analyses included 2-sample t tests at predefined time intervals and mixed-effect linear-quadratic models to assess for difference in change in outcomes across the study duration.
RESULTS:
A significant overall intervention effect on change in glycemic control from baseline was observed at the 24-month interval (P = .03). The mixed-effect model showed a significant intervention by age interaction (P < .001). Among participants aged 12 to 14, a significant effect on glycemic control was observed (P = .009 for change from baseline to 24-month interval; P = .035 for mixed-effect model across study duration), but there was no effect among those aged 9 to 11. There was no intervention effect on child or parent report of adherence; however, associations of change in adherence with change in glycemic control were weak.
CONCLUSIONS:
This clinic-integrated behavioral intervention was effective in preventing the deterioration in glycemic control evident during adolescence, offering a potential model for integrating medical and behavioral sciences in clinical care.
KEY WORDS: type 1 diabetes, children, adolescents, adherence, behavioral intervention, glycemic control
What’s Known on This Subject:
Strategies to assist patients in achieving optimal chronic disease self-management are critical. The complex family and regimen issues surrounding pediatric type 1 diabetes management suggest the need to integrate such strategies into routine clinical care.
What This Study Adds:
This study demonstrates the efficacy of a practical, low-intensity behavioral intervention delivered during routine care for improving glycemic outcomes. Findings indicate that the approach may offer a potential model for integrating medical and behavioral sciences to improve health care.
Improving adherence to complex medical regimens is a long-standing health care challenge. A chronic illness model of care that bases care on both medical and behavioral sciences is needed for patients to develop effective self-care skills.1,2 The need for such a model is evident in the management of type 1 diabetes, which has a complex and burdensome regimen. Although treatment has been marked by advances in insulin and glucose-monitoring technology, these advances can benefit patients only in the context of appropriate self-management behaviors. Diabetes management difficulty increases during preadolescence and adolescence, owing to hormonal3 and developmental4 factors. Consequently, a decline in glycemic control is observed during this period, increasing the risk of short- and long-term complications.5,6 This developmental challenge was evident in a continuous glucose-monitoring study in which the technology showed a beneficial effect for adults, but not for youth; this difference was attributable to different rates of actual use.7 Because adolescent management establishes a trajectory that impacts self-care into adulthood,8,9 a critical opportunity exists for improving diabetes management and subsequent long-term outcomes.
Previous research has identified modifiable behavioral targets associated with diabetes management during this developmental period. Family factors, including greater parental involvement,10,11 monitoring,12 responsibility-sharing,13 and lower family conflict,14–16 as well as greater coping skills17 and self-regulation skills18,19 including problem-solving,20,21 are associated with better diabetes management. Previous studies have shown that behavioral interventions hold promise for addressing these factors and improving diabetes management in youth.17,18,22–31 Findings have yet to result in the translation of behavioral intervention into standard clinical care, however. Barriers include reimbursement issues, staff training, and the reality that most behavioral interventions were not designed for integration into clinical care. This article describes the diabetes management outcomes of a practical, low-intensity, clinic-integrated behavioral intervention for families of youth with type 1 diabetes. We hypothesized that the intervention group would demonstrate less deterioration in adherence and glycemic control relative to the usual-care group.
Methods
Design
The trial was a multicenter, parallel-group study with equal randomization, conducted at 4 large, geographically disperse pediatric endocrinology clinics in the United States (Boston, MA; Chicago, IL; Jacksonville, FL; and Houston, TX).
Participants
Child eligibility criteria included being from 9 to 14.9 years of age, diagnosed with type 1 diabetes for at least 3 months, with a minimum insulin dose of 0.5 μ/kg/day for those diagnosed ≥1 year or 0.2 μ/kg/day for those diagnosed <1 year with at least 2 or more daily injections or use of an insulin pump; most recent hemoglobin A1c (HbA1c) levels >6% and <12% (for those diagnosed <1 year, HbA1c level of >6 at any time after diagnosis); and no other major chronic disease (except well-controlled thyroid, asthma, or celiac disease), cognitive disability, or psychiatric diagnosis. Additional parent/family eligibility criteria included living in a geographically stable home with telephone access, speaking English, having a history of at least 2 clinic visits within the previous 12 months, and having no major psychiatric diagnoses in participating parents.
The sample size of 200 patients per treatment condition was estimated based on detecting a meaningful difference in HbA1c levels between intervention and usual care at a given time interval. By using a 2-sample t test with a 2-sided 5% significance level, the power was at least 95% to detect a difference of 0.5 in HbA1c, assuming a common SD of 1.3 across intervention and usual care for HbA1c changes from baseline, given an anticipated retention rate of 90%. Adjusting for multiplicity by using the Bonferroni correction, this sample size was also adequate, with at least 85% power to detect a 0.5 HbA1c difference at any 6-month interval (6 months, 12 months, 18 months, and 24 months).
Procedures
The study was conducted from January 2006 to March 2009. Participants were recruited by research staff during routine clinic visits. Families could have either 1 or 2 parents participate, but designated 1 parent as the primary caregiver for assessments. Baseline assessments were conducted in-person in the families’ homes or other locations convenient to participants by 2-person interviewing teams not affiliated with the clinics. Families were randomly assigned to intervention or usual care, stratified by age (9 to <12 years and ≥12 to <15 years) and HbA1c levels (≤8.3 and >8.3). A system of random permuted blocks within strata was prepared by the study coordinating center by a person not involved with data collection. A separate randomization list was prepared for each strata; lists were transferred to a sequence of sealed envelopes, each containing the assignment of intervention or usual care. Persons conducting assessments were blinded to study assignment.
Families were enrolled in the study for 2 years; brief questionnaires and biomedical assessments were administered at each clinic visit (typically every 3–4 months). Intervention contacts occurred at each clinic visit for 21 months, with a final in-clinic assessment at the following visit. A telephone assessment was conducted by the coordinating center at study midpoint (9–12 months) and between the 21-month and 24-month visit. Parents and youth each received a total of $115 for completion of all assessments; youth also received $5 for each visit in which blood glucose meter data were provided. Study procedures were approved by the institutional review boards of participating institutions.
Treatment Conditions
Before each visit, research staff contacted families assigned to usual care to facilitate appointment keeping, including providing parking vouchers and acting as a liaison with clinic appointment staff. After completion of the study, families assigned to usual care received a notebook containing the intervention educational information.
The intervention group received the “WE-CAN manage diabetes” intervention at each routine clinic visit. Grounded in social cognitive theory,32 self-regulation models,33,34 and systems theory,35 the intervention was designed to help families improve diabetes management by facilitating problem-solving skills, communication skills, and appropriate responsibility sharing. Intervention contact included a preparation telephone call before clinic visits, in-person contact during clinic visits, and follow-up telephone calls. Specially trained personnel, called health advisors, delivered these components.
One week before each scheduled visit, the health advisor contacted families to help them prepare for the visit, guiding them to consider an issue to discuss. As with families assigned to usual care, the health advisors facilitated appointment keeping, provided parking vouchers, and acted as a liaison with clinic appointment staff. In-clinic sessions were structured by the WE-CAN problem-solving approach, an acronym representing the problem-solving process:
Working together
Identify strengths and areas of difficulty
Collaborate to determine goal to work on
Identify benefits of identified behavior change
Exploring barriers
Explore environmental or situational issues that increase the difficulty of the behavior
Identify unrealistic expectations or maladaptive coping strategies
Identify maladaptive parent-child interaction patterns
Choosing solutions
Explore solutions to overcome barriers and achieve goal
Evaluate solutions to maximize potential for success
Solidify into a concrete action plan
Acting on our plan
Review goal and strategies
Clarify roles and expectations
Determine a future time to discuss progress
Noting results
Review strategies tried and degree of goal achievement
Identify barriers encountered
Evaluate effectiveness of strategies
Revise plan as needed
Families collaboratively identified a goal for improved diabetes management and developed a behavior plan. The problem-solving structure offers a flexible, individualized approach. It is iterative in that the family is taught to examine the results of their behavior and revise future actions to improve outcomes. WE-CAN is similar to other problem-solving approaches used with adolescents.36 The sessions were structured to be ∼30 minutes in length, with flexibility to conform to families’ needs and schedules. Health advisors contacted families 2 and 6 weeks after the visit to assess progress, identify new issues or problems, provide additional ideas, facilitate progress, and provide support.
Health advisors received extensive on-site training in diabetes management and the intervention process. They participated in a 2-day workshop with staff from all clinical sites, during which intervention skills were taught, modeled, and practiced further. Continued on-site practice occurred until adequate proficiency was demonstrated, and periodic review of session audiotapes was used to provide feedback and ensure fidelity. Weekly conference calls and annual in-person trainings were conducted to address issues, ensure maintenance of skills, and facilitate consistency across sites.
Measures
Blood samples were obtained at each visit and shipped to a central laboratory (Joslin Diabetes Center, Boston, MA) for A1c assay (Tosoh A1c 2.2 Plus Glycohemoglobin Analyzer; Tosoh Medics, South San Francisco, CA); the reference range was 4% to 6%. Simultaneous samples were processed with the DCA-2000 (Siemens Healthcare Diagnostics, Deerfield, IL) on site. These results were used to impute replacement values if samples were lost or damaged (1.2% of values).37
Adherence was measured with the Diabetes Self-Management Profile,38,39 a structured interview conducted separately with parents and youth aged 11 and older. The measure has demonstrated adequate internal consistency (α = .76), parent-child agreement (r = 0.61), 3-month test-retest reliability (r = 0.67), and inter-interviewer agreement (r = 0.94). In this study, alphas ranged from .66 to .76.
Blood glucose meter data were obtained at each clinic visit. Patients using multiple meters were asked to bring all meters, or alternatively a printed record if the meter was unavailable (eg, kept at school). The mean number of checks per day for the previous 14 days was calculated.
Demographic variables including age, gender, date of diagnosis, family composition, socioeconomic status, race, and ethnicity were collected; diabetes management regimen was recorded at each visit.
Analyses
Baseline characteristics were summarized with means and SDs for continuous variables and with frequencies and percentages for categorical variables. The primary outcome was HbA1c across the study duration, and the primary null hypothesis to be tested was that there was no significant difference in HbA1c change from baseline between intervention and usual care. Because the effect of the intervention was hypothesized to be cumulative over time, HbA1c change from baseline was first compared at each 6-month interval by using 2-sample t test accounting for correlations among multiple measures from the same subjects in the time interval. This analysis of change scores at each time point facilitates clinical interpretation of findings. Next, HbA1c across the entire study period were fitted by using a mixed-effect linear-quadratic model as the analysis for the primary study outcome. Potential interactions by age strata, HbA1c strata, and diabetes duration were tested by using the same model. For example, the model for testing potential age interaction using the mixed-effect model expressed the mean HbA1c level as a linear-quadratic function of intervention status, number of days from enrollment the HbA1c was measured, and the subject’s age. For better fit of the data, number of days was log-transformed.
The same analytic approach was used to test for group differences in adherence change from baseline, by using t tests at each follow-up interval, and mixed-effect linear-quadratic models to test for difference in change across the study period. To determine the extent to which change in HbA1c was attributable to change in measures of adherence, the relationship of change in adherence with change in HbA1c was tested by using Pearson correlation estimated from repeated bivariate outcomes. All analyses were performed by using SAS software (SAS Institute, Inc, Cary, NC). Null hypotheses were tested, with a 2-sided significance level of 0.05.
Results
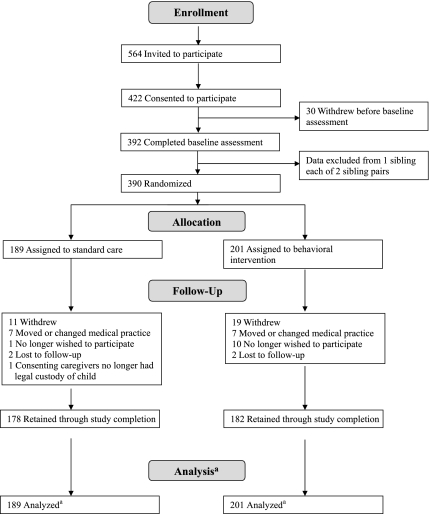
Participant flow from recruitment through follow-up is reported in Fig 1. Of those invited, 75% provided informed consent and 70% completed baseline assessment. Subject retention through study completion was 92%. There were no differences between families retained and those who withdrew by age, gender, ethnicity, baseline HbA1c, or duration of diabetes. No study-related adverse events were reported.
FIGURE 1.
Participant flow through study. a Longitudinal analyses include all available data from each subject through withdrawal or study completion.
Baseline characteristics were well balanced between groups (Table 1). There were no between-group differences in insulin regimen change during the study. Among those assigned to usual care, 22.6% of injection users changed to pump therapy, and 8.1% of pump users changed to injection; among the intervention group, 24.0% of injection users changed to pump therapy, and 7.5% of pump users changed to injection. No between-group differences were observed in clinic attendance frequency. Families assigned to the usual-care group attended 7.4 ± 1.8 clinic visits during the study period, and families in the intervention group attended 7.0 ± 2.2 clinic visits; 93% of families assigned to receive usual care and 89% of families in the intervention group attended ≥5 visits. Intervention-group families received 6.0 ± 2.2 intervention sessions (range: 0–9).
TABLE 1.
Sample Baseline Characteristics
| Control | Intervention | Pa | |
|---|---|---|---|
| Age, y; mean (SD) | 12.4 (1.7) | 12.5 (1.8) | .62 |
| Gender, N (%) | .99 | ||
| Female | 96 (50.8) | 102 (50.7) | — |
| Male | 93 (49.2) | 99 (49.3) | — |
| Race/ethnicity, N (%) | .75 | ||
| White | 131 (74.4) | 145 (75.5) | — |
| Hispanic | 16 (9.1) | 21 (10.9) | — |
| Black | 19 (10.8) | 15 (7.8) | — |
| Other | 10 (5.7) | 11 (5.7) | — |
| Number of adults in the home, N (%) | .95 | ||
| 1 | 25 (14.0) | 26 (13.5) | — |
| 2 | 138 (77.1) | 147 (76.6) | — |
| ≥3 | 16 (8.9) | 19 (9.9) | — |
| Family income, N (%) | .21 | ||
| <$50 000 | 37 (22.0) | 50 (27.3) | — |
| $50 000–$99 999 | 74 (44.0) | 64 (35.0) | — |
| 100 000+ | 57 (34.0) | 69 (37.7) | — |
| Duration of diabetes, y; mean (SD) | 4.9 (3.2) | 4.8 (3.3) | .88 |
| Regimen, N (%) | .75 | ||
| Pump | 62 (32.8) | 69 (34.3) | — |
| Injection | 127 (67.2) | 132 (65.7) | — |
| HbA1c (%), mean (SD) | 8.3 (1.1) | 8.4 (1.2) | .58 |
not applicable.
Test for group differences by using analysis of variance for continuous variables and χ2 for categorical variables.
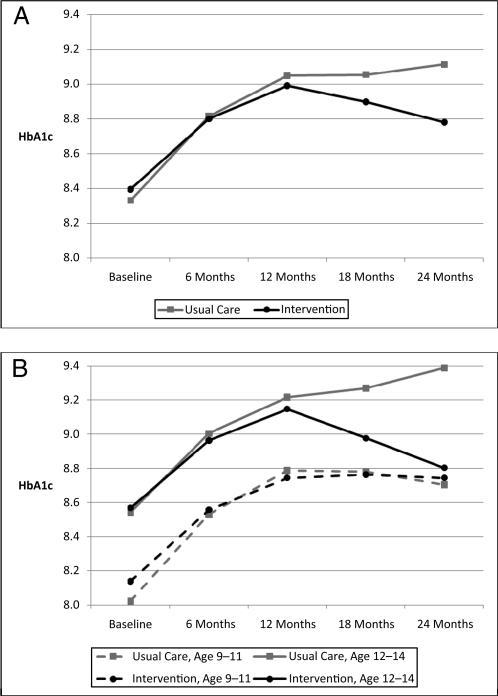
Figure 2A presents the mean HbA1c by group at each 6-month interval. The intervention had a significant effect on HbA1c change from baseline at the 24-month interval (0.44 in the intervention group and 0.76 in the usual-care group, P = .03).
FIGURE 2.
HbA1c across study duration by intervention group. A, Full-sample analysis. B, Analysis by age subgroups.
The mixed-effect linear-quadratic model to compare change in HbA1c over the study duration failed to show overall significance (P = .27); however, a significant interaction by age effect was found (P < .001), indicating a differential effect of the intervention by age group. There was no significant interaction by HbA1c strata, insulin regimen, or diabetes duration. Given the significant age interaction, separate models were tested for each age group. Among the younger-age strata, there was no significant difference in HbA1c change over time (P = .53), but a significant difference was observed among older strata (P = .04).
Mean HbA1c by age group is presented in Fig 2B. Consistent with findings from the mixed-effect model, the intervention showed no effect among the younger patients. Among the older patients, however, the intervention effect on HbA1c change from baseline approached significance by the 18-month interval (0.52 in the intervention group and 0.85 in the usual-care group, P = .07), and it was significant at the 24-month interval (0.33 in the intervention group and 0.87 in the usual-care group, P = .009).
There was no intervention effect on change from baseline for child- or parent-reported adherence (final follow-up, child-reported adherence: 1.28 in the intervention group, −0.03 in the usual-care group, P = .29; parent-reported adherence: −1.0 in the intervention group, −2.0 in the usual-care group, P = .32). Change from baseline in blood glucose monitoring frequency showed a significant adverse effect at the 24-month interval (mean change from baseline: −0.41 for the intervention group, −0.05 for the usual-care group, P = .03). Mixed-effect linear-quadratic models showed no significant group difference in change across the study duration for any measure of adherence, however, and no interaction by age, HbA1c strata, insulin regimen, or duration of diabetes. Change from baseline in parent report of adherence was associated weakly with change from baseline in glycemic control (r = −0.16; P = .01); and change in blood glucose–monitoring frequency was associated weakly with change in glycemic control (r = −0.14; P = .06). Change in child report of adherence was not associated with change in HbA1c (r = −0.01; P = .85).
Discussion
This intervention was designed to incorporate into the health care environment the provision of behavioral methods shown to be effective in changing health-related behaviors. A positive effect on glycemic control relative to usual care occurred among adolescents but not among preadolescents. The effect of the intervention began after 12 months of exposure (about 3–4 intervention sessions) and increased in magnitude across time, supporting the hypothesized cumulative effect of repeated exposure to the intervention process at each clinic visit, with families building and refining their problem-solving skills. It is also possible that the latter intervention sessions were more effective than the earlier ones, because families honed in on the most important issues to address. The skill of the health advisors and their rapport with families also may have grown. The finding also may reflect, in part, the greater intervention effect observed among older participants; however, because this group ranged in age from 12 to 14 years, the effect would not indicate a specific age transition. Among adolescents, the effect was of a clinically meaningful magnitude that, if sustained, would reduce the risk of long-term complications.6,40,41 Glycemic control usually deteriorates during adolescence,8,42 and an intervention that attenuated this increase would be considered a success.
These findings are consistent with those obtained in a smaller study testing a similar approach delivered to the child in the home environment. In that study, a significant improvement in glycemic control relative to the control group was obtained and maintained 2 years after intervention for the older participants but not for the younger participants.27,43 The WE-CAN approach used in this study was delivered to parent and child together and incorporated greater attention to parent-child issues. We anticipated that these changes would make the intervention more effective for youth across the age range; however, findings in this study were virtually identical to those observed previously, suggesting that this approach may be most salient for youth who are beginning to take greater responsibility for their diabetes management.
The finding of a positive intervention effect on HbA1c levels but not on adherence is noteworthy, because the hypothesized effect of this behavioral intervention on HbA1c is one mediated by adherence. Assessment of adherence focuses on the conduct of discrete behaviors, however, and cannot capture higher-level concepts adequately (eg, quality of the use of blood glucose data in decision-making, accuracy of carbohydrate counting, and so forth). Notably, there was only a weak relationship between change in adherence and change in HbA1c. Assessment of adherence to complex medical regimens is notoriously difficult, and associations between adherence and HbA1c have been modest at best.44 Sources of error include imperfect recall and social desirability bias; intervention goal-setting and behavior monitoring elements may have simultaneously produced higher standards and more objective assessment of adherence relative to the control group. Future research should further explore potential mechanisms for the effect on HbA1c levels, such as degree of parent involvement in diabetes management, parent-child conflict, or other management behaviors not specifically assessed by the adherence measure.
The current trial was the first multisite study of a clinic-integrated behavioral intervention for improving diabetes management among families of youth with type 1 diabetes. Strengths include recruitment from 4 sites in diverse geographic regions, use of a centralized laboratory for HbA1c measurement, and an intervention design that is potentially translatable to routine clinical care. To recruit adequate numbers of participants, however, the study was conducted at large pediatric endocrinology centers. It is unknown whether results would generalize to families served by smaller or less specialized practices. Future research should address the utility of this approach delivered in varying practices by existing health care personnel.
Translation of behavioral interventions to the health care setting given current staffing and reimbursement mechanisms is known to be challenging.45 Although this behavioral intervention was designed to be integrated into the health care setting and potentially could be delivered by a broad range of personnel, it nonetheless requires staff time to consult with families at each visit. Sustainability of such an intervention will likely require the ability to obtain reimbursement for this consultation. The goal of advancing the provision of health care to better assist patients in the development of effective self-care skills may require efforts to address such mechanisms in the health care environment.
Conclusions
In most research testing the efficacy of behavioral interventions for chronic illness management, interventions are time-limited; however, it is well recognized that medical care for chronic illness must be ongoing. Findings from this study reveal the utility of incorporating behavioral management into ongoing clinical care. Future research testing this approach across a broader range of clinical settings would be useful to inform translation and dissemination efforts. Although there has been increased awareness of the need for a chronic illness model of health care,1 insufficient research has tested ways to deliver care consistent with this model. This study demonstrates the efficacy of a practical, low-intensity behavioral intervention delivered during routine care. Findings indicate that the approach may offer a potential model for integrating medical and behavioral sciences in health care.
Acknowledgments
The authors acknowledge the contributions of the research staff at the participating clinical sites and the families who participated in the study.
Glossary
- HbA1c
hemoglobin A1c
Footnotes
All authors made substantive intellectual contributions to this article by participating in the concept and design, analysis and interpretation of data, and drafting or critical revision of the manuscript.
This trial has been registered at www.clinicaltrials.gov (identifier NCT00273286).
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by the intramural research program of the National Institutes of Health, Eunice Kennedy Shriver National Institute of Child Health and Human Development, under the following contracts: N01-HD-4-3364, Joslin Diabetes Center, Boston, Massachusetts; N01-HD-4-3361, Nemours Children's Clinic, Jacksonville, Florida; N01-HD-4-3362, Texas Children's Hospital, Houston, Texas; N01-HD-4-3363, Children's Memorial Hospital, Chicago, Illinois; and N01-HD-3-3360, James Bell Associates, Arlington, Virginia. Funded by the National Institutes of Health (NIH).
References
- 1.Glasgow RE, Wagner EH, Kaplan RM, Vinicor F, Smith L, Norman J. If diabetes is a public health problem, why not treat it as one? A population-based approach to chronic illness. Ann Behav Med. 1999;21(2):159–170 [DOI] [PubMed] [Google Scholar]
- 2.Glasgow RE, Hiss RG, Anderson RM, et al. Report of the health care delivery work group: behavioral research related to the establishment of a chronic disease model for diabetes care. Diabetes Care. 2001;24(1):124–130 [DOI] [PubMed] [Google Scholar]
- 3.Amiel SA, Sherwin RS, Simonson DC, Lauritano AA, Tamborlane WV. Impaired insulin action in puberty: a contributing factor to poor glycemic control in adolescents with diabetes. N Engl J Med. 1986;315(4):215–219 [DOI] [PubMed] [Google Scholar]
- 4.Susman-Stillman A, Hyson DM, Anderson FS, Collins WA. Adolescent psychosocial development and adherence to treatment for insulin-dependent diabetes mellitus. In: McNamara JA, Jr, Trotman CA, eds. Creating the Compliant Patient. Ann Arbor, MI: Center for Human Growth and Development. The University of Michigan; 1997:73–101 [Google Scholar]
- 5.Helgeson VS, Siminerio L, Escobar O, Becker D. Predictors of metabolic control among adolescents with diabetes: a 4-year longitudinal study. J Pediatr Psychol. 2009;34(3):254–270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Diabetes Control and Complications Trial Research Group . Effect of intensive diabetes treatment on the development and progression of long-term complications in adolescents with insulin-dependent diabetes mellitus: Diabetes Control and Complications Trial. J Pediatr. 1994;125(2):177–188 [DOI] [PubMed] [Google Scholar]
- 7.Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group . Effectiveness of continuous glucose monitoring in a clinical care environment: evidence from the Juvenile Diabetes Research Foundation continuous glucose monitoring (JDRF-CGM) trial. Diabetes Care. 2010;33(1):17–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bryden KS, Peveler RC, Stein A, Neil A, Mayou RA, Dunger DB. Clinical and psychological course of diabetes from adolescence to young adulthood: a longitudinal cohort study. Diabetes Care. 2001;24(9):1536–1540 [DOI] [PubMed] [Google Scholar]
- 9.Wysocki T, Hough BS, Ward KM, Green LB. Diabetes mellitus in the transition to adulthood: adjustment, self-care, and health status. J Dev Behav Pediatr. 1992;13(3):194–201 [PubMed] [Google Scholar]
- 10.Anderson B, Ho J, Brackett J, Finkelstein D, Laffel L. Parental involvement in diabetes management tasks: relationships to blood glucose monitoring adherence and metabolic control in young adolescents with insulin-dependent diabetes mellitus. J Pediatr. 1997;130(2):257–265 [DOI] [PubMed] [Google Scholar]
- 11.Wysocki T, Taylor A, Hough BS, Linscheid TR, Yeates KO, Naglieri JA. Deviation from developmentally appropriate self-care autonomy: association with diabetes outcomes. Diabetes Care. 1996;19(2):119–125 [DOI] [PubMed] [Google Scholar]
- 12.Ellis DA, Podolski C-L, Frey M, Naar-King S, Wang B, Moltz K. The role of parental monitoring in adolescent health outcomes: impact on regimen adherence in youth with type 1 diabetes. J Pediatr Psychol. 2007;32(8):907–917 [DOI] [PubMed] [Google Scholar]
- 13.Helgeson VS, Reynolds KA, Siminerio L, Escobar O, Becker D. Parent and adolescent distribution of responsibility for diabetes self-care: links to health outcomes. J Pediatr Psychol. 2008;33(5):497–508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Anderson BJ, Vangsness L, Connell A, Butler D, Goebel-Fabbri A, Laffel LM. Family conflict, adherence, and glycaemic control in youth with short duration Type 1 diabetes. Diabet Med. 2002;19(8):635–642 [DOI] [PubMed] [Google Scholar]
- 15.Hauser ST, Jacobson AM, Lavori P, et al. Adherence among children and adolescents with insulin-dependent diabetes mellitus over a four-year longitudinal follow-up: II. Immediate and long-term linkages with the family milieu. J Pediatr Psychol. 1990;15(4):527–542 [DOI] [PubMed] [Google Scholar]
- 16.Wysocki T. Associations among teen-parent relationships, metabolic control, and adjustment to diabetes in adolescents. J Pediatr Psychol. 1993;18(4):441–452 [DOI] [PubMed] [Google Scholar]
- 17.Grey M, Boland EA, Davidson M, Li J, Tamborlane WV. Coping skills training for youth with diabetes mellitus has long-lasting effects on metabolic control and quality of life. J Pediatr. 2000;137(1):107–113 [DOI] [PubMed] [Google Scholar]
- 18.Delamater AM, Bubb J, Davis SG, et al. Randomized prospective study of self-management training with newly diagnosed diabetic children. Diabetes Care. 1990;13(5):492–498 [DOI] [PubMed] [Google Scholar]
- 19.Miller VA, Drotar D. Decision-making competence and adherence to treatment in adolescents with diabetes. J Pediatr Psychol. 2007;32(2):178–188 [DOI] [PubMed] [Google Scholar]
- 20.Hill-Briggs F, Gemmell L. Problem solving in diabetes self-management and control: a systematic review of the literature. Diabetes Educ. 2007;33(6):1032–1050, discussion 1051–1052 [DOI] [PubMed] [Google Scholar]
- 21.Stetson B, Boren S, Leventhal L, et al. Embracing the evidence on problem solving in diabetes self-management education and support. SelfCare. 2010;1(3):83–99 [Google Scholar]
- 22.Carney RM, Schechter K, Davis T. Improving adherence to blood glucose testing in insulin-dependent diabetic children. Behav Ther. 1983;14(2):247–254 [Google Scholar]
- 23.Epstein LH, Beck S, Figueroa J, et al. The effects of targeting improvements in urine glucose on metabolic control in children with insulin dependent diabetes. J Appl Behav Anal. 1981;14(4):365–375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kaplan RM, Chadwick MW, Schimmel LE. Social learning intervention to promote metabolic control in type I diabetes mellitus: pilot experiment results. Diabetes Care. 1985;8(2):152–155 [DOI] [PubMed] [Google Scholar]
- 25.Laffel LM, Vangsness L, Connell A, Goebel-Fabbri A, Butler D, Anderson BJ. Impact of ambulatory, family-focused teamwork intervention on glycemic control in youth with type 1 diabetes. J Pediatr. 2003;142(4):409–416 [DOI] [PubMed] [Google Scholar]
- 26.Méndez FJ, Beléndez M. Effects of a behavioral intervention on treatment adherence and stress management in adolescents with IDDM. Diabetes Care. 1997;20(9):1370–1375 [DOI] [PubMed] [Google Scholar]
- 27.Nansel TR, Iannotti RJ, Simons-Morton BG, Plotnick LP, Clark LM, Zeitzoff L. Long-term maintenance of treatment outcomes: diabetes personal trainer intervention for youth with type 1 diabetes. Diabetes Care. 2009;32(5):807–809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rydén O, Nevander L, Johnsson P, et al. Family therapy in poorly controlled juvenile IDDM: effects on diabetic control, self-evaluation and behavioural symptoms. Acta Paediatr. 1994;83(3):285–291 [DOI] [PubMed] [Google Scholar]
- 29.Schafer LC, Glasgow RE, McCaul KD. Increasing the adherence of diabetic adolescents. J Behav Med. 1982;5(3):353–362 [DOI] [PubMed] [Google Scholar]
- 30.Silverman AH, Hains AA, Davies WH, Parton E. A cognitive behavioral adherence intervention for adolescents with type 1 diabetes. J Clin Psychol Med Settings. 2003;10(2):119–127 [Google Scholar]
- 31.Wysocki T, Harris MA, Buckloh LM, et al. Effects of behavioral family systems therapy for diabetes on adolescents’ family relationships, treatment adherence, and metabolic control. J Pediatr Psychol. 2006;31(9):928–938 [DOI] [PubMed] [Google Scholar]
- 32.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall; 1986 [Google Scholar]
- 33.Leventhal H, Leventhal EA, Cameron L. Representations, procedures, and affect in illness self-regulations: a perceptual-cognitive model. In: Baum A, Revenson TA, Singer JE, eds. Handbook of Health Psychology. Mahwah, NJ: Erlbaum; 2001:19–47 [Google Scholar]
- 34.Leventhal H, Leventhal EA, Contrada RJ. Self-regulation, health and behavior: a perceptual-cognitive approach. Psychol Health. 1998;13:717–733 [Google Scholar]
- 35.Bateson G. Steps to an Ecology of Mind. New York, NY: Ballantine; 1972 [Google Scholar]
- 36.Simons-Morton BG, Haynie D, Saylor K, Crump AD, Chen R. The effects of the Going Places Program on early adolescent substance use and antisocial behavior. Prev Sci. 2005;6(3):187–197 [DOI] [PubMed]
- 37.Tamborlane WV, Kollman C, Steffes MW, et al. Comparison of fingerstick hemoglobin A1c levels assayed by DCA 2000 with the DCCT/EDIC central laboratory assay: results of a Diabetes Research in Children Network (DirecNet) Study. Pediatr Diabetes. 2005;6(1):13–16 [DOI] [PubMed] [Google Scholar]
- 38.Harris MA, Wysocki T, Sadler M, et al. Validation of a structured interview for the assessment of diabetes self-management. Diabetes Care. 2000;23(9):1301–1304 [DOI] [PubMed] [Google Scholar]
- 39.Diabetes Research in Children Network (DirecNet) Study Group . Diabetes self-management profile for flexible insulin regimens: cross-sectional and longitudinal analysis of psychometric properties in a pediatric sample. Diabetes Care. 2005;28(8):2034–2035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.The Diabetes Control and Complications Trial Research Group . The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(14):977–986 [DOI] [PubMed] [Google Scholar]
- 41.Diabetes Control and Complications Trial Research Group . The absence of a glycemic threshold for the development of long-term complications: the perspective of the Diabetes Control and Complications Trial. Diabetes. 1996;45(10):1289–1298 [PubMed] [Google Scholar]
- 42.Mortensen HB, Hougaard P, The Hvidøre Study Group on Childhood Diabetes . Comparison of metabolic control in a cross-sectional study of 2,873 children and adolescents with IDDM from 18 countries. Diabetes Care. 1997;20(5):714–720 [DOI] [PubMed] [Google Scholar]
- 43.Nansel TR, Iannotti RJ, Simons-Morton BG, et al. Diabetes personal trainer outcomes: short-term and 1-year outcomes of a diabetes personal trainer intervention among youth with type 1 diabetes. Diabetes Care. 2007;30(10):2471–2477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hood KK, Peterson CM, Rohan JM, Drotar D. Association between adherence and glycemic control in pediatric type 1 diabetes: a meta-analysis. Pediatrics. 2009;124(6). Available at: www.pediatrics.org/cgi/content/full/124/6/e1171 [DOI] [PubMed] [Google Scholar]
- 45.Pagoto S. The current state of lifestyle intervention implementation research: where do we go next? Trans Behav Med. 2011;1(3):401–405 [DOI] [PMC free article] [PubMed] [Google Scholar]