Abstract
The Relational Psychotherapy Mothers’ Group (RPMG), a developmentally informed, supportive psychotherapy designed to serve heroin-addicted mothers with children up to 16 years of age, aims at addressing psychosocial vulnerabilities, and facilitating optimal parenting, among at-risk mothers. We present preliminary evidence on the efficacy of RPMG as an “add on” treatment in comparison with standard methadone counseling alone. At the end of the 24-week treatment period, mothers receiving RPMG plus standard methadone counseling demonstrated lower levels of risk for child maltreatment, greater involvement with their children, and more positive psychosocial adjustment than women who received methadone counseling alone. Children of RPMG participants also reflected fewer problems in multiple areas. At 6 months posttreatment, RPMG recipients continued to be at a relative advantage, although the magnitude of group differences was often attenuated. Notably, urinalyses indicated that RPMG mothers showed greater improvements in levels of opioid use over time than comparison mothers.
Recent years have seen rapid increases in the number of children at risk for negative outcomes by virtue of maternal substance abuse. Current estimates are that over 3 million American women regularly use illicit drugs (National Center on Addiction and Substance Abuse, 1996), and up to 80% of these women are mothers of at least one child. Drug abusing mothers show elevated levels of psychiatric disturbance and significant problems with child rearing. Not surprisingly, their children also display several psychosocial difficulties: by early adolescence, as many as 65% of children of drug using mothers have been found to have a major psychiatric disorder (Luthar, Cushing, Merikangas, & Rounsaville, 1998).
The constellation of psychosocial vulnerabilities existing among addicted mothers points to the need for multifaceted parenting interventions for them. In this paper, we describe one such intervention, the Relational Psychotherapy Mothers’ Group (RPMG), a treatment that was developed for heroin-addicted mothers with children up to 16 years of age. RPMG is a supportive psychotherapy aimed at facilitating optimal parenting among at-risk mothers and is offered over 24 weekly group sessions which supplement standard methadone treatment. In discussions that follow, we present the theoretical perspectives underlying this intervention and its major defining features, followed by results of a pilot study on its efficacy.
Theoretical Perspectives Underlying the RPMG Intervention
Development of RPMG was based on a multi-variable risk and protective model derived from the literature on resilience in developmental psychopathology. A common view in this literature is that processes influencing individuals’ development operate at three broad levels: those related to the individual, family, and community (Luthar & Zigler, 1991; Werner & Smith, 1992). Consideration of both negative and positive forces within each of these levels is integral to understanding diverse developmental pathways among—and thus in designing effective interventions for—individuals at risk for negative outcomes.
At the individual level, most striking among areas of substance abusing mothers’ vulnerability is their high comorbid psychopathology, particularly in the realms of depression and anxiety (Hawley & Disney, 1992). In recent research on addicted mothers (Luthar et al., 1998), almost 9 out of 10 women were found to have at least one DSM-III-R affective or anxiety disorder diagnosis during their lifetimes. Similarly, given high levels of both past and current ongoing traumatic life events, rates of posttraumatic stress disorder are also high (Fullilove et al., 1993; Mirin, Weiss, Griffin, & Michael, 1991; Najavits, Weiss, & Shaw, 1997).
Recognizing these psychiatric difficulties, the RPMG intervention entails concerted attention to substance abusing mothers’ psychological vulnerabilities, with the view that unless these individuals’ own psychological needs are addressed, attempts to improve their parenting behaviors are unlikely to achieve any lasting success. One half of the 24 sessions in this treatment are thus directly focused on the women’s own functioning, addressing topics such as coping with anger, depression, low self-esteem, and multiple life stressors.
With regard to individual attributes that serve protective functions, salient are addicted mothers’ feelings of regret for past errors. Stereotypes that drug-abusing mothers are “ignorant” about appropriate child rearing are not based in fact (Luthar, Cushing, & McMahon, 1997; Mayes & Bornstein, 1997). Clinical data indicate, to the contrary, that these mothers are often aware that their parenting strategies can be counterproductive (Hawley & Disney, 1992; Levy & Rutter, 1992; Luthar & Suchman, 1999; Luthar & Walsh, 1995). The RPMG intervention thus entails deliberate attempts to harness mothers’ capacities to acknowledge past “errors” as catalysts for changes toward optimal parenting behaviors.
At the familial level, childhood experiences of dysfunctional parenting often constitute a salient risk for substance-abusing women. Many women report having been exposed, as children, to inadequate adult nurturance and either excessively lax or rigid disciplinary styles; physical, sexual, and emotional abuse are also common (Davis, 1990; Grice, Brady, Dustan, Malcolm, & Kilpatrick, 1995; Najavitz et al., 1997; Rohsenow, Corbett, & Devine, 1988). Adversities such as these heighten risks for how addicted mothers themselves come to function as parents. Studies have demonstrated tendencies to use authoritarian disciplinary approaches which reinforce negative attention-seeking behaviors among children (Bauman & Dougherty, 1983; Black & Mayer, 1980); incidents of child maltreatment are also frequently documented (Black & Mayer, 1980; Wasserman & Leventhal, 1993).
Such parenting problems are addressed in various ways within the RPMG intervention. At the most concrete level, 12 of the 24 sessions are focused on specific parenting issues, such as developing strategies for circumventing violent conflict, using alternatives to physical punishment, establishing age-appropriate limits in disciplining children, and fostering developmentally appropriate and warm parenting styles. Second, in cognizance of the women’s negative childhood experiences, the RPMG therapists foster the mothers’ own negotiation of fundamental developmental tasks (e.g., developing trust vs. mistrust in relationships) and serve as role models of effective parenting (e.g., by consistently offering respect and setting firm but nonpunitive limits).
From the standpoint of protective familial factors, critical are the strong desire and potential that most addicted mothers have to benefit from supportive parenting interventions. Contrary to common stereotypes, many substance-abusing women are highly concerned about the well-being of their children and acknowledge substantial confusion regarding appropriate child-rearing strategies (Colten, 1982; Grossman & Schottenfeld, 1992; Hawley & Disney, 1992; Levy & Rutter, 1992; Tunving & Nilsson, 1985). RPMG is grounded in the basic assumption that with adequate support and guidance, many addicted mothers have both the will and capacity to benefit from sensitive interventions (e.g., Greif & Dreschler, 1993; Lief, 1985).
At the level of the community, perhaps the most pronounced risk confronting addicted mothers is exposure to stigma, not only from society in general but also, frequently, from service providers (Chang, Carroll, Behr, & Kosten, 1992; Eliason, Skinstad, & Helene, 1995; Luthar et al., 1997; Mackie–Ramos & Rice, 1988; Najavits et al., 1995). As a result of such stigmas, drug-abusing mothers are often wary of treatment approaches that seem to focus primarily on their “deficits” as parents (Levy & Rutter, 1992), such as those in which they are “taught” parenting skills from a strictly didactic standpoint. Within RPMG, therefore, the effort is to discuss child-rearing issues within the context of supportive psychotherapeutic experiences, using guided discovery approaches as in insight-oriented therapy (e.g., Greif & Drechsler, 1993; Luthar & Walsh, 1995).
Apart from exposure to societal stigmas, a second community-level risk is the dysfunctional informal social networks. Social isolation is a serious problem, and even the few addicted women who do have close relationships report vulnerability to a range of difficulties (Amaro & Hardy–Fanta, 1995; Brunswick & Titus, 1998; Wald, Harvey, & Hibbard, 1995). To illustrate, male partners of many addicted women supply them with drugs yet provide limited emotional, financial, or parenting support; physical and emotional abuse are also common (Dembo et al., 1988; Wald et al., 1995; Wallace, 1991; Wells, Clark, et al., 1994).
Such evidence of problematic relationships is of particular concern given the critical significance of interpersonal relationships for women in general. Stresses associated with gender roles and relations with others have been viewed as contributing to the higher rates of depression among women than men. Furthermore, interpersonal problems often constitute a greater risk for depression among women than problems in other realms of life (see McGrath, Keita, Strickland, & Russo, 1991).
Whereas women’s high investment in relationships may sometimes constitute a risk, it may equally confer advantages from an intervention standpoint, as addicted women can be more responsive than males to positive interpersonal influences in psychotherapy (Kosten, Gawin, Kosten, & Rounsaville, 1993; Luthar, Glick, Zigler, & Rounsaville, 1993; McGrath et al., 1991). Intervention efforts based on affiliation and social ties have been viewed as particularly promising in working with female addicts (Brunswick, Messeri, & Titus, 1992; Webster–Stratton, 1997) because they build on the unmet affiliative needs that are commonly linked with drug use among women (Brunswick, Lewis, & Messeri, 1991).
In view of these factors, RPMG is designed as a supportive psychotherapy group treatment. The use of a group format helps addicted mothers to develop their interpersonal skills, to perceive the universality of many dilemmas pertaining to their roles as women and mothers (e.g., Yalom, 1985), and to benefit from cohesive and mutually supportive interpersonal networks (see Webster–Stratton, 1997).
Defining Features of RPMG
Four central characteristics define RPMG as a psychotherapy intervention. The first is a supportive therapists’ stance. Encompassing the Rogerian constructs of acceptance, empathy, and genuineness (Braswell & Seay, 1984; Weiner, 1983), this stance is viewed as essential for fostering a strong therapeutic alliance and subsequent progress in meeting mothers’ unmet developmental needs.
The second is an interpersonal, relational focus, a component with roots in gender-sensitive perspectives on women as well as in interpersonal psychotherapy (Klerman, Weissman, Rounsaville, & Chevron, 1984). This aspect of RPMG provides the basis for addressing the interpersonal isolation and stress that figure prominently in addicted women’s multiple roles, including those as parents.
With regard to features as a group treat ment, RPMG involves only substance-abusing mothers (not mothers and fathers), and groups are led by female therapists in order to optimize women’s comfort in discussing sensitive issues such as those relating to their own victimization. To accommodate the frequently chaotic schedules of patients in methadone treatment, group membership is open or rotating. Sessions are led by a clinical psychologist who is assisted by a drug counselor from the methadone clinic, thus bringing therapeutic expertise across diverse domains including child development, women’s psychology, and addiction-related issues. All sessions are semistructured, and a therapists’ manual (Luthar, Suchman, & Boltas, 1997) provides a detailed outline for addressing each session topic.
The fourth defining feature of RPMG is discovery-based, insight-oriented parenting skill-facilitation. Rather than “instructing” the mothers about appropriate parenting, therapists encourage the women to explore the strengths and limitations of their own strategies, and guide them toward developing optimal approaches. These goals are pursued via open-ended discussions as well as through specific role plays and “brainstorming” exercises (for further details, please see Luthar & Suchman, 1999; Luthar, Suchman, et al. 1997). The discovery-based, nondirective approach used in RPMG1 serves to empower the mothers, implicitly acknowledging their motivation to become better parents and their own capacities to foster the positive development of their families.
Overview of the Pilot Study
The RPMG treatment was designed, manualized, and tested as part of a 3-year psychotherapy development study. Opioid-abusing women who received this intervention along with standard treatment in their methadone programs (described below) were compared with those receiving standard treatment alone. The effectiveness of RPMG was ascertained via a battery of assessments administered to women on entry into treatment, immediately after the 24-week treatment, and 6 months after treatment completion.
Comparison group
Treatment in the methadone clinics entailed participation in weekly, 1-hr counseling groups in addition to pharmacological intervention (methadone) and periodic meetings with case managers to secure basic needs (e.g., housing, welfare benefits, legal aid). The weekly groups provided the standard drug counseling that is used in methadone clinics (see Mercer, Carpenter, Daley, Patterson, & Vopicelli, 1994; Zackon, McAuliffe, & Ch’ien, 1994). Typically led by certified drug counselors and nurses, these groups are generally focused on providing information on the unfolding of addictions, specific triggers and pitfalls of addictive behaviors, changing addictive life-styles, and developing coping strategies to avoid relapses. The counselor’s stance involves frequent use of didactic approaches and confrontation of behaviors viewed as counterproductive to the goal of abstinence (Mercer et al., 1994; Zackon et al., 1994).
Outcomes assessed
Constructs examined in this study were those specifically targeted by the RPMG intervention and included aspects of the women’s functioning as parents as well as facets of their own psychological functioning. Within the sphere of parenting, the single most critical domain was the mother’s risk for maltreating behaviors, a construct that reflects a serious problem among addicted parents and is centrally targeted by the treatment. For a subset of participants in the study—mothers who had children over 7 years of age—the children’s perceptions of their mothers’ maltreating behaviors were also assessed.
In addition to risk for maltreatment, we also assessed two domains of positive parenting behaviors. These encompassed affective interactions (involvement and communication with the child) and instrumental interactions (limit setting, and promotion of child autonomy and independence).
In assessing the women’s psychosocial adjustment, critical domains in terms of relevance to RPMG were women’s overall feelings of satisfaction and support in their roles as mothers. We also obtained information on depressive symptoms, given the high comorbity between depression and addiction among women. Both mothers’ and children’s reports of the children’s psychological functioning were sought, with the rationale that improvements in mothers’ adjustment might also be reflected in improved functioning among children in their care. Finally, data on the women’s drug use were also examined. Although substance use itself is not specifically targeted within RPMG, it has been suggested that addicted women’s improvements in psychosocial functioning can “carry over” to their substance use as well (e.g., Brunswick et al., 1991, 1992; Najavits et al., 1998).
Therapist ratings
In addition to testing the effectiveness of RPMG, a second objective in this study was to ascertain whether this intervention does in fact provide therapeutic components distinct from those in the drug-counseling treatment. A Therapist Adherence Rating Scale was thus developed, with items based on the defining features of each of the two interventions (RPMG and standard drug counseling). Objectives in developing this instrument were threefold: to obtain preliminary data on its psychometric properties, to determine the degree to which therapists delivering each intervention adhered to its defining characteristics, and to establish the discriminability of the two treatments (i.e., the degree to which they reflected distinct therapeutic ingredients).
In sum, this pilot study was conducted to obtain preliminary data on the effectiveness of RPMG, a therapeutic intervention designed around the scaffolding of risk and protective factors that are known to affect most heroin-addicted women. Treatment success was gauged in conceptually critical outcome domains pertaining to the mothers’ parenting as well as their own psychosocial adjustment. Assessments were conducted at the beginning of treatment, at the end of the 6-month intervention, and at a 6-month follow-up, and a therapist rating scale was used to establish discriminability of the two treatments involved in the study.
Methods
Overview of procedures
Heroin-addicted mothers interested in participating in parenting groups were recruited at three methadone clinics in New Haven, Connecticut. Recruitment occurred via several means including referrals from counselors, visits made by research assistants to ongoing drug-counseling groups and medication lines, and referrals from mothers who had already participated in the study. To be eligible for inclusion, mothers had to (a) have children less than 16 years of age and (b) report subjective experiences of problems with parenting.2 Exclusion criteria included conditions that would impede ability to benefit from group therapy such as cognitive deficits, psychotic thought processes, and suicidality.
All eligible mothers who expressed interest in the study met with a research assistant who explained the nature of the study as a randomized clinical trial. Initial assessments were scheduled with those who agreed to participate, and mothers were randomized to either the RPMG or comparison condition. As noted previously, the RPMG condition entailed weekly RPMG groups in addition to standard treatment at the clinic, whereas in the comparison condition mothers received standard treatment alone. To compensate families for time spent in assessments, a staggered reimbursement schedule was used, such that mothers and children were paid, respectively, $15 and $5 for baseline assessments, $30 and $10 on treatment completion, and $50 and $15 at the 6-month follow-up assessments.
Each 24-week intervention was co-led by a clinical psychologist and a drug counselor from the clinic. In total, five complete RPMG interventions were conducted by two psychologists and five drug counselors. Mothers enrolled in groups as openings occurred. Prior to beginning their groups, all therapists delivering the RPMG treatment received training that involved discussions on underlying theory and specific therapeutic skills, review of session videotapes, and an overview of the therapist manual contents. All RPMG sessions were videotaped and therapists were supervised on a weekly basis.
Sample
A total of 61 heroin-addicted mothers expressed interest in the study. As this was a psychotherapy development study and we were uncertain of the power of the new RPMG intervention to retain patients, we sought to oversample within the RPMG group and randomly assigned two patients on average to RPMG for every one assigned to the comparison group.3 Thus, a total of 37 mothers were enrolled in RPMG and 24 in the comparison condition. At any given time, the number of mothers enrolled in RPMG groups ranged from 4 to 8.
Of the 37 mothers randomized to RPMG, 32 completed treatment,4 yielding an 86% retention rate. Two of the 5 mothers who left treatment were transferred to different clinics, 1 obtained full-time employment, 1 moved to a different city, and 1 left for reasons unknown. Of the 24 mothers in the drug-counseling groups (mandated by the clinics for all patients to remain in the methadone programs), 20 completed treatment, yielding an 83% retention rate. Of the 4 mothers who dropped out, 1 was transferred to a different clinic, 1 left due to a family illness, and 2 left for unknown reasons.
At the time of their 6-month follow-up assessments, we were able to locate a total of 47 women. These included 28 of the 32 RPMG treatment completers and 19 of the 20 comparison treatment completers.
Demographic characteristics of the sample are summarized in Table 1. As indicated, mothers in the sample were primarily from Caucasian backgrounds and low socioeconomic strata.
Table 1.
Demographic characteristics of mothers and children
| RPMGa | DCb | |||
|---|---|---|---|---|
| Marital status: Single | 63 | 70 | ||
| Ethnicity | ||||
| Caucasian | 78 | 65 | ||
| African American | 10 | 30 | ||
| Hispanic | 12 | 5 | ||
| Target children: Agec | ||||
| Less than 2 years | 28 | 15 | ||
| 2–5 years | 3 | 5 | ||
| 6–12 years | 41 | 45 | ||
| 13–16 years | 28 | 35 | ||
| Female target children | 56 | 44 | ||
| RPMG | DC | |||
| Mean | SD | Mean | SD | |
| Mothers’ age | 34.9 | 5.7 | 34.4 | 4.4 |
| Target child’s age | 10.1 | 4.2 | 9.0 | 4.7 |
| Hollingshead SES | 56d | 15.6 | 54.7d | 13.8 |
Note: The two groups did not differ significantly on any of these demographic indices.
Mothers who received RPMG plus standard drug counseling.
Mothers who received drug counseling alone.
Children about whom mothers expressed greatest concern.
Corresponds to Class IV: second-to-lowest class in Hollingshead’s five-class hierarchy of social status (Hollingshead & Redlich, 1958).
Each participant was asked to identify one of her children about whom she was most concerned, and, as noted earlier, identified children of 7 years and older were brought in to complete assessments whenever possible. Of the 52 mothers who completed the post-treatment assessments, 18 had children younger than 7 years of age, and 10 were unable to bring their children to the clinic at both posttreatment and follow-up. Thus, post-treatment and follow-up assessments were each obtained from a total of 24 children.
Measures
Parenting
The Parental Acceptance/Rejection Questionnaire (PARQ; Rohner, 1991), a 60-item measure rated on a 4-point scale, was used to assess maltreatment in the mother–child relationship. The PARQ yields a com posite Maltreatment score comprised of four subscales: Aggression/Hostility, Neglect/Indifference, Undifferentiated Rejection, and low expressed Warmth/Acceptance. Parallel versions of the PARQ assess respectively the mothers’ and children’s perceptions of maternal behaviors. Adequate psychometric properties have been documented for the PARQ (Rohner, 1991). In this sample, the Cronbach’s alpha coefficients for the four subscales ranged between .72 and .89 (median .85) for the mothers and between .72 and .94 (median .88) for the children.
The Parent–Child Relationship Inventory (PCRI; Gerard, 1994), a 78-item measure rated on a 4-point scale, was used to assess the mothers’ reports of positive maternal behaviors. The PCRI consists of six subscales, including Communication, Involvement, Limit Setting, Autonomy, Satisfaction, and Support. Two of these subscales were used to measure mothers’ affective interactions—that is, Communication (capacity to talk and empathize with children) and Involvement (expressed interest in children’s activities). Instrumental interactions were assessed based on the Limit Setting (ability to provide appropriate discipline) and Autonomy (ability to promote a child’s independence) subscales. Adequate psychometric properties have been established for the PCRI (Gerard, 1994), and for this sample of mothers Cronbach’s alpha coefficients for the Communication, Involvement, Limit Setting, and Autonomy subscales ranged between .61 and .80 with a median of .77.
Mothers’ psychosocial adjustment
Mothers’ overall levels of satisfaction with their parenting roles, as well as the degree to which they felt supported in their roles as parents, were assessed via the Satisfaction (enjoyment derived from parenting) and Support (perceived emotional and practical support) subscales from the PCRI. Internal consistency coefficients in this sample were .83 and .64. The 13-item short form for the Beck Depression Inventory (BDI; Beck & Beck, 1972), which has well-documented psychometric properties and concurrent validity with the long form (Gould, 1982), served as the measure of depression. The alpha coefficient in this sample was .89.
Child’s psychosocial adjustment
Children’s psychosocial adjustment levels were assessed via the Behavioral Assessment System for Children (BASC; Reynolds & Kamphaus, 1992), with the Parent Rating Scale (PRS) administered to the mothers and the Self-Report Scale (SRP) to their children. Separate PRS forms are available for different age groups of children: the Preschool (ages 4–5 years), Child (ages 6–11 years) and Adolescent (ages 12–18 years) versions, with 131, 138, and 126 items, respectively, all rated on 4-point scales. The SRP Child (ages 8–11 years) and Adolescent (ages 12–18 years) forms have 152 and 186 items, respectively, each rated on a 2-point (true/false) scale. Composite subscale scores from each BASC form served as measures of children’s adaptation—that is, Internalizing and Externalizing scores from the PRS, and scores on Clinical and School Maladjustment, as well as on Personal Adjustment (encompassing interpersonal relations, self-reliance, and self-esteem) from the SRP. Excellent psychometric properties for the BASC have been documented (Reynolds & Kamphaus, 1992). Within this sample, Cronbach’s alpha coefficients for component PRS subscales ranged between .80 and .93 (median .86) and between .64 and .92 (median .86) for the SRP subscales.
Substance abuse
Computerized records at the women’s methadone clinics were examined to obtain results of random urine toxicology screens (typically conducted at least twice a month) for substance use.
Results
Data reduction and descriptive data
One of the instruments used in this study yields a composite variable combining subscale scores (i.e., maltreatment risk from the PARQ5). To avoid Type I errors in subsequent analyses, we also examined the value of combining subdomains from other instruments that were strongly interrelated. Simple correlations revealed that high conceptual and empirical overlap occurred in two cases (r = .60 for each pair): the Internalizing and Externalizing composites from the BASC-PRS, and the Involvement and Communication subscales from the PCRI. These pairs of scores were thus combined into composites labeled Child Maladjustment and Affective Interactions, respectively, for further analyses.
Means and standard deviations on all outcome variables measured at baseline are presented in Table 2, separately for women enrolled in RPMG and those receiving only drug counseling (henceforth referred to as DC). Correlations among all outcome variables are presented in Table 3.
Table 2.
Means and standard deviations on parenting and psychosocial adjustment variables: Baseline assessments
| RPMGa | DCb | |||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| Parenting | ||||
| Mothers re: self | ||||
| Maltreatment riskc | 97.8 | 21.2 | 101.9 | 19.3 |
| Affective interactiond | 74.2 | 8.2 | 69.3 | 10.7 |
| Instrumental interaction | ||||
| Limit setting | 46.3 | 10.1 | 45.1 | 8.4 |
| Autonomy | 40.6 | 8.3 | 38.6 | 10.6 |
| Children re: mother | ||||
| Maltreatment riskc | 106.2 | 27.0 | 111.1 | 28.7 |
| Psychosocial adjustment | ||||
| Mothers re: self | ||||
| Parenting satisfaction | 49.0 | 7.9 | 42.8 | 11.7 |
| Parenting support | 42.3 | 10.1 | 42.4 | 9.0 |
| Depressive symptoms | 9.6 | 6.8 | 8.8 | 7.0 |
| Mothers re: child | ||||
| Child maladjustmente | 326.3 | 64.1 | 300.3 | 46.4 |
| Children re: self | ||||
| Clinical maladjustment | 46.7 | 7.9 | 52.5 | 7.0 |
| Personal adjustment | 49.6 | 8.2 | 43.5 | 11.6 |
| School maladjustment | 46.9 | 6.0 | 50.1 | 8.6 |
Note: n = 52 mothers and 24 children. Scores that are in standardized form (T scores, mean 50) are italicized.
Mothers who received RPMG plus standard drug counseling.
Mothers who received drug counseling alone.
Derived from PARQ subscales.
Derived from PCRI Involvement and Communication subscales.
Derived from BASC Internalizing and Externalizing subscales.
Table 3.
Intercorrelations among outcome variables: Baseline assessments
| Subscales | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Maltreatment risk—Ma | |||||||||||
| 2. Maltreatment risk—Ca | .31 | ||||||||||
| 3. Affective interactions—Mb | −.42** | −.19 | |||||||||
| 4. Limit setting—M | −.49** | −.03 | .45** | ||||||||
| 5. Autonomy—M | −.16 | .22 | −.05 | .19 | |||||||
| 6. Parenting satisfaction—M | −.56** | −.15 | .50** | .56** | .23† | ||||||
| 7. Parenting support—M | −.14 | −.19 | .08 | .40** | −.12 | .20 | |||||
| 8. Depressive symptoms—M | −.01 | .10 | −.08 | −.14 | .31* | .02 | −.47** | ||||
| 9. Child maladjustment—Mc | .20 | .15 | −.19 | −.45** | .10 | .04 | −.19 | .19 | |||
| 10. Clinical maladjustment—C | .24 | .54** | −.35† | −.33† | −.09 | −.27 | −.29 | .10 | .12 | ||
| 11. Personal adjustment—C | −.24 | −.60** | .60** | .22 | −.09 | .25 | .16 | −.04 | −.31 | −.51** | |
| 12. School maladjustment—C | .02 | .26 | −.44* | −.21 | −.10 | −.07 | −.16 | .24 | .14 | .53** | −.59** |
Derived from PARQ subscales: M, mother report; C, child report.
Derived from PCRI Involvement and Communication subscales.
Derived from BASC Internalizing and Externalizing subscales.
p < .10.
p < .05.
p < .01.
Characteristics of dropouts
To detect potential differences between treatment completers and those who left prior to completion, we conducted t tests on all baseline measures for each condition. There were no significant differences between groups within the RPMG condition. Within the DC condition, significant differences favoring the dropouts occurred in three of the seven outcome domains (affective interaction, limit setting, and parental support). These results must be interpreted with caution, however, due to the low number of mothers who left treatment (n = 4).
Analyses of covariance on central outcomes
Analyses of covariance (ANCOVAs) were conducted to examine outcomes among the mothers receiving RPMG versus mothers receiving DC alone across parenting and psychosocial domains. Repeated measures analyses of variance were considered inappropriate because preliminary analyses showed that, despite randomization to treatment, RPMG and drug-counseling groups significantly differed on several baseline measures (a common occurrence in small to moderate sample sizes; see Cohen & Cohen, 1983; Cook & Campbell, 1979; Kazdin, 1998). Prior to conducting the ANCOVAs, the presence of Treatment × Covariate interactions was ruled out. Separate ANCOVAs were conducted at the end of treatment and follow-up because the latter involved a smaller sample size.
Because the assessments focused explicitly on RPMG treatment targets and we predicted that mothers receiving this intervention would show improvements on these, we used a one-tailed significance test (see Kazdin, 1998). In addition, an effect size (d) of approximately .40 or greater was considered to reflect meaningful differences in functioning. Cohen (1988) has noted that even in the absence of statistical significance, effect sizes (d) approximating .40 represent moderate between-group differences and those approaching .80 represent substantial differences.
Results of the analyses of covariance are presented in Table 4. In this table, we present mean scores at posttreatment and follow-up, which have been adjusted for baseline values in each treatment condition (RPMG + DC, vs. DC alone). Thus, values indicate how well the groups were each doing at posttreatment and follow-up, with means adjusted for baseline differences.
Table 4.
Analyses of covariance for posttreatment and follow-up outcomes
| Posttreatment | Follow-Up | |||||||
|---|---|---|---|---|---|---|---|---|
| Adjusted Means |
Effect Sizea |
Adjusted Means |
Effect Size |
|||||
| RPMG | DC | F Ratio | RPMG | DC | F Ratio | |||
| Parenting | ||||||||
| Mothers re: self | ||||||||
| Maltreatment riskb | 94.9 | 107.0 | 3.77* | .54 | 90.3 | 102.4 | 3.77* | .57 |
| Affective interactionc | 77.4 | 70.4 | 11.66*** | .94 | 77.9 | 73.6 | 3.42* | .54 |
| Instrumental interaction | ||||||||
| Limit setting | 46.4 | 47.0 | .08 | .08 | 46.6 | 47.8 | .44 | .20 |
| Autonomy | 39.5 | 40.5 | .21 | .13 | 38.9 | 41.4 | 1.29 | .33 |
| Children re: mother | ||||||||
| Maltreatment risk | 91.9 | 108.0 | 4.62* | .88 | 91.1 | 96.7 | .43 | .27 |
| Psychosocial adjustment | ||||||||
| Mothers re: self | ||||||||
| Parenting satisfaction | 50.5 | 46.0 | 3.06* | .49 | 51.4 | 48.5 | 1.48 | .35 |
| Parenting support | 44.1 | 44.2 | .00 | .00 | 45.3 | 43.3 | .52 | .21 |
| Depression | 6.7 | 8.8 | 1.65† | .36 | 6.0 | 7.6 | .95 | .28 |
| Mothers re: child | ||||||||
| Child maladjustmentd | 303.6 | 321.4 | .81 | .29 | 286.1 | 313.5 | 1.78† | .45 |
| Children re: self | ||||||||
| Clinical maladjustment | 43.6 | 45.1 | .30 | .22 | 42.7 | 45.0 | .92 | .39 |
| Personal adjustment | 51.0 | 46.5 | 1.66† | .53 | 50.9 | 52.3 | .37 | .25 |
| School maladjustment | 47.3 | 45.3 | .29 | .22 | 44.6 | 44.8 | .00 | .00 |
Note: n = 52 mothers, 24 children at posttreatment; 47 mothers and 24 children at follow-up. All means in italics represent T scores (mean 50).
Effect size (d) of .20 is considered small, .40 moderate, and .80 large (Cohen, 1988).
Derived from PARQ subscales.
Derived from PCRI Involvement and Communication subscales.
Derived from BASC Internalizing and Externalizing subscales.
p < .10, one-tailed.
p < .05, one-tailed.
p < .001, one-tailed.
At the end of the treatment period, RPMG mothers displayed significantly lower maltreatment risk scores than DC mothers based on reports of both mothers and children, with effect sizes in the moderate to large range (d = .54 and .88, respectively). At follow-up, group differences were significant on mothers’ self-reported maltreatment risk (d = .57) but were nonsignificant on children’s reports of mothers’ maltreatment risk (d = .27).
RPMG mothers fared significantly better than DC mothers on Affective Interactions at both posttreatment (d = .94) and follow-up (d = .54). Conversely, no significant differences were found on Instrumental behaviors; neither group showed much improvement over time on either Limit Setting or Autonomy.
In the domain of psychosocial adjustment, RPMG mothers fared significantly better than DC mothers at the end of treatment on satisfaction with their roles as parents (d = .49) and showed marginally lower levels of depressive symptoms (d = .36) as well. By the 6-month follow-up, RPMG mothers continued to show modest advantages in parental satisfaction and depression (d = .35 and .28, respectively), although group differences at this time were not statistically significant. No differences were found on perceptions of support in the parental roles at either the posttreatment or follow-up assessment.
Finally, although not significantly different, small to moderate effect sizes at posttreatment and follow-up indicated that RPMG mothers viewed their children’s maladjustment as somewhat less severe than the DC mothers (d = .29 and .45, respectively). On children’s psychosocial adjustment self-reports, effect sizes ranged from .22 to .53, again demonstrating small to moderate effects favoring the children of RPMG mothers.
Analyses involving other outcome variables
We did not consider retention in treatment to be a valid outcome variable in this pilot study because of different attendance requirements in each condition: DC mothers were required by the clinics to attend all their counseling groups, whereas attendance in RPMG was entirely voluntary. Despite these varying requirements, we found comparable retention rates across the conditions, with 86% mothers completing RPMG and 83% remaining in their DC groups.
Treatment group differences in drug use over time were examined using a random-effects probit regression model. This analysis was considered most appropriate given the capacity to model data across multiple time points, even with incomplete data for some subjects (e.g., due to missed appointments) and uneven gaps between data points representing time intervals (see Hedeker & Mermelstein, 1996).6 Because the outcome variable was binary (presence vs. absence of drug during 1-month period), a random-intercept probit regression model was used and all analyses were run using MIXOR, an analysis program for mixed effects ordinal probit and logistical regression (Hedeker & Gibbons, 1996). For the 13 time points considered in the analyses (baseline and 12 subsequent 1-month intervals), data on average, were available for a total of 11 points among women in this sample.
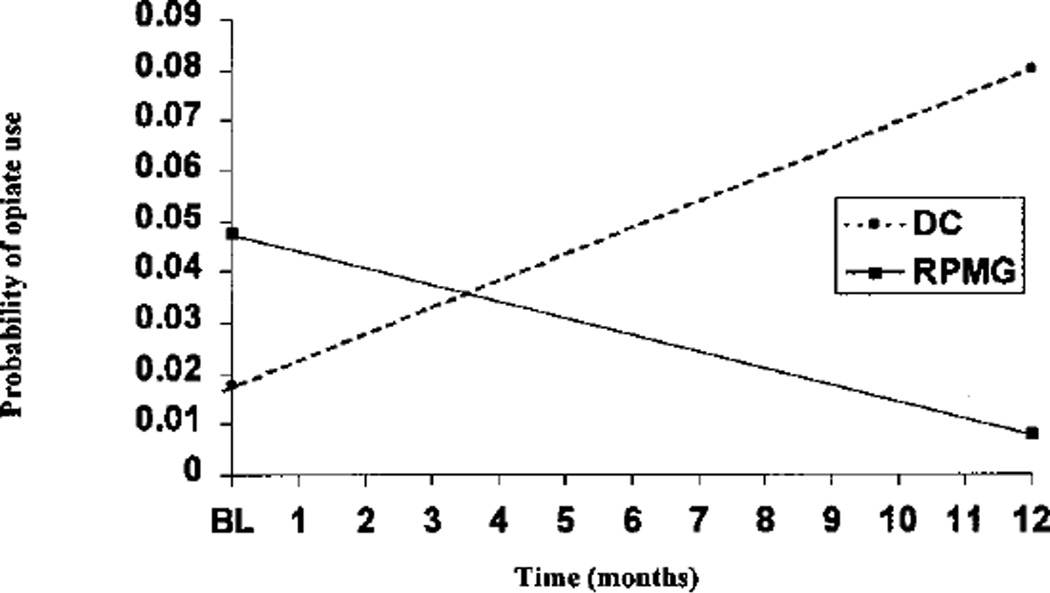
Separate analyses were conducted for the use of opiates, the primary drug for which the women were in treatment, and for cocaine, commonly used among patients in methadone maintenance (Brooner, King, Kidorf, Schmidt, & Be-gelow, 1997; Kosten, Gawin, Kosten, & Rounsaville, 1992; Kreek, 1997). Results are displayed in Table 5. With opiate use as the outcome variable, significant results were obtained for the main effect of time (z = 1.93, p < .05) and for the Treatment Group × Time interaction (z = 3.03, p < .01). The latter finding, displayed graphically in Figure 1, indicated that the probability of opiate use across time decreased for the RPMG group while it increased for the DC group. With cocaine use as the dependent variable, the main effect of time was significant (z = −2.29, p < .05). The Treatment × Time interaction, however, was not significant; RPMG and drug-counseling mothers showed comparable decreases in probability of cocaine use over time.
Table 5.
Results of random-effect regression for opiate and cocaine use
| Opiate | Cocaine | |||||
|---|---|---|---|---|---|---|
| Parameter | Estimate | SE | z | Estimate | SE | z |
| Intercept (at Time 0) | −2.10 | 0.39 | −5.37** | −1.60 | 0.26 | −6.14** |
| Time (per 1 month) | 0.06 | 0.03 | 1.93* | −0.08 | 0.04 | −2.29* |
| Group (DC vs. RPMG) | 0.43 | 0.46 | .95 | −0.43 | 0.29 | −1.50 |
| Group × Time | −0.12 | 0.04 | 3.03** | 0.01 | 0.04 | .25 |
Note: n = 50; no records were available for 2 of the 52 women in the sample.
p < .05, one-tailed.
p < .01, one-tailed.
Figure 1.
Probability for opiate use by treatment group across time (n = 50).
Therapist adherence and treatment discriminability
In developing the Therapist Adherence Rating Scale, we identified a pool of 16 items at the outset which represented the essential therapeutic components of RPMG (12 items) and standard drug counseling (4 items). Detailed scoring instructions were developed for each of these items, along with illustrative examples. Using these materials, two raters, each experienced clinicians themselves and both unaware of the purposes of this research, were trained to rate videotaped therapists participating in the study on each item. The raters then independently observed fresh videotapes of therapists conducting RPMG and DC sessions, rating each of the 16 items on a 5-point Likert scale, for the frequency and intensity with which each item was manifested.7 Overall scores for each subscale were obtained by computing the ratio of total points scored on the Likert scale to the total number of points possible (60 for the RPMG scale, 20 for the DC scale) and then converting this ratio to one with a denominator of 10, to ease interpretation and comparison of scale scores.
Interclass correlations were calculated to represent interrater reliability, using the two-way formula (Shrout & Fleiss, 1979) and with raters considered to be fixed rather than random effects. These calculations were based on independent ratings provided by two raters, each of whom rated 10 therapy sessions. Of the 16 items originally selected for the scale, 4 had interclass correlations below .50 and were considered unreliable. The remaining 12 items comprised the final scale (Table 6).
Table 6.
Therapist adherence rating scale items
| Item | Description |
|---|---|
| RPMG subscale | |
| 1. Warmth/interest | Nonverbal indication of therapist’s concern and interest |
| 2. Empathic understanding | Accurate verbal reflection of affective experience |
| 3. Foster insight | Exploratory approach to addressing problematic situation |
| 4. Foster relational skills | Examine issues concerning interpersonal relationships |
| 5. Foster parenting skills | Examine issues concerning parenting |
| 6. Maintain focus | Maintain discussion focus on session topic |
| 7. Paraphrase succinctly | Identify and clearly state core themes of discussion |
| 8. Appropriate boundaries | Maintain structure, order, and professional stance |
| DC subscale | |
| 1. Expert stance | Therapist assumes expert role as an authority on all issues |
| 2. Confrontational strategies | Direct/explicit questions and probes about drug use |
| 3. Focus on abstinence | Maintain focus on abstinence goals and strategies |
| 4. Focus on drug-free lifestyle | Maintain focus on substitute activities for drug use |
To determine the internal consistency of the two subscales, Cronbach’s alphas were calculated for the RPMG and DC subscales. They were .93 and .80, respectively, indicating excellent internal consistency.
Once acceptable psychometric properties were ascertained, therapists participating in this study (two RPMG and four DC) were each rated on the Therapist Adherence Scale The RPMG therapists rated were the two clinical psychologists who served as senior therapists in all RPMG groups, and the four drug counselors rated were those who conducted the majority of drug counseling sessions at the clinics. Approximately eight sessions of each RPMG therapist and three sessions of each DC clinician were randomly selected for observation and rating.
Therapist adherence and discriminability were determined by first calculating individual therapist mean scores on the RPMG and DC subscales, respectively, and then computing overall means for each group of therapists for each subscale. Substantial differences were found, with RPMG therapists and DC clinicians respectively obtaining means of 7.4 (SD = .74) and 2.9 (SD = .76) on the RPMG subscale and means of 4.4 (SD = 1.1) and 6.4 (SD = 1.9) on the DC subscale. Differences between both pairs of means were statistically significant, F (1, 23) = 78.6 and 39.0, respectively, p < .0001, indicating that therapists conducting the two treatments did in fact offer distinct therapeutic ingredients.
Summary
Results of this pilot study were promising in terms of both the potential effectiveness of RPMG and its apparent discriminability from standard drug-counseling interventions. As compared to mothers receiving standard drug counseling alone, those who received RPMG as a supplemental treatment fared more positively on most targeted parenting domains, as reported by the mothers as well as their children. In addition, data obtained via ratings of videotaped sessions indicate that the two interventions did differ substantively in terms of major therapeutic components.
Discussion
While addicted mothers’ parenting problems are typically viewed as both serious and in tractable, results of this study suggest that supportive, developmentally informed group psychotherapy can foster women’s engagement in treatment and also potentially reduce maladaptive parenting across multiple domains. Moreover, the benefits of such psychotherapy can apparently “spill over” to result in reduced levels of substance use as well.
Among the most simple yet most encouraging results of this study was the 86% retention rate in the voluntary RPMG intervention. Whereas a range of sanctions were associated with the women’s failure to attend regular drug-counseling sessions at the methadone clinics, they faced no clinic-based repercussions if they were to drop out of RPMG. Yet four of every five women who enrolled initially did remain until treatment completion. These findings are in marked contrast with prior reports which have typically indicated dropout rates ranging between 35 and 50% for heroin-addicted women in substance-abuse treatment research (see Chang et al., 1992; Davis, 1994; Gainey, Catalano, Haggerty, & Hoppe, 1995; Ravndal & Vaglum, 1994; Stanton & Shadish, 1997).
The relatively low attrition rates in this study may partly reflect our use of a graduated schedule to reimburse participants, wherein mothers received incrementally higher payments for completing assessment packages as the study progressed. In addition, however, retention in the RPMG groups may have been promoted by the nurturing therapeutic environment provided. Throughout the study, mothers frequently referred to the supportive and nonconfrontational nature of the group as a primary incentive for their continued participation in groups.
In terms of targeted outcomes, participation in RPMG was associated with lower maltreatment risk as reported by both mothers and their children at posttreatment, as well as by maternal report at follow-up. The importance of these findings is underscored by the substantial evidence that (a) as a group, substance-abusing mothers—who often seriously lack emotional and financial supports—are at high risk for child maltreatment (Hawley & Disney, 1992) and (b) exposure to chronic maltreatment exacerbates children’s risks for negative outcomes, with adaptation patterns showing increasing deterioration over time (Chaffin, Kelleher, & Hollenberg, 1996; Cicchetti & Lynch, 1995; Mayes & Bornstein, 1997).
Aside from reductions in maltreatment risk, RPMG mothers reported robust and sustained improvements in affective interactions with their children and in overall feelings of parental satisfaction at posttreatment. As amply documented in the child development literature (e.g., Bowlby, 1969; Cicchetti & Toth, 1997; Cicchetti, Toth, & Lynch, 1995), the absence of negative parental behaviors, such as those connoting neglect or rejection, is a critical though by no means sufficient condition for children’s long-term psychological health. Equally crucial is exposure to positive parenting, as might be reflected in mothers’ everyday expressions of interest in and empathy toward their children.
In contrast to the noteworthy improvements on maltreatment risk, affective interactions, and overall maternal satisfaction, mothers in both treatment conditions showed little change on both facets of instrumental parenting: limit setting and autonomy. While limit-setting scores fell within normal ranges, those on autonomy averaged a full standard deviation below normative values at baseline, treatment completion, as well as follow-up. The consistently low autonomy scores may, in some instances, reflect a high degree of maternal protectiveness toward children living in neighborhoods replete with crime and violence (Luthar, 1999). In addition, however, they might partially reflect mothers’ discomfort with separation from their children. It has been argued that given the dearth of personal supports in their everyday lives, many addicted women find it difficult to promote their children’s emotional independence (Levy & Rutter, 1992). In future work, it would be useful to examine more closely both the connotations and repercussions of the low autonomy that appears to characterize heroin-addicted mothers’ parenting styles.
Patterns of drug use
Notwithstanding that RPMG is a treatment designed for drug-abusing women, the major therapeutic components that define this treatment do not include strategies specifically targeting substance-use behaviors. The decision not to explicitly emphasize drug use was made early in the development of this intervention and was based on two factors. The first encompassed beliefs that drug-abusing women reflect a constellation of problems of which their addiction represents only one part (see Haller, Knisely, Dawson, & Schnoll, 1993; NCASA, 1996; Rounsaville & Kleber, 1986) and that their psychiatric and interpersonal difficulties warrant at least as much therapeutic attention as do problems of maintaining abstinence (Brooks & Tseng, 1995; Haller et al., 1993; Hawley, Halle, Drasin, & Thomas, 1995; Howard, Beckwith, Espinosa, & Tyler, 1995; Luthar, Cushing, et al., 1997; Mathias, 1997). Second, RPMG was designed for women already in treatment for drug use, and most drug-treatment programs focus heavily on substance use and abstinence with less attention to intrapsychic and interpersonal issues (Finkelstein, 1994; Luthar & Walsh, 1995; McMahon & Luthar, 1998; Osher, 1996). Our effort, therefore, has been to supplement the vital and concerted efforts made by drug-treatment clinics to promote abstinence by centrally targeting those domains of need that typically remain neglected in drug counseling.
Decisions in this regard are substantiated by our findings on reductions in RPMG mothers’ substance use levels. As compared to mothers receiving standard counseling alone, RPMG participants showed significantly greater improvements in opioid use as ascertained by highly reliable data sources: random urine checks conducted by the clinics. These findings lend strong support to arguments by Brunswick and colleagues (1991, 1992) that working with substance-abusing women on their interpersonal and psychological needs can have substantial spillover effects on their capacities to abstain from drug use over time.
Caveats and limitations
The absence of observational data on changes in mother–child interactions, recommended (though rarely used) in assessing parenting interventions (see Catalano, Haggerty, Gainey, & Hoppe, 1997; Hawley & Disney, 1992; Mayes & Bornstein, 1995; Webster–Stratton, 1994, 1996; Webster–Stratton & Hammond, 1997), could be viewed as a limitation of this study. Such observations were logistically difficult here due to the wide age span of the mothers’ children—a deliberate decision in designing the intervention.8 Moreover, the absence of observational data must be weighed against evidence (albeit based on a small sample) that the children themselves reported significant changes in their mothers’ behaviors. Children’s own perceptions are arguably at least as relevant as those of “objective observers” in determining the overall quality of maternal–child interactions.
While several group differences were statistically nonsignificant—possibly due to the limited sample size—it should be noted that in comparison with other interventions for substance abusers, average RPMG effect sizes at posttreatment (.39) and follow-up (.32) compare favorably. In a meta-analysis of 83 randomized clinical trials conducted to assess the efficacy of psychosocial interventions, Feingold, Carroll, Johnson, and Rounsaville (1998) found a mean posttreatment effect size (d) of .23 across all interventions for treatment efficacy. Further analyses based on type of control group indicated that studies with “less potent” control groups (including “treatment as usual,” as in this study) yielded effect sizes averaging only .11—approximately one third those achieved for RPMG.
Although promising, results of this pilot study cannot be viewed as definitive for several other reasons. First, the RPMG therapists’ manual underwent revisions throughout the 3-year study, such that mothers who enrolled early in the study received treatments similar, but not identical, to later-enrolling participants. Second, we know little about the degree of variability in the treatment received by women in the comparison group, because drug-counseling sessions, unlike RPMG meetings, were not all videotaped in this pilot research. Third, the sample of this study is not necessarily representative of methadone clinic populations in general (as suggested, e.g., by the greater proportion of Caucasian than minority mothers among our participants). Finally, our results may partly reflect varying “doses” of treatment across conditions, as mothers in the RPMG groups received this intervention in addition to all standard treatment that was available to the comparison group mothers. Each of these problems has been considered in a new randomized clinical-trials study with a relatively large sample (currently ongoing), in which we seek to provide more rigorous empirical evidence of the effectiveness of RPMG for both maternal and child outcomes.
Conclusions
Developmental psychologists concerned with interventions and social policies have long accepted the value of focusing on the “whole child,” rather than on individual aspects of children’s functioning in isolation from others (Bronfenbrenner, 1986; Cowen, 1994; Zigler, 1998; Zigler & Trickett, 1978). In parallel fashion, future therapeutic efforts with addicted mothers must move toward increased focus on the “whole parent” and strive for greater balance, with attention to multiple serious adversities (as well as salient strengths), rather than remaining overwhelmingly focused on issues of addiction and relapse prevention alone. Without question, managing addiction is of critical importance for maintaining gains in other spheres. However, there is a need for drug-treatment providers to give more consideration than has been conventionally accorded to the powerful intrapsychic and interpersonal stresses that heroin-using women contend with on an ongoing basis.
As future intervention approaches are expanded, therefore, it is critical that addicted mothers’ needs as women and as parents are explicitly considered in developing treatment plans. For individuals who attend substance-abuse clinics, access to mental health treatment within other service delivery systems is often seriously restricted by various factors including limited economic resources, lack of child care and transportation facilities, diverse institutional barriers, and, often, negative stereotyping by professionals with a limited understanding of drug abuse (McMahon & Luthar, 1998). If drug-abuse treatment providers were to provide more direct attention to these women’s psychological and parenting concerns, this could not only improve the mothers’ personal functioning—including refractory problems of substance abuse—but could also serve critical preventive functions for many of their highly vulnerable children over the long term.
Acknowledgments
This research was supported by Research Scientist Development Award K21-DA00202, and by P50-DA09241, RO1-DA10726, and RO1-DA11498. Deborah Boltas contributed substantially to the design and implementation of the intervention described here. Our sincere thanks to Bruce Rounsaville of Yale, Rosalyn Liss of the APT Foundation, and Doreen Czechowicz of NIDA for their ongoing support of this work. We also gratefully acknowledge assistance from Kathleen Carroll, Thomas McMahon, Cindy Morgan, Laurel Bidwell, Charla Nich, and other members of the Psychotherapy Center at the Yale Substance Abuse Center.
Footnotes
Portions of this work were presented at the Rochester Symposium on Developmental Psychopathology, Approaches to Prevention and Intervention, Rochester, NY, November 13–16, 1996.
Whereas the overall approach in RPMG is nondirective, therapists occasionally make active, directive interventions (e.g., if harm to their children or to the mothers themselves seems imminent).
Baseline assessment indicated that all mothers who reported subjective distress in parenting did in fact reflect problems (e.g., in terms of clinical cutoff scores) on one or more domains measured.
This was achieved by adjusting the randomization odds such that subjects had a two-thirds chance of being assigned to RPMG.
Treatment completers were considered those who continued to attend throughout the 24 weeks, missing no more than two consecutive sessions and attending at least half of all group meetings.
The four PARQ domains were in fact highly correlated (median r = .67 for mothers and .66 for children).
Random-effects regression models (RRMs) were not considered appropriate to analyze major psychosocial outcomes (Table 4) for several reasons (see Gibbons et al., 1993; Laird & Ware, 1982; Tate & Hakanson, 1993). First, having only three repeated observations can seriously constrain the reliability of slope estimates, particularly when outcomes have large short-term variability such as feelings of depression; (Tate & Hakanson, 1993). Second, our sample size, particularly for child assessments, was small, and RRM requires comparatively large samples (Gibbons et al., 1993). Third, our data for psychosocial outcomes were synchronous; assessments were obtained across fixed times with equal intervals of 6 months each and equivalent end points, rendering irrelevant one of the greatest advantageous of this technique—the ability to deal with unequal time intervals.
Such considerations notwithstanding, exploratory RRMs were conducted with major outcome variables in Table 4. As is typically the case (Nich & Carroll, 1997), findings were similar to those from the analyses of variance. Effects displayed as significant in Table 4 were generally replicated as having significant effects in Treatment Group × Time interactions within the RRMs.
Additional details on scoring procedures are available from the authors by request.
The decision to include mothers of children in a wide age range was guided by several considerations. First, most existing interventions for substance-abusing mothers target women with infants; mothers of children over 2 years represent a neglected group. Second, preventive interventions are critical not only for addicted mothers of young children but also for mothers of preteen or teen youth who are in a period of high risk for the onset of many deviant behaviors (see Luthar et al., 1998). Third, using a relatively wide age span of children allows mothers not only to gain a better understanding of their children’s current functioning but also to be prepared for the continuum of changes as their children grow older. Finally, among the most efficacious ways to influence the parenting behavior of opiate addicted mothers is via direct feedback and support of their peers (e.g., Stinchfield, Owen, & Winters, 1994), and including mothers of children encompassing a broad age span allows for exchange of a relatively wide range of parenting perspectives.
References
- Amaro H, Hardy–Fanta C. Gender relations in addiction and recovery. Journal of Psychoactive Drugs. 1995;27:325–337. doi: 10.1080/02791072.1995.10471698. [DOI] [PubMed] [Google Scholar]
- Bauman PS, Dougherty FE. Drug-addicted mothers’ parenting and their children’s development. International Journal of the Addictions. 1983;18:291–302. doi: 10.3109/10826088309039348. [DOI] [PubMed] [Google Scholar]
- Beck AT, Beck RW. Screening depressed patients in family practice: A rapid technique. Postgraduate Medicine. 1972;52:81–85. doi: 10.1080/00325481.1972.11713319. [DOI] [PubMed] [Google Scholar]
- Black R, Mayer J. Parents with special problems: Alcoholism and opiate addiction. Child Abuse and Neglect. 1980;4:45–54. [Google Scholar]
- Bowlby J. Attachment: Vol. 1. Attachment and loss. New York: Basic Books; 1969. [Google Scholar]
- Braswell M, Seay T. Approaches to counseling and psychotherapy. 2nd ed. Prospect Heights, IL: Waveland Press; 1984. [Google Scholar]
- Bronfenbrenner U. Ecology of the family as a context for human development: Research perspectives. Developmental Psychology. 1986;22:723–742. [Google Scholar]
- Brooks JS, Tseng L-J. Maternal drug use, personality, child-rearing practices, and toddlers’ sadness. Psychological Reports. 1995;76:912–914. doi: 10.2466/pr0.1995.76.3.912. [DOI] [PubMed] [Google Scholar]
- Brooner RK, King VL, Kidorf M, Schmidt CW, Begelow GE. Psychiatric and substance use comorbidity among treatment-seeking opioid abusers. Archives of General Psychiatry. 1997;54:71–80. doi: 10.1001/archpsyc.1997.01830130077015. [DOI] [PubMed] [Google Scholar]
- Brunswick A, Lewis C, Messeri P. A life span perspective on drug use and affective distress in an African-American sample. Journal of Community Psychology. 1991;19:123–135. [Google Scholar]
- Brunswick AF, Messeri PA, Titus SP. Predictive factors in adult substance abuse: A prospective study of African-American adults. Washington, DC: American Psychological Association; 1992. [Google Scholar]
- Brunswick A, Titus S. Heroin patterns and trajectories in an African American cohort (1969–1990) In: Inciardi J, Harison L, editors. Drugs, health and social policy series: Vol. 6. Heroin in the age of crack-cocaine. Thousand Oaks, CA: Sage; 1998. pp. 77–108. [Google Scholar]
- Catalano R, Haggerty K, Gainey R, Hoppe M. Reducing parental risk factors for children’s substance misuse: Preliminary outcomes with opiate-addicted patients. Substance Use & Misuse. 1997;32:699–721. doi: 10.3109/10826089709039371. [DOI] [PubMed] [Google Scholar]
- Chaffin M, Kelleher K, Hollenberg J. Onset of physical abuse and neglect: Psychiatric, substance abuse, and social risk factors from prospective community data. Child Abuse & Neglect. 1996;20:191–203. doi: 10.1016/s0145-2134(95)00144-1. [DOI] [PubMed] [Google Scholar]
- Chang G, Carroll KM, Behr HM, Kosten TR. Improving treatment outcome in pregnant opiate-dependent women. Journal of Substance Abuse Treatment. 1992;9:327–330. doi: 10.1016/0740-5472(92)90026-k. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D, Lynch M. Failures in the expectable environment and their impact on individual development: The case of child maltreatment. In: Cicchetti D, Cohen DJ, editors. Developmental psychopathology: Vol. 2. Risk, disorder and adaptation. New York: Wiley; 1995. pp. 32–71. [Google Scholar]
- Cicchetti D, Toth SL. Transactional ecological systems in developmental psychopathology. In: Luthar SS, Burack JA, Cicchetti D, Weisz JR, editors. Developmental psychopathology: Perspectives on adjustment, risk, and disorder. New York: Cambridge University Press; 1997. [Google Scholar]
- Cicchetti D, Toth SL, Lynch M. Bowlby’s dream comes full circle: The application of attachment theory to risk and psychopathology. In: Ollendick TH, Prinz RJ, editors. Advances in clinical child psychology. Vol. 17. New York: Plenum Press; 1995. [Google Scholar]
- Cohen J, Cohen P. Applied multiple regression/correlation analysis for the behavioral sciences. Hillsdale, NJ: Erlbaum; 1983. [Google Scholar]
- Cohen LH. Measurement of life events. In: Cohen LH, editor. Life events and psychological functioning: Theoretical and methodological issues. Newbury Park, CA: Sage; 1988. pp. 11–30. [Google Scholar]
- Colten M. Attitudes, experiences, and self-perceptions of heroin-addicted mothers. Journal of Social Issues. 1982;38:77–92. [Google Scholar]
- Cook TD, Campbell DT. Quasi-experimentation: Design and analysis issues for field settings. Chicago: Rand McNally; 1979. [Google Scholar]
- Cowen EL. The enhancement of psychological wellness: Challenges and opportunities. American Journal of Community Psychology. 1994;22:149–179. doi: 10.1007/BF02506861. [DOI] [PubMed] [Google Scholar]
- Davis S. Drug treatment decisions of chemically-dependent women. The International Journal of the Addictions. 1994;29:1287–1304. doi: 10.3109/10826089409047943. [DOI] [PubMed] [Google Scholar]
- Davis SK. Chemical dependency in women: A description of its effects and outcomes on adequate parenting. Journal of Substance Abuse Treatment. 1990;7:225–232. doi: 10.1016/0740-5472(90)90045-r. [DOI] [PubMed] [Google Scholar]
- Dembo R, Williams L, Wish ED, Dertke M, Berry E, Getreu A, Washburn M, Schmeidler J. The relationship between physical and sexual abuse and illicit drug use: A replication among a new sample of youths entering a juvenile detention center. International Journal of Addictions. 1988;23:89–100. doi: 10.3109/10826088809056189. [DOI] [PubMed] [Google Scholar]
- Eliason MJ, Skinstad AH, Helene A. Drug/alcohol addictions and mothering. Alcoholism Treatment Quarterly. 1995;12:83–96. [Google Scholar]
- Feingold A, Carroll KM, Johnson D, Rounsaville BJ. Efficacy of psychosocial interventions with substance abusers: A meta-analysis. Paper presented at the 106th Annual Convention of the American Psychological Association; San Francisco. 1998. [Google Scholar]
- Finkelstein N. Treatment issues for alcohol- and drug-dependent pregnant and parenting women. Health & Social Work. 1994;19:7–15. doi: 10.1093/hsw/19.1.7. [DOI] [PubMed] [Google Scholar]
- Fullilove M, Fullilove R, Smith M, Winkler K, Michael C, Panzer P, Wallace R. Violence, trauma, and post-traumatic stress disorder among women drug users. Journal of Traumatic Stress. 1993;6:533–543. [Google Scholar]
- Gainey RR, Catalano RF, Haggerty KP, Hoppe MJ. Participation in a parent training program for methadone clients. Addictive Behaviors. 1995;20:117–125. doi: 10.1016/0306-4603(94)00053-2. [DOI] [PubMed] [Google Scholar]
- Gerard AB. Parent–Child Relationship Inventory (PCRI) manual. Los Angeles: Western Psychological Services; 1994. [Google Scholar]
- Gibbons RD, Hedeker D, Ilkin I, Waternaux C, Kraemer HC, Greenhouse JB, Shea MT, Imber SD, Sotsky SM, Watkins JT. Some conceptual and statistical issues in analysis of longitudinal psychiatric data: Application to the NIMH Treatment of Depression Collaborative Research Program dataset. Archives of General Psychiatry. 1993;50:739–750. doi: 10.1001/archpsyc.1993.01820210073009. [DOI] [PubMed] [Google Scholar]
- Gould J. A psychometric investigation of the standard and short form Beck Depression Inventory. Psychological Reports. 1982;51:1167–1170. doi: 10.2466/pr0.1982.51.3f.1167. [DOI] [PubMed] [Google Scholar]
- Grice D, Brady K, Dustan L, Malcolm R, Kilpatrick D. Sexual and physical assault history and posttraumatic stress disorder in substance-dependent individuals. American Journal on Addictions. 1995;4:297–305. [Google Scholar]
- Greif GL, Drechsler M. Common issues for parents in a methadone maintenance group. Journal of Substance Abuse Treatment. 1993;10:339–343. doi: 10.1016/0740-5472(93)90018-w. [DOI] [PubMed] [Google Scholar]
- Grossman J, Schottenfeld R. Pregnancy and Women’s Issues. In: Kosten T, Kleber H, editors. Clinician’s guide to cocaine addiction. New York: Guilford; 1992. pp. 374–388. [Google Scholar]
- Haller DL, Knisely JS, Dawson KS, Schnoll SH. Perinatal substance abusers: Psychological and social characteristics. Journal of Nervous & Mental Disease. 1993;181:509–513. doi: 10.1097/00005053-199308000-00006. [DOI] [PubMed] [Google Scholar]
- Hawley T, Disney E. Crack’s children: The consequences of maternal cocaine abuse. Social Policy Report: Society for Research in Child Development. 1992;4:1–23. [Google Scholar]
- Hawley TL, Halle TG, Drasin RE, Thomas NG. Children of addicted mothers: Effects of the “crack epidemic” on the caregiving environment and the development of preschoolers. American Journal of Orthopsychiatry. 1995;65:364–379. doi: 10.1037/h0079693. [DOI] [PubMed] [Google Scholar]
- Hedeker D, Gibbons RD. MIXOR: A computer program for mixed effects ordinal regression analysis. Computer Methods and Programs in Biomedicine. 1996;49:229–252. doi: 10.1016/0169-2607(96)01720-8. [DOI] [PubMed] [Google Scholar]
- Hedeker D, Mermelstein RJ. Application of random-effects regression models in relapse research. Addiction. 1996;91 Suppl.:S211–S229. [PubMed] [Google Scholar]
- Hollingshead AB, Redlich FC. Social class and mental illness. New York: Wiley; 1958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard J, Beckwith L, Espinosa M, Tyler R. Development of infants born to cocaine-abusing women: Biological/maternal influences. Neurotoxicology and Teratology. 1995;17:403–411. doi: 10.1016/0892-0362(94)00077-q. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Research design in clinical psychology. 3rd ed. Boston: Allyn & Bacon; 1998. [Google Scholar]
- Klerman GL, Weissman MM, Rounsaville BJ, Chevron ES. Interpersonal psychotherapy of depression. New York: Basic Books; 1984. [Google Scholar]
- Kosten TA, Gawin FH, Kosten TR, Rounsaville BJ. Gender differences in cocaine use and treatment response. Journal of Substance Abuse Treatment. 1993;10:63–66. doi: 10.1016/0740-5472(93)90100-g. [DOI] [PubMed] [Google Scholar]
- Kosten TR, Rosen MI, Schottenfeld R, Ziedonis D. Buprenorphine for cocaine and opiate dependence. Psychopharmacology Bulletin. 1992;28:15–19. [PubMed] [Google Scholar]
- Kreek MJ. Opiate and cocaine addictions: Challenge for pharmacotherapies. Pharmacology Biochemistry and Behavior. 1997;57:551–569. doi: 10.1016/s0091-3057(96)00440-6. [DOI] [PubMed] [Google Scholar]
- Laird NM, Ware JH. Random-effects models for longitudinal data. Biometrics. 1982;38:963–974. [PubMed] [Google Scholar]
- Levy SJ, Rutter E. Children of drug abusers. New York: Lexington; 1992. [Google Scholar]
- Lief N. The drug user as a parent: Intervening with special populations. International Journal of Addictions. 1985;20:63–97. doi: 10.3109/10826088509074829. [DOI] [PubMed] [Google Scholar]
- Luthar SS. Poverty and children’s adjustment. Thousand Oaks, CA: Sage; 1999. [Google Scholar]
- Luthar SS, Cushing G, McMahon TJ. Interdisciplinary interface: Developmental principles brought to substance abuse research. In: Luthar SS, Burack JA, Cicchetti D, Weisz JR, editors. Developmental psychopathology: Perspectives on adjustment, risk, and disorder. New York: Cambridge University Press; 1997. pp. 437–456. [Google Scholar]
- Luthar SS, Cushing G, Merikangas K, Rounsaville BJ. Multiple jeopardy: Risk/protective factors among addicted mothers’ offspring. Development and Psychopathology. 1998;10:117–136. doi: 10.1017/s0954579498001333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar SS, Glick M, Zigler E, Rounsaville BJ. Social competence among cocaine abusers: Moderating effects of comorbid diagnoses and gender. American Journal of Drug and Alcohol Abuse. 1993;19:283–298. doi: 10.3109/00952999309001619. [DOI] [PubMed] [Google Scholar]
- Luthar S, Suchman N. Developmentally informed parenting interventions: The Relational Psychotherapy Mothers’ Group. In: Cicchetti D, Toth S, editors. Rochester Symposium on Developmental Psychopathology. Vol. 9: Developmental approaches to prevention and intervention; Rochester, NY: University of Rochester Press; 1999. pp. 271–309. [Google Scholar]
- Luthar S, Suchman N, Boltas D. Relational Parenting Mothers’ Group: A therapist’s manual. New Haven, CT: Yale University; 1997. Unpublished manuscript. [Google Scholar]
- Luthar SS, Walsh K. Treatment needs of drug-addicted mothers: Integrated parenting psychotherapy interventions. Journal of Substance Abuse Treatment. 1995;12:341–348. doi: 10.1016/0740-5472(95)02010-1. [DOI] [PubMed] [Google Scholar]
- Luthar SS, Zigler E. Vulnerability and competence: A review of research on resilience in childhood. American Journal of Orthopsychiatry. 1991;61:6–22. doi: 10.1037/h0079218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackie–Ramos R, Rice J. Group psychotherapy with methadone maintained pregnant women. Journal of Substance Abuse Treatment. 1988;5:151–161. doi: 10.1016/0740-5472(88)90004-9. [DOI] [PubMed] [Google Scholar]
- Mathias R. Mental health problems of addicted mothers linked to infant careand development. NIDA Notes [online serial] 1997 January/February;12(1) Available via ftp. Host name: nida.nih.gov. Directory: NIDA_Notes/NN97Index.html/#Number1.
- Mayes LC, Bornstein MH. Developmental dilemmas for cocaine-abusing parents and their children. In: Lewis M, Bendersky M, editors. Mothers, babies and cocaine: The role of toxins in development. Hillsdale, NJ: Lawrence; 1995. pp. 251–272. [Google Scholar]
- Mayes LC, Bornstein MH. The development of children exposed to cocaine. In: Luthar SS, Burack J, Cicchetti D, Weisz JR, editors. Developmental psychopathology: Perspectives on adjustment, risk, and disorder. New York: Cambridge University Press; 1997. pp. 166–188. [Google Scholar]
- McGrath E, Keita GP, Strickland B, Russo N. Women and depression: Risk factors and treatment issues. Washington, DC: American Psychological Association; 1991. [Google Scholar]
- McMahon TJ, Luthar SS. Bridging the gap for children as their parents enter substance abuse treatment. In: Hampton RL, Senatore V, Gullota TP, editors. Substance abuse, family violence, and child welfare: Bridging perspectives: Vol. 10. Issues in children’s and families’ lives. Thousand Oaks, CA: Sage; 1998. pp. 143–186. [Google Scholar]
- Mercer D, Carpenter G, Daley D, Patterson C, Vopicelli J. Group drug counseling manual. University of Pittsburgh Medical Center; 1994. Unpublished manuscript. [Google Scholar]
- Mirin SM, Weiss RD, Griffin ML, Michael JL. Psychopathology in drug abusers and their families. Comprehensive Psychiatry. 1991;32:36–51. doi: 10.1016/0010-440x(91)90068-n. [DOI] [PubMed] [Google Scholar]
- Najavits LM, Griffin ML, Luborsky L, Frank A, et al. Therapists’ emotional reactions to substance abusers: A new questionnaire and initial findings. Psychotherapy. 1995;32:669–677. [Google Scholar]
- Najavits LM, Weiss RD, Shaw SR. The link between substance abuse and posttraumatic stress disorder in women: A research review. American Journal on Addictions. 1997;6:273–283. [PubMed] [Google Scholar]
- Najavits LM, Weiss RD, Shaw SR, Muenz LR. “Seeking safety”: Outcome of a new cognitive–behavioral psychotherapy for women with posttraumatic stress disorder and substance dependence. Journal of Traumatic Stress. 1998;11:437–456. doi: 10.1023/A:1024496427434. [DOI] [PubMed] [Google Scholar]
- National Center on Addiction and Substance Abuse at Columbia University (NCASA) Substance abuse and the American woman. New York: NCASA; 1996. [Google Scholar]
- Nich C, Carroll K. Now you see it, now you don’t: A comparison of traditional versus random-effects regression models in the analysis of longitudinal follow-up data from a clinical trial. Journal of Consulting and Clinical Psychology. 1997;65:252–261. doi: 10.1037//0022-006x.65.2.252. [DOI] [PubMed] [Google Scholar]
- Osher FC. A vision for the future: Toward a service system responsive to those with co-occurring addictive and mental disorders. American Journal of Orthopsychiatry. 1996;66:71–76. doi: 10.1037/h0080156. [DOI] [PubMed] [Google Scholar]
- Ravndal E, Vaglum P. Treatment of female addicts: The importance of relationships to parents, partners, and peers for the outcome. The International Journal of the Addictions. 1994;29:115–125. doi: 10.3109/10826089409047372. [DOI] [PubMed] [Google Scholar]
- Reynolds CR, Kamphaus RW. BASC: Behavioral Assessment System for Children. Circle Pines, MN: American Guidance Service; 1992. [Google Scholar]
- Rohner RP. Handbook for the study of parental acceptance and rejection. University of Connecticut at Storrs; 1991. Unpublished manuscript. [Google Scholar]
- Rohsenow DJ, Corbett R, Devine D. Molested as children: A hidden contribution to substance abuse? Journal of Substance Abuse Treatment. 1988;5:13–18. doi: 10.1016/0740-5472(88)90032-3. [DOI] [PubMed] [Google Scholar]
- Rounsaville B, Kleber H. Psychiatric disorders in opiate addicts: Preliminary findings on the course and interaction with program type. In: Meyers RE, editor. Psychopathology and addictive disorders. New York: Guilford Press; 1986. [Google Scholar]
- Shrout PE, Fleiss JL. Interclass correlations: Uses in assessing rater reliability. Psychological Bulletin. 1979;86:420–429. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- Stanton MD, Shadish WR. Outcome, attrition, and family–couples treatment for drug abuse: A meta-analysis and review of the controlled, comparative studies. Psychological Bulletin. 1997;122:170–191. doi: 10.1037/0033-2909.122.2.170. [DOI] [PubMed] [Google Scholar]
- Stinchfield R, Owen PL, Winters KC. Group therapy for substance abuse: A review of the empirical research. In: Fuhriman A, Burlingame GM, editors. Handbook of group psychotherapy: An empirical and clinical synthesis. New York: Wiley; 1994. pp. 458–488. [Google Scholar]
- Tate RL, Hakanson JE. Analyzing individual status and change with hierarchical linear models: Illustration with depression in college students. Journal of Personality. 1993;61:181–206. doi: 10.1111/j.1467-6494.1993.tb01031.x. [DOI] [PubMed] [Google Scholar]
- Tunving K, Nilsson K. Young female drug addicts in treatment: A 12 year perspective. Journal of Drug Issues. 1985;15:367–382. [Google Scholar]
- Wald R, Harvey SM, Hibbard J. A treatment model for women substance users. International Journal of the Addictions. 1995;30:881–888. doi: 10.3109/10826089509067013. [DOI] [PubMed] [Google Scholar]
- Wallace B. Crack cocaine: A practical treatment approach for the chemically dependent. New York: Brunner/Mazel; 1991. [Google Scholar]
- Wasserman DR, Leventhal JM. Maltreatment of children born to cocaine-abusing mothers. American Journal of Diseases of Children. 1993;147:1324–1328. doi: 10.1001/archpedi.1993.02160360066021. [DOI] [PubMed] [Google Scholar]
- Webster–Stratton C. Advancing videotape parent training: A comparison study. Journal of Consulting and Clinical Psychology. 1994;62:583–593. doi: 10.1037//0022-006x.62.3.583. [DOI] [PubMed] [Google Scholar]
- Webster–Stratton C. Early intervention with videotape modeling: Programs for families of children with oppositional defiant disorder or conduct disorder. In: Hibbs E, Jensen P, editors. Psychosocial treatments for child and adolescent disorders: Empirically based strategies for clinical practice. Washington, DC: American Psychological Association; 1996. pp. 435–474. [Google Scholar]
- Webster–Stratton C. From parent training to community building. Families in Society. 1997;78:156–171. [Google Scholar]
- Webster–Stratton C, Hammond M. Treating children with early-onset conduct problems: A comparison of child and parent training interventions. Journal of Consulting and Clinical Psychology. 1997;65:93–109. doi: 10.1037//0022-006x.65.1.93. [DOI] [PubMed] [Google Scholar]
- Weiner IB. Clinical methods in psychology. New York: Wiley–Interscience; 1983. [Google Scholar]
- Wells EA, Clark LL, Calsyn DA, Saxon AJ, Jackson TR, Wrede AF. Reporting of HIV risk behaviors by injection drug using heterosexual couples in methadone maintenance. Drug & Alcohol Dependence. 1994;36:33–38. doi: 10.1016/0376-8716(94)90007-8. [DOI] [PubMed] [Google Scholar]
- Werner EE, Smith RS. Overcoming the odds: High risk children from birth to adulthood. Ithaca, NY: Cornell University Press; 1992. [Google Scholar]
- Yalom I. The theory and practice of group psychotherapy. New York: Basic Books; 1985. [Google Scholar]
- Zackon F, McAuliffe W, Ch’ien MN. Recovery training and self-help: Relapse prevention and aftercare for drug addicts. Washington, DC: National Institute on Drug Abuse; 1994. [Google Scholar]
- Zigler E. A place of value for applied and policy studies. Child Development. 1998;69:532–542. [Google Scholar]
- Zigler E, Trickett PK. IQ, social competence, and evaluation of early childhood intervention programs. American Psychologist. 1978;33:789–798. [Google Scholar]