Summary
This study of 25 brains at the pontomedullary junction defined the different possible origins of the perforating arteries and lateral spinal arteries in relation to the posterior inferior cerebellar arteries (PICAs).
- If the PICA emerges from the common trunk of the AICA-PICA coming from the basilar artery, it never gives perforating arteries or a lateral spinal artery on the lateral surface of the brain stem but supplies blood to a part of the ipsilateral cerebellar hemisphere.
- If the PICA arises extradurally at C1, it never gives perforating arteries for the lateral surface of the brain stem, but it gives pial branches for the posterior surface of the medulla oblongata and is always the origin of the lateral spinal artery.
- If the PICA emerges in the intradural vertebral artery, it is the source of the perforating arteries for the lateral surface of the brain stem and of the blood supply of the ipsilateral cerebellum.
Key words: medulla oblongata, posterior inferior cerebellar artery (PICA), perforating arteries, lateral spinal artery
Introduction
The pontomedullary junction is supplied by the confluence of the vertebral and basilar arteries and the posterior inferior cerebellar arteries, where a large number of perforating arteries arise1,4,5,7-10,12-17. From these arteries also emerge the lateral spinal arteries responsible for the vascularization of the posterior surface of the medulla oblongata6,11.
This region is increasingly solicited in interventional neuroradiological procedures for embolization or arterial aneurysm, dissections, arteriovenous malformations, dural fistula or repair of an occlusive disease. The procedures sometimes require occlusion of an intradural segment of the vertebral artery, occasionally including the origin of the PICA.
Knowledge of the role of pre- and post-PICA segments of the intradural vertebral artery in pontine vascularization is therefore vital, and this anatomy should even be envisaged so as to anticipate the risk for lateral ischemia after endovascular treatment.
Material and Methods
For the present study, we used 25 brains from subjects who had given their bodies to medicine. These bodies had been injected with a formaldehyde solution 1-2 weeks before the study; the head was then sectioned at the lower cervical level. The vertebral and carotid arteries were then catheterized and, after washing with soapy water followed by acetone, neoprene 671 A (Safic-Alcan) was injected in 23 cases in a carotid artery until reflux was obtained in the other arteries that had been clamped. In two cases, the arteries were injected with a mixture of black or blue-gelatin India ink.
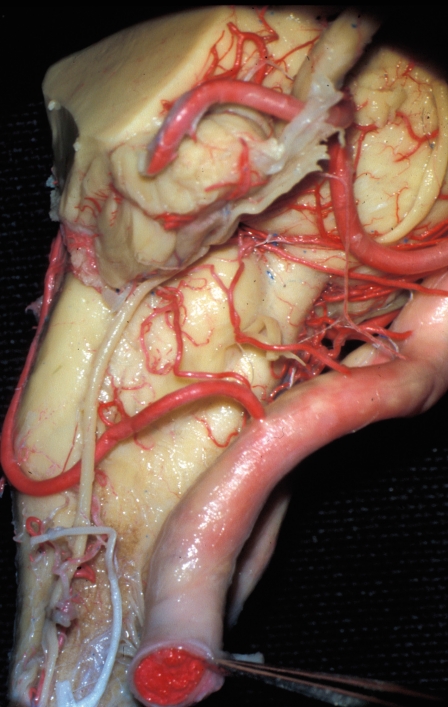
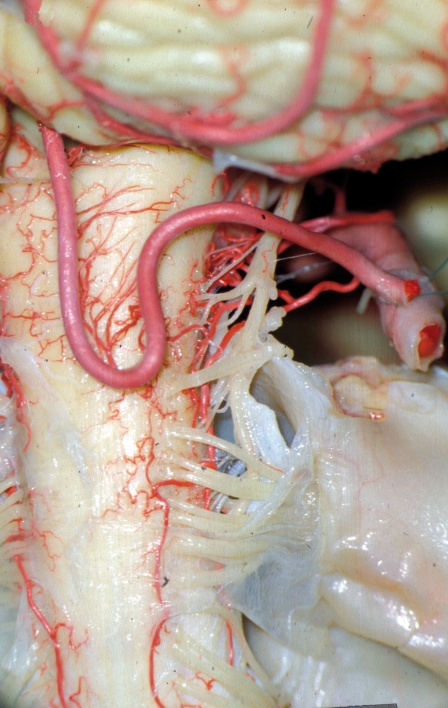
Figure 1.
Anterior view showing the three possibilities of PICA emergence; right, emergence of the vertebral artery; left, emergence of the basilar artery by the AICA-PICA common trunk and extradural emergence at C1.
We performed a cervical laminectomy and then a craniotomy. This allowed en bloc ablation of the head and of the upper part of the cervical medulla with resection of the two internal carotid arteries at the superior part of the two cavernous sinuses and the two vertebral arteries where they cross the dura mater. These brains were then studied and photographed in 3D with a surgical microscope (Wild Leitz, Nikon D80).
Anatomical Review
The inferior posterior cerebellar artery (PICA) most often emerges from the vertebral artery in its intradural segment, typically either 2 cm from the basilar artery or much more proximally, or always epidural from the vertebral artery. It can arise from the common trunk with the anterior inferior cerebellar artery (AICA) of the basilar artery.
Finally, it can emerge from the vertebral artery in its extracranial portion at different levels (C2-C3), the ascending pharyngeal artery, the occipital artery, or other embryonic arteries such as the hypoglossal or proatlantal arteries, and more exceptionally from the ascending cervical artery2. In its typical form, the artery has a tortuous course circling around or within the roots of the four last cranial nerves16. At this point, it gives perforating branches for the lateral part of the brain stem and the olive sharing the area with the branches coming from the basilar artery, the AICA, and the vertebral artery1,4,5,7-10,12-17. It then descends vertically and produces a first caudal loop on the anterior surface of the tonsil.
The artery then follows an ascending course between the dorsal surface of the medulla oblongata and the cerebellar tonsil, at the top of which a second convex loop runs rostrally, the cranial loop; this is where it divides into its two main branches: the vermian branch and the tonsillar branch.
The vermian branch classically feeds the inferior part of the vermis, i.e., the pyramid, the tuber, the uvula, and the nodule. The tonsillar branch supplies the lower part of the semilunar lobule, the caudal lobule and the biventer lobule2,8,16,17.
The study of these anatomical features and the region’s blood supply showed the extraordinary diversity of the PICA variations in clinical practice.
Results
This study of 25 brains (50 left and right sides) showed that the PICA was present in all cases; we counted 54. In 36 cases, the PICA emerged from the vertebral artery; in 11 cases, it arose with the AICA either from the basilar artery (ten AICA-PICA cases) or the vertebral artery (one PICA-AICA case); in seven cases, the PICA arose in the extradural portion of the vertebral artery in C1.
In five cases, there was a double artery because of the presence of an AICA-PICA common trunk, with a complementary PICA in four cases emerging from the vertebral artery and in one case an extradural C1 complementary artery. The study found four large arteries emerging from the vertebral artery that could give first a perforating artery for the lateral surface of the brain stem, then a meningeal artery for the cerebellar falx (which does not provide any branches for the cerebellum).
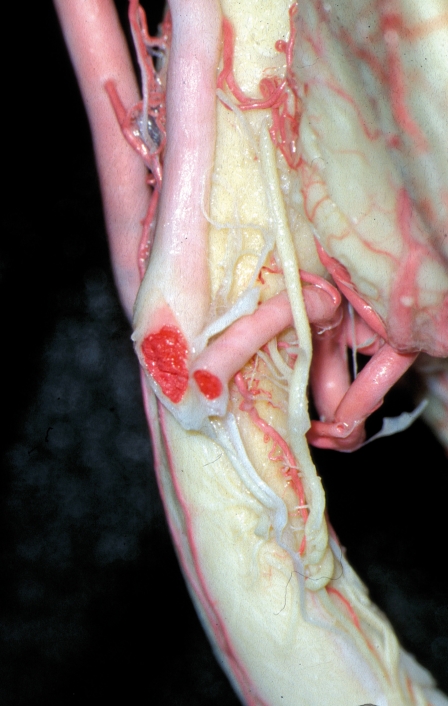
Figure 2.
Right lateral view showing the caudal loop of the PICA. No perforating arteries emerge from the vertebral artery under the PICA’s emergence.
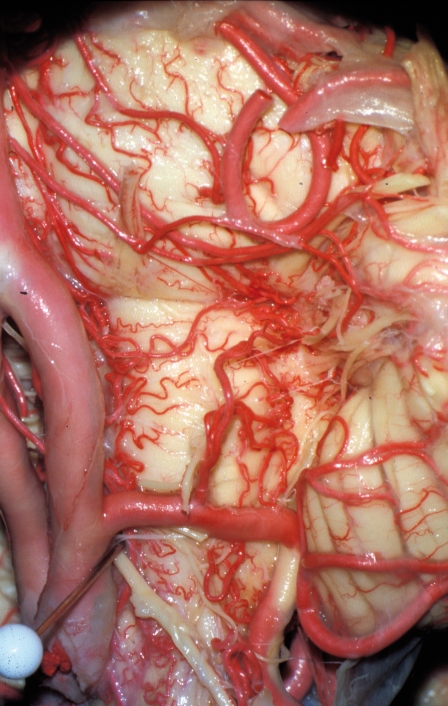
Figure 3.
Left lateral view. The PICA arises from an AICA-PICA common trunk. The perforating arteries for the olive and the lateral spinal artery emerge from the vertebral artery.
The lateral part of the brain stem, at the pontomedullary junction, produces the olivary area at the pontomedullary junction, limited above by the superior pontine sulcus, in front by the preolivary sulcus, and behind by the posterolateral sulcus and the origin of the accessory, vagus and glossopharyngeal nerves.
This region is supplied above by the perforating vessels from the AICA, in front by the branches coming directly from the basilar artery or the superior cerebellar artery, below by branches coming either from the vertebral artery or the PICA. In our study, none of the branches supplying the olive arose from the AICA-PICA common trunks or from the PICA arising from the extradural portion of the vertebral artery.
In all other cases, the PICA emerging from the vertebral artery gave rise to quite large caliber perforating vessels supplying the olive (mean, 2.2). In 48 cases out of 50, no perforating arteries arose from the vertebral artery between its entry in the dura mater and the PICA’s emergence.
In three cases, when the PICA emerged high, i.e., less than 2 cm from the basilar artery, we found a perforating vessel emerging from the PICA origin. In cases where the perforating arteries emerged from a proximal PICA, perforating vessels emerging from the vertebral artery could exist distally from the PICA’s origin and supply the lateral nucleus (mean, 1.3). When the PICA arose from the AICA-PICA common trunk of the basilar artery or in the extradural situation (C1-PICA), all the perforating branches emerged from the vertebral artery (mean 2.6).
Figure 4.
Left lateral view showing a C1-PICA from which arises the lateral spinal artery.
Figure 5.
Posterior view showing an example of bilateral C1-PICA with their long course in the cerebellomedullary cistern; note the emergence of the lateral spinal arteries from the two PICAs, left and right.
In summary
Three patterns were found:
1) the PICA was intradural and proximal and there could be a branch supplying the more distal brain stem arising from the vertebral artery or 2) the PICA was intradural and distal and it provided the branch for the brain stem, with more rarely another more proximal contribution, or 3) an AICA-PICA or an extradural PICA and the intradural vertebral artery provided the branch or branches for the brain stem following the two classical positions.
Anastomoses
The surgical microscope study of the olivary area showed that in approximately one case out of two there were more or less large caliber superficial anastomoses joining either the AICA branches and the basilar artery branches, the basilar and vertebral artery branches, the basilar artery branches and the PICA, or the AICA and PICA branches. This reflects a course that is nearly the same between the vessels whose names vary depending on the area supplied.
Lateral spinal artery
The lateral spinal artery can emerge classically either from the vertebral artery when the PICA is in the distal intradural position or in the PICA when it is in the lower proximal position or emerging extradurally (C1-PICA).
Figure 6.
Right lateral view showing a pial anastomosis at the surface of the olive between the PICA branches and the branches of the superior cerebellar artery arising from the basilar artery.
Figure 7.
Anterior view showing a large-caliber anastomosis between a hypoplastic vertebral artery (black pin) and a C1-PICA.
We found this artery 50 times. In nine cases, it emerged from the PICA with in seven cases the emergence of a C1-PICA. In the 41 other cases, it arose from the vertebral artery at the point where it entered the cranial cavity (36 cases) or even just before penetrating the dura mater (five cases): in these 41 cases, the PICA emerged from the distal vertebral artery of an AICA-PICA.
In all cases, we noted that this lateral spinal artery coursed between the posterior surface of the denticulate ligament in front and the anterior surface of the posterior roots of C1, C2, and C3 in the upper part parallel to the spinal accessory nerve, that it received anastomoses from the arteries of the C2, C3, and C4 roots, that it presented anastomoses on the medial line with the contralateral artery, and finally that it gave ascending branches for the posterior surface of the brain stem.
Vascularization of the posterior part of the medulla oblongata
In ten cases, we found that the PICA participated in supplying the medulla oblongata, supplying blood to the posterior cords or rather the inferior cerebellar peduncle. Here there were anastomoses with branches arising from the lateral spinal artery.
In seven cases out of ten, there was an extracranial PICA (C1 PICA), remarkable for the existence of an extremely low caudal loop, where normally the small pial arteries arise to supply blood to the posterior side of the brain stem (mean, 4.5).
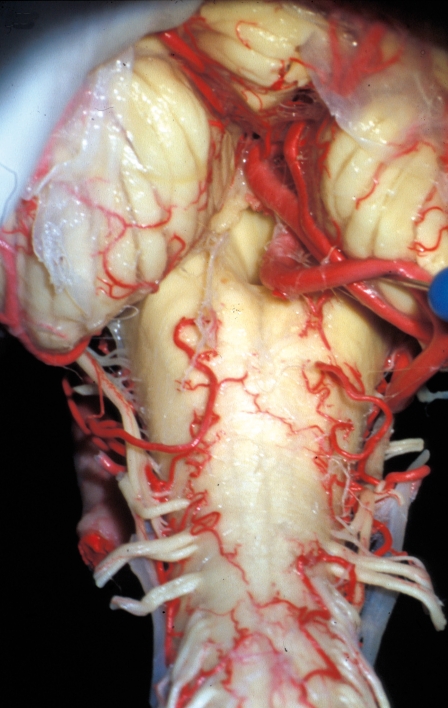
Figure 8.
Posterior view showing the blood supply of the posterior surface of the pontomedullary junction; right, the pial branches emerge from the PICA; left, the blood supply comes from the lateral spinal artery.
Figure 9.
Posterior view showing a C1-PICA giving the lateral spinal artery and the pial branches for the posterior surface of the medulla oblongata.
In summary
The more the PICA arose early in the vertebral artery, the more it supplied the posterior surface of the medulla oblongata and therefore ran toward the posterior surface of the brain stem. Likewise, the later it arose from the intradural vertebral artery, the more it supplied the anterior and lateral surfaces.
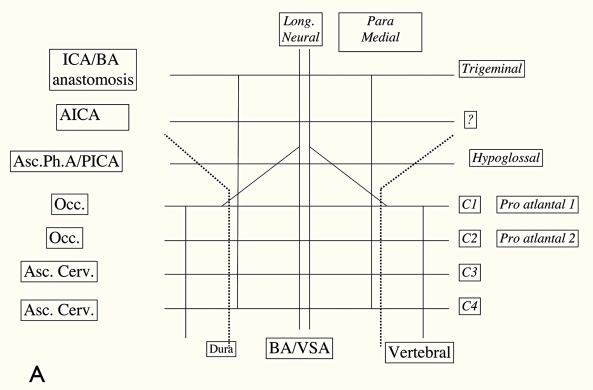
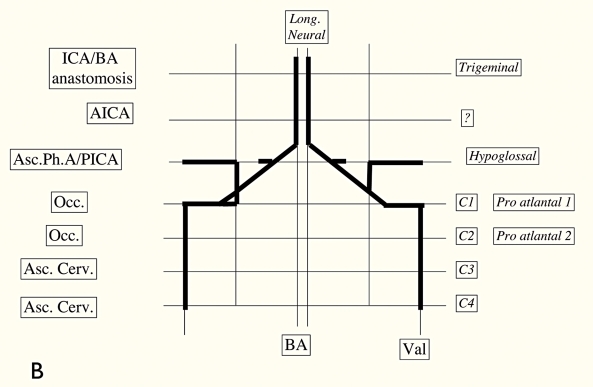
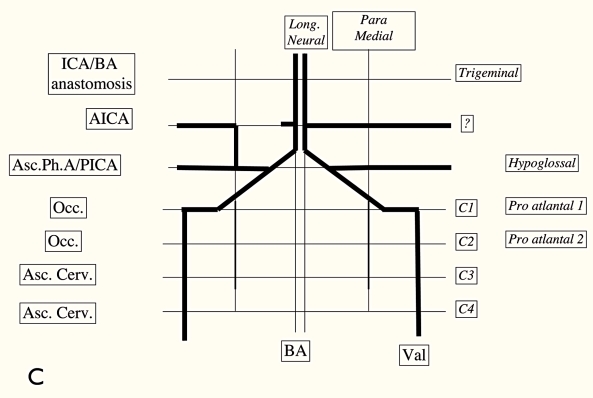
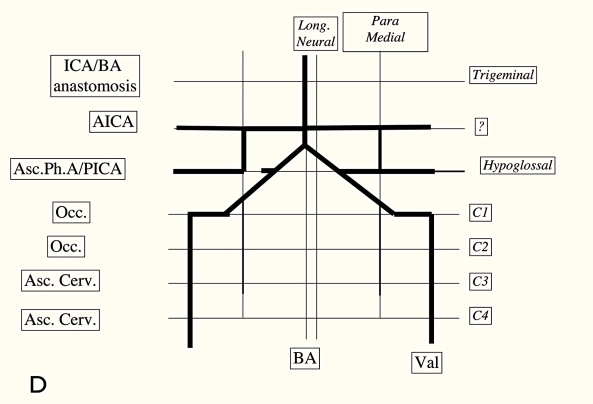
Figure 10.
A,B,C,D) Diagram showing the different possibilities of the emerging PICA (redrawn with modifications after 7).
Discussion
This study confirmed a certain number of classical notions already described in the literature. However, it specified that the length of the caudal loop classically located at the inferior edge of the tonsil, or slightly above, can be much longer. Every time we found an extremely low, tortuous, or long loop, it was a C1-PICA, i.e., a PICA arising extradurally.
Cerebellum blood supply is classically provided equally by the right and left PICAs. Notably, this blood supply can become bihemispheric, i.e., one of the posterior inferior cerebellar arteries can supply the entire vermis, the ipsilateral hemisphere, but even also part of the contralateral hemisphere.
This is seen when, for example, a PICA emerges from the vertebral side and an AICA-PICA arises from the other side of the basilar trunk: the vermis blood supply will therefore be provided totally by the PICA emerging from the vertebral artery.
Vascularization of the anterior surface of the medulla oblongata and olive has been the subject of numerous publications (e.g., 1, 4, 5): all authors agree that the topographic vascular redundancy should be respected, but few of them have mentioned the highly frequent pial anastomoses at the surface of the brain stem, anastomoses that we found in one case out of two.
The number of perforating arteries for the brain stem seems relatively unimportant. However, it is more important to note that no perforating branch supplying the lateral surface of the brain stem comes from a C1-PICA or a AICA-PICA. In the other cases, if the PICA emerges from the intradural vertebral artery, it can be considered that all the perforating arteries come from the PICA except when it is proximal; but there is no perforating artery emerging from the vertebral artery upstream of this PICA.
The existence of more or less large-caliber anastomoses should not hide the fact that the pial arteries emerge from the perforating arteries providing blood to either the cranial nerves or the cranial nerve nuclei, as has been studied remarkably well in earlier works4,11,15,17.
The lateral spinal artery always emerges from the PICA or as a variation from the C1-PICA; on a short segment, this PICA can therefore be considered as none other that the lateral spinal artery, which explains that it can supply the posterior surface of the medulla oblongata, as does the lateral spinal artery, i.e., the posterior cords, before recruiting or vascularizing a usually vermian cerebellar area. With the dilatation of a pial artery, this explanation is confirmed by the existence of the PICA whose loop gives the cerebellar falx artery, of several lateral spinal arteries emerging from a common trunk of the vertebral artery at the origin of the lateral spinal artery and a posterior meningeal or a low-arising superior cerebellar artery emerging from the vertebral artery, supplying the posterior spinal artery and the meningeal artery of the cerebellar falx.
The lateral spinal artery can therefore arise from the vertebral artery in its intracranial course or from the PICA in the extracranial position (C1) or from the vertebral artery in its extracranial portion. In these three situations, even if the lateral spinal artery is not visible on angiography, it should be assumed to exist.
Since Ariens Kappers’s study3, it can be assumed that the vertebral artery is the artery of the first cranial nerve.
This artery has an anterior part following the anterior fibers, which is divided into an ascending branch, the future vertebral artery that will join the basilar trunk, and a descending branch, the anterior spinal artery. The posterior component of the artery of the first cranial nerve is none other than the lateral spinal artery that follows the posterior fibers of the nerve.
Conclusions
The PICA can present in three different situations:
- Emergence of an AICA-PICA common trunk arising from the basilar artery and never giving perforating arteries to the lateral surface of the brain stem or to the lateral spinal artery, but supplying blood to the ipsilateral cerebellar hemisphere. The perforating arteries then arise from the vertebral artery and the hemivermis can be supplied by the contralateral PICA.
- Extracranial emergence at C1, never giving perforating arteries for the lateral surface of the brain stem (in this case, the perforating arteries emerge from the vertebral artery), with a very long course in the cerebellomedullary cistern, giving pial branches for the posterior surface of the medulla oblongata and always at the origin of the lateral spinal artery.
- Emergence of the vertebral artery; in this case, the PICA is at the origin of the perforating arteries of the brain stem and the blood supply of the ipsilateral cerebellum (and of the vermis if there is a contralateral AICA-PICA common trunk); in nearly all cases, no perforating arteries arise from the vertebral artery between its penetration in the skull and the emergence of the PICA. The lateral spinal artery emerges preferentially from the vertebral artery just before or after its dural penetration.
References
- 1.Akar ZC, Dujovny M, et al. Microvascular anatomy of the anterior surface of the medulla oblongata and olive. J Neurosurg. 1995;82:97–105. doi: 10.3171/jns.1995.82.1.0097. [DOI] [PubMed] [Google Scholar]
- 2.Amarenco P, Hauw JJ. Anatomie des artères cérébelleuses. Rev Neurol. (Paris) 1989;145(4):267–276. [PubMed] [Google Scholar]
- 3.Ariens Kappers CU. Anatomie comparée du système nerveux. Paris: Masson et Cie; 1947. pp. 524–532. [Google Scholar]
- 4.Duvernoy HM. Human Brainstem Vessels. Berlin Heidelberg New York: Springer-Verlag; 1978. [Google Scholar]
- 5.Grand W, Budny JL, et al. Microvascular surgical anatomy of the vertebrobasilar junction. Neurosurg. 1997;40(6):1219–1225. doi: 10.1097/00006123-199706000-00021. [DOI] [PubMed] [Google Scholar]
- 6.Lasjaunias P, Vallee B, et al. The lateral spinal artery of the upper cervical spinal cord. J Neurosurg. 1985;63:235–241. doi: 10.3171/jns.1985.63.2.0235. [DOI] [PubMed] [Google Scholar]
- 7.Lasjaunias P, Berenstein A, terBrugge KG. Surgical Neuroangiography. 1, 2nd. ed Springer-Verlag; 2003. pp. 224–260. [Google Scholar]
- 8.Lister JR, Rhoton AL, Jr, et al. Microsurgical anatomy of the posterior inferior cerebellar artery. Neurosurg. 1982;10(2):170–199. [PubMed] [Google Scholar]
- 9.Mahmood A, Dujovny M, et al. Microvascular anatomy of foramen caecum medullae oblongata. J Neurosurg. 1991;75:299–304. doi: 10.3171/jns.1991.75.2.0299. [DOI] [PubMed] [Google Scholar]
- 10.Maillot Cl, Koritke JG. Les origines du tronc artériel spinal postérieur chez l’homme. CR Assoc Anat. 1970;149::837–847. [PubMed] [Google Scholar]
- 11.Marinkovic SV, Gibo H. The surgical anatomy of the perforating branches of the basilar artery. Neurosurgery. 1993;33(1):80–87. doi: 10.1227/00006123-199307000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Marinkovic S, Gibo H, Milisavljevic M. The surgical anatomy of the relationships between the perforating and the leptomeningeal arteries. Neurosurg. 1996;39(1):72–83. doi: 10.1097/00006123-199607000-00016. [DOI] [PubMed] [Google Scholar]
- 13.Mercier P, Brassier G, et al. Predictability of the cervical origin of the anterior spinal artery. Interventional Neuroradiology. 1997;3:283–288. doi: 10.1177/159101999700300402. [DOI] [PubMed] [Google Scholar]
- 14.Mercier P, Brassier G, et al. Is the foramen caecum the uppermost part of the spinal medulla? Interventional Neuroradiology. 1999;5:307–312. doi: 10.1177/159101999900500407. [DOI] [PubMed] [Google Scholar]
- 15.Stopford JSB. The arteries of the pons and medulla oblongata. J Anat Physiol. 1916;50:131–164. [PMC free article] [PubMed] [Google Scholar]
- 16.Vallee B, Person H, et al. Anatomie microchirurgicale du tronc de l’artère cérébelleuse postéro-inférieure. Neurochirugie. 1982;28:383–389. [PubMed] [Google Scholar]
- 17.Yasargil MG. Microneurosurgery. Vol 1 and 2. Stuttgart: Georg Thieme Verlag; 1984. [Google Scholar]