Summary
This study was designed to elucidate the generating mechanism, diagnosis and treatment of traumatic carotid cavernous fistula (tCCF) concomitant with pseudoaneurysm in the sphenoid sinus. Six cases of tCCF concomitant with pseudoaneurysm in the sphenoid sinus were analyzed in this study. Clinical history, neurological examination, CT and MRI scans, pre- and postembolization cerebral angiograms and follow-up data were included.
All patients presented with massive epistaxis and symptoms of tCCF. The pseudoaneurysms and fistulas were occluded with detachable balloons, and preservation of the parent artery in two cases. One patient also had indirect carotid cavernous fistula (CCF) on the contralateral side embolized by transfacial vein approach with microcoils. Complete symptom resolution was achieved in all cases, without procedure related complications. During the follow-up period all patients returned to work.
Falling from a high speed motorcycle without wearing a helmet may be one of the main causes of this disease. The site of impact during the accident mostly localizes in the frontal and lateral of the orbit. Intracavernous sinus hypertension of tCCF combining with fracture of the lateral wall of the sphenoid may lead to the formation of a pseudoaneurysm in the sphenoid sinus. MRI scan is very helpful in the diagnosis of this disease before the patient receives angiography. Detachable balloon occlusion of the pseudoaneurysm and fistula is a safe and efficient treatment.
Key words: pseudoaneurysm, head injury, epistaxis, interventional therapy
Introduction
The development of tCCF after closed head trauma is well-known phenomenon, and the treatment result is acceptable29. Traumatic pseudoaneurysm in the sphenoid sinus is a very rare cause of epistaxis, but it is a life-threatening clinical situation when left untreated14,28,26,1,2. There is less documentation of tCCF with concomitant pseudoaneurysm in the sphenoid sinus. This paper presents six cases in detail discussing the generating mechanism, diagnosis and treatment methods.
Materials and Methods
Patient characteristics
This patient series consisted of one woman and five men whose mean age was 37 years (range, 31-48 yrs). The clinical and morphological data for the cases are listed in Table 1. All patients of this group had episodes of massive epistaxis, once (n=2), twice (n=2), three times (n=2), blood transfusion was necessary for stabilization of vital signs in every episode. All patients suffered severe head trauma by falling from a high speed motorcycle without wearing a helmet. All patients underwent pre- and postangiographic neurological examinations and CT scanning. In the last case before angiographic magnetic resonance imaging studies were available. According to the patients’ statement, the scars and the CT scan, we also analysed the site of the impact. All patients were treated by endovascular techniques. Follow-up data were acquired during office visits and by contacting patients by telephone or letter. The follow-up periods ranged from ten months to eight years (mean, 60 months).
Table 1.
Summary of the cases.
| Case | Age/ | Trauma | Symptoms | Interval* | CT | Treatment | Outcome |
|---|---|---|---|---|---|---|---|
| No | Sex | Results | |||||
|
| |||||||
| 1 | 48/M | MCA(D) | Left proptosis, | 7 days | Sphenoid fracture | DBO | Normal |
| chemosis bruit, | and hematoma | ||||||
| sixth nverve palsy, | |||||||
| epistaxis | |||||||
|
| |||||||
| 2 | 31/F | MCA(P) | Left ptosis, | 30 days | Sphenoid, | DBO | Normal |
| unilateral blindness, | zygomatic arch | ||||||
| epistaxis | and ribs fracture | ||||||
|
| |||||||
| 3 | 33/M | MCA(D) | Left chemosis, | + | SAH, sphenoid, | DBO | Normal |
| coma, | right femru and | ||||||
| epistaxis | orbit roof fracture | ||||||
|
| |||||||
| 4 | 36/M | MCA(D) | Left chemosis, | 7 days | Left front, | DBO/ | Normal |
| ptosis, bruit | orbit roof fracture, | MCO | |||||
| and epistaxis | bilateral front | ||||||
| lobe contusion | |||||||
|
| |||||||
| 5 | 30/M | MCA(D) | Left loss | + | Left | DBO | Normal |
| of vision, bruit, | zygomaticum, ethmoid | ||||||
| epistaxis | and sphenoid fracture, | ||||||
| hematoma | |||||||
|
| |||||||
| 6 | 44/M | MCA(D) | Right chemosis, | 3 days | Right basal ganglis | DBO | Normal |
| visual field defect, | infarction, zygomatic | ||||||
| bruit and epistaxis | arch, sphenoid and | ||||||
| ehtmoid fracture | |||||||
* interval between the initial symptoms of traumatic carotid cavernous fistula and the presentation fo epistaxis.
+ immediately after trauma. - MCA(D) = motorcycle accident driver; MCA(P) = motorcycle accident passenger. DBO = detachable balloon occlusion, MCO = microcoil occlusion.
Endovascular procedures
Five endovascular procedures were performed with local anesthesia and light neuroleptic analgesia, to allow continuous neurological monitoring. The bilateral transfemoral approach and full systemic heparinization were applied in all cases. A simple occlusion test with clinical monitoring was performed for 30 minutes before permanent internal carotid artery (ICA) sacrifice. The fistulas, pseudoaneurysm and parent artery occlusion were achieved in four cases with detachable latex balloons (Balt Extrusion, Montmorency, France), and preservation of the parent artery in the other two cases. In the fourth case, who also had indirect carotid cavernous fistula on the contralateral side, because we had occluded the ipsilateral internal carotid artery, the contralateral side cavernous sinus was embolized with microcoils via the transfacial vein - superior ophthalmic vein approach under general anaesthesia, and preservation of the parent artery.
Representative cases
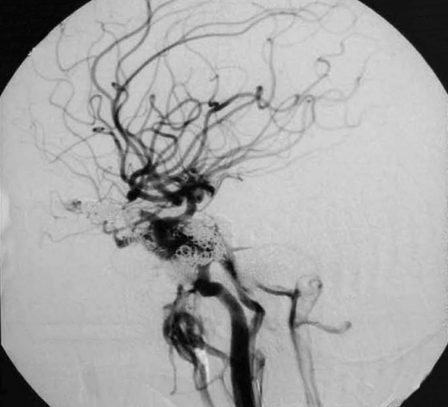
Patient 5
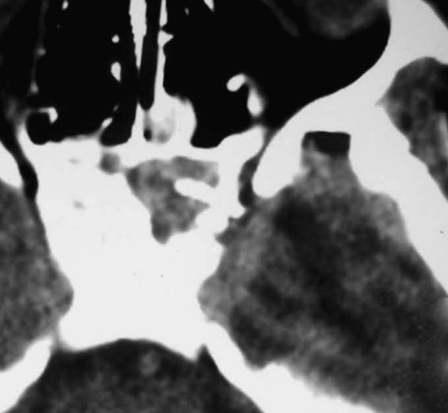
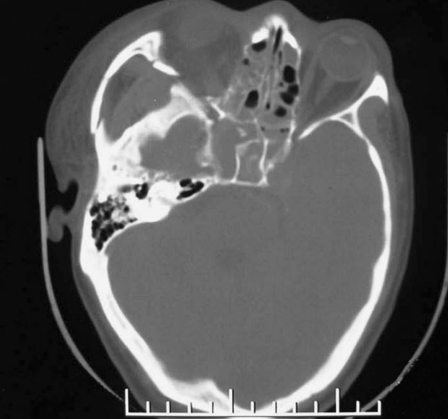
This 30-year-old man presented with massive epistaxis after a fall from a high speed motorcycle. Early CT scans revealed subdural hematoma and brain contusion in the left temporal lobe, hematoma in the sphenoid sinus, fractures in the sphenoid sinus lateral wall and carotid canal (figure 1A).
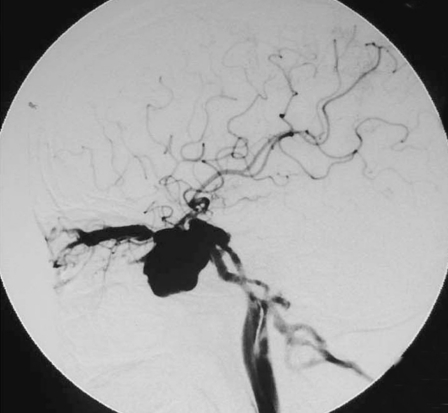
Figure 1.
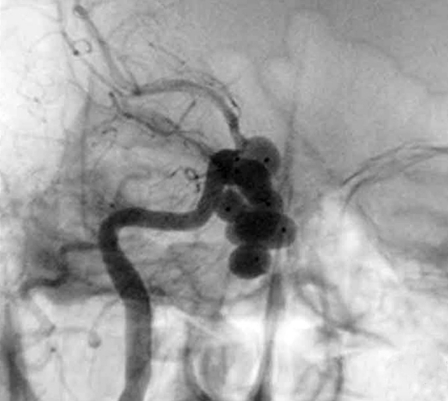
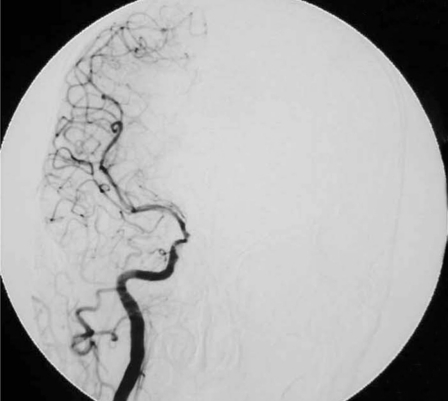
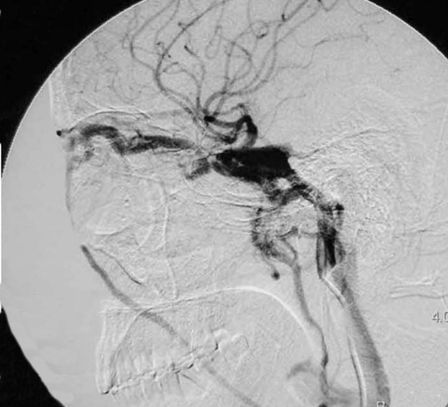
Case 5, a 30-year-old man presented with massive epistaxis after a fall from a high speed motorcycle. A) Early axial CT scans revealed hematoma in the sphenoid sinus, fractures in the left sphenoid sinus lateral wall and carotid canal. B) Lateral unsubtraction film of left internal carotid injection suggested a pseudoaneurysm of the cavernous segment filling the sphenoid sinus and a tCCF originating from the left ICA C3. C) Anteroposterior view of the same artery injection. D) Anteroposterior subtraction film of the same artery injection showed the pseudoaneurysm and the draining vein of the fistula. E) After the fistula and the pseudoaneurysm was occluded using only one detachable latex balloon, lateral unsubtraction film demonstrated the site of the balloon. F) Preservation of the parent artery.
A.
B.
C.
D.
E.
F.
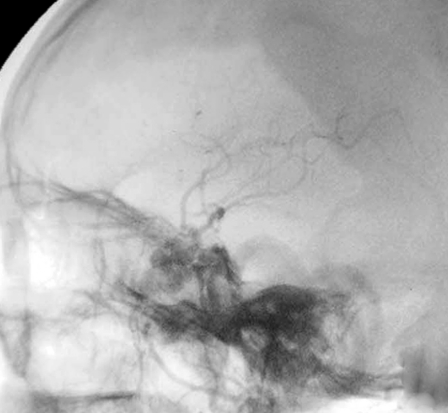
After surgical removal of the subdural hematoma and decompression, he regained consciousness and complained of intracranal bruit and left total vision loss. Cerebral angiography performed two months after trauma disclosed a pseudoaneurysm of the cavernous segment filling the sphenoid sinus and a tCCF originating from the left ICA C3 (figure 1B-D). Test occlusion of the left ICA was well tolerated for 30 minutes without development of focal neurological deficits, then the fistula and the pseudoaneurysm were occluded using only one detachable latex balloon, with preservation of the parent artery (figure 1E,F).
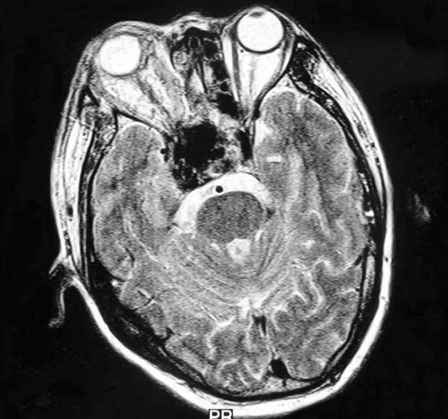
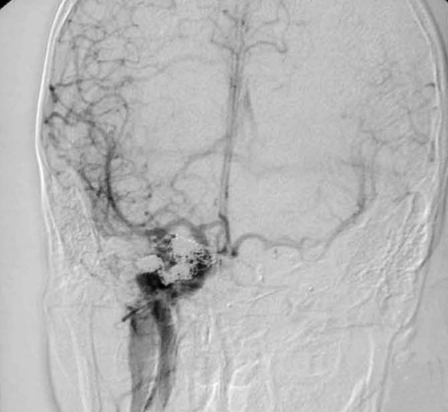
Patient 6
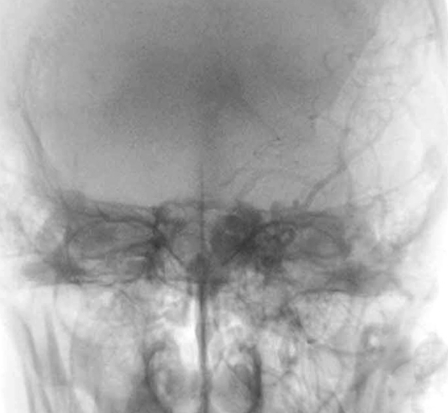
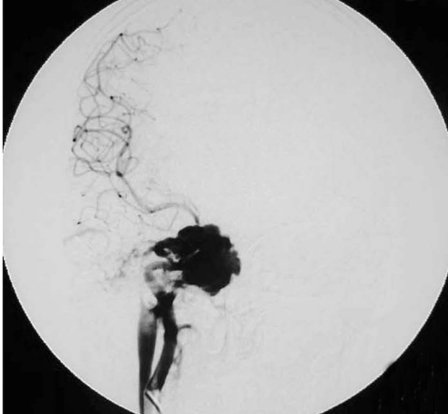
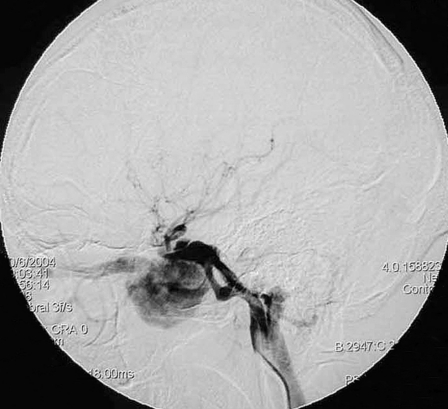
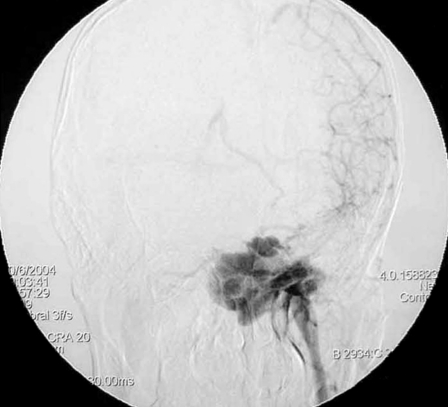
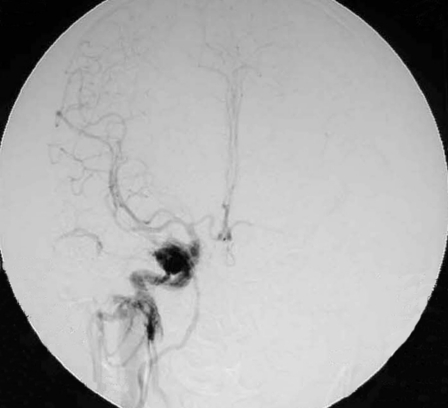
This 44-year-old man with right side chemosis, visual field defect and intracranal bruit had suffered trauma caused by a falling from a high speed motorcycle, and had an episode of massive epistaxis three days after the accident. Early CT scans revealed fracture at the right zygomatic arch, sphenoid and ethmoid sinus, soft-tissue density in the sphenoid sinus (figure 2A). The diagnosis was confirmed by subsequent MRI scan which demonstrated right basal ganglia infarction, a large signal void aneurysm in the sphenoid sinus and a dilated right side cavernous sinus (figure 2B). An irregular pseudoaneurysm projecting anteroinferiorly into the sphenoid sinus concomitant with tCCF was found on right internal carotid angiography. There was minimal flow in the supraclinoid portion of the right ICA, and the right A1 was dysplastic (figure 2C,D). After seven ballons were detached into the lumen of pseudoaneurysm, the fistula and pseudoaneurysm were occluded by the eighth detachable latex balloon with preservation of the parent artery (figure 2E,F).
Figure 2.
Case 6, a 44-year-old man with right side chemosis, visual field defect, intracranal bruit had suffered trauma caused by a falling from high speed motorcycle, and had episode of massive epistaxis three days after the accident. A) Early CT scans revealed fracture at the right zygomatic arch, sphenoid and ethmoid sinus, soft tissue density in the sphenoid sinus. B) Subsequent T2-weighted axial MRI scan demonstrated a large signal-void aneurysm in the sphenoid sinus and a dilated right side cavernous sinus. C?An irregular pseudoaneurysm projecting anteroinferiorly into the sphenoid sinus with concomitant traumatic carotid cavernous fistula draining via the superior ophthalmic vein and inferior petrosal sinus was found on lateral view of right interal carotid angiogram. D) Anteroposterior view also demonstrated that there was minimal flow in the supraclinoid portion of the right ICA,and the right A1 was dysplastic. E) Anteroposterior unsubtracted and F) subtracted film showed the fistula and the pseudoaneurysm were occluded by the eight detachable latex balloons with preservation of the parent artery.
A.
B.
C.
D.
E.
F.
Patient 4
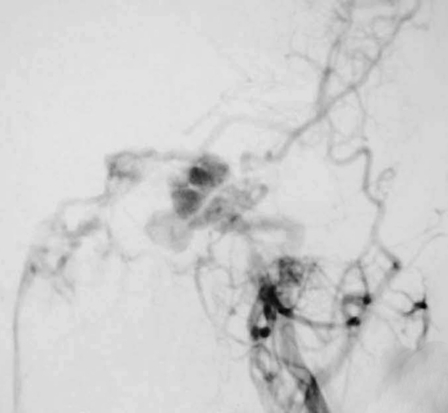
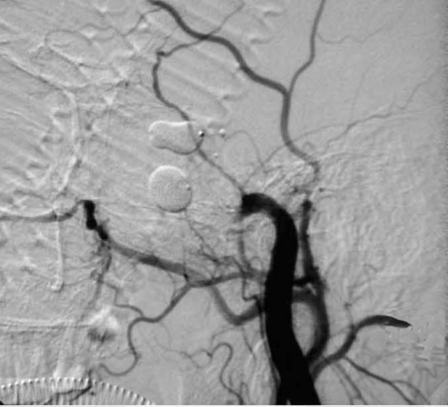
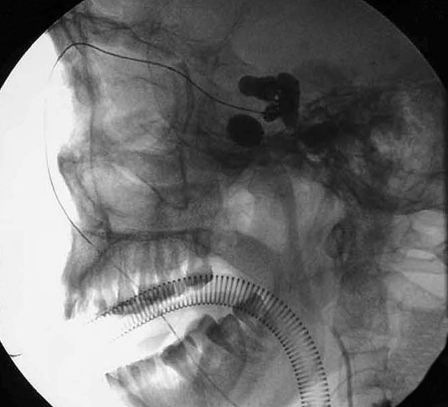
This 36-year-old male was brought to our department with the chief complaint of recurrent epistaxis, intracranial bruit, left chemosis, ptosis and proptosis for two weeks after a motorcycle accident. Initial CT scans revealed left frontal, bilateral orbit roof and sphenoid sinus lateral wall fractures, bilateral frontal lobe contusions. Angiography demonstrated bilateral tCCF, with tears in the intracavernous portions of both ICA. There was minimal flow in the supraclinoid portion of the left ICA. The right ICA and the vertebral circulation maintained supply to the left hemisphere through patent anterior and posterior communicating arteries. There was a pseudoaneurysm projecting anteroinferiorly into the sphenoid sinus in the cavernous portion of the left ICA (figure 3A-D). Endovascular balloon occlusion of the left CCF failed due to the size of the tear. The ICA was therefore occluded with another two balloons, one at the level of the fistula and the other proximal to the pseudoaneurysm. This achieved closure of the fistula and isolation of the pseudoaneurysm (figure 3E). Because the right ICA had to be preserved, the right CCF was embolized by the facial vein - superior ophthalmic vein route under general anaesthesia with microcoils (figure 3F-H). The patient’s symptoms resolved completely after the procedure and he made a satisfactory recovery. Another angiogram three months later demonstrated the right ICA maintained supply to the left hemisphere through patent anterior communicating arteries, minimal residual shunting was found in the right side and there had been complete resolution of the left pseudoaneurysm (figure 3I).
Figure 3.
Case 4, this 36-year-old man was brought to our department with the chief complaint of recurrent epistaxis, intracranial bruit, left chemosis, ptosis and proptosis for two weeks after a motorcycle accident. Lateral view (A) and anteroposterior view (B) of left internal carotid angiogram demonstrated a tCCF and a pseudoaneurysm projecting anteroinferiorly into the sphenoid sinus in the cavernous portion. Lateral view (C) and anteroposterior view (D) of the right internal carotid angiogram revealed a tCCF draining via the superior ophthalmic vein - facial vein and inferior petrosal sinus. E) The lateral view of the carotid angiogram demonstrated the ICA was occluded with four detachable latex balloons. This achieved closure of the fistula and isolation of the pseudoaneurysm. F,G) The procedure of the right cavernous sinus embolization via a right facial vein - superior ophthalmic vein route with microcoils. H) Posterior embolization angiogram and I) another angiography 3 months later demonstrated the right internal carotid artery maintained supply to the left hemisphere through patent anterior communicating artery, minimal residual shunting was found in the right side and there had been complete resolution of the left pseudoaneurysm.
A.
B.
C.
D.
E.
F.
G.
H.
I.
Results
This group of patients constituted about 12% (6/51) of all tCCF patients in the same period. All lesions resulted from non-penetrating trauma caused by falling from a high speed motorcycle; five patients were drivers and one was a passenger. The site of impact was mostly localized in the frontal and lateral parts of the orbit. All patients presented with massive epistaxis and symptoms of tCCF. Two patients of this group had episodes of intracranal bruit, chemosis and epistaxis simultaneously right after the injury, the interval between these two groups of symptoms in the other four patients ranged from three days to one month. The pseudoaneurysm and fistulas were occluded with detachable balloons, and preservation of the parent artery in two cases. One patient also had indirect carotid cavernous fistula on the contralateral side, embolized by transfacial vein approach under general anaesthesia with microcoils. Complete symptom resolution was achieved in all cases, without procedure related complications. The follow-up periods ranged from ten months to eight years with no symptom recurrence, all patients returned to their normal life.
Discussion
Traumatic intracranial pseudoaneurysms are rare lesions, constituting only 0.15% to 0.40% of all intracranial aneurysms20. Traumatic pseudoaneurysms presenting with recurrent epistaxis are even rarer, from 1928 when Birley and Trotter first reported such a case to 1990, only about 100 cases have been reported in the world literature3,14. Traumatic CCF concomitant with pseudoaneurysm in the sphenoid sinus presenting with epistaxis is an extremely rare occurrence with few reports in the literature4,15,21,18,19.
It is well known that the ICA is divided into four portions: cervical, petrous, cavernous and cerebral. In the cavernous portion, the carotid first ascends to the posterior clinoid process, then curves forward along the side of the sphenoid sinus and curves again forward along the side of the sphenoid sinus and curves again upward to emerge medial to the anterior clinoid process.
This portion is approximately 2 cm in length and, on average, 2.3 mm lateral to the pituitary gland. In some instances, it may course more medially and indent the lateral wall of the sphenoid sinus13. An anatomy study with cadaver dissection done by Renn and Rhoton24 showed the carotid artery bulging into the sinus in 71% of the cadaver specimens. The bony layer covering the ICA was less than 1 mm thick in 66% of their specimens, and 4% had no bony layer and were covered only by dura and sinus mucosa. Severe head trauma can result in sufficient injury to the cavernous portion of the ICA can result in a CCF, a pseudoaneurysm, dissection of the artery, or rupture and fatal hemorrhage10. Blunt head injury may result in pseudoaneurysm formation from shearing forces of hemorrhages in the artery wall, thus weakening the artery. Some authors thought the pounding of the blood against the weakened arterial wall was responsible for further stretching of the artery and forming the pseudoaneurysm that took time and might have occurred within months or years before epistaxis6.
Two patients of this group had episodes of intracranial bruit, chemosis and epistaxis simultaneously right after the injury, the interval between these two groups of symptoms in the other four patients ranged from three days to one month. When these two groups of symptoms occurred simultaneously, it probably resulted from direct puncture to the sphenoid sinus wall and proximal ICA. In the other condition, we presumed that the intracavernous high pressure of CCF further destroyed the fractured sphenoid sinus wall, which might explain the delayed epistaxis.
Traumatic carotid cavernous fistula concomitant with pseudoaneurysm in the sphenoid sinus reported in the literature mostly resulted from penetrating head trauma and motor vehicle accidents4,18,19,26. Intracavernous carotid artery pseudoaneurysm occurring after transsphenoidal microsurgery has been well reported11,12, but we never found reported concomitant with CCF. Six patients in this group were all caused by falling from a high speed motorcycle without wearing a helmet, five were drivers, one was a passenger. According to the patients’ statements, the scars in the face and the CT scan, the site of impact was mostly localized in the frontal and lateral part of the orbit. All six patients suffered multiple skull fractures, especially the lateral wall of the sphenoid sinus, adjoining the sphenoid sinus and ethmoid sinus. From the anatomy aspect, the sphenoid sinus is situated in the centre of the skull base, anterior ethmoid sinus, lateral sphenoid ridge, basilar part of the occipital bone and petrous part of the posterior temporal bone. So we presume that if the impact comes from the frontal and lateral part of the orbit, the strength transmits along the sphenoid ridge to the lateral wall of the sphenoid sinus, which is more fragile and fracture occurs more frequently. When the impact comes anteriorly, the ethmoid sinus will absorb part of the force. At the same time the shape of the sphenoid sinus seems more resistant to force coming anteriorly, and sphenoid sinus fracture occurs more seldom.
Death is three times less likely if the pseudoaneurysm is diagnosed before it has ruptured, compared with diagnosis after rupture22. Therefore, prompt diagnosis and treatment are very important. In 1961, Maurer et Al17 noted the triad of unilateral blindness, frontal fracture and massive delayed epistaxis after non-penetrating head trauma, due to internal carotid aneurysm with rupture into the sphenoid sinus. In the present series, all six patients suffered multiple skull fractures and recurrent epistaxis, three cases showed vision loss on the affected side, four cases showed chemosis and intracranal bruit. So we think patients presenting with Maurer’s triad combining with symptoms of traumatic carotid cavernous fistulas should be evaluated for the development of pseudoaneurysm as soon as possible. In case 5, according to the patient’s clinical history and CT scan, the diagnosis was made before angiography. In case 6, the pseudoaneurysm and tCCF were demonstrated on MRI, and the diagnosis was also made before the angiography. So we think that an MRI scan is very helpful in diagnosis of this disease before the patient receives angiography. Still it is very important to make the distinction between a pseudoaneurysm associated with a CCF and a large venous varix associated with a CCF. In our experience, the dilated venous varix associated with a CCF cannot destroy the lateral wall of the sphenoid sinus, it is simply limited in the cavernous sinus. If the contrast agent goes into the sphenoid sinus during angiography, a pseudoaneurysm can be confirmed.
Many methods have been reported to treat intracavernous pseudoaneurysm, such as endovascular stent and coils, endovascular covered stent, detachable balloons, direct surgical repair the internal carotid, trapping procedure, etc.5,7,8,26. But for traumatic carotid cavernous fistula with concomitant pseudoaneurysm in the sphenoid sinus, the treatment methods are confined to endovascular coils, detachable balloons and trapping procedures4,15,18,19. At present, most neuroradiologists believe that a traumatic pseudoaneurysm is only a fragile sac surrounded by organizing blood clot that may even disappear with fibrinolysis, there may be little tissue to hold or buttress the balloon in place over the laceration in the carotid artery. In 1987, Fox et Al9 recommended the placement of balloons to trap the main artery rather than placement of balloons directly into the aneurysm because of the potential for recurrent epistaxis if the balloon is extruded through the sphenoid sinus. All six lesions in our group were treated with detachable balloons and preservation of the parent arteries was achieved in two cases with a follow-up period of 10 months and 11 months without any recurrent bleeding. In the sixth patient, we placed eight detachable latex balloons into the pseudoaneurysm sac, and the fistula and the pseudoaneurysm were occluded with preservation of the parent artery. So we presume that most of the pseudoaneurysm sacs are not so fragile except for the line of bone fracture and the site of the sphenoid ostia, the lateral wall and the septa of the sphenoid may offer enough support for the balloons. So for some of these patients, we still have a chance to preserve the parent artery. Even if we can preserve the parent artery, we still emphasize the importance of examining cross collateral blood flow by placement of additional catheters through the opposite femoral route. Recently, Shin et Al25 reported intranasal extrusion of the endovascular coil after occluding internal carotid artery for massive epistaxis. It is well known that the neck of a pseudoaneurysm is not so strong as the neck of a true aneurysm, and we think the endvascular microcoil is too soft to occlude the neck of a pseudoaneurysm tightly. Therefore, the endovascular microcoil should not be the first choice for this disease. Covered stent can reconstruct a damaged vessel, and it has been used to treat traumatic pseudoaneurysm and traumatic carotid cavernous fistula in reports16,23,27, but the stiffness and high dose anti-platelet and anti-coagulants still limit its wider use. In summary, traumatic carotid cavernous fistula concomitant with pseudoaneurysm in the sphenoid sinus is a rare lesion with a very high mortality. To recognize the generating mechanism of this disease thoroughly and to improve the treatment result, we still have a long way to go!
References
- 1.Bavinzski G, Killer M, et al. False aneurysms of the intracavernous carotid artery. Report of 7 cases. Acta-Neurochir (Wien) 1997;139:37–43. doi: 10.1007/BF01850866. [DOI] [PubMed] [Google Scholar]
- 2.Bhatoe HS, Suryanarayana KV, Gill HS. Recurrent massive epistaxis due to traumatic intracavernous internal carotid artery aneurysm. J Laryngol Otol. 1995;109:650–652. doi: 10.1017/s0022215100130932. [DOI] [PubMed] [Google Scholar]
- 3.Birley JL, Trotter W. Traumatic aneurysm of the intracranial portion of the internal carotid artery. Brain. 1928;5:184–208. [Google Scholar]
- 4.Borba R, Sonda I, et al. Carotid-cavernous fistula with lethal epistaxis: case report. Arq-Neuropsiquiatr. 2001;59:276–279. [PubMed] [Google Scholar]
- 5.Celil G, Engin D, et al. Intractable epistaxis related to cavernous carotid artery pseudoaneurysm: treatment of a case with covered stent. Auris Nasus Larynx. 2004;31:275–278. doi: 10.1016/j.anl.2004.03.007. [DOI] [PubMed] [Google Scholar]
- 6.Chambers EF, Rosenbaum AE, et al. Traumatic aneurysms of cavernous internal carotid artery with secondary epistaxis. Am J Neuroradiol. 1981;2:405–409. [PMC free article] [PubMed] [Google Scholar]
- 7.Dolenc V. Direct microsurgical repair of intracavernous vascular lesions. J Neurosurg. 1983;58:824–831. doi: 10.3171/jns.1983.58.6.0824. [DOI] [PubMed] [Google Scholar]
- 8.Fontela PS, Tampieri D, et al. Posttraumatic pseudoaneurysm of the intracavernous internal carotid artery presenting with massive epistaxis. . Pediatr Crit Care-Med. 2006;7:260–262. doi: 10.1097/01.PCC.0000216418.01278.5E. [DOI] [PubMed] [Google Scholar]
- 9.Fox AL, Vinuela F, et al. Use of detachable balloons for proximal artery occlusion in the treatment of unclippable cerebral aneurysms. J Neurosurg. 1987;66:40–46. doi: 10.3171/jns.1987.66.1.0040. [DOI] [PubMed] [Google Scholar]
- 10.Fox JL. In: Radiology. Fox JL, editor. vol 1 Intracranial Aneurysms. New York: Springer Verlag NY Inc; 1983. pp. 496–548. [Google Scholar]
- 11.Hattori I, Iwasaki K, et al. Treatment of a ruptured giant internal carotid artery pseudoaneurysm following transsphenoidal surgery: case report and literature review. No Shinkei Geka. 2006;34:1141–1146. [PubMed] [Google Scholar]
- 12.Kai Y, Hamada J, et al. Successful treatment with bypass and interventional surgery for a ruptured pseudo carotid artery aneurysm after transsphenoidal surgery: a case report. No Shinkei Geka . 2001;29:241–245. [PubMed] [Google Scholar]
- 13.Kline LB, Acker JD, Post MJ. Computed tomographic evaluation of the cavernous sinus. Ophthalmology. 1982;89:374–385. doi: 10.1016/s0161-6420(82)34781-8. [DOI] [PubMed] [Google Scholar]
- 14.Lee JP, Wang AD. Epistaxis due to traumatic intracavernous aneurysm: case report. J Trauma. 1990;30:619–22. doi: 10.1097/00005373-199005000-00017. [DOI] [PubMed] [Google Scholar]
- 15.Luo CB, Teng MM, et al. Endovascular embolization of recurrent traumatic carotid-cavernous fistulas managed previously with detachable balloons. J Trauma. 2004;56:1214–1220. doi: 10.1097/01.ta.0000131213.93205.57. [DOI] [PubMed] [Google Scholar]
- 16.Madan A, Mujic A, et al. Traumatic carotid artery-cavernous sinus fistula treated with a covered stent. Report of two cases. J Neurosurg. 2006;104:969– 973 . doi: 10.3171/jns.2006.104.6.969. [DOI] [PubMed] [Google Scholar]
- 17.Maurer MY, Mills M, German WJ. Triad of unilateral blindness, orbital fracture and massive epistaxis in head injury. J Neurosurg. 1961;18:837–846. doi: 10.3171/jns.1961.18.6.0837. [DOI] [PubMed] [Google Scholar]
- 18.Millman B, Giddings NA. Traumatic carotid-cavernous sinus fistula with delayed epistaxis. Ear Nose Throat J. 1994;73(6):408–411. [PubMed] [Google Scholar]
- 19.Nakao S, Sato S, et al. Massive epistaxis due to traumatic intracavernous carotid aneurysm associated with carotid-cavernous fistula. Case report. Neurol Med-Chir (Tokyo) 1987;27:456–462. doi: 10.2176/nmc.27.456. [DOI] [PubMed] [Google Scholar]
- 20.Parkinson D, West M. Traumatic intracranial aneurysms. . J Neurosurg. 1980;52:11–20. doi: 10.3171/jns.1980.52.1.0011. [DOI] [PubMed] [Google Scholar]
- 21.Pothula VB, Reddy KT, Nixon TE. Carotico-cavernous fistula following septorhinoplasty. J Laryngol Otol. 1999;113:844–846. doi: 10.1017/s0022215100145360. [DOI] [PubMed] [Google Scholar]
- 22.Ramos A, Tobio R, et al. Traumatic aneurysm of the internal carotid artery: a late finding presenting as a mass in the sphenoid sinus. Am J Neuroradiol. 1996;17:222–225. [PMC free article] [PubMed] [Google Scholar]
- 23.Redekop G, Marotta T, Weill A. Treatment of traumatic aneurysms and arteriovenous fistulas of the skull base by using endovascular stents. Neurosurg. 2001;95(3):412–419. doi: 10.3171/jns.2001.95.3.0412. [DOI] [PubMed] [Google Scholar]
- 24.Renn WH, Rhoton Al. Microsugical anatomy of the sellar region. J Neurosug. 1975;43:288–298. doi: 10.3171/jns.1975.43.3.0288. [DOI] [PubMed] [Google Scholar]
- 25.Shin YS, Kim SY, Moon SK. Intranasal extrusion of the endovascular coil after occluding internal carotid artery for massive nasopharyngeal bleeding. Otolaryngol Head Neck Surg. 2005;133:644. doi: 10.1016/j.otohns.2004.09.113. [DOI] [PubMed] [Google Scholar]
- 26.Uzan M, Cantasdemir M, Seckin MS, et al. Traumatic intracranial carotid tree aneurysms. Neurosurgery. 1998;43:1314–20. doi: 10.1097/00006123-199812000-00024. discussion 1320-2. [DOI] [PubMed] [Google Scholar]
- 27.Vincent S, Jean-Francois DW, et al. Pseudoaneurysm of the internal carotid artery: treatment with a covered stent. . Cardiovasc Intervent Radiol. 2001;24:283–285. doi: 10.1007/s00270-001-0012-z. [DOI] [PubMed] [Google Scholar]
- 28.Wang AN, Winfield JA, Gucer G. Traumatic internal carotid artery aneurysm with rupture into the sphenoid sinus. Surg Neurol. 1986;25:77–81. doi: 10.1016/0090-3019(86)90120-5. [DOI] [PubMed] [Google Scholar]
- 29.Wu Z, Wang C, et al. Endovascular embolization of traumatic carotid cavernous fistulas. Chin Med J. 1999;112:433–437. [PubMed] [Google Scholar]