Abstract
Sexual and gonadal dysfunction/infertility are quite common in patients with chronic kidney disease. Forty percent of male and 55% of female dialysis patients do not achieve orgasm. The pathophysiology of gonadal dysfunction is multifactorial. It is usually a combination of psychological, physiological, and other comorbid factors. Erectile dysfunction in males is mainly due to arterial factors, venous leakage, psychological factors, neurogenic factors, endocrine factors, and drugs. Sexual dysfunction in females is mainly due to hormonal factors and manifests mainly as menstrual irregularities, amenorrhea, lack of vaginal lubrication, and failure to conceive. Treatment of gonadal dysfunction in chronic kidney disease is multipronged and an exact understanding of underlying pathology is essential in proper management of these patients.
Keywords: Chronic kidney disease, gonadal dysfunction, infertility, menstrual abnormalities
INTRODUCTION
Gonadal dysfunction is a common occurrence in patients with chronic kidney disease (CKD). Sexual dysfunction begins much before CKD-stage 5 and usually does not reverse with renal replacement therapy.[1,2] There is limited literature on sexual problems (other than fertility related) in CKD patients. While male sexual dysfunction in CKD includes decreased libido, erectile dysfunction, premature or delayed ejaculation, and difficulty in achieving orgasm, female CKD patients have decreased libido, difficulty in achieving orgasm, lack of vaginal lubrication, pain during intercourse, and infertility.[1] The gonadal dysfunction worsens with progression of CKD. Up to 40% of male patients and 55% of female patients on hemodialysis have difficulty in achieving orgasm.[1] Thirty-three percent patients report no sexual activity and 44% report only one sexual activity per week. Menstrual irregularities in CKD patients include amenorrhea (most common) and premature menopause, oligomenorrhea, polymenorrhea, and menorrhagia. Pregnancy is extremely uncommon as one progress from CKD-3 to 5D.[3] Frequency of conception among females of childbearing age undergoing renal replacement therapy ranges from 0.3 to 1.5% per year.[4]
Pathophysiology of gonadal dysfunction differs in male and female CKD patients and includes psychological factors and organic factors. The important factors playing a role in gonadal dysfunction in patients with CKD are discussed below.
MALE SEXUAL DYSFUNCTION
Erectile dysfunction
Erectile dysfunction can be seen in up to 40–80% of hemodialysis patients. Although psychological factor plays an important role, effective renal replacement therapy improves fitness, libido, and potency. Erectile dysfunction in CKD is multifactorial and includes decreased arterial blood flow, venous leakage due to shunts, altered penile smooth muscle function, hormonal disturbances, side effect of medications, and neurogenic dysfunction. The etiological factors are often classified into organic and psychological causes; however, the two factors are interwoven. An optimal therapy for erectile dysfunction should be able to manage all the above-mentioned factors.[5,6]
Arterial factors
A prerequisite for penile erection includes adequate penile blood flow and intracavernosal arterial blood pressure (BP) >80 mmHg. During the initial stages of erection, the penile arterial BP is 20 mmHg less than the pelvic arterial BP. During the later stages, the penile blood flow increases above the systemic BP by contraction of penile muscles (bulbus spongiosus and ischiocavernosus). The pelvic arterial BP needs to be around 80–100 mmHg to maintain a penile BP of 80 mmHg. However, with arterial occlusive disease, the BP in pelvic vessels drops to around 70 mmHg, and hence erectile dysfunction occurs before other peripheral manifestations of arterio-occlusive disease.
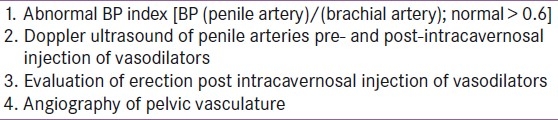
Vascular problems accounts for 60% of non-uremic impotence.[7,8] However, there is no sufficient data on obstructive vascular problems causing impotence in CKD. Patients with CKD have accelerated atherosclerosis and vascular calcification, and hence obstructive vascular problem could contribute to impotence in at least similar fraction in CKD patients. CKD patients have delayed erection at early stages, followed by decreased penile rigidity and nocturnal penile tumescence (NPT) and finally erectile impotence. The exact pathophysiology of CKD resulting in vascular impotence is not clear. However, increasing age, diabetes mellitus, dyslipidemia, hyperhomocysteinemia, and disturbed calcium/phosphorous metabolism could result in accelerated atherosclerosis and vascular calcification of pelvic arteries. Autonomic neuropathy of CKD could also alter penile blood circulation, which is discussed later. The arterial causes of erectile dysfunction can be diagnosed by Doppler ultrasound or angiography [Table 1].
Table 1.
Diagnosis of arteriogenic impotence
Venous leakage
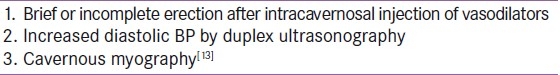
Venous occlusion with normal arterial flow is also an important cause of impotence in uremic patients. Inability to have persistent erection is suggestive of smooth muscle dysfunction and impaired veno-occlusion.[9] Impaired relaxation of penile smooth muscle results in efflux of blood from cavernous space, resulting in erectile dysfunction. Precocious aging and enhanced fibrosis results in decreased fibroelastic compliance of smooth muscle. Pentosidine concentrations are 22 times higher in CKD and 3–4 times in transplant recipients in comparison to healthy controls. Pentosidine concentration is also higher in the corpus cavernosum and thought to be involved in pathogenesis of erectile dysfunction.[10–12] Diagnosis of venous leakage is summarized in Table 2.
Table 2.
Diagnosis of venous insufficiency
Neurogenic and psychogenic factors
Neurogenic: Erection is a complex process and includes neural, hormonal, and local substances. Three neurogenic process of erection are:
Psychogenic erection: Visual and auditory stimuli/impulse from brain reach via thoracolumbar nerve to cavernous nerve.
Reflex erection: Occurs with sensory stimulation of receptors along the shaft of penis. Somatic nerve provides the afferent supply while the efferent supply is by the pelvic nerve (S2, 3, 4).
Nocturnal erection: Occurs during rapid eye movement (REM) sleep due to increased sensitivity to low androgen levels.[14]
Sacral parasympathetic stimulation causes vasodilatation of penile arteries and increases the blood flow. Increase in blood flow results in increased oxygen concentration and hence increased ability to synthesize nitric oxide (NO). NO in turn leads to smooth muscle relaxation and progressive entrapment of blood in corpus cavernosum.[15,16]
Autonomic neuropathy is a common complication seen in CKD patients. Parasympathetic dysfunction is seen in two-third of patients >65 years of age and one-third of younger patients. Autonomic neuropathy improves after several months of intensive renal replacement therapy.[17,18]
Psychogenic: CKD patients have higher prevalence of depression.[19] There are also other psychogenic factors like stress, decreased appetite, fear of procedure or medications, etc. which can aggravate impotence in CKD patients. Male hemodialysis patients with psychogenic cause of impotence have a normal 3–5 NPT/night during REM sleep. Lack of nocturnal erection is a reliable test for organic erectile impotence in patients with psychogenic erectile dysfunction.[20,21]
Drug-induced erectile dysfunction
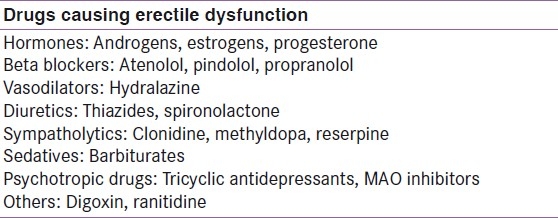
Decreased libido and potency can also be due to adverse effect of many drugs used in CKD [Table 3]. These drugs interfere with neurovascular control of penile arteries and smooth muscle and neuro-endocrine regulation. Alcohol and tobacco are also important causes of reduced sexual function in CKD.[22] Antihypertensive drugs are one of the commonly used class of drugs, which can lead to erectile dysfunction in CKD patients.[23]
Table 3.
Commonly used drugs causing erectile dysfunction in patients with CKD
FEMALE SEXUAL DYSFUNCTION
Vaginal and menstrual abnormalities
Female patients on dialysis have low plasma estrogen levels (due to hyperprolactinemia) resulting in atrophic vaginitis, decreased pubic hair, and pruritus. Normal midcycle karyopyknosis (vaginal cytology) is absent.[24,25] However, the prevalence and spectrum of vaginal infections remain the same as in general population. Menstrual irregularities are very common in uremia. Amenorrhea is seen in 50–100% of patients with CKD-5. Many patients start to have menstrual cycles on initiation of dialysis while others remain amenorrheic. Of the patients who menstruate, 50–80% have polymenorrhea, menorrhagia (probably due to anovualtory cycle which is seen in >90%) or oligomenorrhea.[26–28] Uremic coagulopathy and heparinization during hemodialysis intensify abnormal menstrual bleeding. Increase in ovarian cyst formation can occur in uremic patients and it needs to be distinguished from polycystic ovarian syndrome and other androgen producing tumors.[29]
No data is available regarding the prevalence of female sexual dysfunction, such as desire, orgasm, or pain disorders in chronic kidney disease.
HORMONAL ABNORMALITIES IN CHRONIC KIDNEY DISEASE
Pulsatile secretion of gonadotrophin releasing hormone (GnRH) from hypothalamus regulates pituitary secretion of gonadotrophins [luteinizing hormone (LH) and follicular stimulating hormone (FSH)]. In addition to GnRH, adrenergenic, dopaminergic substances, endorphins, oxytocin, neuropeptide-Y, and leptin also regulate pituitary gonadotrophin secretion.
Uremic effect on gonadotrophins (LH and FSH)
Males
Uremia affects local amino acid neurotransmitter outflow in hypothalamus, significantly affecting the release of GnRH and hence affecting gonadotrophin synthesis and secretion in both males and females.[30,31] In vast majority of patients, there is a normal LH secretion response to exogenous LH releasing hormone (LHRH) stimulation. The plasma LH level is elevated in hemodialysis patients compared to healthy controls. This increased level is due to prolonged half-life of immunoreactive and bioactive LH as well as increased secretion of immunoreactive LH.[32] Although the frequency of LH peaks remains normal, the maximal level and duration of LH peaks is reduced. In view of prolonged half-life of LH in uremia, there is significant decrease in pulsatile secretion of LH.[33] This leads to low levels of testosterone in uremic patients while the serum estradiol and total estrogens levels are usually elevated.[34,35] The decreased testosterone level produces a diminished normal feedback suppression of LH, thus causing persistently high levels of LH.[36] In addition, endogenous opiates also negatively control pulsatile LH release.[37] Plasma β-endorphin and β-lipotropin levels are normal in uremic subjects. However, administration of naloxone increases LH pulses in uremic patients in both males and females.[38,39] Tumor necrosis factor (TNF)-α increases LH, reduces testosterone, and has no effect on FSH. TNF-α levels are increased in CKD due to inflammatory state of the disease.[40] Similar to LH, FSH levels are normal toelevated in CKD. FSH stimulates spermatogenesis and has a negative feedback via inhibin (synthesized by Sertoli cells of the ovary). Inhibin levels increases in CKD but do not correlate with FSH/LH levels. FSH secretion is also inhibited by increased estrogen in CKD, resulting in only mildly elevated level of FSH in CKD despite decreased spermatogenesis.[41–44]
Females
The pulsatile secretion of GnRH is disturbed in females as well, resulting in infertility. Gonadotrophin secretion is calcium dependent. Disturbed calcium and phosphorous metabolism in CKD results in altered gonadotrophin secretion. Serum LH level is significantly elevated and response to LHRH stimulation is delayed; however, the negative feedback of estrogen on hypothalamus is intact. The pulsatile secretion of LH is disturbed in females and some studies have even documented complete absence of pulsatile secretion. Exogenous estrogen does not induce LH surge in uremic patients, suggesting impaired positive feedback mechanism. FSH is within normal limits in follicular and luteal phases. LHRH causes only mild rise in FSH and decreased FSH/LH ratio is suggestive of hypothalamic – hypophyseal dysregulation.[45]
Uremic effect on prolactin
Serum prolactin level as well as its biological activity is increased in CKD.[46] Serum prolactin level rise correlates with decline in glomerular filtration rate. Increase in serum prolactin levels is primarily due to decreased dopaminergic inhibition of prolactin release from pituitary gland and secondarily due to decreased LHRH release. Prolactin is considered as a uremic toxin causing loss of libido, impaired erection, and infertility. It can also cause gynecomastia and galactorrhea in males and menstrual abnormalities (amenorrhea and oligomenorrhea) and galactorrhea in females (0–40% of CKD-5D patients). The prolactin increase is blunted with thyrotrophin-releasing hormone stimulation in both the sexes.[47]
Uremic effect on testicular/ovarian hormones
In addition to the effect on hypothalamus and pituitary, uremia also affects the adrenal, ovarian, and testicular hormones directly. Massachusetts Male Aging Study concluded that only dehydroepiandrosterone sulfate (adrenal androgen) and not testosterone correlated with impotence.[19] Androgen receptors are present in parasympathetic system and limbic system and thought to play an important role in erection. Uremic patients have low serum testosterone levels. Testosterone binding capacity remains normal; hence, free testosterone levels are also decreased.[48,49] Low testosterone is due to decreased production, increased metabolic and dialytic clearance, alteration in testosterone binding capacity. The normal circadian rhythm is, however, maintained. High serum LH and normal testosterone level suggests resistance at the level of interstitial cells of Leydig. Low testosterone levels along with high FSH levels (described above) leads to impaired spermatogenesis.[50] Not only spermatogenesis, but sperm motility is also affected causing oligospermia and azoospermia and thus male infertility. These changes occur early in the disease course and worsen as kidney disease progresses. A successful kidney transplantation restores the hypothalamic-pituitary-testicular axis and recovery of spermatogenesis can occur. However, this recovery depends on the extent of injury to seminiferous tubules and males with higher levels of FSH tend to have poor recovery.[50]
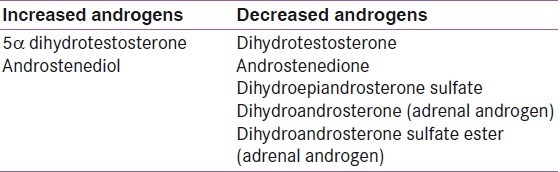
In females, estradiol concentration is normal in premenopausal uremic patients; however, in patients with hyperprolactinemia, estradiol levels are lower. Cyclical variation in estradiol concentration is absent in uremic females. Luteinization of follicles is very rare in uremic patients, and hence the progesterone rise during second half of menstrual cycle is absent (non-luteal progesterone is normal to low).[45] The various changes in androgen levels are summarized in Table 4.
Table 4.
Androgen concentration in chronic kidney disease
Other hormonal abnormalities
Role of hyperparathyroidism in sexual problems is not clear. Interleukin-2 and TNF-α reduce plasma testosterone concentration with and without LH stimulation.[51,52] Use of 1,25 dihydroxy vitamin D3 reduces prolactin secretion and lowers prolactin in uremic patients.
PRINCIPLE OF MANAGEMENT OF SEXUAL DYSFUNCTION IN CHRONIC KIDNEY DISEASE
As the sexual dysfunction in CKD is multifactorial, a careful assessment of the degree and nature of sexual dysfunction needs to be done. A detailed psychological evaluation should be carried out which includes assessment of marital and family discord, depression, stress, and life stage. Medication remains an important cause of sexual dysfunction and details of the drugs need to be noted and changed appropriately if permissible. Treatment of anemia to target range (11–12g%) and intensification of renal replacement therapy improves sexual dysfunction and quality of life in CKD patients.[25] Appropriate management of vascular insufficiency, zinc deficiency, secondary hyperparathyroidism, and autonomic dysfunction improves sexual performances in CKD patients. Endocrine assessment of serum estrogen, progesterone, and prolactin needs to be carried out. Female CKD patient with increased prolactin levels needs treatment with bromocriptine and improvement with bromocriptine is seen in patients with cyclic GnRH secretion. Sildenafil therapy improves erectile dysfunction caused by both psychogenic and organic factors.[14] For male CKD patients who do not respond to Sildenafil, treatment options include intracavernous injection of alprostadil and the use of vacuum or constriction devices.[53]
CONCLUSION
Gonadal dysfunction is very common in male and female CKD patients. The frequency of sexual dysfunction increases as renal function deteriorates. Decreased libido, difficulty in becoming aroused and achieving orgasm, erectile and ejaculatory dysfunction, lack of vaginal lubrication, menstrual irregularities, and amenorrhea are the common problems in patients with CKD. The pathophysiology of gonadal dysfunction in CKD is multifactorial, hence it is important to identify the primary etiology and treat it.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Finkelstein SH, Finkelstein FO. Evaluation of sexual dysfunction in dialysis patients. In: Nissenson AR, Fine RN, editors. Dialysis Therapy. 3rd ed. Philadelphia: Hanley and Belfus; 2002. pp. 368–73. [Google Scholar]
- 2.Palmer BF. Sexual dysfunction in uremia. J Am Soc Nephrol. 1999;10:1381–8. doi: 10.1681/ASN.V1061381. [DOI] [PubMed] [Google Scholar]
- 3.Zingraff J, Jungers P, Pélissier C, Nahoul K, Feinstein MC, Scholler R. Pituitary and ovarian dysfunctions in women on haemodialysis. Nephron. 1982;30:149–53. doi: 10.1159/000182452. [DOI] [PubMed] [Google Scholar]
- 4.Holley JL, Schmidt RJ, Bender FH, Dumler F, Schiff M. Gynecologic and reproductive issues in women on dialysis. Am J Kidney Dis. 1997;29:685–90. doi: 10.1016/s0272-6386(97)90120-7. [DOI] [PubMed] [Google Scholar]
- 5.Abram HS, Hester LR, Sheridan WF, Epstein GM. Sexual functioning in patients with chronic renal failure. J Nerv Ment Dis. 1975;160:220–6. doi: 10.1097/00005053-197503000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Bommer J, Tschöpe W, Ritz E, Andrassy K. Sexual behaviour of haemodialyzed patients. Clin Nephrol. 1976;6:315–8. [PubMed] [Google Scholar]
- 7.May AG, DeWeese JA, Rob CG. Changes in sexual function following operation on the abdominal aorta. Surgery. 1969;65:41–7. [PubMed] [Google Scholar]
- 8.Virag R. Impotence: A new field in angiology. Int Angiol. 1984;13:217–20. [Google Scholar]
- 9.Bellinghieri G, Lo Forti B, Savica V. The penile color wave doppler test in the study of uraemic impotence. Med Sci Res. 1992;20:95–7. [Google Scholar]
- 10.Sell DR, Monnier VM. End-stage renal disease and diabetes catalyze the formation of pentose derived cross-link from aging human collagen. J Clin Invest. 1990;85:380–4. doi: 10.1172/JCI114449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tarcan T, Azadzoi KM, Siroky MB, Goldstein I, Krane RJ. Age-related erectile and voiding dysfunction: The role of arterial insufficiency. Br J Urol. 1998;82(Suppl 1):26–33. doi: 10.1046/j.1464-410x.1998.0820s1026.x. [DOI] [PubMed] [Google Scholar]
- 12.Hricik DE, Schulak JA, Sell DR, Fogarty J, Monnier M. Effects of kidney-pancreas transplantation on plasma pentosidine. Kidney Int. 1993;43:398–403. doi: 10.1038/ki.1993.58. [DOI] [PubMed] [Google Scholar]
- 13.Truss MC, Djamilian MH, Tan HK, Hinrichs H, Feistner H, Stief CG, et al. Single potential analysis of cavernous electrical activity. Eur Urol. 1993;24:358–65. [PubMed] [Google Scholar]
- 14.Levy A, Crowley T, Gingell C. Non-surgical management of erectile dysfunction. Clin Endocrinol (Oxf) 2000;52:253–60. doi: 10.1046/j.1365-2265.2000.00954.x. [DOI] [PubMed] [Google Scholar]
- 15.Kim N, Vardi Y, Padma Nathan H, Daley J, Goldstein I, Saenz de Tejada I. Oxygen tension regulates the nitric oxide pathway: Physiological role in penile erection. J Clin Invest. 1993;91:437–42. doi: 10.1172/JCI116220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rajfer J, Aronson WJ, Bush PA, Dorey FJ, Ignarro LJ. Nitric oxide as a mediator of relaxation of the corpus cavernosum in response to nonadrenergic, noncholinergic neurotransmission. N Engl J Med. 1992;326:90–4. doi: 10.1056/NEJM199201093260203. [DOI] [PubMed] [Google Scholar]
- 17.Campese VM, Procci WR, Levitan D, Romoff MS, Goldstein DA, Massry SG. Autonomic nervous system dysfunction and impotence in uraemia. Am J Nephrol. 1982;2:140–3. doi: 10.1159/000166629. [DOI] [PubMed] [Google Scholar]
- 18.Zucchelli P, Turani A, Zuccala A, Santoro A, Degli Esposti E, Chiarini C. Dysfunction of the autonomic nervous system in patients with end-stage renal failure. Contrib Nephrol. 1985;45:69–81. doi: 10.1159/000410449. [DOI] [PubMed] [Google Scholar]
- 19.Feldman HA, Goldstein I, Hatzchristou DG, Krane RL. Impotence and its medical and psychosocial correlates: Results of the Massachusetts male aging study. J Urol. 1994;151:54–61. doi: 10.1016/s0022-5347(17)34871-1. [DOI] [PubMed] [Google Scholar]
- 20.Massry SG, Goldstein DA, Procci WR, Kletsky OA. Impotence in patients with uraemia.A possible role for parathyroid hormone. Nephron. 1997;19:305–10. doi: 10.1159/000180907. [DOI] [PubMed] [Google Scholar]
- 21.Muir JW. Bromocriptine improves reduced libido and potency in men receiving maintenance hemodialysis. Clin Nephrol. 1983;20:8–14. [PubMed] [Google Scholar]
- 22.Mannino DH, Klevens RM, Flanders WD. Cigarette-smoking: An independent risk factor for impotence. Am J Epidemiol. 1994;140:1003–8. doi: 10.1093/oxfordjournals.aje.a117189. [DOI] [PubMed] [Google Scholar]
- 23.Grimm RH, Jr, Grandits GA, Prineas RJ, McDonald RH, Lewis CE, Flack JM, et al. Long term effects on sexual function of 5 antihypertensive drugs and nutritional hygienic treatment in hypertensive men and women.Treatment of Mild Hypertension Study (TOMHS) Hypertension. 1997;29:8–14. doi: 10.1161/01.hyp.29.1.8. [DOI] [PubMed] [Google Scholar]
- 24.Michaelides N, Humke W. Erfahrungen bei der gynäkologischen Betrteuung von Patientinnen mit chronischer Niereninsuffizienz. Nieren-und Hochdruckkrankheiten. 1993;22:187–92. [Google Scholar]
- 25.Schaefer RM, Kokot F, Wernze H, Geiger H, Heideland A. Improved sexual function in hemodialysis patients on recombinant erythropoietin: A possible role for prolactin. Clin Nephrol. 1989;31:1–5. [PubMed] [Google Scholar]
- 26.Goodwin NJ, Valenti C, Hall JE, Friedman EA. Effects of uraemia and chronic hemodialysis on the reproductive cycle. Am J Obstet Gynaecol. 1968;100:528–35. doi: 10.1016/s0002-9378(15)33488-8. [DOI] [PubMed] [Google Scholar]
- 27.Larsen NA. Sexual problems of patients on RDT and after renal transplantation. In: Cameron JS, editor. Proceedings of the European Dialysis and Transplantation Association. Baltimore, MD: 1972. p. 271. [PubMed] [Google Scholar]
- 28.Morley JE, Distiller LA, Epstein S, Katz M, Gold C, Sagel J, et al. Menstrual disturbances in chronic renal failure. Horm Metab Res. 1979;11:68–72. doi: 10.1055/s-0028-1092683. [DOI] [PubMed] [Google Scholar]
- 29.Thaysen JH, Olgaard K, Jensen HG. Ovarian cysts in women on chronic intermittent haemodialysis. Acta Med Scand. 1975;197:433–7. doi: 10.1111/j.0954-6820.1975.tb04947.x. [DOI] [PubMed] [Google Scholar]
- 30.Schaefer F, Vogel M, Kerkhoff G, Woitzik J, Daschner M, Mehls O. Experimental uraemia affects hypothalamic amino acid neurotransmitter milieu. J Am Soc Nephrol. 2001;12:1218–27. doi: 10.1681/ASN.V1261218. [DOI] [PubMed] [Google Scholar]
- 31.Schaefer F, van Kaick B, Veldhuis JD, Stein G, Schärer K, Robertson WR, et al. Changes in the kinetics and biopotency of luteinizing hormone in hemodialyzed men during treatment with recombinant human erythropoietin. J Am Soc Nephrol. 1994;5:1208–15. doi: 10.1681/ASN.V551208. [DOI] [PubMed] [Google Scholar]
- 32.Schaefer F, Veldhuis JD, Robertson WR, Dunger D, Schärer K. The Cooperative Study Group on Pubertal Development in Chronic Renal Failure.Immunoreactive and bioactive luteinizing hormone in pubertal patients with chronic renal failure. Kidney Int. 1994;45:1465–76. doi: 10.1038/ki.1994.191. [DOI] [PubMed] [Google Scholar]
- 33.Veldhuis JD, Wilkowski MJ, Zwart AD, Urban RJ, Lizarralde G, Iranmanesh A, et al. Evidence for attention of hypothalamine gonadotropin-releasing hormone (GnRH) impulse strength with preservation of GnRH pulse frequency in men with chronic renal failure. J Clin Endocrinol Metab. 1993;76:648–54. doi: 10.1210/jcem.76.3.8445020. [DOI] [PubMed] [Google Scholar]
- 34.Bommer J, Kugel M, Schwöbel B, Ritz E, Barth HP, Seelig R. Improved sexual function during recombinant human erythropoeitin therapy. Nephrol Dial Transplant. 1990;5:204–7. doi: 10.1093/ndt/5.3.204. [DOI] [PubMed] [Google Scholar]
- 35.Sawin CT, Longcope C, Schmitt GW, Ryan RJ. Blood levels of gonadotropins and gonadal hormones in gynecomastia associated with chronic haemodialysis. J Clin Endocrinol Metab. 1973;36:988–90. doi: 10.1210/jcem-36-5-988. [DOI] [PubMed] [Google Scholar]
- 36.Rodger RS, Morrison L, Dewar JH, Wilkinson R, Ward MK, Kerr DN. Loss of pulsatile luteinising hormone secretion in men with chronic renal failure. Br Med J (Clin Res Ed) 1985;291:1598–600. doi: 10.1136/bmj.291.6509.1598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Swamy AP, Woolf PD, Cestero RV. Hypothalmic pituitary-ovarian axis in uraemic women. J Lab Clin Med. 1979;93:1066–72. [PubMed] [Google Scholar]
- 38.Grzeszcak W, Kokot F, Dulawa J. Effects of naloxone administration on endocrine abnormalities in chronic renal failure. Am J Nephrol. 1987;7:93–100. doi: 10.1159/000167442. [DOI] [PubMed] [Google Scholar]
- 39.Tay CC, Glasier AF, Illingworth PJ, Baird DT. Abnormal twenty-four hour pattern of pulsatile luteinizing hormone secretion and the response to naloxone in women with hyperprolactinaemic amenorrhoea. Clin Endocrinol (Oxf) 1993;39:599–606. doi: 10.1111/j.1365-2265.1993.tb02415.x. [DOI] [PubMed] [Google Scholar]
- 40.Van der Poll T, Romijn JA, Endert E, Sauerwein HP. Effects of tumor on the hypothalamic-pituitary-testicular axis in healthy men. Metabolism. 1993;42:303–7. doi: 10.1016/0026-0495(93)90078-3. [DOI] [PubMed] [Google Scholar]
- 41.Sasagawa I, Tateno T, Suzuki Y, Yazawa H, Ichiyanagi O, Nakada T, et al. Circulating levels of inbibin in hemodialysis males. Arch Androl. 1998;41:167–71. doi: 10.3109/01485019808994887. [DOI] [PubMed] [Google Scholar]
- 42.Rudolf K, Kunkel S, Rudolf H, Falkenhagen D, Rüting M. [Basal and gonadotropin releasing hormone-stimulated gonadotropin secretion in patients with chronic uraemia] Zentralbl Gynakol. 1988;110:683–8. [PubMed] [Google Scholar]
- 43.Lim VS, Fang VS. Restoration of plasma testosterone levels in uraemic men with clomiphene citrate. J Clin Endocrinol Metab. 1976;43:1370–7. doi: 10.1210/jcem-43-6-1370. [DOI] [PubMed] [Google Scholar]
- 44.Barton CH, Mirahamadi MK, Vairi ND. Effects of long-term testosterone administration on pituitary-testicular axis in end-stage renal failure. Nephron. 1982;31:61–4. doi: 10.1159/000182618. [DOI] [PubMed] [Google Scholar]
- 45.Lim VS, Henriquez C, Sievertsen G, Frohman LA. Ovarian function in chronic renal failure: Evidence suggesting hypothalamic anovulation. Ann Intern Med. 1980;93:21–7. doi: 10.7326/0003-4819-93-1-21. [DOI] [PubMed] [Google Scholar]
- 46.Biasioli S, Mazzali A, Foroni R, D’Andrea G, Feriani M, Chiaramonte S, et al. Chronobiological variations of prolactin (PRL) in chronic renal failure (CRF) Clin Nephrol. 1988;30:86–92. [PubMed] [Google Scholar]
- 47.Bommer J, Ritz E, del Pozo E, Bommer G. Improved sexual function in male haemodialysis patients on bromocriptine. Lancet. 1979;2:496–7. doi: 10.1016/s0140-6736(79)91553-8. [DOI] [PubMed] [Google Scholar]
- 48.Ramirez G, Butcher D, Brüggemeyer CD, Ganguly A. Testicular defect: The primary abnormality in gonadal dysfunction of uraemia. South Med J. 1987;80:698–701. doi: 10.1097/00007611-198706000-00008. [DOI] [PubMed] [Google Scholar]
- 49.Johansen KL. Testosterone metabolism and replacement therapy in patients with end-stage renal disease. Semin Dialysis. 2004;17:202–208. doi: 10.1111/j.0894-0959.2004.17307.x. [DOI] [PubMed] [Google Scholar]
- 50.Anantharaman P, Schmidt RJ. Sexual function in chronic kidney disease. Adv Chr Kidney Dis. 2007;14:119–25. doi: 10.1053/j.ackd.2007.01.002. [DOI] [PubMed] [Google Scholar]
- 51.Wark JD. Regulation by 1,25-dihydroxyvitamin D3 (1,25(OH) 2 D3) of specific gene expression in GH pituitary cells. In: Norman AW, Schaefer K, Grigolet HG, Herrath DV, editors. Vitamin D: A Chemical, Biochemical and Clinical Update. Berlin: Walter de Gruyter; 1985. pp. 901–2. [Google Scholar]
- 52.Mauduit C, Jaspar JM, Poncelet E, Charlet C, Revol A, Franchimont P, et al. Tumor necrosis factor-alpha antagonizes follicle-stimulating hormone action in cultured sertoli cells. Endocrinology. 1993;133:69–76. doi: 10.1210/endo.133.1.8319591. [DOI] [PubMed] [Google Scholar]
- 53.Finkelstein FO, Shirani S, Wuerth D, Finkelstein SH. Therapy Insight: Sexual dysfunction in patients with chronic kidney disease. Nat Clin Pract Nephrol. 2007;3:200–7. doi: 10.1038/ncpneph0438. [DOI] [PubMed] [Google Scholar]


