Abstract
Aim:
Deficiency of Vitamin D is prevalent in the general population, especially in Chronic Kidney Disease (CKD) patients. The exact prevalence of Vitamin D deficiency is unknown in post renal transplant recipients. The classical and non-classical effects of vitamin D deficiency are complicated by the use of steroids and calcineurin inhibitors (CNIs) in the renal transplant population. The aim of this study is to document the prevalence of Vitamin D deficiency in the post renal transplant population.
Materials and Methods:
A total of 51 renal transplant recipients under follow-up at Indraprastha Apollo Hospital, between June 2009 and March 2011, were enrolled in this study. Parathormone (PTH), 25(OH)-vitaminD3, calcium, and phosphate levels were determined in all the patients. The patients were then classified into different groups based on the severity of the Vitamin D deficiency, time since transplantation, and level of graft function.
Results:
Overall, four patients (8%) were vitamin D sufficient, 17 patients (33%) insufficient, 26 patients (51%) mildly deficient, and four (8%) severely deficient. The degree of deficiency did not differ with reference to the time since transplant or level of graft function. Sixty-nine percent had high PTH level, 22% were normal, and 9% had a low parathyroid hormone level. There was an inverse correlation between Vitamin D deficiency and serum PTH level.
Conclusion:
In this study, there was a high prevalence of vitamin D deficiency in renal transplant recipients. This did not get corrected, despite nutritional improvement or normalization of the glomerular filtration rate (GFR) post transplantation. Therefore, the study emphasizes routine evaluation and proper supplementation of Vitamin D in all post renal transplant patients.
Keywords: 25(OH)-vitamin D3, calcium, phosphate, parathormone, renal transplant recipients, Vitamin D
INTRODUCTION
Nutritional Vitamin D deficiency is prevalent in the general population of India.[1] Hypovitaminosis D has also been demonstrated in CKD patients.[2,3] The post transplant period is associated with improved renal function and resumption of 1α-hydroxylation by the graft kidney, but it does not correct the nutritional Vitamin D deficiency. Rapid bone loss often occurs in the first year post transplant, and is presumed to be a result of steroids and other immunosuppressive therapies.
In our country, the exact prevalence of nutritional Vitamin D deficiency in this population is unknown. This study has been conducted to quantify hypovitaminosis D. It also aims to analyze the correlation of the level of Vitamin D with different levels of graft function, time since transplant, and other biochemical parameters like parathromone, calcium, and phosphorus.
MATERIALS AND METHODS
A total of 51 post transplant patients, either admitted to wards or attending the outdoor clinic at Indraprastha Apollo Hospital, were enrolled in the study. The study was initiated with the approval of the Institutional Ethics Committee and an informed consent was obtained. The deficiency was classified as per the Kidney Disease Outcomes Quality Initiative (KDOQI) guidelines:[4]
Sufficient: more than 30 ng / ml
Insufficient: 16 – 30 ng / ml
Mild deficiency: 5-15 ng / ml
Severe deficiency: less than 5 ng / ml
Patients with malabsorption syndrome , chronic diarrhea, and ileostomy were excluded. Vitamin D was measured by the electrochemiluminescence immunoassay (ECLIA), using cobase immunoassay analyzer.
The patients were divided into three groups according to the time since transplant, namely, peri-transplant (within 15 days of transplant), intermediate (16 days to one year), and late transplant group (more than one year).
The study population was also divided into three groups as per the eGFR (calculated by the Cockcroft-gault formula); first — eGFR more than 60 ml / minute, second — eGFR 20 – 59 ml / minute, and third — e GFR less than 20 ml / minute.
Statistical analysis
An independent t-test was used to compare the mean values between the groups. Logistic regression analysis was used to examine the level of association between the Vitamin D level and PTH, and calcium and phosphorous. A p-value < 0.05 was considered statistically significant. We used the SPSS package version 16 for statistical analysis.
RESULTS
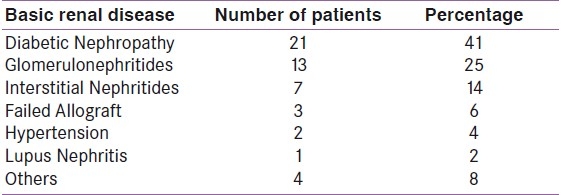
Of a total of 51 patients; eight (16%) were women and 43 (84%) were men. The basic renal disease of the patients is shown in Table 1.
Table 1.
Basic renal disease
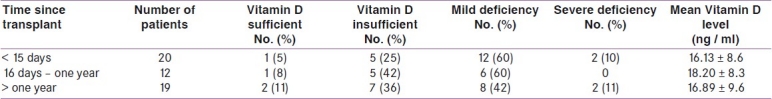
Overall, 8% (n = 4) of the study population had sufficient serum vitamin D level, 33% (n = 17) had an insufficient serum vitamin D level, 51% (n = 26) had mild deficiency, and 8% (n = 4) had severe deficiency [Figure 1]. The mean Vitamin D levels in different groups according to the time since transplant are shown in Table 2. No significant difference was observed between the peri-transplant and intermediate groups (P = 0.3587), and the intermediate and late groups (P = 0.3906).
Figure 1.
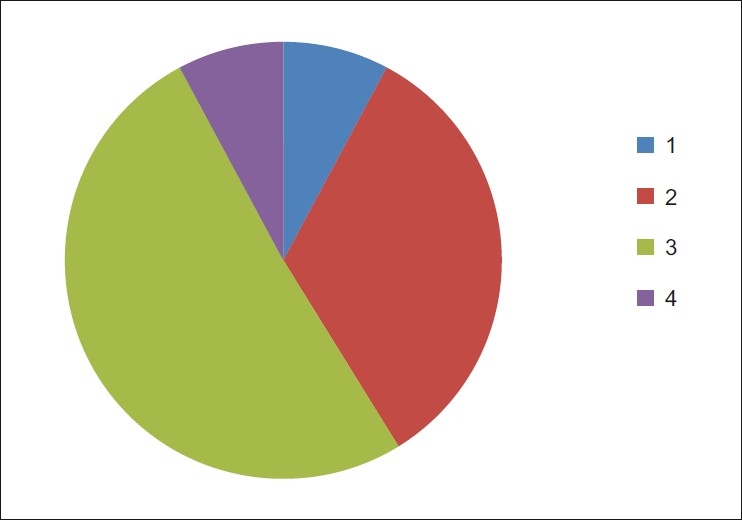
Pie diagram showing the overall status of Vitamin D in the study population: 1. Vitamin D sufficient, 2. Vitamin D insufficient, 3. mild deficiency, 4. severe deficiency
Table 2.
Vitamin D status according to time since transplant
The median intact PTH level in the study population was 358 pgm / ml (range 7.8 pgm / ml-502 pgm / ml). Sixty-nine percent of the subjects had high parathyroid levels, whereas, 22% had normal PTH levels, and 9% had low values (as per the KDOQI guidelines for the range of eGFR). Regression analysis revealed a negative correlation between PTH and 25(OH)-vitamin D3 levels (r = - 0.317). Most of the patients had an eGFR of more than 60 ml / minute (n-32), whereas, only eight patients had eGFR less than 20 ml / minute. Regression analysis did not reveal any correlation between 25(OH)-vitamin D3 and graft function (r = 0.0725).
DISCUSSION
In our study, 92% of the patients had hypovitaminosis D; 33% had insufficiency, 51% had mild deficiency, and 8% had severe deficiency. There was an inverse correlation between the levels of PTH and Vitamin D. However, there was no correlation of the Vitamin D levels with eGFR and time since transplant.
Mithal et al.,[1] reported that 96% of the neonates, 91% of healthy school girls, 78% of healthy hospital staff, and 84% of the pregnant women had hypovitaminosis D. A study by Sakhuja et al.,[2] demonstrated deficiency of 25(OH)-vitamin D3 was seen universally in CKD patients and more than three-quarters of the healthy control subjects.
Renal transplant corrects the states of 1-α hydroxylation and hyperparathyroidism over a period of six months to one year. In view of this, we divided the post-transplant period into three groups; first — the peri-transplant group (within 15 days of transplantation — probably the group representing extension of pretransplant hypovitaminosis D, second — the intermediate group (16 days to one year), and third — the late transplant group (more than one year). The mean Vitamin D levels in each group were 16.13 + / - 8.64 ngm / ml, 18.2 + / - 8.26 ngm / ml, 16.89 + / - 9.57 ngm / ml, respectively. There was no statistically significant difference observed between the above-mentioned groups. The above finding implied that improvement of GFR in transplant recipients was not associated with improvement in the 25(OH)-vitaminD3 status. This was in accordance with the study by Farmer et al.[5]
In our study population, the median serum intact PTH was 358 pgm / ml, with a range of 7.8 pgm / ml – 502pgm / ml. Sixty-nine percent (n = 35) had high PTH; 22% (n = 11) had normal PTH, and 9% (n = 5) had low PTH. We found a negative correlation between Vitamin D and PTH levels (r = - 0.317). The PTH level decreased in many patients post transplantation, secondary to improvement in kidney function and restoration of 1α-hydroxylation. However, persistent hyperparathyroidism in the post-transplant period was also prevalent and multi-factorial; for example, persistent tertiary adenoma, post-transplant hypercalciuria, impaired graft function, steroid-induced impaired intestinal calcium absorption, and hypovitaminosis D. In a recent study by Reinhardt et al.,[6] which included 129 renal transplant recipients, the authors demonstrated an inverse correlation between 25(OH)-vitamin D3 and PTH, eight months post transplantation. Stavroulopoulos et al.,[7] in their study, also found an inverse correlation between 25(OH)-vitamin D3 and the PTH serum levels, in long-term transplant recipients.
Most of the patients in the study group (62%) had good graft function, 22% had intermediate graft function, and 16% had poor graft function. Two of the eight patients with poor graft function had severe deficiency; however, it was not statistically significant due to the small number of patients in this category. The correlation between serum creatinine and serum 25(OH)-vitamin D3 did not reach statistical significance (r = 0.0725). This was in accordance with the study by Bettina Ewers.[8] Our data implied that hypovitaminosis D was almost equally distributed in all the three graft function groups. It was possibly explained by the fact that good graft function could improve 1α hydroxylation and thereby improve the 1, 25(OH)2 vitaminD3 status, but not the 25(OH)-vitaminD3 deficiency.
CONCLUSION
In this study, there was a high prevalence of hypovitaminosis D in renal transplant recipients. This did not get corrected despite nutritional improvement or normalization of GFR, post transplantation. Therefore, the study emphasizes routine evaluation and proper supplementation of 25(OH)-vitaminD3 in all post renal transplant patients. It would be reasonable to supplement the vitamin, as recommended, for normal people.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Mithal A, Wahl DA, Bonjour JP, Burckhardt P, Dawson-Hughes B, Eisman JA, et al. IOF Committee of Scientific Advisors (CSA) Nutrition Working Group.Global vitamin D status and determinants of hypovitaminosis D. Osteoporosis Int. 2009;20:1807–20. doi: 10.1007/s00198-009-0954-6. [DOI] [PubMed] [Google Scholar]
- 2.Jabbar Z, Aggarwal PK, Chandel N, Sakhuja V, Jha V. Vitamin D deficiency in Indian CKD patients. Ind J Nephrology. 2007;17:93–4. [Google Scholar]
- 3.Jabbar Z, Aggarwal PK, Kohli HS, Jha V. High prevalence of vitamin D deficiency in north Indian adults is exacerbated in those with chronic kidney disease. Nephrology. 2009;14:345–9. doi: 10.1111/j.1440-1797.2008.01082.x. [DOI] [PubMed] [Google Scholar]
- 4.NKF / KDOQI Clinical Practice Guidelines For Bone Metabolism And Disease In Chronic Kidney Disease. Am J Kidney Dis. 2003;42(Suppl 3):S1–202. [PubMed] [Google Scholar]
- 5.Farmer CK, Hampson G, Abbs IC, Hilton RM, Koffiman CG, Fogelman I, et al. Late low dose steroid withdrawal in renal transplant recipients increases bone formation and bone mineral density. Am J Transplant. 2006;6:2929–36. doi: 10.1111/j.1600-6143.2006.01557.x. [DOI] [PubMed] [Google Scholar]
- 6.Reinhardt W, Bartelworth H, Jockenhövel F, Schmidt-Gayk H, Witzke O, Wagner K, Heemann UW, Reinwein D, Philipp T, Mann K. Sequential changes of biochemical bone parameters after kidney transplantation. Nephrol Dial Transplant. 1998;13:436–42. doi: 10.1093/oxfordjournals.ndt.a027843. [DOI] [PubMed] [Google Scholar]
- 7.Stavroulopoulos A, Cassidy MJ, Porter CJ, Hosking DJ, Roe SD. Vitamin D status in renal transplant recipients. Am J Transplant. 2005;7:2546–52. doi: 10.1111/j.1600-6143.2007.01978.x. [DOI] [PubMed] [Google Scholar]
- 8.Ewers B, Gasbjerg A, Moelgaard C, Frederiksen AM, Marckmann P. Vitamin D status in kidney transplant patients: Need for intensified routine supplementation. Am J Clin Nutr. 2008;87:431–7. doi: 10.1093/ajcn/87.2.431. [DOI] [PubMed] [Google Scholar]


