Abstract
A 67-year-old female was admitted to the hospital with a history of lethargy, memory impairment, confusion, anorexia and gait imbalance for 2 weeks duration. She did not have any history of fall or head injury. She had total hip replacement 1 year back and was on orthopedic follow-up. Magnetic resonance imaging (MRI) on admission revealed no focal abnormalities. Routine biochemistry detected hypercalcemia, and she was treated with I/V fluid, diuretics and glucocorticoids. She was screened thoroughly to exclude occult malignancy. After 7 days of admission, a follow-up orthopedic prescription revealed that she was getting inj. Arachitol 6 lac units every week for last 3 months. On the 9th day of admission, she was detected to have very high serum 25(OH) vitamin D level (254.70 ng/ml). Patient was discharged after 2 weeks after her serum calcium came down to normal range with the advice of no dietary calcium and vitamin D intake. Her 25(OH) vitamin D level remained high for the next 6 months. Now she is completely asymptomatic and her serum 25(OH) D is normal.
Keywords: Hypercalcemia, injectable vitamin D, vitamin D toxicity
INTRODUCTION
Vitamin D is a frequently prescribed drug for various indications. Unfortunately, there is poor awareness of the various preparations and dosages of this hormone. This sometimes leads to easily avoidable errors in prescription, with unwanted adverse effects. This article highlights such a case.
CASE REPORT
Mrs. P. G., a 67-year-old housewife, got admitted to the hospital with a history of memory impairment, confusion, lethargy, generalized weakness and gait imbalance of 2 weeks duration. She did not give any history of fall or head injury. There was no history of fever, headache, cough, urinary symptoms or any focal weakness. She was hypertensive for last 20 years, which was well under control with Amlodipine (5 mg/day). Her part history revealed that she had undergone total right hip replacement 1 year back and had regular follow-up checkups with the orthopedic surgeon.
Examination
On examination, the patient was conscious and co- operative, oriented, but with cognitive impairment and some irrelevant talk and could not recollect recent events.
The other findings were as follows: BP 170/100, a febrile pulse 100/mt, RR 20/mt, chest clear. Cardiovascular examination did not reveal any abnormality. Abdomen showed no hepatosplenomegaly. Central nervous system (CNS) examination showed that there was generalized muscle weakness without any focal deficit. Jerks were normal. Planters were down.
MRI brain showed age-related diffuse cerebral cortical atrophy. There was no infarction or space-occupying lesion.
The laboratory investigations revealed the following results: Hb 11.7 g/dl, total count 10,900, poly 68%, lymphocytes 27%, monocytes 3%, eosinophils 2%, erythrocyte sedimentation rate (ESR) 18 mm/1 hour, urine R/E NAD, urea 42 mg/dl, creatinine 1.9 mg/dl, Na 140 mEq/l, potassium 3.5 mEq/l, FT4 1.38 ng/dl, thyroid stimulating hormone (TSH) 0.80 mIU/l, cholesterol 167 mg/dl, low density lipoprotein (LDL) 96 mg/dl, high density lipoprotein cholesterol (HDL-C) 40 mg/dl, triglyceride (TG) 154 mg/ dl, serum bilirubin 0.93 mg/dl, albumin 3.2 g/ dl, globulin 5.0 g/dl, alanine transaminase (ALT) 68 IU/l, aspartate transaminase (AST) 48 IU/l. Cerebrospinal fluid (CSF) study revealed normal results (glucose 100 mg/dl, protein 33.1 mg/dl); serum calcium level was 14.0 mg/dl and magnesium level was 1.7 mg/dl.
Electrocardiogram (ECG) showed bifasicular block. Echocardiography revealed concentric left ventricular hypertrophy. Ultrasound of the abdomen was normal. High-resolution computed tomography (HRCT) chest was essentially normal
On the 7th day of admission, repeat serum calcium revealed a level of 13.2 mg/dl. Parathormone (PTH) was 14.8 pg/ ml and vitamin D 25(OH) was 254.7 ng/ml.
Mammography results were normal.
Course in hospital
Neurological exam and magnetic resonance imaging (MRI) brain ruled out any cerebral lesion. For hypercalcemia, she was investigated for any occult malignancy which was ruled out., She was treated with intravenous fluid, diuretics and glucocorticoid and was improving clinically. On the 7th day, a follow-up prescription from orthopedic surgeon revealed that she received inj. Arachitol 6 lacs IU intramuscularly, every week for the last 4 months On the 9th day of admission, her serum vitamin D 25(OH) was detected to be high and a diagnosis of hypervitaminosis D leading to hypercalcemia was considered. She was improving clinically and her serum calcium came down to normal in the next 2 weeks and was discharged with prescription of antihypertensive and with the advice to take food with no vitamin D and calcium. She continued to have high vitamin D level even after 4 months of discharge [vitamin D 25(OH) 215.52 ng/ml] which came down to normal (66.67 ng/ml) 6 months after discharge from the hospital.
At present, she is completely asymptomatic. A repeat vitamin D 25(OH) after 6 months showed a level of 77.67 ng/ml.
DISCUSSION
In this case report, a classical case of hypervitaminosis D and its consequences is being presented. Hypervitaminosis D can occur when pharmaceutical vitamin D is taken in excess as in this reported case. The manifestation could be related to hypercalcemia, as in this case.[1] There may be features of hypercalciuria or metastatic calcification, but in this case they were not found.
Symptoms of vitamin D toxicity[2]
Hypercalcemia
Hypercalciuria
Kidney stones
Hyperphosphatemia
Polyuria
Polydipsia
Ectopic calcification of soft tissues (kidney and lung)
Nausea/vomiting
Anorexia
Constipation
Headache
Hypertension
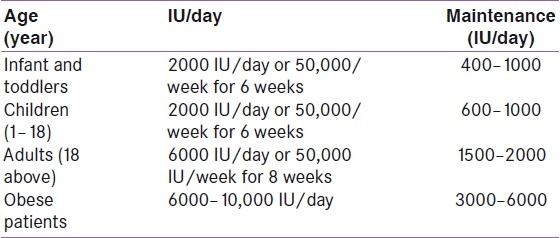
Diagnosis of vitamin D toxicity is confirmed by high serum calcium, high serum vitamin D 25(OH) and normal PTH. Treatment consists of stopping of vitamin D intake and avoiding all calcium containing food in diet (such as milk, curd, etc.). Considering the awareness on vitamin D deficiency across the globe, it is always better to follow the guidelines laid down by several consensus groups. The recently published clinical practice guidelines (June 2011) by the American Endocrine Society on evaluation, treatment and prevention of vitamin D deficiency are given in Table 1
Table 1.
Treatment and prevention strategies of vitamin D deficiency (to achieve a blood level of 25(OH)D above 30 ng/ml[3])
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Hathcoch JN, Glao A, Vieth R, Haeny R. Risk assessment for vitamin D. Am J Clin Nutr. 2007;85:6–18. doi: 10.1093/ajcn/85.1.6. [DOI] [PubMed] [Google Scholar]
- 2.Bonillon R. Endocrinology. 6th ed. 2010. Vitamin D: From photosynthesis, metabolism, and action to clinical application; pp. 1089–110. [Google Scholar]
- 3.Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911–30. doi: 10.1210/jc.2011-0385. [DOI] [PubMed] [Google Scholar]


