Abstract
A 50-year-old woman presented with chronic epigastric abdominal pain and constipation. She underwent diagnostic upper and lower endoscopy for further evaluation. Several hours following the procedure, she developed chest and subcutaneous emphysema of her upper chest, neck, and face. A chest X-ray demonstrated marked subcutaneous emphysema, pneumopericardium, and pneumomediastinum. A CT scan revealed a small leak at the rectosigmoid junction. Because the patient did not have peritoneal signs, she was treated conservatively and discharged on hospital day seven. The complications of both esohagogastroduodenoscoy, and colonoscopy are discussed, with an emphasis on perforations.
Keywords: pneumopericardium, pneumomediastinum, subcutaneous emphysema, pneumoretroperitoneum
Introduction
Esophagogastroduodenoscopy (EGD) and colonoscopy are commonly utilized procedures in the evaluation of gastrointestinal disease. According to a study by the Center for Disease Control and Prevention (CDC), physicians performed approximately 14.2 million colonoscopies and 2.8 million sigmoidoscopies in the United States in 2002.1 While both are deemed relatively safe, complications include abdominal pain and bloating, nausea, diarrhea, hemorrhage, and perforation. We present a rare case report following diagnostic colonoscopy resulting in extraperitoneal leak, causing marked upper body subcutaneous emphysema, pneumopericardium, pneumomediastinum and pneumoretroperitoneum.
Case Report
A 50-year-old woman with intermittent bouts of mid-epigastric pain for the previous five years, on occasion associated with nausea and vomiting, became worse in the last two weeks. She reported chronic constipation with as few as one bowel movement per week. The patient denied bright red blood, melena, fever, chills, nausea, vomiting, or any other constitutional symptoms. Her medical history included migraine headaches, allergic rhinitis, hyperlipidemia, tubal ligation, and negative EGD two years before. Her symptoms were somewhat relieved by laxatives. The rest of the work-up was unremarkable and she was scheduled for upper endoscopy and colonoscopy on the same day.
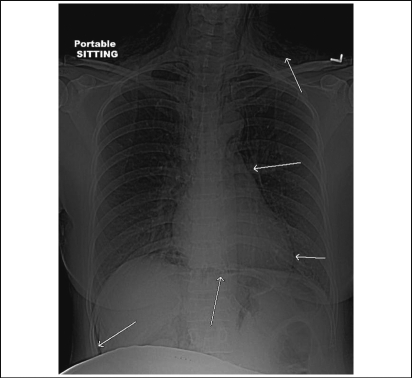
Both the EGD and colonoscopy were diagnostically negative without any biopsies taken and no acute complications were noted during and immediately after the procedure. Several hours later, the patient developed chest pain and presented to the emergency department where she had evidence of subcutaneous emphysema of her upper chest, neck, and face. The patient was afebrile but tachycardic, and had leukocytosis up to 18,300 with 11% bands. The patient subsequently developed abdominal discomfort without obvious peritoneal signs, chest radiograph revealed marked subcutaneous emphysema, pneumopericardium, and pneumomediastinum (Figure 1).
Figure 1.
Chest radiograph showing marked subcutaneous emphysema, pneumopericardium and pneumomediastinum.
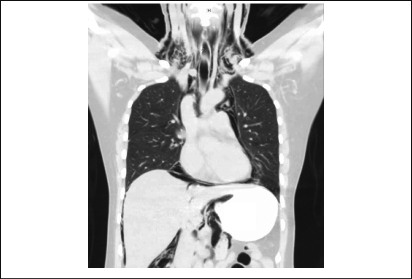
CT scan of the chest, abdomen, and pelvis showed extensive emphysema in the neck, mediastinum, and retroperitoneum, and possible intraperitoneal air (Figure 2). Cardiothoracic and general surgeons were consulted. CT esophagram scan was performed as the patient could not tolerate fluoroscopy, but revealed no leak. The patient was admitted, started on broad-spectrum antibiotics; because she did not have peritoneal signs she was followed clinically with serial examinations. A repeat CT scan of the chest, abdomen, and pelvis was performed the next day showing a small contrast leak into the mesentery at the rectosigmoid junction (Figure 3). The patient remained clinically stable and afebrile with the leukocytosis improving over the next three days. Clear liquids were started on hospital day 5 and she was discharged on full liquids 2 days later. On follow up, the patient reported no problems and the marked facial, neck, and upper chest emphysema had completely resolved.
Figures 2.
Coronal view of CT chest and abdomen showing extensive emphysema in the neck, mediastinum and retroperitoneum, and possible intraperitoneal air.
Figure 3.
Sagital view of CT of the pelvis showing a small leak into the mesentery at the rectosigmoid junction.
Discussion
Although perforation is a relatively rare complication following EGD or colonoscopy, it is the most worrisome. Post-EGD perforations occur between 0.03%–0.1% of the time,2–3 while post-colonoscopy perforations occur at a rate of 0.4%–1.9%4 with a mortality rate of 0.02%–0.15%.5 Perforations occur more commonly with therapeutic than diagnostic endoscopy.5–6 Several factors have been found to increase the risk of complications, including concurrent diverticulitis, inflammatory bowel disease, tumors, old age, diabetes, and cardiovascular disease.7–8 Patients with intraperitoneal perforations typically present within 12 hours of the procedure with pain, fever, abdominal distension, nausea and vomiting, tachycardia, hypotension, and peritoneal signs.6,9
Subcutaneous emphysema following colonoscopy can be palpated as crepitus and is a common manifestation of extraperitoneal air traveling along the track of the mesentery. In these rare situations described only in case reports, radiography can reveal collections of extraperitoneal air, such as pneumoperitoneum, pneumoretroperitoneum, pneumopericardium, pneumomediastinum, and pneumothorax.4–5 Extraperitoneal perforations without peritoneal signs can be managed conservatively with nasogastric suction, nothing by mouth, bowel rest, and empiric antibiotics, while larger perforations (usually with intraperitoneal air as well) require primary closure of the bowel perforation with or without bowel segment resection.9 Endoscopic clipping of the perforation has also been described.4 Regardless of conservative or surgical management, extraperitoneal air commonly resolves within 72 hours.5 Because this patient did not have peritoneal signs, a conservative approach was taken and followed with serial abdominal examinations. This approach shows the importance of clinical judgment and surgeon experience in deciding whether to operate or treat conservatively.
Upper and lower endoscopy is often used in the evaluation of gastrointestinal complaints and, although safe, perforations do occur. Rarely, the perforation is extraperitoneal leading to subcutaneous emphysema and other collections of air, such as pneumopericardium, pneumomediastinum, pneumoperitoneum and pneumoretroperitoneum. Management depends on the size of the perforation as well as systemic involvement. Conservative treatment may be utilized in patients with contained perforations and no peritoneal signs. Extraperitoneal air is commonly reabsorbed within 72 hours with the remainder of recovery focused on regaining bowel function.
Acknowledgements
We would like to thank Jay Shepard MD, for his help in choosing the radiographic images for this study.
Footnotes
None of the authors identify any conflict of interest.
References
- 1.Seef LC, Richards TB, Shapiro JA, Nadel MR, Manninen DL, Given LS. How many endoscopies are performed for colorectal cancer screening? Results for the CDC's survey of endoscopic capacity. Gastroent. 2004;127:1670–1677. doi: 10.1053/j.gastro.2004.09.051. [DOI] [PubMed] [Google Scholar]
- 2.Merchea A, Cullinane DC, Sawyer MD, et al. Esophagogastroduodenoscopy-associated gastrointestinal perforations: A single-center experience. Surgery. 2010;148:876–882. doi: 10.1016/j.surg.2010.07.010. [DOI] [PubMed] [Google Scholar]
- 3.Kavic SM, Basson MD. Complications of endoscopy. Am J Surg. 2001;181:319–332. doi: 10.1016/s0002-9610(01)00589-x. [DOI] [PubMed] [Google Scholar]
- 4.Park NS, Choi JH, Lee DH, et al. Pneumoretroperitoneum, pneumomediastinum, pneumopericardium, and subcutaneous emphysema after colonoscopic examination. Gut Liver. 2007;1(1):79–81. doi: 10.5009/gnl.2007.1.1.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bakker J, van Kersen F, Bellaar SJ. Pneumopericardium and pneumomediastinum after polypectomy. Endoscopy. 1991;23(1):46–47. doi: 10.1055/s-2007-1010607. [DOI] [PubMed] [Google Scholar]
- 6.Majeski J, Lynch W, Durst G. Esophageal perforation during esophagogastroduodenoscopy. Am J Surg. 2009;198:e56–e57. doi: 10.1016/j.amjsurg.2009.02.008. [DOI] [PubMed] [Google Scholar]
- 7.Newstead B, Smith JE. A pain in the neck. JR Army Med Corps. 2010;156(2):100–101. doi: 10.1136/jramc-156-02-07. [DOI] [PubMed] [Google Scholar]
- 8.Capello M, Randazzo C, Peralta S, et al. Subcutaneous emphysema, pneumomediastinum, pneumoperitoneum after diagnostic colonoscopy for ulcerative colitis: A rare but possible complication in patients with multiple risk factors. Int J Colorectal Dis. 2011;26(3):393–394. doi: 10.1007/s00384-010-1005-7. [DOI] [PubMed] [Google Scholar]
- 9.Avgerinos DV, Llaguna OH, Lo AY, et al. Evolving management of colonoscopic perforations. J Gastrointest Surg. 2008;12:1783–1789. doi: 10.1007/s11605-008-0631-7. [DOI] [PubMed] [Google Scholar]