Abstract
Introduction:
Tobacco use remains a major public health problem worldwide. Water-pipe smoking is spreading rapidly and threatening to undermine the successes achieved in tobacco control.
Methods:
A school-based longitudinal study in the city of Irbid, Jordan, was performed from 2008 to 2010. All seventh-grade students in 19 randomly selected schools, out of a total of 60 schools in the city, were enrolled at baseline and surveyed annually.
Results:
Of the 1781 students enrolled at baseline 1,701 (95.5%) were still in the study at the end of the second year of follow-up (869 boys, median age at baseline 13 years). Ever and current water-pipe smoking were higher than those of cigarette smoking at baseline (ever smoking: 25.9% vs. 17.6% and current smoking: 13.3% vs. 5.3% for water-pipe and cigarette smoking, respectively; p < .01 for both) but cigarette smoking caught up by the second year of follow-up (ever smoking: 46.4% vs. 44.7%; p = .32 and current smoking: 18.9% vs. 14.9%; p < .01). Water pipe–only smokers at baseline were twice as likely to become current cigarette smokers after 2 years compared with never smokers (relative risk (RR) = 2.1; 95% CI = 1.2, 3.4). A similar pattern was observed for cigarette-only smokers at baseline (RR = 2.0; 95% CI = 0.9, 4.8).
Conclusions:
Prevalence of water-pipe and cigarette smoking increased dramatically over the 2-year follow-up period with similar patterns in boys and girls, although girls had lower prevalence in all categories. Water-pipe smoking at baseline predicted the progress to cigarette smoking in the future and vice versa.
Introduction
Tobacco use continues to be the leading cause of preventable morbidity and mortality worldwide (World Health Organization, 2008). Due to the adoption of successful policies and interventions, tobacco use has been on the decline over the past 30 years in most developed societies, especially among adults (Centers for Disease Control and Prevention, 2007; van der Wilk and Jansen, 2005). These successes, however, are still limited in many parts of the world, mainly due to lack of adoption, or enforcement, of tobacco control policies (World Health Organization, 2011). The Eastern Mediterranean region (EMR), consisting mainly of Arab countries, is one region that continues to experience an escalating tobacco epidemic. For example, between 1990 and 1997, cigarette consumption increased 24% in the Middle East, while most other regions did not witness such a trend (Shafey, 2007). The EMR, moreover, is threatened by a reemerging method of tobacco use, namely water-pipe smoking (a.k.a., hookah, shisha, narghile) (Maziak, Ward, Afifi Soweid, & Eissenberg, 2004).
A water pipe has a head, a body, a bowl, and a hose with a mouthpiece. The tobacco is filled in a concavity in the head, and a piece of lit charcoal is placed on top of the tobacco. When users inhale through the mouthpiece, air is drawn over the charcoal, becomes heated, and produces smoke as it passes through the tobacco on its way through the water and to the smoker (Shihadeh, 2003).
Epidemiological trends in water-pipe smoking are alarming, and what started as a “social” phenomenon in the EMR has become a global phenomenon. Prevalence estimates of water-pipe smoking surpassed those of cigarette smoking among youth in the EMR, and the rest of the world is catching up. According to various estimates, about a quarter of youth in several societies in the EMR are current (past month) water-pipe smokers (Maziak, 2011). These trends are even registering at younger ages, as was demonstrated by the Global Youth Tobacco Survey (GYTS). The GYTS is the most comprehensive global surveillance effort of tobacco use among youth involving more than half a million of 13- to 15-year olds assessed from 209 surveys in 95 countries. Current smoking of cigarettes among middle/high school students was reported to be 10.3%, 4.0%, and 8.5%, in Jordan (2007), Egypt (2005), and Lebanon (2005), respectively. Current smoking of “tobacco products other than cigarettes” among middle/high school students was reported to be 9.5%, 10.1%, and 40.0%, in Jordan (2007), Egypt (2005), and Lebanon (2005), respectively. Recent time trends from the GYTS (1999–2008) shows that while cigarette smoking is either stable or declining, other forms of tobacco use are showing a rising trend, most notably water-pipe smoking (Warren et al., 2009). Jordan is one example of this phenomenon, where among students 13–15 years of age, current cigarette smoking has declined from 17.7% in 2003 to 10.3% in 2007, while current use of “other tobacco products” increased from 20.0% to 26.4% in the same time period (Centers for Disease control and Prevention, 2008). This other tobacco products are widely accepted as being water-pipe smoking in that part of the world.
Despite widespread misperception about water pipe’s reduced harm and addictiveness (frequently misattributed to the “filtering” effect of water), available evidence suggests that water pipe use is associated with considerable harm and is addictive (Akl et al., 2010; Maziak, 2011; Raad et al., 2010). Moreover, water-pipe smoking can also undermine tobacco control, as it can be used as a replacement for cigarettes among quitters, or can serve as a gateway to cigarette (Jensen, Cortes, Engholm, Kremers, & Gislum, 2010; Ward et al., 2007). In this study, we report for the first time the trends in cigarette and water-pipe smoking among adolescents from a longitudinal, school-based study in Irbid, Jordan. The objectives of this study are to (a) assess time trends in smoking initiation among youth for both cigarette and water pipe, (b) assess the validity of youth’s perceptions regarding future intentions to smoke, and (c) evaluate the gateway hypothesis that water-pipe use increases the risk of subsequent cigarette smoking.
Methods
Participants
The study methodology has been published elsewhere (Mzayek, Khader, Ward, Eissenberg & Maziak, 2011). Briefly, a list of city school names and number of students was obtained from the Department of Education in the city of Irbid, Jordan (population ≈330,000) and was verified for accuracy and completeness. Nineteen out of a total of 60 schools were randomly selected in Fall 2007 using a stratified, cluster sampling. The schools were stratified by gender (male schools, female schools, and mixed-gender schools) and by type (public, private) to ensure representativeness of the sample. Within each gender/type stratum, a random sample of schools was selected with probability proportional to size. All seventh-grade students in the selected schools were enrolled in the study and were followed up annually for 2 years (eighth and ninth grades). There were 5,287 seventh graders in the city of whom 1,876 were invited to participate and 1,781 (95%) agreed to enroll in the study.
The survey questionnaire was developed in accordance with international guidelines (World Health Organization, 1998), as well as instruments that were used and tested in Arabic (Maziak, Eissenberg, & Ward, 2005; Tamim et al., 2007). The questionnaire was comprised of four modules: sociodemographic module (including, age, gender, number of persons in the household, number of rooms of the house, father and mother’s education level, and daily allowance), cigarette smoking module, water-pipe smoking module, and the fourth module asking about tobacco ads and smoking warnings, family and school environment, peer influences, and students’ attitude to quitting smoking. Special attention was devoted to the clarity of items to allow for similar cognitive processing by the respondents. For example, concept- or linguistic-laden questions were avoided (e.g., to assess peer pressure, we asked about “smoking among close friends” rather than “peer pressure”). The questionnaire was piloted in 86 boys and 67 girls from four schools in Irbid and further modified to address issues revealed during the piloting.
Procedures and Definitions
The questionnaire was group-administered by one of the study personnel. In each classroom, a study staffer explained the purpose of the study to students, showed them how to answer the questionnaire, and answered their questions. To improve the validity of students’ responses, no teachers or other school personnel were allowed in the classroom during data collection.
The following definitions of smoking status were used: “Ever smoking” is ever smoking a cigarette/water pipe, even a puff or two. “Current smoking” is reported tobacco use (cigarette, water pipe) in the past 30 days. “Regular smoking” is smoking at least once a week in the past 30 days. “Never smoking” is reporting never having experimented with tobacco. The intention to smoke is assessed from responses to the question: “Do you think that you may start to smoke cigarettes [waterpipe] next year?” To obtain more stable estimations, “yes” and “maybe” responses are grouped together because of the small numbers in each category. The positive predictive value (PPV) of this question is calculated by dividing number who answered “yes/maybe” to this question and became ever-smokers after 2 years by the total number who answered “yes/maybe” on the question:
Parental consent and students’ assent were obtained from all participants. The study was reviewed and approved by the Jordan University for Science and Technology and the University of Memphis institutional review boards.
Statistical Analysis
Data were summarized as number and percent of total. Chi-square test was used to compare smoking prevalence in boys and girls and between water pipe and cigarettes. McNemar test was used to compare smoking status over time (between baseline and 2-year follow-up). Because the study used a complex sampling design, all analyses were weighted in order to provide more accurate estimates of variance. School weights were calculated by multiplying number of schools selected from each stratum with the probability of selecting a particular school and taking the inverse of the result. Weighted analyses were performed using “Complex Samples” procedure in SPSS, which takes into account both the stratification and the clustering of the sample when calculating the confidence intervals around the estimates. Statistical analysis was performed using SPSS v. 19.0 (SPSS Inc, Chicago, IL).
Results
Of the 1,781 students enrolled at baseline, 1,701 (95.5%) were still in the study and completed the 2-year follow-up survey (869 boys, median age at baseline 13 years). Prevalence of ever and current cigarette smoking was considerably higher in boys than girls both at baseline and follow up (p < .01 for all comparisons). The same findings were observed for water-pipe smoking although the differences between boys and girls were smaller than those of cigarette smoking for both ever and current WP smoking (p < .01 for all comparisons; Table 1).
Table 1.
Change in Prevalence of Indicators of Tobacco Smoking Between Seventh Grade (Baseline, Mean Age 13) and Ninth Grade in Northern Jordan, by Gender
| Smoking status | Boys, N = 869, n (%) | Girls, N = 832, n (%) | Total, N = 1,701, n (%) |
| Ever cigarettes smoking | |||
| Baselinea | 226 (26.0) | 73 (8.8) | 299 (17.6) |
| Two-year follow-upab | 453 (52.1) | 217 (26.1) | 760 (44.7) |
| Ever water-pipe smoking | |||
| Baselinea | 295 (33.9) | 145 (17.4) | 440 (25.9) |
| Two-year follow-upab | 491 (56.5) | 298 (35.8) | 789 (46.4) |
| Ever any smoking (cigarettes and/or water pipe) | |||
| Baselinea | 368 (42.3) | 166 (20.0) | 534 (31.4) |
| Two-year follow-upab | 588 (67.7) | 351 (42.2) | 939 (55.2) |
| Current cigarettes smoking | |||
| Baselinea | 75 (8.6) | 15 (1.8) | 90 (5.3) |
| Two-year follow-upab | 201 (23.1) | 53 (6.4) | 254 (14.9) |
| Current water-pipe smoking | |||
| Baselinea | 166 (19.1) | 61 (7.3) | 227 (13.3) |
| Two-year follow-upab | 213 (24.5) | 108 (13.0) | 321 (18.9) |
| Current any smoking (cigarettes and/or water pipe) | |||
| Baselinea | 192 (22.1) | 67 (8.1) | 259 (15.2) |
| Two-year follow-upab | 296 (34.1) | 130 (15.6) | 426 (25.0) |
Note. aDifference between boys and girls is statistically significant (p < .01 for all).
Difference from baseline is statistically significant (p < .01 for all).
Ever smoking any kind (cigarette and/or water pipe) was reported by 31.4% of students at baseline and increased to 55.2% 2 years later, while current smoking any kind was reported by 15.2% of students at baseline and increased to 25.0% 2 years later (Table 1).
Time Trends in Cigarette Smoking
Overall, ever cigarette smoking increased 2.5 times during the 2-year follow-up period (from 17.6% to 44.7%; p < .01), while current cigarette smoking almost tripled during the same period (from 5.3% to 14.9%; p < .01). When analyzed by gender, similar trends were observed in both sexes (Table 1).
For never smokers at baseline, among the 643 boys, 227 (35.3%) became ever smokers 2 years later—of which 95 (14.8%) were current and 40 (6.2%) were daily smokers. While among the 759 never-smoker girls, 143 (18.8%) became ever smokers 2 years later—of which 32 (4.2%) were current and 5 (0.7%) were daily smokers (Table 2).
Table 2.
Smoking Patterns at 2-Year Follow-up Among Never Smokers at Baseline, by Gender
| Cigarettea | Boys, N = 868b | Girls, N = 832 | Total, N = 1,700b |
| Never-smoker at baseline: n (%) | 643 (74.1) | 759 (91.2) | 1,402 (82.5) |
| At 2-year follow up | |||
| Never-smoker | 416 (64.7) | 616 (81.1) | 1,032 (73.6) |
| Ever-smoker | |||
| Did not smoke in the past month | 132 (20.5) | 111 (14.6) | 243 (17.3) |
| Current (but not daily) | 55 (8.6) | 27 (3.6) | 82 (5.8) |
| Daily | 40 (6.2) | 5 (0.7) | 45 (3.2) |
| Water pipea | Boys, N = 844b | Girls, N = 811b | Total, N = 1,655b |
| Never-smoker at baseline: n (%) | 564 (66.8) | 675 (83.2) | 1,239 (74.9) |
| At 2-year follow-up | |||
| Never-smoker | 378 (67.0) | 535 (79.2) | 913 (73.7) |
| Ever-smoker | |||
| Did not smoke in the past month | 101 (17.9) | 84 (12.4) | 185 (14.9) |
| Current (but not daily) | 73 (12.9) | 54 (8.0) | 127 (10.3) |
| Daily | 12 (2.1) | 2 (0.3) | 14 (1.1) |
Note. ap < .05 for all comparisons between boys and girls.
Numbers differ from Table 1 because of missing data on smoking frequency in Year 2.
Time Trends in Water-Pipe Smoking
The change over time for water-pipe smoking was less prominent than that of cigarette smoking. Prevalence of ever water-pipe smoking increased 1.8 times during the 2-year follow-up period (from 25.9% to 46.4%; p < .01), while current water-pipe smoking increased 1.4 times during the same period (from 13.3% to 18.9%; p < .01). Similar to finding from cigarette smoking, change of water-pipe smoking over time was essentially similar in boys and girls—both for ever and current water-pipe smoking (Table 1).
For never smokers at baseline, among the 564 boys, 196 (33.0%) became ever smokers 2 years later—of which 85 (15.1%) were current and 12 (2.1%) were daily smoker (Table 3). While among the 675 never-smoker girls at baseline, 140 (20.7%) became ever smokers 2 years later—of which 56 (8.3%) were current and 2 (0.3%) were daily smokers (Table 2).
Table 3.
Effect of Baseline Perceived Intention to Smoke Cigarette and Water Pipe in the Future Among Never-Smokers at Baseline
| Do you think that you may start to smoke cigarettes next year? | Boys, n (%) | Girls, n (%) | Total, n (%) |
| “No” | 586 (91.3) | 702 (92.6) | 1,288 (92.0) |
| Smoking status at 2-year follow up | |||
| Never-smokers | 388 (66.2) | 571 (81.3) | 959 (74.4) |
| Ever-smokers | 198 (37.8) | 131 (18.7) | 329 (25.5) |
| Did not smoke in the past month | 117 (20.0) | 104 (14.8) | 221 (17.2) |
| Current smoker | 81 (13.8) | 27 (3.8) | 108 (8.4) |
| “Yes/maybe” | 56 (8.7) | 56 (7.4) | 112 (8.0) |
| Smoking status at 2-year follow up | |||
| Never-smokers | 27 (48.2) | 45 (80.3) | 72 (64.3) |
| Ever-smokers | 29 (51.8) | 11 (19.7) | 40 (35.7) |
| Did not smoke in the past month | 15 (26.8) | 6 (10.7) | 21 (18.7) |
| Current smoker | 14 (25.0) | 5 (8.9) | 19 (17.0) |
| Do you think that you may start to smoke water pipe next year? | Boys, n (%) | Girls, n (%) | Total, n (%) |
| “No” | 502 (89.2) | 621 (92.1) | 1123 (90.8) |
| Smoking status at 2-year follow up | |||
| Never-smokers | 344 (68.5) | 490 (78.9) | 834 (74.3) |
| Ever-smokers | 158 (31.5) | 131 (21.1) | 289 (25.7) |
| Did not smoke in the past month | 87 (17.3) | 80 (12.9) | 167 (14.9) |
| Current smoker | 71 (14.1) | 51 (8.2) | 122 (10.8) |
| “Yes/maybe” | 61 (10.8) | 53 (7.9) | 114 (9.2) |
| Smoking status at 2-year follow up | |||
| Never-smokers | 33 (54.1) | 45 (84.9) | 78 (68.4) |
| Ever-smokers | 28 (45.9) | 8 (15.1) | 36 (31.6) |
| Did not smoke in the past month | 14 (22.9) | 4 (7.5) | 18 (15.8) |
| Current smoker | 14 (22.9) | 4 (7.5) | 18 (15.8) |
When comparing time trends of water-pipe smoking to those of cigarette smoking in this group, the higher prevalence of water-pipe smoking at baseline (25.9% vs. 17.6%; p < .01, and 13.3% vs. 5.3%; p < .01, for ever and current smoking, respectively) disappeared after 2 years for ever smoking (46.4% vs. 44.7%; p = .32) but remained significant for current smoking although the difference became smaller (18.9% vs. 14.9%; p < .01).
Intention to Smoke
The longitudinal study design provides an opportunity to test the predictive validity of adolescents’ perceptions of smoking initiation in the future. This was assessed by asking never smokers at baseline whether they may start smoking cigarette or water pipe (separately) in the future. A higher proportion of boys who answered “yes/maybe” to the question: “Do you think that you may start to smoke cigarettes next year?” became ever or current smokers after 2 years, as compared with those who answered “no” to the same question (51% vs. 37.8% for ever smokers and 25.0% vs. 13.8% for current smokers). The corresponding numbers for girls were 19.7% versus 18.7% and 8.9% versus 3.8% for ever and current smoking, respectively (Table 3). However, in both sexes, these comparisons did not reach statistical significance (p > .2 for all comparisons). PPV for this question was 51% for boys and 19.6% for girls.
For water pipe, the differences between those who answered “yes/maybe” and “no” to the same question were even smaller than those for cigarette smoking (p > .2 for all comparisons). PPV was 45.9% for boys and 9.6% for girls (Table 3).
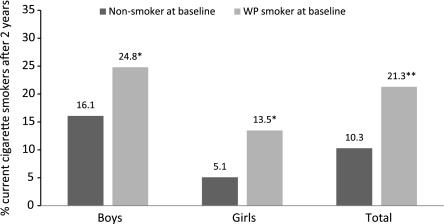
Gateway Hypothesis
This study allowed for the first time to examine the gateway hypothesis, which postulates that water pipe can provide a gateway for cigarette smoking in cigarette-naïve individuals. In this analysis, we compared current cigarette smoking at 2-year follow up between those who were nonsmokers (water pipe or cigarette) at baseline and those who were current water-pipe smokers at baseline. Results showed that water pipe–only smokers at baseline are twice as likely to become current cigarette smokers after two years as never-smokers at baseline [relative risk (RR) = 2.1; 95% CI = 1.2, 3.4, Figure 1]. The same observation held in boys (RR = 1.5; 95% CI = 1.0, 2.5) and girls (RR = 2.6; 95% CI = 1.2, 5.6; Figure 1). However, the reverse also was true; current cigarette smokes at baseline were twice as likely to become current water-pipe smokers after 2 years as never smokers at baseline (RR = 2.0; 95% CI = 0.9, 4.8), data not shown. No gender-specific analysis was performed because of the small number of current cigarette smokers at baseline.
Figure 1.
Progression to current cigarette smoking among water-pipe smokers versus nonsmokers at baseline. *p < .05, **p < 0.01.
Discussion
This is the first longitudinal study comparing cigarette and water-pipe smoking among young adolescents in a Middle Eastern setting. This study shows that smoking is widespread and quickly increasing among this young population. The overall observed pattern indicates a more extensive experimentation with and usage of water pipe at baseline, with quick catch up of cigarette smoking 2 years later. During the 2-year observation period, ever smoking doubled to reach half of study students, while current smoking increased by 66% to reach a quarter of them. Water-pipe smoking has become the No. 1 tobacco use method among the studied youths, especially among girls. About a third of boys and a fifth of girls had already tried water-pipe smoking by age 13 years. By age 15, about half of all studied youths had already tried a water pipe, and a fifth of them were current water-pipe smokers. Cigarette smoking was also an important health risk in this population, especially among boys where about a quarter were current smokers at age 15.
The spread of water-pipe smoking among youths in the EMR is a phenomenon that has been increasingly documented in the past decade. Data from GYTS, involving more than 90,000 13- to 15-year olds in the EMR, show that the prevalence of other-than-cigarette tobacco use (mostly water pipe in the EMR) is more than twice that of cigarettes (Warren, Jones, Eriksen, & Asma, 2006). Even outside the EMR, evidence is accumulating in support of the global spread of water-pipe smoking among youth (Maziak, 2011; Warren et al., 2009). Likewise, emerging evidence among college students in the United States suggests that water-pipe smoking, hardly seen a decade ago, is becoming the second-most common form of smoking among this population (Cobb, Ward, Maziak, Shihadeh, & Eissenberg, 2010; Primack et al., 2008). For example, in a survey conducted in 2008 among 3,770 of college students from 8 universities in North Carolina, ever water-pipe smoking was reported by 40% of students, while current water-pipe smoking was reported by 17% of the sample—compared with 25% who reported current cigarette smoking (Sutfin et al., 2011).
That water-pipe smoking is increasing rapidly among the youths, especially in the EMR, raises the question of how much of the observed increase in the prevalence of water-pipe smoking in this study was due to true within-individual change, and how much was due to the secular trend operating on the population level. Our data do not allow for answering this question accurately, as we did not measure water-pipe smoking among the seventh graders each year during the study period. It is difficult, therefore, to tease out the within-individual increase from the population trend. However, a rough estimate of the magnitude of the secular trend in the population can be derived from GYTS, which studied smoking trend in a similar, albeit a little older, population. Current “non-cigarette tobacco uses”—widely considered a proxy to water-pipe smoking in the EMR—increased by 6 percentage points from 2003 to 2007 in Jordan (from 20% to 26%). So, roughly speaking, and assuming a steady trend, it is estimated that 2–3 percentage points of the observed water-pipe smoking increase during the study period is maybe attributable to the population trend. This is equivalent to 30–50% of the observed increase in current water-pipe smoking in this study (Table 1). However, we think that the true effect of the population trend in our study, while still important, is smaller than that in GTYS because of the younger age of our population.
One of the salient epidemiological patterns of water-pipe smoking, at least in the EMR, concerns women’s susceptibility to water-pipe smoking. This is evidenced by the greater gender difference in cigarette smoking compared with water pipe in the EMR (Maziak, Ward, & Eissenberg, 2007). In this study, current water-pipe smoking among girls was four times higher at baseline—and two times higher at 2-year follow-up—than cigarette smoking. No such differences were observed in boys. This relatively higher prevalence of water-pipe use among girls may indicate a more social tolerance of water-pipe smoking than cigarette’s (Maziak et al., 2004). For example, in a study by Tamim et al. (2007) of 2,443 schoolchildren in Lebanon (average age 15), about one-quarter of cigarette smokers, compared with two-thirds of water-pipe smokers, said that one or both parents knew about their smoking. Given that water-pipe smoking is associated with considerable health effects and that it can lead to cigarette smoking, those trends may translate into increased smoking prevalence among women in the EMR with corresponding increase in smoking-related morbidity and mortality among them.
Compared with water pipe, this study showed that cigarette smoking uptake seems to have a later but more accelerated time dynamic. So, while current water-pipe smoking increased by about 42% within the 2-year observation period, cigarette smoking almost tripled. Part of this may be due to the higher prevalence of water-pipe smoking at baseline compared with cigarette smoking (as presented in Table 1). That is, those who are likely to become water-pipe smokers take up the habit at a younger age. It also can be due to the faster development of dependence among cigarette smokers compared with water pipe because of easy accessibility of cigarettes and their faster nicotine delivery. However, caution must be practiced when extrapolating from one method of tobacco use to another in terms of use patterns, dependence, or policy. For example, available evidence indicates a difference in the dependence experience between cigarette and water-pipe smokers, with more prominent social domain for water-pipe dependence (Maziak et al., 2005). However, universal application of smoke-free and minors’ access policies is expected not only to protect nonsmokers from exposure to harmful emissions associated with smoking but also to prevent some of young smokers from becoming water-pipe smokers and hooked on tobacco (Noonan, 2010).
Intention to smoke in the future among never-smoker boys predicted later onset of smoking, where boys who expressed intention to try smoking in the next year were approximately 1.5 times more likely to do so than those who did not. Similar patterns were observed for cigarette and water-pipe smoking, but the association did not reach statistical significance. No similar finding was observed among girls. Other studies investigating intention to smoke reported similar inconclusive findings (Skara, Sussman, & Dent, 2001; Stanton, Barnett, & Silva, 2005). However, this study is the first to investigate intention to smoke of water pipe.
This study provides a unique opportunity to examine the “gateway hypothesis” postulating that water-pipe smoking can predispose to cigarette smoking. Some anecdotal evidence points to this possibility (Asfar et al., 2008; Hammal, Mock, Ward, Eissenberg, & Maziak, 2008). A recent study among 762 Danish youth provides the first prospective evidence that water pipe use may predict progression to regular cigarette smoking (Jensen et al., 2010). However, all participants in that study were already experimenting with cigarettes at baseline, which makes it impossible to disentangle the effect of water-pipe smoking per se. This study allows examining whether cigarette-naïve water-pipe smokers are more likely to become cigarette smokers over time as compared with nonsmokers. As these data show, water-pipe smoking at baseline predicts cigarette smoking at 2-year follow-up. However, cigarette smoking at baseline also predicts future water-pipe smoking. Together, these findings simply indicate that these students are still experimenting with smoking at this stage, where any tobacco use leads to more tobacco use, rather than the notion that water pipe is a unique gateway for cigarette smoking. The observed effect of water-pipe smoking on future cigarette smoking, however, is still important given the considerably higher prevalence of water-pipe smoking at baseline and the ready accessibility of cigarettes. This makes the water pipe problematic not only in terms of exposing smokers and nonsmokers to associated harms but also by thwarting tobacco control efforts in general.
This study has some limitations. First, studying students only in one city limits the generalizability of the findings throughout the EMR, despite the close social and cultural similarities among nations in that region. Second, as is the case in most epidemiological survey studies, tobacco use was based on self-report; thus some degree of misclassification is likely, although self-reports of tobacco use by adolescents has been repeatedly shown to be reasonably accurate (Dolcini, Adler, Lee, & Bauman, 2003; Post et al., 2005). Finally, this study followed up students only until ninth grade, and some uptake is likely to occur after that, so these findings may not reflect the full extent of the problem.
Funding
National Institute on Drug Abuse (R01 DA024876) K.D.W. and W.M.
Declaration of Interests
None declared.
References
- Akl EA, Gaddam S, Gunukula SK, Honeine R, Jaoude PA, Irani J. The effects of waterpipe tobacco smoking on health outcomes: A systematic review. International Journal of Epidemiology. 2010;39:834–857. doi: 10.1093/ije/dyq002. doi: 10.1093/ije/dyq002. [DOI] [PubMed] [Google Scholar]
- Asfar T, Weg MV, Maziak W, Hammal F, Eissenberg T, Ward KD. Outcomes and adherence in Syria's first smoking cessation trial. American Journal of Health Behavior. 2008;32:146–156. doi: 10.5555/ajhb.2008.32.2.146. doi: 10.5555/ajhb.2008.32.2.146. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Cigarette smoking among adults—United States, 2006. Morbidity Mortality Weekly Report. 2007;56:1157–1161. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5644a2.htm. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Global Tobacco Surveillance System Data (GTSSData) 2008. Retrieved from: http://apps.nccd.cdc.gov/gtssdata/Ancillary/DataReports.aspx?CAID=1. [Google Scholar]
- Cobb C, Ward KD, Maziak W, Shihadeh AL, Eissenberg T. Waterpipe tobacco smoking: An emerging health crisis in the United States. American Journal of Health Behavior. 2010;34:275–285. doi: 10.5993/ajhb.34.3.3. doi: 10.5555/ajhb.2010.34.3.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolcini MM, Adler NE, Lee P, Bauman KE. An assessment of the validity of adolescent self-reported smoking using three biological indicators. Nicotine and Tobacco Research. 2003;5:473–483. doi: FEADEAKUJ1PQJ54A. [PubMed] [Google Scholar]
- Hammal F, Mock J, Ward KD, Eissenberg T, Maziak W. A pleasure among friends: How narghile (waterpipe) smoking differs from cigarette smoking in Syria. Tobacco Control. 2008;17 doi: 10.1136/tc.2007.020529. e3. doi: 10.1136/tc.2007.020529. [DOI] [PubMed] [Google Scholar]
- Jensen PD, Cortes R, Engholm G, Kremers S, Gislum M. Waterpipe use predicts progression to regular cigarette smoking among Danish youth. Substance Use and Misuse. 2010;45:1245–1261. doi: 10.3109/10826081003682909. doi: 10.3109/10826081003682909. [DOI] [PubMed] [Google Scholar]
- Maziak W. The global epidemic of waterpipe smoking. Addictive Behavior. 2011;36:1–5. doi: 10.1016/j.addbeh.2010.08.030. doi: 10.1016/j.addbeh.2010.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maziak W, Eissenberg T, Ward KD. Patterns of waterpipe use and dependence: Implications for intervention development. Pharmacology Biochemistry and Behavior. 2005;80:173–179. doi: 10.1016/j.pbb.2004.10.026. doi: 10.1016/j.pbb.2004.10.026. [DOI] [PubMed] [Google Scholar]
- Maziak W, Ward KD, Afifi Soweid RA, Eissenberg T. Tobacco smoking using a waterpipe: A re-emerging strain in a global epidemic. Tobacco Control. 2004;13:327–333. doi: 10.1136/tc.2004.008169. doi: 10.1136/tc.2004.008169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maziak W, Eissenberg T, Ward KD. Interventions for waterpipe smoking cessation. Cochrane Database of Systematic Reviews. 2007;4 doi: 10.1002/14651858.CD005549.pub2. CD005549. doi:10.1002/14651858.CD005549.pub2. [DOI] [PubMed] [Google Scholar]
- Mzayek F, Khader Y, Eissenberg T, Ward K, Maziak W. Design, baseline results of Irbid longitudinal, school-based smoking study. American Journal of Health Behavior. 2011;35:746–755. [PMC free article] [PubMed] [Google Scholar]
- Noonan D. Exemptions for hookah bars in clean indoor air legislation: A public health concern. Public Health Nursing. 2010;27:49–53. doi: 10.1111/j.1525-1446.2009.00826.x. doi: 10.1111/j.1525-1446.2009.00826.x. [DOI] [PubMed] [Google Scholar]
- Post A, Gilljam H, Rosendahl I, Meurling L, Bremberg S, Galanti MR. Validity of self reports in a cohort of Swedish adolescent smokers and smokeless tobacco (snus) users. Tobacco Control. 2005;14:114–117. doi: 10.1136/tc.2004.008789. doi: 10.1136/tc.2004.008789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Primack BA, Sidani J, Agarwal AA, Shadel WG, Donny EC, Eissenberg TE. Prevalence of and associations with waterpipe tobacco smoking among U.S. university students. Annals of Behavioral Medicine. 2008;36:81–86. doi: 10.1007/s12160-008-9047-6. doi: 10.1007/s12160-008-9047-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raad D, Gaddam S, Schunemann HJ, Irani J, Abou Jaoude P, Honeine R, et al. Effects of waterpipe tobacco smoking on lung function: A systematic review and meta-analysis. Chest. 2011;139:764–774. doi: 10.1378/chest.10-0991. doi: 10.1378/chest.10-0991. [DOI] [PubMed] [Google Scholar]
- Shafey O. Health issues in the Arab American community. Global epidemiology and health hazards of tobacco use: Arab world patterns. Ethnicity and Disease. 2007;17:S3–13–S13–S15. [PubMed] [Google Scholar]
- Shihadeh A. Investigation of mainstream smoke aerosol of the argileh water pipe. Food and Chemical Toxicology. 2003;41:143–152. doi: 10.1016/s0278-6915(02)00220-x. doi:10.1016/S0278-6915(2)00220.x. [DOI] [PubMed] [Google Scholar]
- Skara S, Sussman S, Dent CW. Predicting regular cigarette use among continuation high school students. American Journal of Health Behavior. 2001;25:147–156. doi: 10.5993/ajhb.25.2.7. [DOI] [PubMed] [Google Scholar]
- Stanton WR, Barnett AG, Silva PA. Adolescents’ intentions to smoke as a predictor of smoking. Preventive Medicine. 2005;40:221–226. doi: 10.1016/j.ypmed.2004.05.026. doi: 10.1016/j.ypmed.2004.05.026. [DOI] [PubMed] [Google Scholar]
- Sutfin EL, McCoy TP, Reboussin BA, Wagoner KG, Spangler J, Wolfson M. Prevalence and correlates of waterpipe tobacco smoking by college students in North Carolina. Drug and Alcohol Dependence. 2011;115:131–136. doi: 10.1016/j.drugalcdep.2011.01.018. doi: 10.1016/j.drugalcdep.2011.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamim H, Al-Sahab B, Akkary G, Ghanem M, Tamim N, El Roueiheb Z, et al. Cigarette and nargileh smoking practices among school students in Beirut, Lebanon. American Journal of Health Behavior. 2007;31:56–63. doi: 10.5555/ajhb.2007.31.1.56. doi: 10.5555/ajhb.2007.31.1.56. [DOI] [PubMed] [Google Scholar]
- Van der Wilk EA, Jansen J. Lifestyle-related risks: Are trends in Europe converging? Public Health. 2005;119:55–66. doi: 10.1016/j.puhe.2004.04.008. doi: 10.1016/j.puhe.2004.04.008. [DOI] [PubMed] [Google Scholar]
- Ward KD, Eissenberg T, Gray JN, Srinivas V, Wilson N, Maziak W. Characteristics of U.S. waterpipe users: A preliminary report. Nicotine and Tobacco Research. 2007;9:1339–1346. doi: 10.1080/14622200701705019. doi: 10.1080/14622200701705019. [DOI] [PubMed] [Google Scholar]
- Warren CW, Jones NR, Eriksen MP, Asma S. Patterns of global tobacco use in young people and implications for future chronic disease burden in adults. Lancet. 2006;367:749–753. doi: 10.1016/S0140-6736(06)68192-0. doi: 10.1016/S0140-6736(06)68192-0. [DOI] [PubMed] [Google Scholar]
- Warren CW, Lea V, Lee J, Jones NR, Asma S, McKenna M. Change in tobacco use among 13-15 year olds between 1999 and 2008: Findings from the Global Youth Tobacco Survey. Global Health Promotion. 2009;16(Suppl. 2):38–90. doi: 10.1177/1757975909342192. doi: 10.1177/1757975909342192. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Guidelines for controlling and monitoring the tobacco epidemic. Geneva, Switzerland: WHO; 1998. [Google Scholar]
- World Health Organization. The global burden of disease: 2004 update. 2008. Retrieved from http://www.who.int/healthinfo/global_burden_disease/2004_report_update/en/ [Google Scholar]
- World Health Organization. WHO report on the global tobacco epidemic, 2011: Warning about the dangers of tobacco. 2011. Retrieved from http://www.who.int/tobacco/global_report/2011/en/ [Google Scholar]