Summary
This study evaluated angiographic and clinical results in patients with a dural arteriovenous fistula (DAVF) who underwent percutaneous transvenous embolization.
Retrospective chart analysis and radiographic studies were performed in 23 patients (aged 11-70 yrs) with a DAVF treated with percutaneous transvenous embolization in the past five years. Lesions were located in the anterior cranial fossa, cerebellar tentorium, transverse-sigmoid sinus and cavernous sinus. All procedures were analyzed with regard to presentation, delivery, angiographical and clinical outcome.
Data for 23 patients (age range, 11-70 yrs, mean age 49.5yrs) with DAVFs (cavernous sinus[CS], n=17; transverse-sigmoid sinus, n=3; anterior cranial fossa, n=2; cerebellar tentorium, n=1) were retrospectively reviewed. The DAVFs were treated with coils or a combination with Onyx via different transvenous approaches, in 28 procedures. Cerebral angiography was performed to confirm the treatment.
The mean clinical follow-up period was 22.1 months.
Transvenous treatment of intracranial DAVFs can be safe and effective if various transvenous approaches are attempted. Percutaneous transvenous embolization with detachable platinum coils or a combination with Onyx is effective in the treatment of DAVFs.
Key words: arteriovenous fistula, cavernous sinus, dural arteriovenous malformation, transvenous embolization
Introduction
DAVFs represent 10 to 15% of intracranial arteriovenous malformations46,48,56. Their classification is determined on the basis of the arterial supply or the venous drainage pattern46,48,53,56. Carotid cavernous fistulae (CCFs) are classified as direct (Barrow Type A) fistulae, which are often posttraumatic high-flow shunts between the cavernous portion of the internal carotid artery (ICA) and the cavernous sinus (CS), or indirect dural fistulae (Barrow Type B-D). Multiple arterial feeders arise from the ICA (Barrow Type B), the external carotid artery (ECA) (Barrow Type C), or both (Barrow Type D), with numerous microfistulae within the sinus wall4. Recently published classifications of DAVFs (e.g., Cognard’s classification) are based on the pattern of drainage for estimation of bleeding risks8. Depending on the DAVFs location and the venous drainage, clinical presentations range from asymptomatic to symptomatic1,7,15,16,26,36,38, with pulse-synchronous bruit, headaches, neurological deficits, venous hypertensive encephalopathy with dementia, or intracranial hemorrhage resulting from venous hypertension.
The decision to treat is based on the venous drainage pattern, the natural history of the lesion, the severity of presenting symptoms, the patient’s general condition, angiographic features, the location of the DAVF, and the morbidity and mortality rates of the procedure being considered. The goals of treatment are the prevention of risks and the elimination of symptoms caused by the arteriovenous shunt. Because of the bleeding risk, intracranial DAVFs with retrograde cortical drainage often require an anatomic cure. They can be treated with different modalities, such as endovascular procedures with transvenous and transarterial1,11,17,19-25,33,35,37,42,43,49-57, surgery7,10,12,13,16,18,29,41,55,58, gamma knife surgery39,40,44,45,51, or combinations of the three15,30,31,33; in selected cases, the lesions can be treated conservatively22.
Transvenous embolization with coils has become the standard treatment for DAVFs27,47,48. Today, transarterial Onyx embolization has been used preoperatively or as additional therapy to prompt the cure rate. This study presents our experience of different transvenous embolization techniques for the treatment of intracranial DAVFs and transvenous administration of Onyx.
Patient and Methods
Between February 2003 and February 2008, 23 patients (nine females, 14 males) with DAVFs involving the anterior cranial fossa (ACF), cerebellar tentorium, transverse-sigmoid sinus (TSS) and cavernous sinus (CS) were treated by percutaneous transvenous embolization at Beijing Tiantan Hosptial. Symptoms, locations of DAVFs, and access routes of venous embolization in each case are presented in Tables 1 and 2.
Table 1.
Clinical features of patients with CDAVFs who underwent transvenous embolization with detachable coils and Onyx.
| Patient | Age(yr)/ | Loca- | Type* | Feeders | Drainage | Symptoms | Endovascular | Compli- | Outcome | Follow-up |
|---|---|---|---|---|---|---|---|---|---|---|
| No. | Sex | tion | technique | cations | period | |||||
|
| ||||||||||
| 1. | 17/M | R | Barrow D/ | Right ICA | Right SOV | Right proptosis | 1. TVE: right SOV; coils; | None | Cure | 62 mths |
| Cognard IIa | and ECA | success; complete | ||||||||
|
| ||||||||||
| 2. | 68/F | R | Barrow D/ | Right ICA | Both SOVs | Bilateral proptosis, | 1. TVE: right FV, coils; | None | Cure | 59 mths |
| Cognard IIa | and ECA | Pulsatile tinnitus | success; complete | |||||||
|
| ||||||||||
| 3. | 64/F | R | Barrow D/ | Right ICA | Right SOV | Right chemosis, | 1. TVE: right InfPS, coils; | None | Right CNVI palsy | 54 mths |
| Cognard IIa | and ECA | and InfPS | Right CNVI palsy, | success; complete | resovled | |||||
| Pulsatile tinnitus | within 6 mths | |||||||||
|
| ||||||||||
| 4. | 38/F | L | Barrow D/ | Right ICA | Right SOV | Right proptosis | 1. TVE: right InfPS; coils; | None | Cure | 50 mths |
| Cognard IIa | and ECA | success; complete | ||||||||
|
| ||||||||||
| 5. | 11/M | L | Barrow D/ | Both ICAs | Left SOV, | Left proptosis, | 1. TVE: left InfPS; coils; | None | ||
| Cognard IIa | and ECAs | SupPS, | Left CNVI palsy, | success; incomplete | ||||||
| and InfPS | Pulsatile tinnitus | 2. TVE: left InfPS; coils; | None | left CNVI palsy | 42 mths | |||||
| success; complete | resolved within 2 mo | |||||||||
|
| ||||||||||
| 6. | 39/M | L | Barrow D/ | Both ICAs | Left SOV | Right chemosis | 1. TVE: left InfPS; coils; | None | Cure | 41 mths |
| Cognard IIa | and left ECA | and InfPS | success; complete | |||||||
|
| ||||||||||
| 7. | 68/F | L | Barrow D/ | Right ICA, | Right SOV, | Bilateral chemosis, | 1. TVE: left InfPS, coils; | None | Left CNVI palsy | 30 mths |
| Cognard IIa | both ECAs | both InfPS | Left CNVI palsy | success; incomplete | and developed brain | |||||
| Pulsatile tinnitus | 2. TAE: right MMA, coils; | infarction at follow- | ||||||||
| success; complete | up | |||||||||
|
| ||||||||||
| 8 | 64/F | B | Barrow D/ | Both ICAs | Both SOV, | Bilateral blurred | 1. TVE: left InfPS; coils; | Left CNVI | Left CNVI palsy | 20 mths |
| Cognard III | and ECAs | SupPS, | vision | success; incomplete | palsy | resolved within 6 mths | ||||
| InfPS and | 2.TVE: left SupPS; | None | ||||||||
| right SphS | failed | |||||||||
|
| ||||||||||
| 9. | 44/F | R | Barrow D/ | Both ICAs | Right SOV, | Right proptosis, | 1. TVE: left InfPS, coils; | None | Left CNVI palsy | 12 mths |
| Cognard IIa | and ECAs | both InfPS | Right CNVI, | success; incomplete | resolved within 6 mths | |||||
| Pulsatile tinnitus | 2.TVE: left InfPS, coils; | None | ||||||||
| success; complete | ||||||||||
|
| ||||||||||
| 10. | 46/F | B | Barrow D/ | Both ICAs | Both SOV, | Bilateral chemosis, | 1. TVE: right InfPS, coils; | None | ||
| Cognard IIa | and ECAs | and InfPS | Pulsatile tinnitus | success; incomplete | ||||||
| 2. TVE: left InfPS, coils; | None | Cure | 12 mths | |||||||
| success; complete | ||||||||||
|
| ||||||||||
| 11. | 37/F | R | Barrow D/ | Right ICA | Right SOV, | Right chemosis, | 1. TVE: right InfPS, coils; | Local | Cure | 3 mths |
| Cognard III | and ECA | InfPS and | Pulsatile tinnitus | success; complete | alopecie on | |||||
| SphS | the right side | |||||||||
|
| ||||||||||
| 12 | 54/M | L | Barrow D/ | Both ICAs | Left InfPS | Left CNIII | 1. TVE: left InfPS; | TCR | Left CNIII palsy | 13 mths |
| Cognard IIa | palsy | Coils and Onyx; | resolved within 3 mths | |||||||
| success complete | ||||||||||
|
| ||||||||||
| 13. | 36/M | L | Barrow D/ | Right ICA | Right SOV | Right proptosis | 1. TAE: Incomplete; | None | Cure | 12 mths |
| Cognard IIa | and ECA | and chemosis | 2. TVE: right FV | |||||||
| Onyx; success;complete | ||||||||||
|
| ||||||||||
| 14. | 69/F | R | Barrow D/ | Both ICAs | Right SOV | Right CNIII | 1. TVE: right FV; | None | Right CNIII palsy | 9 mths |
| Cognard IIa | palsy | Coils and Onyx; success; | resoved within 3 mths | |||||||
| complete | ||||||||||
|
| ||||||||||
| 15. | 57/M | R | Barrow D/ | Both ICAs | Both InfPS | Right CNIII | 1. TVE: right InfPS; | TCR | Right CNIII palsy | 5 mths |
| Cognard IIa | and ECAs | palsy | Coils and Onyx; success; | resolved within 2 mths | ||||||
| complete | ||||||||||
|
| ||||||||||
| 16. | 54/M | L | Barrow D/ | Both ICAs | Left InfPS | Pulsatile tinnitus | 1. TVE: left InfPS; | None | Left CNVI palsy | 4 mths |
| Cognard IIa | and ECAs | Left CNVI | Coils and Onyx; | resolved | ||||||
| palsy | success complete | |||||||||
|
| ||||||||||
| 17. | 43/M | B | Barrow D/ | Both ICAs | Left SOV | Left proptosis, | 1. TVE: left InfPS, | None | ||
| Cognard IIa | and ECA | and both InfPS | Chemosis and | coils and Onyx, Incomplet | ||||||
| Pulsatile tinnitus | 2.TVE: right InfPS, | Right CNVI | Right CNVI palsy | 2 mths | ||||||
| Coils and Onyx; | palsy | resolved | ||||||||
| success complete | ||||||||||
|
| ||||||||||
| *.Barrow type and Cognard classification. R, right; L, left; F, female; M, male; SOV, superior ophthalmic vein; mo, months; InfPS, inferior petrosal sinus; FV, facial vein; | ||||||||||
| SupPS, superior petrosal sinus; ICA:internal carotid artery; ECA:external carotid artery; CNIII, the third cranial nerve; CNVI, the sixth cranial nerve; TCR, trigeminocardiac reflex; | ||||||||||
| TAE, transarterial embolization; TVE, transvenous embolization. 2, two sessions. | ||||||||||
Table 2.
Clinical features of patients with DAVFs in other locations who underwent transvenous embolization with detachable coils.
| Patient | Age(yr)/ | Loca- | Type* | Feeders | Drainage | Symptoms | Endovascular | Compli- | Outcome | Follow-up |
|---|---|---|---|---|---|---|---|---|---|---|
| No. | Sex | tion | technique | cations | period | |||||
|
| ||||||||||
| 18. | 65/M | ACF | Cognard III | Left EA | FPV | Dementia | 1. TAE: left OA, | None | ||
| and ECA | seizure | Onyx-18, | ||||||||
| success, incomplete | ||||||||||
| 2.TVE: SSS; | None | Cure | 9 mths | |||||||
| coils; | ||||||||||
| success; complete | ||||||||||
|
| ||||||||||
| 19 | 48/M | ACF | Cognard III | Both EAs | Both FPVs | Headaches, right? | 1. TVE:SSS, | None | Cure | 3 mths |
| and ECAs | visual disturbance | coils; | ||||||||
| success; complete | ||||||||||
|
| ||||||||||
| 20. | 70/M | Tentoium(R) | Cognard IV | Right ICA | Right BVR | SAH | 1. TAE: right MMA | |||
| and ECA | coils, | |||||||||
| success, incomplete | ||||||||||
| 2. TVE: right BVR, | None | Cure | 4 mths | |||||||
| coils; | ||||||||||
| success; complete | ||||||||||
|
| ||||||||||
| 21. | 50/M | TSS(L) | Cognard IIa | Left ICA, | Right TSS | Headaches | 1. TVE:left TSS; | None | Cure | 36 mths |
| ECA and VA | coils; | |||||||||
| success; complete | ||||||||||
|
| ||||||||||
| 22. | 40/M | TSS(R) | Cognard IIa+b | Right ICA, ECA | Left TSS, | Headaches, | 1. TAE: right ECA; | None | ||
| and both VAs | right Labbe | Pulsatile tinnitus, | coils; success; | |||||||
| vein | incomplete | |||||||||
| 2. TVE: left TSS | None | Cure | 24 mths | |||||||
| coils, success, complete | ||||||||||
|
| ||||||||||
| 23. | 56/M | TSS(L) | Cognard IIa | Left ICA | Right TSS | Pulsatile tinnitus | 1. TAEl:left ECA; | |||
| Both ECAs | coils; success; incomplete | |||||||||
| and VAs | 2. TVE: right TSS | Pulsatile | ||||||||
| coils; success; incomplete | None | tinnitus | 2 mths | |||||||
|
| ||||||||||
| *.Cognard classification. | ||||||||||
| R, right; L, left; M, male;AFC, anterior cranial fossa; EA, ethmoidal artery; FPV, frontal polar vein; OA, ophthalmal artery; ICA:internal carotid artery; ECA:external carotid artery; | ||||||||||
| SSS, superior sagittal sinus; BVR, basal vein of Rosenthal; TSS, transverse-sigmoid sinus; mo, moths; TAE, transarterial embolization; TVE, transvenous embolization. | ||||||||||
Bilateral selective ICA and ECA angiography and vertebral artery angiography were performed for all patients, for assessment of the feeding arteries, fistula sites and venous drainage. The arteriovenous shunts were approached via the venous route. We first placed 6-French sheaths in the femoral artery and vein. A 5-French catheter in the carotid artery allowed observation of the shunt, acquisition of roadmaps, and angiographic monitoring of the procedure. A second 5-French catheter was placed in the jugular vein. A microcatheter (Marathon/Echelon, MTI-EV3, Irvine, CA, USA) was navigated coaxially via different venous approaches. The microguidewire (Mirage/Silverspeed 10, MTI-EV3, Irvine, CA, USA; Transend 0.014, Boston Scientific, USA) was then carefully introduced and advanced to the fistula portion, followed by the microcatheter. Subsequently, the draining vein or sinus was packed using detachable platinum coils or a combination with Onyx, using real-time digital subtraction fluoroscopic mapping.
Seventeen patients (nine female and eight male patients; age range, 11-69 yrs, mean age 47.6 yrs) presented with spontaneous DAVFs of the CS of Barrow Types D. Symptoms included chemosis and proptosis (n=12), pulsatile tinnitus (n=9), VI cranial palsy (n=5), III cranial nerve palsy (n=3), blurred vision (n=1). According to the classification described by Cognard et Al21, the 17 CDAVFs were Type II (n=14) and Type III (n=3). Nine patients underwent angiographic follow-up (range three to eight months; mean 6.3 months). The rationale for not requiring angiographic follow-up was clinical cure (without any symptoms). Clinical follow-up status was supplemented by telephone interviews and follow-up periods ranged from two to 62 months (mean 25.3 months).
Six male patients (age range 40-70 yrs; mean age 54.8 yrs) demonstrated DAVFs located in TSS (n=3), ACF (n=2) and cerebellar tentorium (n=1). Symptoms included headaches (n=3), pulsatile tinnitus (n=2), seizure (n=1), visual disturbances (n=1), dementia (n=1), and SAH (n=1). According to the classification described by Cognard et Al21, the DAVFs were of Type IIa (n=2), Type IIa+b (n=1), Type III (n=2) and Type IV (n=1). The fistulae were spontaneous. Clinical follow-up periods for this group ranged from two to 36 months (mean, 13 months).
Results
Twenty-three patients with DAVFs were reviewed in this series. Twenty-one DAVFs were completely embolized with detachable platinum coils or a combination with Onyx. The clinical data, and the angiographic results are summarized in Tables 1 and 2.
Transvenous embolization of the CS.
Twenty-two transvenous and two transarterial approaches were performed for the group of 17 DAVFs of the CS. Sixteen patients with DAVFs were initially treated with a transvenous route while one patient was treated with a transarterial route first. If the drainage was to the ipsilateral CS and/or predominantly posteriorly, then we first approached via the internal jugular vein (IJV)-inferior petrosal sinus (InfPS)-CS (n=13). If the InfPS could be passed (n=13), then the success rate was high, with complete occlusion in 16 cases. The more invasive direct SOV approach was chosen only if alternative endovascular transvenous routes had failed (one out of 17 cases) to yield complete occlusion of the fistula. The transvenous approach via the facial vein (FV) was possible in two cases with complete occlusion of the fistula. An alternative approach via the superior petrosal sinus was performed in one case but failed.
Follow-up outcome
Sixteen of the 17 DAVFs (94.1%) of the CS were cured anatomically and clinically. One patient (5.9%) with initial left VIth cranial nerve palsy did not completely resolve and developed brain infarction at 30-month follow-up. We encountered complications in five cases (29.4%): one patient developed local alopecia on the right side due to X-ray radiation, two patients developed reflexive bradyarrythmia and two patients demonstrated CNVI palsy after transvenous treatment. Angiographic follow-up (4-7 months; mean five months) was obtained in six patients. There was one recanalization in one patient; additional coil embolization was performed in five patients with residual fistulae. Residual aneurysm resolved in four patients with one failure.
Illustrative cases
Patient 9
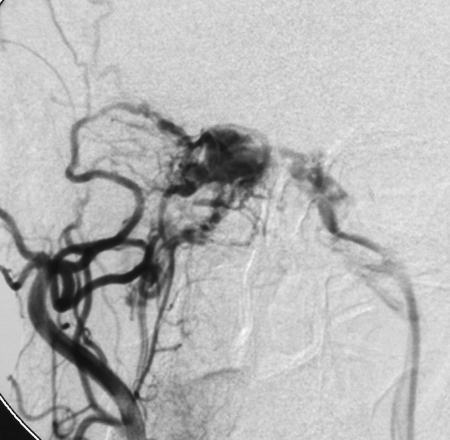
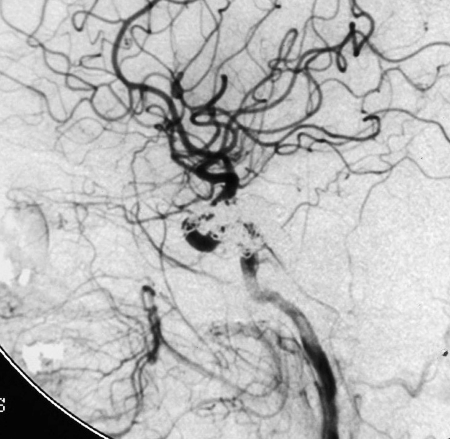
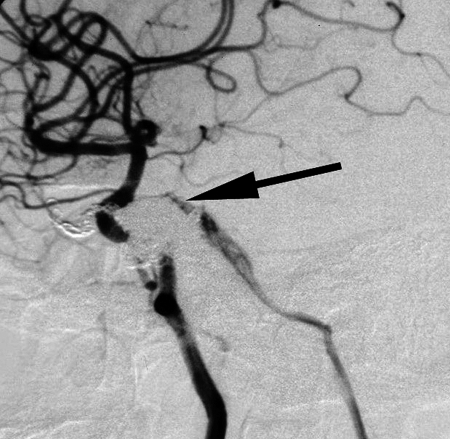
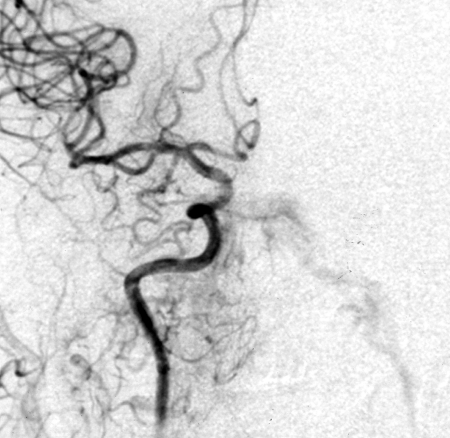
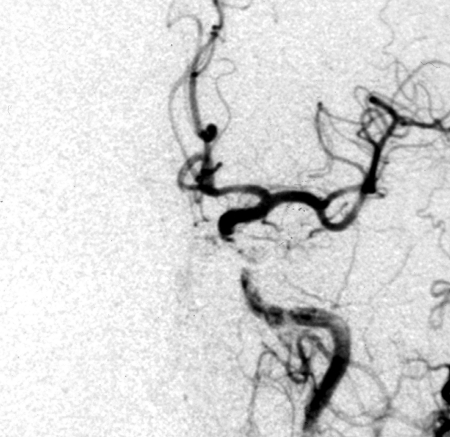
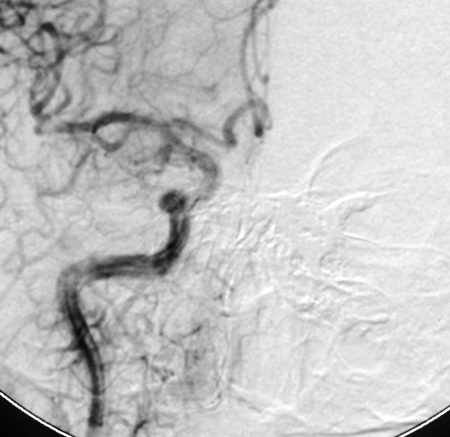
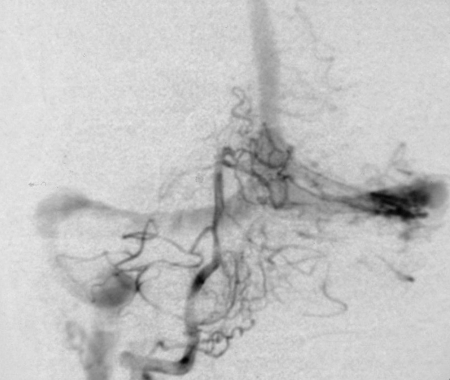
A 44-year-old woman demonstrated right proptosis and IVth cranial nerve palsy and excessive pulsatile bruits. Cerebral angiography revealed a DAVF of the right CS. Angiography of the right CCA demonstrated persistent filling of the left InfPS (Figure 1A). Therefore, a transvenous approach was chosen. The microcatheter was navigated through the left InfPS and the intercavernous sinus to the right CS (Figure 1C). The right CS was occluded with 28 standard coils (Figure 1D,E). However, the pulsatile tinnitus was still persistent at six-month follow-up study. Control angiography demonstrated recurrence of the fistula (Figure 1F) and the same procedure was performed (Figure 1G). The residual fistula was occluded completely by another six standard coils (Figure 1H).
Figure 1.
Patient 9, a 44-year-old woman demonstrated a cavernous DAVF of Barrow Type D/Cognard Type IIa. Right CCA angiogram, anteroposterior projection (A), left CCA angiogram, lateral projection (B) showing a CDAVF fed by both internal and external carotid arteries, mainly drained to the left InfPS and the right SOV. Frontal superselective angiogram of the right CS (C) showing the microcatheter positioned close to the fistula site. After embolization, anterograms of the right common carotid artery (lateral view, D) and left common carotid artery (lateral view, E) demonstrating complete occlusion of the fistula. F) Six months later, lateral angiogram of the right ICA showing persistent filling of the residual fistula (arrow). G) Occlusion of the intercavernous sinus (arrow) with several standard coils. H) Arteriogram of the right ICA (lateral view) after complete embolization of the right-side fistula.
A.
B.
C.
D.
E.
F.
G.
H.
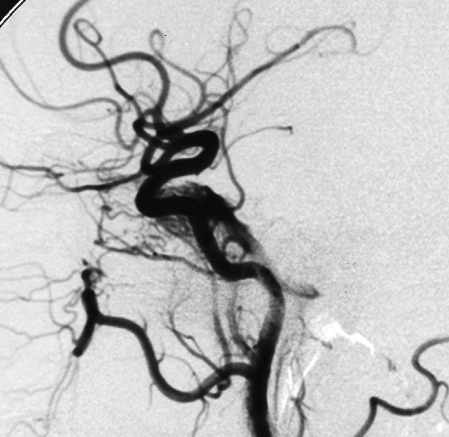
Patient 12
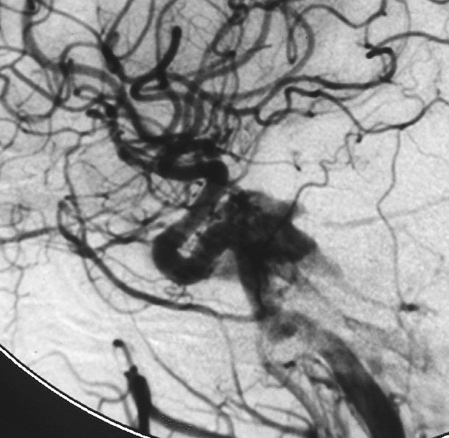
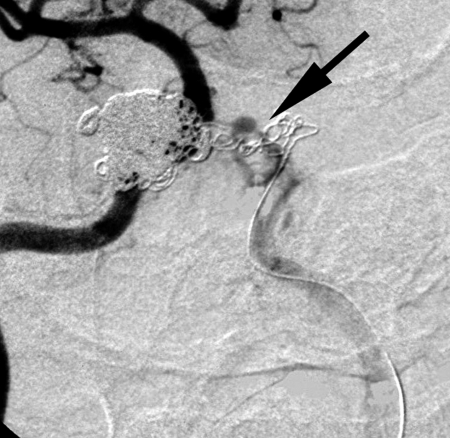
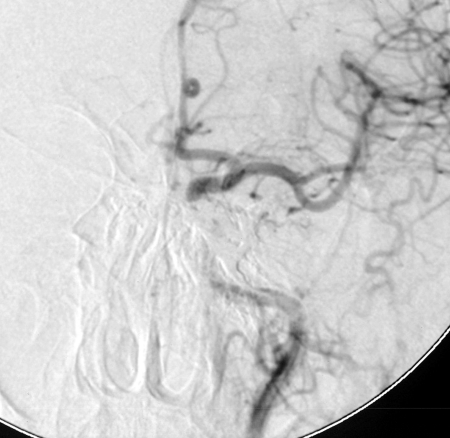
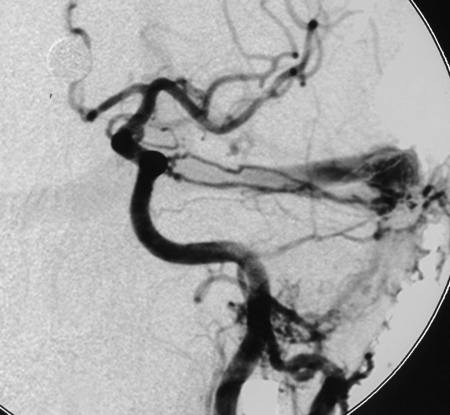
A 54-year-old man presented with blepharotosis, diplopia and chemosis. Cerebral angiograms showed a cavernous DAVF (Figure 2A,B). Recommendation was made for transvenous embolization of this lesion. Onyx injection was performed after three standard coils (two 5x12, one 6x15) were introduced until control angiogram revealed complete occlusion of the DAVF. The patient’s symptoms resolved within three months, there was no recanalization on seven-month follow-up angiograms (Figure 2 G,H).
Figure 2.
Patient 12, a 54-year-old man with a Barrow Type D/Cognard Type IIa DAVF. Right common carotid artery (CCA) angiogram, anteroposterior projection (A), left CCA angiogram, anteroposterior projection (B) showing a DAVF fed by both internal carotid arteries, mainly drained to the left inferior petrosal sinus and the left superior ophthalmic vein. Superselective angiogram (C) showing the tip of microcatheter in the left cavernous sinus. Right CCA angiogram, anteroposterior projection (D) and left CCA angiogram, anteroposterior projedtion (E) after embolization showing the DAVF is completely occluded. Skull X-ray film (F) after embolization, anteroposterior projection, showing the left CS and paracavernous sinuses were completely occluded (arrows). Seven months later, control angiograms of the right CCA (anteroposterior view, G) and left CCA (H), demonstrating no recanalization of the fistula points.
A.
B.
C.
D.
E.
F.
G.
H.
Transvenous embolization in other locations
For the group of DAVFs in other locations, clinical symptoms included headaches (n=3), pulsatile tinnitus (n=2), seizure (n=1), visual disturbances (n=1), dementia (n=1), and SAH (n=1).
Five DAVFs experienced cures, and one patient (1/6) experienced improvement. We performed six transvenous approaches usually via the IJV-saggital sinus (SS), IJV-TSS and leptomeningeal routes. The technical success rate was 100% (six out of six cases), with complete occlusion in 83.33% of cases (five out of six cases). The rate of incomplete occlusion was 16.67% (one out of six cases). For four patients, we performed the transarterial approach prior to transarterial embolization.
Follow-up outcome
Angiographic follow-up was obtained in two patients with cure. For one patient, patency of residual DAVF after endovascular treatment of a TSS DAVF on the left side and tinnitus was stable, another five patients were cured at clinical follow-up.
Illustrative cases
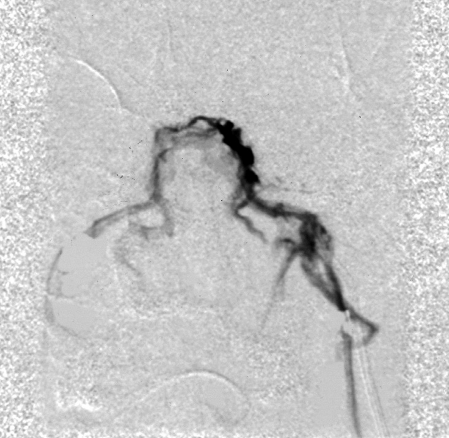
Patient 23
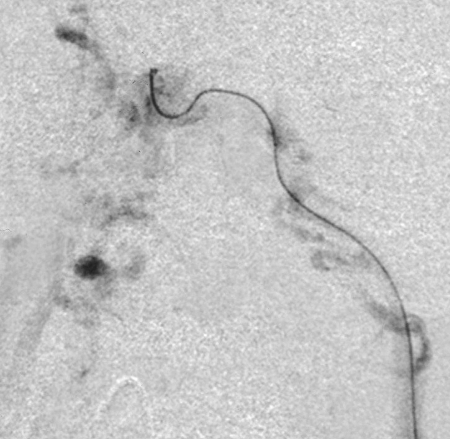
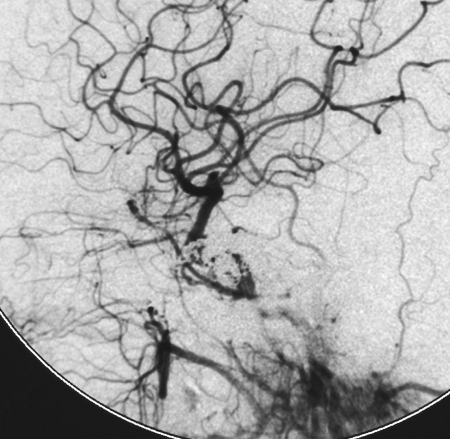
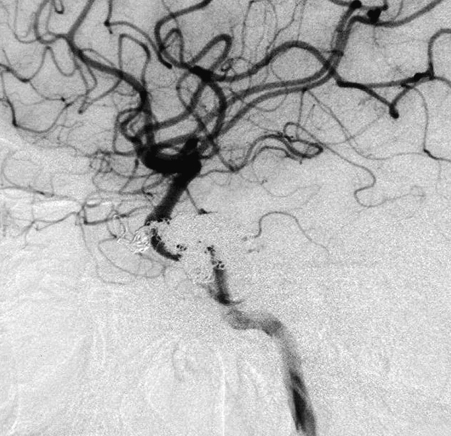
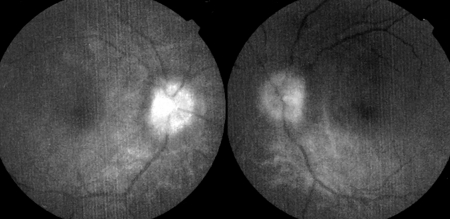
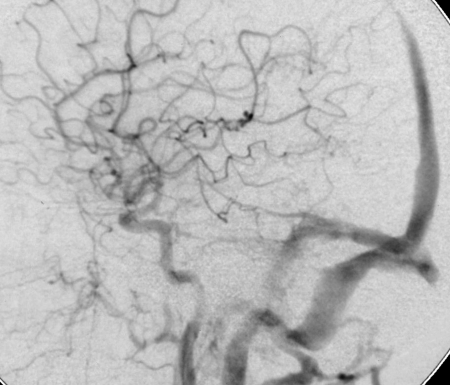
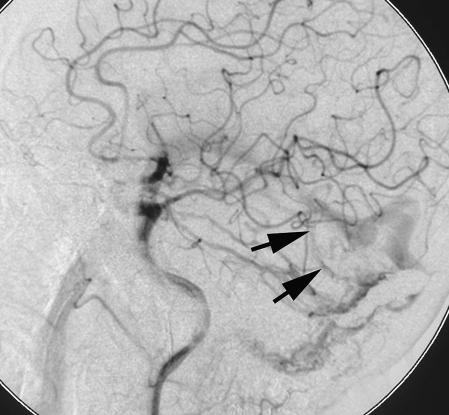
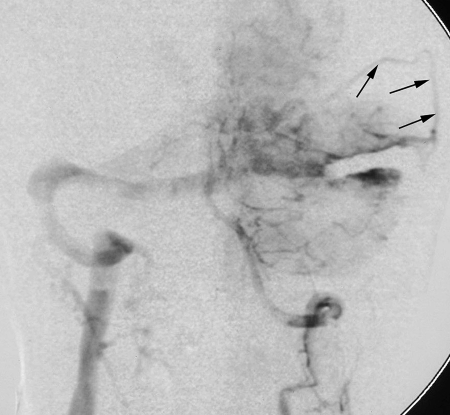
A 56-year-old man with headaches and pulsatile tinnitus demonstrated a left TSS Cognard Type IIa DAVF (Figure 3). An ophthalmological examination revealed bilateral papilledema (Figure 3A). Cerebral angiography demonstrated multiple feeders arising from the left ECA and ICA (Figure 3B) and basal artery system (Figure 3C) with a parallel venous channel. One transarterial and one transvenous embolization of the TSS DAVF were performed. These procedures and occlusion of the ECA feeders significantly reduced the size of the fistula (Figure 3E,F). After transvenous embolization of the left TSS, control angiography demonstrated obliteration of the parallel channel, with preservation of the patent parent sinus (Cognard Type I). During the subsequent months the patient?s tinnitus was in stable condition and no further neurological symptoms were noted, ophthalmological examination was not available.
Figure 3.
Patient 23, a 56-year-old man with a left Cognard Type IIa DAVF, with SSS reflux. A) An ophthalmological examination revealed bilateral papilledema. B) Arteriogram of the left CCA (arterial phase, lateral view), showing multiple feeders arising from the ICA and ECA. C) Arteriogram of the right VA (arterial phase, frontal view), showing multiple feeders arising from the VA. D) The microcatheter was navigated into the left TSS via the right IJV-TSS. E,F) Arteriograms (lateral view) of the left common carotid artery (E) and left VA. The residual fistula was Cognard Type I with parallel venous channel was coiled and the parent sinus was patent, with preservation of the venous outflow (arrows) of the temporal lobe through the vein of Labbe.
A.
B.
C.
D.
E.
F.
Discussion
Depending on their venous drainage patterns, intracranial DAVFs can cause headaches, dementia, chemosis, protosis, bruit, and, rarely, infarction or hemorrhage. The data of our patients confirmed previous studies7,12,27,38,40,50,56. The clinical presentation is closely related to the degree of shunting, cerebral venous hypertension, and the pattern of venous drainage, with or without impaired cortical function46. Despite spontaneous remission, which occurs in 9.4 to 50% of cases22, treatment is indicated in cases with cortical drainage (Cognard Type IIb or greater), hemorrhage, progressive neurological deficits, or intractable headaches or tinnitus. Although the cure rate of DAVFs by transarterial embolization has been promoted by Onyx, it is limited in smaller arteriovenous fistula DAVFs53. Transvenous embolization is still a good option for DAVFs with multiple feeding arteries, especially as they cannot be cured by transarterial embolization19-21. Our 23 patients represent 32.76% (the remaining patients were treated with transarterial embolization or neurosurgery) of the patients who underwent embolization for treatment of DAVFs at our institution in the past ten years. This reflects the evolution of transvenous approaches at a single institution in a period of five years. In our series, the anatomic cure rates were 94.1% (16/17) for DAVFs of the CS and 83.3% (1/6) for DAVFs at other locations. All patients, including those without anatomic cures, experienced improvement.
When catheterization is possible, transvenous embolization is associated with a high rate of permanent long-term occlusion. Occlusion can be achieved with placement of coils via a transvenous route.
Transvenous embolization of CS
There are different transvenous routes to the CS, i.e., by way of the InfPS, contralateral InfPS, basilar plexus or circular sinus, through the FV, angular vein, and SOV, or through the pterygoid plexus2-6,9,14,19,25,27,35,36,42,43,47,52. To achieve complete occlusion, the cavernous sinus was tightly packed with GDC. This tight packing may have accounted for the intense nausea and vomiting. Transient VIth or IIIrd nerve palsy following coil embolization for cavernous DAVF are well known events2. The complex nature of the fistula, the unexpected difficulty in the placement of detachable coils, and our previous experience with Onyx in the treatment of DAVFs promoted us to use Onyx in the treatment of our patien19,20,38.
Transvenous embolization of DAVFs in other locations
For DAVFs in the ACF, we prefer the transvenous procedure with the softest EDC and free coils to fit the draining frontal veins and to minimize the risk of damage and rupture of the frontal veins, appreciating the risk of visual compromise from embolic occlusion of the central retinal artery. Although the venous approach through the elongated, ectactic and potentially fragile pial veins is considered difficult and risky, several cases of tentorial DAVF have been treated by transvenous embolization9,21,23.
If the affected TSS is isolated or exhibits prominent retrograde drainage to the cortical veins and is not a functional part of the venous circulation, then sinus occlusion can be performed via an endovascular procedure. There was anterograde flow in the vein of Labbe in one case of a lateral sinus fistula, after transvenous embolization of the TSS with sparing of the vein of Labbe.
Kubo et Al30 concluded, on the basis of their three cases and a review of the literature, that second fistulae can occur after complete embolization, with latency periods of more than one year and this finding was confirmed by Kiyosue et Al26. For this reason, we occluded all main feeding arteries prior to obliteration of the affected sinus in our cases with DAVFs of the tentorium and TSS to prevent development of cortical venous reflux and intracranial hemorrhage. In one patient with a TSS DAVF with a parallel venous channel of the transverse/sigmoid sinus converted a Cognard Type IIa DAVF into a Cognard Type I DAVF with a patent parent sinus.
Conclusions
Transvenous treatment of intracranial DAVFs can be a highly effective method if various transvenous approaches are attempted. Onyx is a promising embolic agent for the transvenous treatment of DAVFs, and its physical properties warrant further appraisal in larger series of patients. The advantages make this an attractive alternative to various platinum coils already described.
References
- 1.Abrahams JM, Begley LJ, et al. Alternative management considerations for ethmoidal dural arteriovenous fistula. Surgical Neurology. 2002;58(6):410–417. doi: 10.1016/s0090-3019(02)00871-6. [DOI] [PubMed] [Google Scholar]
- 2.Aihara N, Mase M, et al. Deterioration of ocular motor dysfunction after transvenous embolization of dural arteriovenous fistula involving the cavernous sinus. Acta Neurochir. 1999;141:707–710. doi: 10.1007/s007010050365. [DOI] [PubMed] [Google Scholar]
- 3.Arat A, Cekirge S, et al. Transvenous injection of Onyx for casting of the cavernous sinus for the treatment of a carotid-cavernous fistula. Neuroradiology. 2004;46:1012–1015. doi: 10.1007/s00234-004-1244-9. [DOI] [PubMed] [Google Scholar]
- 4.Barrow DL, Sector RH, et al. Classification and treatment of spontaneous carotid cavernous fistula. J Neurosurg. 1985;62:248–256. doi: 10.3171/jns.1985.62.2.0248. [DOI] [PubMed] [Google Scholar]
- 5.Benndorf G, Bender A, et al. Treatment of a cavernous sinus dural arteriovenous fistula by deep orbital puncture of the superior ophthalmic vein. Neuroradiology. 2001;43:499–502. doi: 10.1007/s002340000508. [DOI] [PubMed] [Google Scholar]
- 6.Benndorf G, Bender A, et al. Transvenous occlusion of dural cavernous sinus fistulas through the thrombosed inferior petrosal sinus: report of four cases and review of the literature. Surg Neurol. 2000;54:42–54. doi: 10.1016/s0090-3019(00)00260-3. [DOI] [PubMed] [Google Scholar]
- 7.Benndorf G, Schmidt S, et al. Tentorial dural arteriovenous fistula presenting with various visual symptoms related to anterior and posterior visual pathway dysfunction: case report. . Neurosurgery. 2003;53:222–227. doi: 10.1227/01.neu.0000068873.63576.5e. [DOI] [PubMed] [Google Scholar]
- 8.Cognard C, Gobin YP, et al. Cerebral dural arteriovenous fistulas: clinical and angiographic correlation with a revised classification of venous drainage. Radiology. 1995;194:671–680. doi: 10.1148/radiology.194.3.7862961. [DOI] [PubMed] [Google Scholar]
- 9.Deasy NP, Gholkar AR, et al. Tentorial dural arteriovenous fistulas: endovascular treatment with transvenous coil embolization. Neuroradiology. 1999;41:308–312. doi: 10.1007/s002340050754. [DOI] [PubMed] [Google Scholar]
- 10.Deshmukh VR, Chang S, et al. Bilateral ethmoidal dural arteriovenous fistulas: a previously unreported entity: case report. Neurosurgery. 2005;57(4):E809. doi: 10.1093/neurosurgery/57.4.e809. [DOI] [PubMed] [Google Scholar]
- 11.Defreyne L, Vanlangenhove P, et al. Transvenous embolization of a dural arteriovenous fistula of the anterior cranial fossa: preliminary results. Am J Neuroradiol. 2000;21:761–765. [PMC free article] [PubMed] [Google Scholar]
- 12.Deshmukh VR, Maughan PH, Spetzler RF. Resolution of hemifacial spasm after surgical obliteration of a tentorial arteriovenous fistula: case report. Neurosurgery. 2006;58(1):E202. doi: 10.1227/01.neu.0000192386.89105.82. [DOI] [PubMed] [Google Scholar]
- 13.Fujita A, Tamaki N, et al. A tentorial dural arteriovenous fistula successfully treated with interruption of leptomeningeal venous drainage using microvascular Doppler sonography: case report. Surg Neurol. 2001;56:56–61. doi: 10.1016/s0090-3019(01)00492-x. [DOI] [PubMed] [Google Scholar]
- 14.Goldberg RA, Goldey SH, et al. Management of cavernous sinus-dural fistulas. Indications and techniques for primary embolization via the superior ophthalmic vein. Arch Ophthamol . 1997;115(6):823–824. doi: 10.1001/archopht.1996.01100130699011. [DOI] [PubMed] [Google Scholar]
- 15.Halbach VV, Higashida RT, et al. Dural arteriovenous fistulas supplied by ethmoidal arteries. Neurosurgery. 1990;26:816–823. doi: 10.1097/00006123-199005000-00014. [DOI] [PubMed] [Google Scholar]
- 16.Iwamuro Y, Nakahara I, et al. Tentorial dural arteriovenous fistula presenting symptoms due to mass effect on the dilated draining vein: case report. Surg Neurol. 2006;65:511–515. doi: 10.1016/j.surneu.2005.07.076. [DOI] [PubMed] [Google Scholar]
- 17.Jahan R, Gobin YP, et al. Transvenous embolization of a dural arteriovenous fistula of the cavernous sinus through the contralateral pterygoid plexus. Neuroradiology. 1998;40:189–193. doi: 10.1007/s002340050566. [DOI] [PubMed] [Google Scholar]
- 18.Jesus OD, Rosado JE. Tentorial dural arteriovenous fistula obliteration using the petrosal approach. Surg Neurol. 1999;51:164–167. doi: 10.1016/s0090-3019(97)00414-x. [DOI] [PubMed] [Google Scholar]
- 19.Jiang C, Lv X, et al. Transvenous Embolization of Cavernous Sinus Dural Arteriovenous Fistula with Onyx-18 and Plentinum coils: Technical Note. NRJ-Neuroradiol J. 2007;20(3):47–52. doi: 10.1177/197140090702000317. [DOI] [PubMed] [Google Scholar]
- 20.Jiang C, Lv X, et al. Transvenous embolization with Onyx for dural arteriovenous fistula of cavernous sinus: a report of two case reports. NRJ-Neuroradiol J. 2007;20(6):718–725. doi: 10.1177/197140090702000617. [DOI] [PubMed] [Google Scholar]
- 21.Jiang C, Lv X, et al. Transarterial and transvenous embolization for tentorial dural arteriovenous fistula: case report. . NRJ-Neuroradiol J. 2007;20(6):726–729. doi: 10.1177/197140090702000618. [DOI] [PubMed] [Google Scholar]
- 22.Kai Y, Hamada J, et al. Treatment of cavernous sinus dural arteriovenous fistulas by external manual carotid compression. . Neurosurgery. 2007;60:253–258. doi: 10.1227/01.NEU.0000249274.49192.3B. [DOI] [PubMed] [Google Scholar]
- 23.Kajita Y, Miyachi S, et al. A dural arteriovenous fistula of the tentorium successfully treated by intravascular embolization. Surg Neurol. 1999;52:294–298. doi: 10.1016/s0090-3019(99)00076-2. [DOI] [PubMed] [Google Scholar]
- 24.Kallmes DF, Jensen ME, et al. Percutaneous transvenous coil embolization of a Djindjian type 4 tentorial dural arteriovenous malformation. . Am J Neuroradiol. 1997;18:673–676. [PMC free article] [PubMed] [Google Scholar]
- 25.Kazekawa K, Iko M, et al. Dural AVFs of the cavernous sinus: transvenous embolization using a direct superficial temporal vein approach. Radiation Medicine. 2003;21(3):138–141. [PubMed] [Google Scholar]
- 26.Kim MS, Han DH, et al. Posterior fossa hemorrhage caused by dural arteriovenous fistula: case reports. Surg Neurol. 2003;59:512–517. doi: 10.1016/s0090-3019(03)00077-6. [DOI] [PubMed] [Google Scholar]
- 27.Kim DJ, Kim DI, et al. Results of transvenous embolization of cavernous dural arteriovenous fistula: A single-center experience with emphasis on complications and management. Am J Neuroradiol. 2006;27(10):2078–2082. [PMC free article] [PubMed] [Google Scholar]
- 28.Kiyousue H, Tanoue S, et al. Recurrence of dural arteriovenous fistula in another location after selective transvenous coil embolization: Report of two cases. Am J Neuroradiol. 2002;23:689–692. [PMC free article] [PubMed] [Google Scholar]
- 29.Komotar RJ. Clinicoradiological review: bilateral ethmoidal artery dural arteriovenous fistulas. Neurosurgery. 2007;60(1):131–136. doi: 10.1227/01.NEU.0000249196.53656.53. [DOI] [PubMed] [Google Scholar]
- 30.Kong DS, Kwon KH, et al. Combined surgical approach with intraoperative endovascular embolization for inaccessible dural arteriovenous fistulas. Surg Neurol. 2007;68:72–78. doi: 10.1016/j.surneu.2006.10.018. [DOI] [PubMed] [Google Scholar]
- 31.Krisht AF, Burson T. Combined pretemporal and endovascular approach to the cavernous sinus for the treatment of carotid-cavernous dural fistulas: technical case report. Neurosurgery. 1999;44(2):415–418. doi: 10.1097/00006123-199902000-00113. [DOI] [PubMed] [Google Scholar]
- 32.Kubo M, Kuwayama N, et al. Dural arteriovenous fistulas developing at different locations after resolution of previous fistulas: Report of three cases and review of the literature. Am J Neuroradiol. 2002;23:787–789. [PMC free article] [PubMed] [Google Scholar]
- 33.Kuwayama N, Endo S, et al. Surgical transvenous embolization of a cortically draining carotid cavernous fistula via a vein of the sylvian fissure. Am J Neuroradiol. 1998;19(7):1329–1332. [PMC free article] [PubMed] [Google Scholar]
- 34.Lawton M, Chun J, et al. Ethmoidal dural arteriovenous fistule: an assessment of surgical and endovascular management. . Neurosurgery. 1999;45(4):805. doi: 10.1097/00006123-199910000-00014. [DOI] [PubMed] [Google Scholar]
- 35.Lefkowitz M, Giannotta SL, et al. Embolization of neurosurgical lesions involving the ophthalmic artery. Neurosurgery . 1998;43(6):1298–1303. doi: 10.1097/00006123-199812000-00016. [DOI] [PubMed] [Google Scholar]
- 36.Leonard F, Jeffrey B, Nicholas JV. Cavernous sinus fistulas: carotid cavernous fistulas and dural arteriovenous malformations. Current Neurology & Neuroscience Reports. 2003;3(5):415–420. doi: 10.1007/s11910-003-0025-x. [DOI] [PubMed] [Google Scholar]
- 37.Liu HM, Huang YC, et al. Transarterial embolization of complex cavernous sinus dural arteriovenous fistulas with low-concentration cyanoacrylate. Neuroradiology. 2000;42:766–770. doi: 10.1007/s002340000405. [DOI] [PubMed] [Google Scholar]
- 38.Lv X, Li Y, Wu Z. Endovascular treatment of the anterior cranial fossa dural arteriovenous fistulas. Neuroradiology. 2008;50:433–437. doi: 10.1007/s00234-007-0346-6. [DOI] [PubMed] [Google Scholar]
- 39.Masahiro S, Hiroki K, et al. Stereotactic radiosurgery for tentorial dural arteriovenous fistulas draining into the vein of Galen: reports of two cases. Neurosurgery. 2000;46(3):730. doi: 10.1097/00006123-200003000-00039. [DOI] [PubMed] [Google Scholar]
- 40.Matsushige T, Nakaoka M, et al. Tentorial dural arteriovenous malformation manifesting as trigeminal neuralgia treated by stereotactic radiosurgery: a case report. Surg Neurol. 2006;66:519–523. doi: 10.1016/j.surneu.2006.01.022. [DOI] [PubMed] [Google Scholar]
- 41.Mayfrank L, Reul J, et al. Microsurgical interhemispheric approach to dural arteriovenous fistulas of the floor of the anterior cranial fossa. Minimally Invasive Neurosurgery. 1996;39(3):74–77. doi: 10.1055/s-2008-1052221. [DOI] [PubMed] [Google Scholar]
- 42.Nakamura M, Tamaki N, et al. Selective transvenous embolization of dural carotid-cavernous sinus fistulas with preservation of sylvian venous outflow. Report of three cases. J. Neurosurg. 1998;89(5):825–829. doi: 10.3171/jns.1998.89.5.0825. [DOI] [PubMed] [Google Scholar]
- 43.Oishi H, Arai H, et al. Complications associated with transvenous embolization of cavernous dural arteriovenous fistula. . Acta Neurochir. 1999;141:1265–1271. doi: 10.1007/s007010050429. [DOI] [PubMed] [Google Scholar]
- 44.Pannu Y, Shownkeen H, et al. Obliteration of a tentorial dural arteriovenous fistula causing spinal cord myelopathy using the cranio-orbital zygomatic approach. Surg Neurol. 2004;62:463–467. doi: 10.1016/j.surneu.2004.01.017. [DOI] [PubMed] [Google Scholar]
- 45.Patrik RT, Harry JC, et al. Evolution of the management of tentorial dural arteriovenous malformations. Neurosurgery. 2003;52(4):750–762. doi: 10.1227/01.neu.0000053221.22954.85. [DOI] [PubMed] [Google Scholar]
- 46.Paula-Lucas C, Pereica-Caldas J-G-M, Prandini MN. Do leptomeningeal venous drainage and dysplastic venous dilation predict hemorrhage in dural arteriovenous fistula? Surg Neurol. 2006;66:S3:2–S3:6. doi: 10.1016/j.surneu.2006.02.040. [DOI] [PubMed] [Google Scholar]
- 47.Quinones D, Duckwiler G, et al. Embolization of dural cavernous fistulas via superior ophthalmic vein approach. Am J Neuroradiol. 1997;18(5):921–928. [PMC free article] [PubMed] [Google Scholar]
- 48.Roy D, Raymond J. The role of transvenous embolization in the treatment of intracranial dural arteriovenous fistulas. Neurosurgery. 1997;40(6):1133–1144. doi: 10.1097/00006123-199706000-00004. [DOI] [PubMed] [Google Scholar]
- 49.Satomci J, Satoh K, et al. Angiographic changes in venous drainage of cavernous sinus dural arteriovenous fistulas after palliative transarterial embolization or observational management: a proposed stage classification. Neurosurgery. 2005;56:494–502. doi: 10.1227/01.neu.0000153750.95524.62. [DOI] [PubMed] [Google Scholar]
- 50.Siekmann R, Weber W, et al. Transvenous treatment of a dural arteriovenous fistula of the transverse sinus by embolization with platinum coils and Onyx HD 500+. Interventional Neuroradiology. 2005;11(3):281–286. doi: 10.1177/159101990501100314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.So-Hyang I, Chang WO, Dae HH. Surgical management of an unruptured dural arteriovenous fistula of the anterior cranial fossa: natural history for 7 years. Surg Neurol. 2004;62:72–75. doi: 10.1016/j.surneu.2003.07.018. [DOI] [PubMed] [Google Scholar]
- 52.Suzuki S, Lee DW, et al. Transvenous treatment of spontaneous dural carotid-cavernous fistulas using a combination of detachable coils and Onyx. Am J Neuroradiol. 2006;27(6):1346–1349. [PMC free article] [PubMed] [Google Scholar]
- 53.Toulgoat F, Mounayer C, et al. Transarterial embolization of intracranial dural arteriovenous malformations with ethylene vinyl alcohol copolymer (Onyx-18). J Neuroradiol. 2006;33(2):105–114. doi: 10.1016/s0150-9861(06)77239-x. [DOI] [PubMed] [Google Scholar]
- 54.Troffkin NA, Graham CB, et al. Combined transvenous and transarterial embolization of a tentorial-incisural dural arteriovenous malformation followed by primary stent placement in the associated stenotic straight sinus. Case report. J. Neurosurg . 2003;99(3):579–583. doi: 10.3171/jns.2003.99.3.0579. [DOI] [PubMed] [Google Scholar]
- 55.Tu YK, Liu HM, Hu SC. Direct surgery of carotid cavernous fistulas and dural arteriovenous malformations of the cavernous sinus. Neurosurgery. 1997;41(4):798–806. doi: 10.1097/00006123-199710000-00006. [DOI] [PubMed] [Google Scholar]
- 56.Urtasun F, Biondi A, et al. Cerebral dural arteriovenous fistulas: percutaneous transvenous embolization. Radiology. 1996;199 (1):209–217. doi: 10.1148/radiology.199.1.8633147. [DOI] [PubMed] [Google Scholar]
- 57.Watanabe T, Matsumaru Y, et al. Multiple dural arteriovenous fistulas involving the cavernous and sphenoparietal sinuses. Neuroradiology. 2000;42:771–774. doi: 10.1007/s002340000332. [DOI] [PubMed] [Google Scholar]
- 58.White DV, Sincoff EH, Abdulrauf SI. Anterior ethmoidal artery: mirosurgical anatomy and ethmoidal considerations. Neurosurgery. 2005;56(4) ONS(2):406–410. doi: 10.1227/01.neu.0000156550.83880.d0. [DOI] [PubMed] [Google Scholar]