Summary
The treatment of giant, large, multiple or wide-necked carotid siphon aneurysms has always represented a challenge for neurosurgeons and neuroradiologists. Very recently the use of stents with tiny holes has been proposed by two companies: Balt Silk Stent in Europe and Pi-peline in America. We have used the Silk stent on a few patients and describe our first case who now has an eleven month follow-up. The carotid siphon presented three converging aneurysms sharing a very large common neck. The Silk stent (Balt Extrusion, Montmorency, France) was deployed through a 4F Balt introducer. The procedure was uneventful and very quick. As soon as the stent was positioned contrast medium stagnation was displayed within the aneur-ysm. The patient’s post-operative course was normal and she was discharged three days later in good health.
Key words: intracranial stenting, siphon aneurysms, interventional neuroradiology
Introduction
The treatment of giant, large, multiple or wide-necked carotid siphon aneurysms has always represented a challenge for neurosurgeons and neuroradiologists1-5. The endovascular approach offered acceptable solutions with a variety of techniques but proved difficult lacking an optimal solution: carotid embolization with non detachable balloons and later with detachable ones, embolization of the siphon with coils associated or not with coiling of the aneurysmal cavity, embolization of the aneurysm with coils using the remodelling technique6, using coils and an intracranial stent to protect the aneurysm neck, using a balloon or stent-assisted Onyx embolization, etc. None of these techniques was completely satisfactory and they lacked a definite impact on aneurysm symptoms, namely mass effect.
Very recently the use of stents with tiny holes has been proposed by two companies: Balt Silk Stent in Europe and Pipeline in America. We have used the Silk stent on a few patients and this report describes the first one who now has eleven months of follow-up. The choice of this technique was based on long-standing experience that the reduction in size of aneurysms occluded by balloons without any material inside the aneurysm itself has a better effect on symptoms because of the reduced mass effect.
Case Report
A 59-year-old woman presented with a few months’ history of pain in the territory of the II and III branches of the left trigeminal nerve. Brain MR scan with angiographic sequences performed elsewhere disclosed an aneurysm in the supraclinoid portion of the left internal carotid artery. The patient was referred to our institution for appropriate treatment.
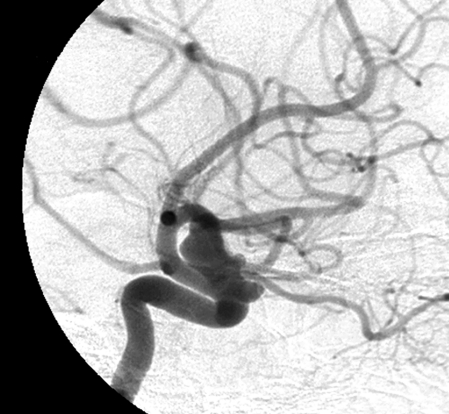
Diagnostic angiography revealed three converging wide-necked aneurysms of different sizes in the left carotid-ophthalmic artery region. The carotid siphon was broad and with irregular morphology.
The patient was assessed together with neurosurgeons and offered endovascular treatment with placement of an intracranial Silk stent (Balt Extrusion, Montmorency, France) in the left carotid siphon in front of the neck shared by the three aneurysms. On obtaining her informed consent, the patient was transferred from Neurosurgery to the Neuroradiology ward.
Material and Methods
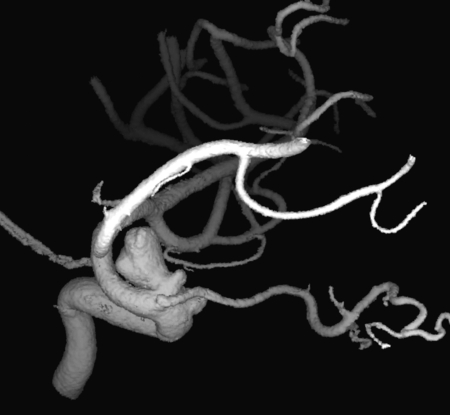
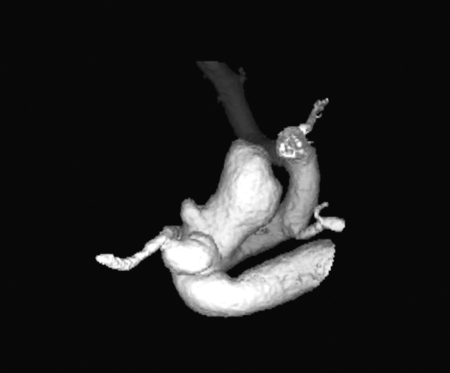
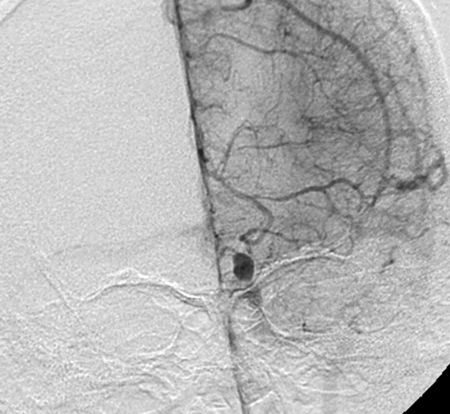
The carotid siphon presented three converging aneurysms (Figures 1 and 2) sharing a very large common neck. We confirmed the indication to use the Silk stent to occlude the aneurysmal cavity without deploying material inside the lesions.
Figure 1.
Digital subtraction angiography. A) Anteroposterior view. B) Lateral view. Note the three left carotid siphon aneurysms the last of which is the largest.
A.
B.
Figure 2.
Digital subtraction angiography. A) Oblique view. B,C) Three-dimensional reconstructions: these scans better display the size and irregular morphology of the aneurysms and their relations with the ophthalmic artery.
A.
B.
C.
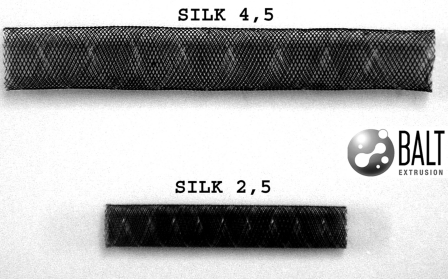
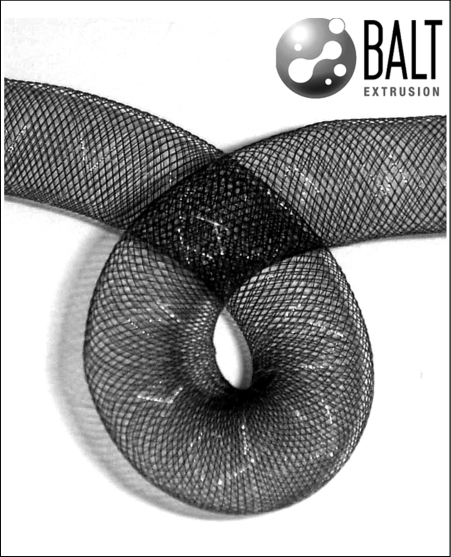
Angiographic evaluation was performed as usual with a 4F Terumo Headhunter and the Silk stent (Balt Extrusion, Montmorency, France; Figure 3A,B) was deployed through a 4F Balt introducer (Figure 3C). The procedure was uneventful and lasted only ten minutes.
Figure 3.
Photographs of the Silk stent (A, B) and the Balt-Leonardi-Chapot introducer (C): diameter 4F, length 90 cm.
A.
B.
C.
Just after stent placement contrast medium stagnation was displayed within the aneurysm. The patient’s post-operative course was normal and she was discharged three days later after follow-up MR angiography. The patient was given antiplatelet therapy and had a further three MR follow-up scans at one, three and six months after the endovascular procedure disclosing stent patency and signal change within the aneurysm.
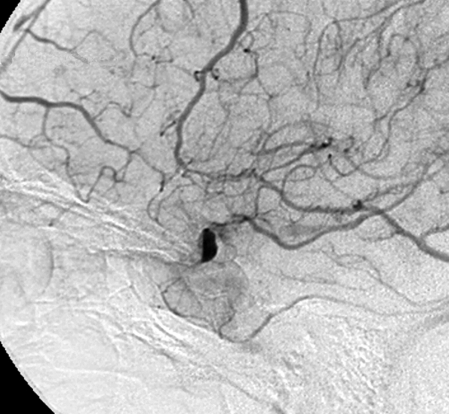
Three months after suspending antiplatelet therapy the patient underwent follow-up with digital angiography showing complete exclusion of the aneurysm from the circulation and a recovery of normal left carotid siphon morphology.
Anticoagulation and Antiplatelet Therapy
The patient was prepared administering a double antiplatelet therapy for three days before the procedure (ticlopidine 250 mg x 2 and aspirin 300 mg x 1). During the procedure she was treated with heparin 5000 U and aspirin 1000 mg. After the procedure we continued heparin for 48 hours and double antiplatelet for one week with ticlopidine 250 mg x 2, reduced to once in the following three weeks. Aspirin continued for six months.
Results
Immediately after stent deployment significant contrast medium stagnation was observed inside the aneurysm (Figures 4 and 5). Follow-up was performed by MR angiography with difficulty discerning whether the aneurysm was clotting or not. After the end of the antiplatelet therapy, we waited two more months and then performed digital subtraction angiography with the excellent result of complete aneurysm occlusion (Figure 6).
Figure 4.
Digital subtraction angiography. A) Anteroposterior view. B) Lateral view. Angiographic follow-up just after stent deployment, start of the venous phase with evident stagnation of contrast medium within the aneurysm. C) Unsubtracted digital angiography lateral view showing the stent and late stagnation of contrast medium.
A.
B.
C.
Figure 5.
Digital subtraction angiography. A) Anteroposterior view. B) Lateral view. Follow-up scans nine months after stent placement showing complete exclusion of the aneurysm from the circulation and recovery of normal left carotid siphon morphology.
A.
B.
Figure 6.
Digital subtraction angiography. A-C) Three-dimensional reconstructions obtained at follow-up nine months after stent placement.
A.
B.
C.
Conclusions
This new approach seems to be the best possible solution to the treatment of carotid siphon aneurysms. Of course more experience is needed to establish the occlusion time and the evolution of stented aneurysms. Ten patients have been treated in our department to date and the results will be presented after the long follow-up needed. We believe that aneurysm occlusion will be completed only after the interruption of antiplatelet therapy.
Acknowledgments
The authors thank Léopold and Nicholas Plowiecki, Aldo Cerruti and Marco Reale for their support, help and ongoing work for the best of our discipline, Interventional Neuroradiology.
References
- 1.Leonardi M, Dall’Olio M, et al. Intracranial stenting in the treatment of wide-necked aneurysms. Interventional Neuroradiology. 2007;13:19–30. doi: 10.1177/159101990701300103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Phatouros CC, Sasaki TYJ, et al. Stent-supported coil embolization: the treatment of fusiform and wide-neck aneurysms and pseudoaneurysms. Neurosurgery. 2000;47:107–115. doi: 10.1097/00006123-200007000-00023. [DOI] [PubMed] [Google Scholar]
- 3.Jou LD, Quick CM, et al. Computational approach to quantifying hemodynamic forces in giant cerebral aneurysms. Am J Neuroradiol. 2003;24:1804–1810. [PMC free article] [PubMed] [Google Scholar]
- 4.Roy D, Milot G, Raymond J. Endovascular treatment of unruptured aneurysms. Stroke. 2001;32:1998–2004. doi: 10.1161/hs0901.095600. [DOI] [PubMed] [Google Scholar]
- 5.Higashida RT, Halbach VV, et al. Initial clinical experience with a new self-expanding nitinol stent for the treatment of intracranial cerebral aneurysms: the Cordis Enterprise stent. Am J Neuroradiol. 2005;26:1751–1756. [PMC free article] [PubMed] [Google Scholar]
- 6.Moret J, Cognard C, et al. Reconstruction technique in the treatment of wide-neck intracranial aneurysms. Long-term angiographic and clinical results: apropos of 56 cases. J Neuroradiol. 1997;24:30–44. [PubMed] [Google Scholar]