Abstract
Adolescent sexual risk-taking is common and often occurs under the influence of alcohol. Although alcohol use emerges in early adolescence, there is little empirical research examining whether growth in alcohol use during this developmental period predicts later risky sexual behavior. Such information could provide a critical opportunity for the prevention of sexually transmitted infections and unwanted teenage pregnancies. The current study examined alcohol use as a developmental mediator of the relationship between conduct problems, impulsivity, poverty, race and menarche assessed at age 11, and sexual risk-taking among girls at age 16. The sample comprised 499 participants of the Pittsburgh Girls Study (57.7% African American and 42.3% European American) interviewed annually for 6 years between age 11 and 16. The results of the conditioned latent growth curve model showed that the rate of increase in alcohol use, and African American race, predicted higher rates of sexual risk-taking at age 16. However, European American race predicted the intercept and slope of alcohol use. When mediation was tested, the results showed that age 12 use and an increase in propensity for alcohol use between 12 and 15 explained the relationship between European American race and later risky sex, but this was not the case for African American girls. Use of alcohol at age 12 also mediated the association between early menarche and subsequent sexual risk-taking. The implications of the findings for sexual risk prevention are discussed.
Keywords: Risky sex, Girls, Alcohol use, Adolescence, Latent growth curves
High rates of sexual risk-taking behaviors, such as inconsistent condom use, multiple serial and/or concurrent sexual partners, and early age of first sexual intercourse among adolescents are major public health concerns (Centers for Disease Control and Prevention [CDC] 2009a; Poulin and Graham 2001). Recent reports indicate that there are 9.1 million diagnosed cases of sexually transmitted infections (STIs) among 15–24 year olds each year (CDC 2009b), that adolescents account for half of all new human immunodeficiency virus (HIV) infections (American Social Health Association 2005), and that the U.S. continues to have the highest rate of teenage pregnancy among developed countries (Abma et al. 2004). Increasing trends, such as a 42% increase in the period from 2000–2004 in the number of youth living with HIV/acquired immune deficiency syndrome (AIDS; CDC 2008) give further cause for concern.
Data show that adolescent girls pay a particularly high price for sexual risk-taking. In addition to the greater burden of teen parenthood (Cabrera et al. 2000), teenage girls are more likely than same-age boys to contract STIs (Quinn and Overbaugh 2005), including HIV, chlamydia, and gonorrhea (CDC 2009a). Racial/ethnic disparities also exist. Beginning in early adolescence, higher rates of STIs and unplanned pregnancies have been reported among African American adolescent girls compared with their European American counterparts (CDC 2009a; Hallfors et al. 2007). For example, between the ages of 10 and 14 years, African American girls are 11.4 times more likely to contract chlamydia, and 21.6 times more likely to contract gonorrhea than are European American girls (CDC 2009a). Evidence is mixed as to whether these disparities can be accounted for by differences in sexual risk behaviors. African American youth tend to initiate sexual intercourse at younger ages (Upchurch et al. 1998) and to report higher rates of multiple sexual partners (Ku et al. 2002) than European American youth. Other data however, indicate that African American adolescent girls are less likely than European American girls to engage in high-risk behaviors despite higher rates of STIs (Halpern et al. 2004), and are equally likely to report condom use (CDC 2009b), suggesting that other factors contribute to race disparities in vulnerability. Lower family income for example, is known to be associated with a greater likelihood of engaging in risky sexual behavior (Upchurch et al. 1999) possibly reflecting differences in future orientation, perceived life opportunities and available social roles (Brener and Collins 1998; Whitaker et al. 2000).
It is well established that the consumption of alcohol independently influences decisions around sex, and undermines skills for condom negotiation (e.g. Cooper 2002). Drinking alcohol is also linked with a greater number of sexual partners, condom accidents and an increased incidence of STIs (Brookmeyer and Henrich 2009; Stueve and O’Donnell 2005). The co-occurrence of alcohol use and risky sex is prevalent during adolescence: Over 20% of high school students reported that they were under the influence of alcohol during their last sexual interaction (CDC 2009b). More distally, alcohol use has been shown to predict timing of onset of sexual intercourse (e.g., Santelli et al. 2004). However, although alcohol use increases rapidly in early adolescence (Johnson et al. 2005), it is not known whether the rapidity with which propensity for alcohol use increases is an important risk factor for later sexual risk-taking. Evidence from a multi-wave longitudinal study of European American male and female youth followed from mid adolescence (age 15) to 28 years supports the notion that this dimension of alcohol use is important (Dogan et al. 2010). The results of this study showed that growth in alcohol use predicted a faster increase in the number of yearly sexual partners during late adolescence, after accounting for the effects of covariates such as conduct problems and aggression. The reverse relationship (i.e., increasing sexual partners predicting increased alcohol use) was not supported. Establishing whether such a relationship also holds in early adolescence, when the prevalence of alcohol use first begins to escalate, could provide critical opportunities for the prevention of adverse sexual health outcomes. The current study aims to improve understanding of these prospective relationships among adolescent girls.
Sexual risk-taking is frequently conceptualized along with other risky behaviors, including alcohol use, as part of a Problem Behavior Syndrome (Donovan and Jessor 1985). Consistent evidence from clinic-referred and community samples has shown that both conduct disorder (CD) and poor impulse control are associated with sexual risk-taking, such as early onset sexual intercourse and involvement with multiple partners (Crockett et al. 2006; Kahn et al. 2002) as well as earlier onset, and more rapid escalation of alcohol use and more problematic use of alcohol (e.g., Soloff et al. 2000; Tarter et al. 1999). In one prospective study of predominantly European American children, impulsiveness at age 3 predicted age of first romantic relationship and alcohol use at age 16, which in turn predicted greater number of sexual partners at age 19 (Zimmer-Gembeck et al. 2004). Although not formally tested in the study, this finding suggests that adolescent alcohol use may mediate the relationship between early behavior problems and poor impulse control in childhood, and sexual risk-taking in young adulthood.
The current study examines whether an increasing propensity to use alcohol among young adolescent females predicts subsequent sexual risk-taking in mid-adolescence and whether these developmental changes in alcohol use mediate the associations between early symptoms of CD and poor impulse control, and later risky sexual behavior. Prior research however suggests that these relationships will differ by race. First, African American youth tend to show a later onset of alcohol use (Wallace et al. 2003), and follow different developmental trajectories of alcohol use compared to European American teenagers (Flory et al. 2006). Second, it has been argued that Problem Behavior Theory does not explain the sexual behaviors of African American and European American youth equally well (Doljanac and Zimmerman 1998). For example, some studies have reported little correspondence between sexual risk-taking and either alcohol use or behavior problems among African American adolescents (e.g., Stanton et al. 1993), whereas others have reported a similar degree of covariation (Farrell et al. 1992). Third, early biological maturation is associated with earlier onset of alcohol use in girls (e.g., Lanza and Collins 2002) and with higher rates of alcohol use (Costello et al. 2006), yet it also tends to be more characteristic of African American than European American girls (Herman-Giddens et al. 1997). There has been a dearth of research examining these complex relationships and it remains unclear whether the relationships between early pubertal maturation, emerging alcohol use, and sexual risk-taking behaviors vary by race.
The current study examined the prospective relations between the development of alcohol use and sexual risk-taking in an urban community sample of African American and European American adolescent girls. Four hypotheses were tested. First we expected that symptoms of CD and impulsivity, early age of menarche, race and household poverty at age 11 (before sexual activity was initiated) would predict sexual risk-taking at age 16. Second, we hypothesized that onset and an increase in an individual’s propensity to use alcohol between ages 12 and 15 years would predict age 16 risky sexual behavior. Third, we tested the hypothesis that emerging alcohol use would mediate the relationship between the age 11 distal predictors and risky sex. Finally, we hypothesized that the mediating effects of increasing alcohol use on the relationship between distal predictors and risky sexual behavior would be stronger for European American than for African American girls.
Method
Sample Description
Participants in the current study were drawn from the Pittsburgh Girls Study (PGS): a longitudinal study of a community sample of 2,451 girls, ages 5–8 at the first assessment, and their primary caretakers. The PGS sample was identified following an enumeration of the City of Pittsburgh. In this process, all households in the poorest third of city neighborhoods, and 50% of the households in the remaining neighborhoods were sampled (see Hipwell et al. 2002; Keenan et al. 2010 for details). The analyses presented here use six waves of data collected prospectively on the oldest cohort of girls (N=622 at age 8 in assessment wave 1), from the age of 11 to 16 years. Retention of the original sample was high, with 88.1% participants (N=548) completing the ninth annual interview at age 16 years.
In order to examine specific relationships between alcohol use and risky sex for African American and European American girls, we excluded the small number of girls (N=33) representing other races. We also excluded one girl who reported that she had initiated sexual intercourse with a boy by age 11. Data on age 16 risky sexual behaviors were not available for 15 girls either because their caregivers requested that questions pertaining to sex should not be asked, or the girls refused to answer. Descriptive statistics for the final sample (N=499) of 288 (57.7%) African American and 211 (42.3%) European American girls are shown in Table 1.
Table 1.
Descriptive statistics for study variables (N=499)
| N (%) | Mean (SD) | European American (N=211)
|
African American (N=288)
|
p | |||
|---|---|---|---|---|---|---|---|
| N (%) | Mean (SD) | N (%) | Mean (SD) | ||||
| Covariates at age 11 | |||||||
| Public assistance | 130 (26.7) | 26 (12.7) | 64 (36.7) | *** | |||
| Conduct problems | .98 (1.7) | .78 (1.7) | 1.13 (1.7) | * | |||
| Impulsivity | 1.98 (1.7) | 1.63 (1.5) | 2.23 (1.8) | *** | |||
| Menarche | 139 (30.5) | 44 (23.7) | 95 (35.3) | ** | |||
| Rates of alcohol use | |||||||
| Age 12 | 77 (15.8) | 39 (18.9) | 38 (13.5) | ns | |||
| Age 13 | 91 (18.6) | 54 (26.0) | 37 (13.1) | *** | |||
| Age 14 | 135 (27.8) | 84 (41.0) | 51 (18.2) | *** | |||
| Age 15 | 157 (32.2) | 90 (43.9) | 67 (23.8) | *** | |||
| Age 16 risky sex behaviors | |||||||
| ≥ 2 partners | 57 (11.4) | 19 (9.0) | 38 (13.2) | ns | |||
| Inconsistent BC | 102 (20.4) | 32 (15.2) | 70 (24.3) | * | |||
| Pregnant | 27 (5.4) | 5 (2.4) | 22 (7.6) | ** | |||
| STI | 7 (1.4) | 3 (1.4) | 4 (1.4) | ns | |||
p<.05,
p<.01,
p<.001.
BC Birth Control, STI Sexually Transmitted Infection
There was differential attrition across the 6 years of follow-up by racial group. A greater percentage of European American (54%) than African American (46%) families were lost to follow-up (χ2[1]=4.57, p<.05). However, there were no significant differences between retained participants and those lost to follow-up on any other variables used in the study.
Procedure
Separate in-home interviews for the girl and caretaker were conducted annually by trained interviewers using a laptop computer. All study procedures were approved by the University of Pittsburgh Institutional Review Board. Families were compensated for their participation.
Measures
Sexual risk-taking was assessed by girl report using the Adolescent Sexual Activity Index (ASAI, Hansen et al. 1999) administered from age 11 onwards. In this, and every subsequent annual administration of the ASAI, girls who reported having sexual intercourse with a boy in the past year were also asked to report on the number of sexual partners. Three additional items assessed frequency and method of birth control, whether or not they had been pregnant and whether they had been diagnosed or treated for an STI in the past year. Frequency of birth control was assessed by asking: ‘Think of the times you have had sexual intercourse with a boy. How often did you use birth control? By that we mean condoms, birth control pill or patch, withdrawal, the boy pulls out etc.’ Four response choices were given: ‘never,’ ‘sometimes,’ ‘most of the time,’ and ‘always.’ If the girl responded ‘sometimes’ or more often, she was also asked which form(s) of birth control she used. Following prior research (e.g., Locke and Newcomb 2008), a risky sex index was created from four dichotomized items assessed at age 16: i) had sexual intercourse with two or more partners in the past year; ii) did not ‘always’ use birth control, and/or did not use condoms; iii) had been pregnant in the past year; and iv) had an STI in the past year (see Table 1). Of girls reporting STIs, 71.4% also reported inconsistent birth control, 42.9% had two or more sexual partners, and 28.6% had become pregnant in the past year. Of girls who had become pregnant, 85.7% reported inconsistent use of birth control, 28.6% had two or more partners and 7.1% contracted an STI. Becoming pregnant and contracting an STI were thus not fully accounted for by either reported number of sexual partners or use of birth control, including condoms. Of those girls who had ever had sexual intercourse, the ages of initiation were as follows: 3.9% at age 12, 3.9% at age 13, 11.8% at 14, 21.9% at 15 and the remaining 58.5% at 16 years. ‘Young age at first sexual intercourse’ was not included in the index to ensure that predictors temporally pre-dated the outcome variable. Girls reporting no sexual activity in the past year were coded as not engaging in sexual risk-taking. The majority (78.9%) of 16 year-old girls reported no sexually risky behavior, 11.2% reported one, 8.1% reported two and 1.7% reported three or four behaviors.
Alcohol Use
Girls reported on any use of beer, wine, or distilled spirits in the past year, using items adapted from the Rutgers Health and Human Development Project (Pandina et al. 1984). Among 12-year-old girls reporting use in the past year, all reported drinking less than once per month. Due to the low variability in the frequency of alcohol use, past year reports of any alcohol use (coded 0=no, 1=yes) at ages 12–15 were used.
Conduct problems and impulsivity were assessed using caregiver reports on the Child Symptom Inventory–4th edition (CSI-4; Gadow and Sprafkin 1994). Items assessed the severity of clinical symptoms consistent with DSM-IV criteria (American Psychiatric Association 1994). The 15 symptoms of CD (e.g., ‘How often has she bullied, threatened, or intimidated someone?’) and three symptoms of impulsivity (e.g., ‘Had difficulty awaiting turn in group activities’) were scored on 4-point scales (0=never to 3= very often) to generate severity scores. Adequate concurrent validity, sensitivity and specificity of CD and impulsivity symptom scores to clinicians’ diagnoses have been reported for the CSI (Gadow and Sprafkin 1994). In the present study, the internal consistency coefficient was α=.73 for CD items and .76 for impulsivity items at age 11.
Pubertal Maturation
Onset of menarche by age 11 was assessed using one item scored as 0 (no) or 1 (yes) on the Pubertal Development Scale (Petersen et al. 1988). Although menarche occurs relatively late in the pubertal process, this salient event has greater immediate adaptive significance than other more gradual maturational processes (Ge et al. 2001) and allows for comparability with other studies.
Data Analytic Plan
Race differences in the study variables were first examined using ANOVAs for continuous scores and chi square analyses for categorical (binary) variables, and Spearman’s rho coefficients were used to evaluate the magnitude of association among the age 11 predictors. The main effects of the age 11 variables on subsequent risky sexual behavior, were then examined by conducting bivariate ordinal regressions.
Latent growth curve models (LGCMs) were used to characterize change in girls’ propensity for alcohol use from ages 12–15 years. The models were estimated using a weighted least squares estimator in Mplus 6 (Muthén and Muthén 2010) to allow for non-normally distributed data. Missing data on dependent variables were handled using the expectation maximization (EM) algorithm. Model fit was evaluated using the χ2 goodness of fit test, comparative fit index (CFI), Tucker-Lewis index (TLI), and root-mean-square error of approximation (RMSEA). For CFI and TLI, we used the conventional cutoff ≥. 90 for acceptable fit, and ≥. 95 for good fit. RMSEA values between .05–.08 represent acceptable fit, whereas values <.05 indicated good fit (McDonald and Ho 2002).
We first estimated an unconditional LGCM. Time points were fixed incrementally to reflect the annual assessment schedule (i.e., age 12 fixed at 0, age 13 fixed at 1, age 14 fixed at 2, and age 15 fixed at 3). We expected that the intercept and slope variance and slope mean parameters would be significant, indicating variability around age 12 alcohol use and change over time, as well as a steady increase in alcohol use propensity between 12 and 15 years. We then tested the fit of the model conditioned on race, and age 11 household poverty, conduct problems, impulsivity, and menarche. Risky sex at age 16 was regressed on the growth model, and the putative interaction between race and the slope of alcohol use predicting risky sex at age 16 was tested using a series of nested multiple group latent growth curve models (cf. Muthén and Curran 1997). The nested model constrained a single parameter (e.g., path coefficient) to be equal for African American and European American girls. We used a χ2 difference test to compare the nested model with the base model that assumed the parameter to be unequal across race. If the constraint did not result in a significantly worse fit over the base model, the parameter was assumed to be equal for both races.
Finally, we examined whether the alcohol use latent factors mediated the relationship between age 11 predictors and age 16 risky sex. Mediation effects were tested regardless of whether there were significant direct effects between the age 11 predictors and alcohol trajectories and risky sex, given that the requirement of a direct effect prior to testing for mediation has been shown to significantly reduce statistical power to detect an effect (Shrout and Bolger 2002).
Results
Descriptive Statistics
Among the families receiving public assistance, 12.7% were European American and 36.7% were African American caregivers (χ2 [1]=39.10, p<.001, see Table 1). Conduct problems and impulsivity scores were higher among African American girls than among European American girls (F[1,496]=4.81, p<.05 and F[1,496]=15.18, p<.001 respectively). Severity of conduct problems were moderately correlated with impulsivity scores (Spearman’s rho=.425, p<.001). Approximately one third (31%) of girls had reached menarche by age 11, a rate that was significantly higher for African American girls than European American girls (χ2 [1]=7.05, p<.01). In addition, European American girls were more likely than African American girls to report alcohol use at ages 13, 14 and 15, but were less likely to report inconsistent use of birth control, and were less likely to have been pregnant in the past year.
Main Effects of Age 11 Predictors on Risky Sex at Age 16
Bivariate ordinal regression analyses showed that African American race (Wald=9.11, p<.01), living in household poverty (Wald=8.87, p<.01) and higher levels of impulsivity symptoms (Wald=5.69, p<.05) at age 11 predicted sexual risk-taking 5 years later. Severity of conduct problems at age 11 and reaching menarche by age 11 did not show direct effects on risky sex in mid-adolescence.
Unconditional Latent Growth Curve Models
The unconditional LGCM for alcohol use in the total sample fit the data well: χ2 [3] =2.83, p=.42; CFI=1.00; TLI=1.00; and RMSEA<.001. The LGCM had a significant mean slope, Ms=.18, z=7.15, p<.001, confirming that there was significant growth in propensity for alcohol use across early adolescence. The Ms value of 0.18 can be interpreted as the increase in proportion of alcohol users per year (0.18×3 [T15 - T12]=.54), which corresponds to a 54% increase in the proportion of users across ages 12 to 15 years. The variances for the intercept and slope were Di=0.65, z=6.41, p<.001 and Ds=.08, z=3.13, p<.01 respectively, indicating substantial variation across girls in both initial use and trajectory of use. Initial levels of alcohol use were negatively associated with propensity to use alcohol over time (b=−.09, z=−2.05, p=.04). A linear slope fit the data best; when testing a quadratic trend in slope, the model failed to converge.
Model Including Race, Conduct Problems, Impulsivity, Menarche and Poverty as Covariates
The linear model including covariates also fit the observed data well: χ2[11]=14.40, p=.35; CFI=.998; TLI=.994; and RMSEA=.01. The severity of girls’ conduct problems at age 11 was associated with a greater likelihood of alcohol use at age 12 (β=.13, p=.01). Reaching menarche by age 11 also predicted an increased likelihood of alcohol use in the following year (β=.19, p=.04). A reduced likelihood of alcohol use at age 12 was predicted by living in poverty at age 11 (β=−.18, p=.03), and by African American race (β=−.42, p<.001). Level of impulsivity at age 11 was not associated with alcohol use in the following year.
The rate of increase in alcohol use between ages 12 and 15 years was predicted by girls’ race (β=−.43, p<.001), indicating a faster rate of growth among European American than African American girls. In contrast, conduct problems, impulsivity, menarche and household poverty were unrelated to change in the propensity to use alcohol between ages 12 and 15.
Effect of the Conditioned Models on Risky Sex at Age 16, Controlling for Race, Conduct Problems, Impulsivity, Menarche and Poverty
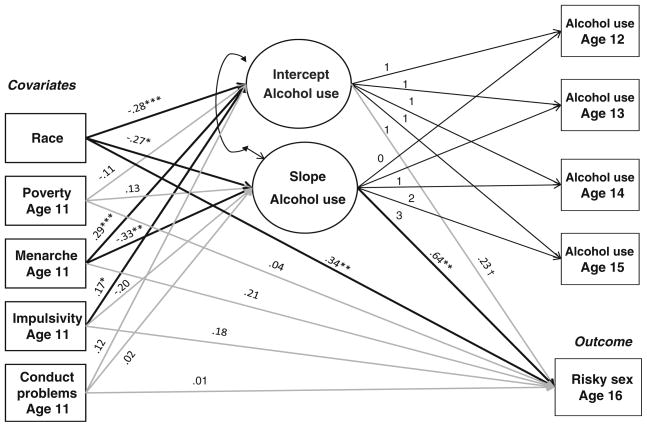
To examine the unique effects of the conditioned baseline model on later risky sex, risky sex at age 16 was then regressed on the latent variable growth factors and the covariates. Standard indicators showed that the model continued to fit the data well: χ2 [16]=20.02, p=.22; CFI=.995; TLI=.985; and RMSEA=.02. Higher initial level of alcohol use at age 12 was marginally related (β=.23, p=.07) to a greater likelihood of engaging in risky sex at age 16 (see Fig. 1). However, a more rapid increase in alcohol use from ages 12–15 was significantly associated with risky sex at age 16 (β=.64, p<.01). Race was also uniquely associated with risky sex. Thus, African American girls were more likely to engage in risky sex at age 16 (β=.34, p<.01) after controlling for conduct problems, poor impulse control, household poverty and menarche. None of the other covariates uniquely predicted risky sex at age 16 in this model.
Fig. 1.
Final conditioned latent growth curve model of risky sex at age 16, controlling for race, conduct problems, impulsivity, menarche and poverty. Note: †p<.10, *p<.05, **p<.01, ***p<.001. Standardized beta weights are shown. For clarity, the parameters between the covariates are excluded. The bivariate relationships between the covariates are provided in the text
Multiple group latent growth curve analyses did not reveal any race difference for risky sex regressed on the growth in alcohol use (Δχ2[1]=1.48, p=.224), indicating that the relation between race and propensity to use alcohol predicting risky sex did not differ substantially between African American and European American girls.
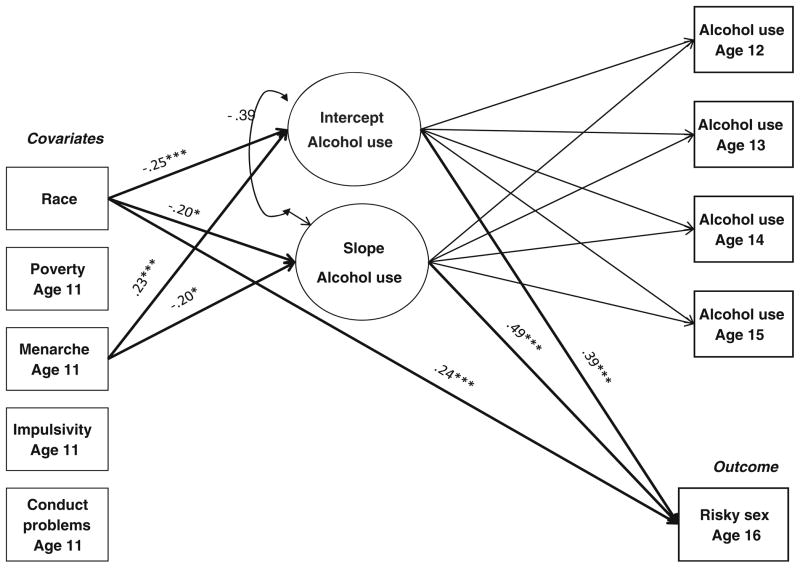
Finally, the mediating effects of alcohol use on the relationships between distal predictors and risky sex were tested. The results showed specific indirect effects for race on risky sex at age 16 via the intercept of alcohol use (β=−.10, p<.01) and the rate of change in alcohol use (β=−.095, p<.05). Thus, initial level of alcohol use and a faster rate of increase in alcohol use mediated the relationship between European American girls and the likelihood of engaging in risky sex at age 16 years. However a direct effect of race also remained (β=.24, p<.001) indicating that African American girls engaged in higher rates of risky sex, and this was not explained by initial levels or change in alcohol use (see Fig. 2). The results also showed that use of alcohol at age 12 mediated the effects of early menarche on subsequent risky sex (β=.09, p<.01), and there was a trend for a mediating effect of rate of increase in alcohol use on the association between early menarche status and risky sex outcome (β=− .11, p=.063). Neither initial level of alcohol, nor growth in the rate of alcohol use mediated the effects of conduct problems, impulsivity or household poverty on risky sex.
Fig. 2.
Mediating effects of alcohol use on the relationships between distal predictors and risky sex. Note: *p<.05, ***p<.001. Standardized beta weights are shown. For clarity, only the mediated paths that are significant are shown. The beta weights for all other paths are available from the author on request. Results showed indirect paths from race to risky sex via the intercept of alcohol use (β=−.10, p<.01) and rate of change in alcohol use (β=−.095, p<.05). Analyses also revealed an indirect path from menarche at age 11 to risky sex via the intercept of alcohol use (β=.09, p<.01)
Discussion
The current study extends the large body of work reporting on the association between alcohol use and sexual risk-taking by examining the predictive utility of developmental change in alcohol use across early adolescence in a community sample of girls. Our findings showed an increasing propensity to use alcohol across the early adolescent period, an effect that was primarily due to a higher rate of alcohol use at age 12 and a faster rate of increase in alcohol use across subsequent years among European American compared with African American girls. Indeed, both use of alcohol at age 12, and increasing likelihood of alcohol use over time, mediated the effects of European American race on subsequent risky sex after controlling for the effects of problem behaviors and low SES. Increasing use of alcohol by European American girls may result in sexual risk-taking via alcohol’s adverse effects on decision making, awareness of social norms or perceptions of acceptable behavior (Parsons et al. 2004). Alternatively, the link between more rapid increases in alcohol use and later sexual risk-taking may result from the subjective experience of alcohol’s effect on serotonin and gamma-aminobutyric acid brain receptors (Graham et al. 2000) with the effect of reducing anxiety about the consequences of one’s actions, resulting in deceased cognitive restraint and increased risk-taking.
The results also showed that African American girls were at higher risk than European American girls for engaging in risky sex at age 16 after controlling for household poverty, conduct problems, impulsivity and early menarche. Furthermore, this association was not explained by emerging patterns of alcohol use. Thus, in the current sample, alcohol acted as a differential risk mechanism for girls of African and European American race, and this is consistent with prior studies that have reported little covariation between sexual risk-taking and alcohol use among African American adolescents (e.g., Stanton et al. 1993). In fact, the variables included in the current analyses did not explain the disparity in sexual risk-taking across these racial groups. These results add to the growing contention that contextual factors (e.g., structure of sexual contact networks, negative attitudes towards contraception, neighborhood disadvantage) might better account for racial/ethnic disparities in HIV and STI risk than individual-level determinants (Adimora and Schoenbach 2005; Fichtenberg et al. 2009; Lightfoot and Milburn 2009; Thorburn and Bogart 2005). Identifying contextually sensitive mechanisms of sexual risk-taking is clearly an important avenue for future research and tailored prevention programming.
The findings of the LGCMs also revealed that reaching menarche by age 11 predicted alcohol use in the following year, and that alcohol use at age 12 mediated the effect of early maturation on later risky sexual behavior. Although not significant, there was a trend for increasing use of alcohol to mediate the effect of menarche by age 11 on sexual risk-taking. This pattern of results is consistent with prior findings indicating that the association between early pubertal maturation and high-risk behaviors among girls is relatively short-lived, and that by mid-adolescence any direct effects have generally dissipated (Dick et al. 2000). It should be noted however, that in the current study, more than 30% of the sample had already reached menarche by age 11 and as a result, this variable may not have been the most sensitive indicator of early maturation or a subgroup at highest risk for problematic behaviors. Future work using other indices of physical development such as Tanner stage timing or rapidity of maturation either singly or in combination with timing of menarche may provide important insights into the groups at highest risk at a young age. Nevertheless, the current results are congruent with prior evidence suggesting that early pubertal development has an indirect effect on later risk-taking behaviors via proximal mediating causal factors (Caspi et al. 1993). Our findings suggest that early emerging alcohol use is one such mediating factor.
Although bivariate associations were revealed between conduct problems, poor impulse control, and household poverty and engaging in risky sex 5 years later, there were no direct or mediated effects of these distal predictors in the multivariate models. These results appear to qualify early reports of direct links between low SES and behavior problems on risky sex (Kahn et al. 2002; Upchurch et al. 1999). Furthermore, controlling for household poverty did not account for the association between African American race and sexual risk-taking. However, given that sexual risk-taking is prevalent among adolescents and there is generally little to distinguish sexual activity from sexual risk-taking in mid-adolescent girls (Hipwell et al. 2011), multiple developmental pathways are likely to be operating. For example, Zimmer-Gembeck and Helfand (2008) suggested that dispositional traits (e.g., poor impulse control) combined with problem behaviors may be important predictors of early sexual debut, which is then associated with a greater number of sexual partners, lower rates of contraception use, and increased rates of unwanted pregnancy and STIs by mid-adolescence (e.g., Kaestle et al. 2005; Niccolai et al. 2004). A pathway to more typical onset of adolescent sexual behavior may comprise biological characteristics (e.g., earlier maturation), some minor problem behaviors (e.g., experimentation with alcohol) and cultural norms about the acceptability of teenage pregnancy. In addition to heterogeneity in pathways to sexual risk-taking, there is likely to be heterogeneity among the girls scoring high on sexual risk-taking. For example, some girls may have planned to become pregnant because they perceived support from extended family and the community (Azibo 1996), others may have prioritized intimacy in relationships over safe sexual practices (Kerrigan et al. 2007). In these cases, there may have been little covariation between condom use and other high risk behaviors. Research that aims to parse this heterogeneity by examining the moderating effects of contextual and normative factors as well as the developmental clustering of risk and protective factors for different sexual risk behaviors (e.g., inconsistent contraception use, multiple partners) is clearly needed.
Limitations and Future Directions
Several methodological limitations should be noted. First, the current study relied on self-reported STI information and no corroborative biological data were available. Given that asymptomatic STIs are prevalent and adolescent awareness of infection tends to be low (Kane et al. 2001), the rate of STIs in the current sample is likely to be underestimated. Second, we elected to combine girls reporting no sexual activity in the past year with girls who were sexually active but not engaging in risky behaviors. It is possible that this approach masked some developmental heterogeneity whereby some of these girls may have engaged in sexual risk behaviors at an earlier time, then desisted. However, data suggest that sexual risk-taking is relatively stable (e.g., 60% of girls in the current sample using birth control inconsistently at age 15 also reported inconsistent use at age 16, χ2=23.2, df=1, p<.001). Nevertheless, the approach of combining these possibly different types of girls into one group likely produced more conservative findings about the predictive utility of increasing alcohol use for subsequent sexual risk-taking than if prior sexual history was also considered in the model. Although examination of this developmental variability was beyond the scope of the current paper, it is clearly an important question that warrants further investigation. Third, girls’ report of any alcohol use included sips, tastes as well as full standard drinks, and frequency of use was not examined. The low threshold for endorsing alcohol use may have further increased the heterogeneity within the sample, and diluted the strength of the associations with risky sex and the covariates. Furthermore, evidence from studies of adults has shown that the distal consequences of alcohol use depend on lifetime cumulative volume consumed, the way alcohol is drunk, and the context in which the drinking occurs (Leigh 2002). For example, heavy drinking episodes with intoxication are associated with higher sexual risks than lighter or non-binge drinking. These distinctions were not made in the current analyses due to the low variability in the frequency of alcohol use in this early developmental period, but it is possible that differing trajectories of alcohol use patterns were differentially related to sexual risk-taking. In addition, event-level analyses could provide more specific results about the role of alcohol in episodes of risky sexual behavior. Finally, marijuana use is also known to be related to sexual risk-taking (Lowry et al. 1994), and unlike alcohol, appears to be equally prevalent among African American and European American adolescents (Johnston et al. 2006). Future studies examining change in an individual’s propensity to use marijuana may identify this substance as an important predictor of risky sexual behavior for both African American and European American girls. Additional considerations for future research include assessment mode effects. For example, the interviewer-administered interview used in the current study may have yielded lower rates of use than self-administered questionnaires or computer-assisted self-interviews (Turner et al. 1998; Wright et al. 1998). Furthermore, although self-reports of substance use obtained in the context of good rapport, privacy and with the assurance of confidentiality are generally valid (Brener et al. 2003; Harrell 1997; Winters et al. 2008), biological procedures could be incorporated into future work to provide additional information about the accuracy of adolescent reports (Wagenaar et al. 1993).
The current study results point to the need for STI/teen pregnancy prevention efforts that focus on slowing the rate of increase in alcohol use in early adolescence. Such psycho-educational intervention efforts may be delivered effectively in schools (Toler et al. 2000), and may reduce both high-risk sexual behaviors as well as alcohol use-related problems (Cooperman et al. 2005). However, culturally tailored prevention programming is needed, given that alcohol use serves as a differential risk mechanism for girls of African American and European American race. Our results further highlight the disproportionate vulnerability of African American girls for sexual risk-taking, irrespective of emerging use of alcohol, and indicate a need for focused interventions to improve sexual health behaviors. Prior work has demonstrated the effectiveness of peer and adult-led programs that are skills-based, age appropriate, and that use cognitive-behavioral principles to elicit safer sex practices among adolescents (e.g., CDC 2010; Jemmott et al. 2006). Nevertheless, contextual factors that are differentially distributed by race may partially explain race differences in sexual risk-taking as well as the associated negative consequences. Such factors need to be identified and incorporated into universal prevention efforts.
Acknowledgments
This research was supported by grants from the National Institute of Mental Health (MH071790 & MH056630), the National Institute on Drug Abuse (DA012237), the FISA Foundation, and the Falk Fund. The authors would like to thank the participants and their families for their many contributions to this study.
Contributor Information
Alison Hipwell, Email: hipwellae@upmc.edu, Western Psychiatric Institute & Clinic, University of Pittsburgh Medical Center, 3811 O’Hara St, Pittsburgh, PA 15213, USA.
Stephanie Stepp, Western Psychiatric Institute & Clinic, University of Pittsburgh Medical Center, 3811 O’Hara St, Pittsburgh, PA 15213, USA.
Tammy Chung, Western Psychiatric Institute & Clinic, University of Pittsburgh Medical Center, 3811 O’Hara St, Pittsburgh, PA 15213, USA.
Vanessa Durand, Department of School Psychology, Duquesne University, Canevin Hall, Pittsburgh, PA 15282, USA.
Kate Keenan, Department of Psychiatry and Behavioral Neuroscience, University of Chicago, 5841 South Maryland Avenue, Chicago, IL 60637, USA.
References
- Abma J, Martinez G, Mosher W, Dawson B. Teenagers in the United States: Sexual activity, contraceptive use, and childbearing, 2002. Vital & Health Statistics - Series 23, Data from the National Survey of Family Growth. 2004:1–48. [PubMed] [Google Scholar]
- Adimora A, Schoenbach V. Social context, sexual networks, and racial disparities in rates of sexually transmitted infections. Journal of Infectious Diseases. 2005;191:S115–122. doi: 10.1086/425280. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- American Social Health Association. State of the nation 2005: Challenges facing STD prevention among youth - research, review and recommendations. Research Triangle Park, NC: Author; 2005. [Google Scholar]
- Azibo D. Mental health defined Africentrally. In: Azibo D, editor. African psychology in historical perspective and related commentary. Trenton, NJ: Africa World Press; 1996. pp. 47–56. [Google Scholar]
- Brener N, Collins J. Co-occurrence of health-risk behaviors among adolescents in the United States. Journal of Adolescent Health. 1998;22:209–213. doi: 10.1016/S1054-139X(97)00161-4. [DOI] [PubMed] [Google Scholar]
- Brener N, Billy J, Grady W. Assessment of factors affecting the validity of self-reported health-risk behavior among adolescents: Evidence from the scientific literature. Journal of Adolescent Health. 2003;33:436–457. doi: 10.1016/s1054-139x(03)00052-1. [DOI] [PubMed] [Google Scholar]
- Brookmeyer K, Henrich C. Disentangling adolescent pathways of sexual risk taking. Journal of Primary Prevention. 2009;30:677–696. doi: 10.1007/s10935-009-0196-6. [DOI] [PubMed] [Google Scholar]
- Cabrera N, Tamis-LeMonda C, Bradley R, Hofferth S, Lamb M. Fatherhood in the twenty-first century. Child Development. 2000;71:127–136. doi: 10.1111/1467-8624.00126. [DOI] [PubMed] [Google Scholar]
- Caspi A, Lynam D, Moffitt TE, Silva P. Unraveling girls’ delinquency: Biological, dispositional, and contextual contributions to adolescent misbehavior. Developmental Psychology. 1993;29:19–30. [Google Scholar]
- Centers for Disease Control and Prevention. HIV/AIDS Surveillance Report 2006. Vol. 18. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2008. [Google Scholar]
- Centers for Disease Control and Prevention. Sexually transmitted disease morbidity for selected STDs by age, race/ethnicity and gender 1996–2008. 2009a Retrieved May 6, 2010, from http://wonder.cdc.gov/std-v2008-race-age.html.
- Centers for Disease Control and Prevention. Sexually transmitted disease surveillance, 2008. Atlanta, GA: Department of Health and Human Services; 2009b. [Google Scholar]
- Centers for Disease Control and Prevention. Bringing high-quality HIV and STD prevention to youth in schools. Atlanta, GA: Department of Health and Human Services; 2010. [Google Scholar]
- Cooper M. Alcohol use and risky sexual behavior among college students and youth: Evaluating the evidence. Journal of Studies on Alcohol. 2002;(Suppl 14):101–117. doi: 10.15288/jsas.2002.s14.101. [DOI] [PubMed] [Google Scholar]
- Cooperman N, Falkin G, Cleland C. Changes in women’s sexual risk behaviors after therapeutic community treatment. AIDS Education and Prevention. 2005;17:157–169. doi: 10.1521/aeap.17.3.157.62901. [DOI] [PubMed] [Google Scholar]
- Costello E, Foley D, Angold A. 10-year research update review: The epidemiology of child and adolescent psychiatric disorders: II. Developmental epidemiology. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:8–25. doi: 10.1097/01.chi.0000184929.41423.c0. [DOI] [PubMed] [Google Scholar]
- Crockett L, Raffaelli M, Shen YL. Linking self-regulation and risk proneness to risky sexual behavior: Pathways through peer pressure and early substance use. Journal of Research on Adolescence. 2006;16:503–525. [Google Scholar]
- Dick D, Rose R, Viken R, Kaprio J. Pubertal timing and substance use: Associations between and within families across late adolescence. Developmental Psychology. 2000;36:180–189. [PubMed] [Google Scholar]
- Dogan S, Stockdale G, Widaman K, Conger R. Developmental relations and patterns of change between alcohol use and number of sexual partners from adolescence through adulthood. Developmental Psychology. 2010;46:1747–1759. doi: 10.1037/a0019655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doljanac R, Zimmerman M. Psychosocial factors and high-risk sexual behavior: Race differences among urban adolescents. Journal of Behavioral Medicine. 1998;21:451–467. doi: 10.1023/a:1018784326191. [DOI] [PubMed] [Google Scholar]
- Donovan J, Jessor R. Structure of problem behavior in adolescence and young adulthood. Journal of Consulting and Clinical Psychology. 1985;53:890–904. doi: 10.1037//0022-006x.53.6.890. [DOI] [PubMed] [Google Scholar]
- Farrell A, Danish S, Howard C. Risk factors for drug use in urban adolescents: Identification and cross-validation. American Journal of Community Psychology. 1992;20:263–286. doi: 10.1007/BF00937910. [DOI] [PubMed] [Google Scholar]
- Fichtenberg C, Muth S, Brown B, Padian N, Glass T, Ellen J. Sexual network position and risk of sexually transmitted infections. Sexually Transmitted Infections. 2009;85:493–498. doi: 10.1136/sti.2009.036681. [DOI] [PubMed] [Google Scholar]
- Flory K, Brown T, Lynam D, Miller J, Leukefeld C, Clayton R. Developmental patterns of African American and Caucasian adolescents’ alcohol use. Cultural Diversity & Ethnic Minority Psychology. 2006;12:740–746. doi: 10.1037/1099-9809.12.4.740. [DOI] [PubMed] [Google Scholar]
- Gadow K, Sprafkin J. Child Symptom Inventories manual. Stonybrook, NY: Checkmate Plus; 1994. [Google Scholar]
- Ge X, Conger R, Elder G. Pubertal transition, stressful life events, and the emergence of gender differences in adolescent depressive symptoms. Developmental Psychology. 2001;37:404–417. doi: 10.1037//0012-1649.37.3.404. [DOI] [PubMed] [Google Scholar]
- Graham K, West P, Wells S. Evaluating theories of alcohol-related aggression using observations of young adults in bars. Addiction. 2000;95:847–863. doi: 10.1046/j.1360-0443.2000.9568473.x. [DOI] [PubMed] [Google Scholar]
- Hallfors D, Iritani B, Miller W, Bauer D. Sexual and drug behavior patterns and HIV and STD racial disparities: The need for new directions. American Journal of Public Health. 2007;97:125–132. doi: 10.2105/AJPH.2005.075747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halpern C, Hallfors D, Bauer D, Iritani B, Waller M, Cho H. Implications of racial and gender differences in patterns of adolescent risk behavior for HIV and other sexually transmitted diseases. Perspectives on Sexual and Reproductive Health. 2004;36:239–247. doi: 10.1363/psrh.36.239.04. [DOI] [PubMed] [Google Scholar]
- Hansen W, Paskett E, Carter L. The Adolescent Sexual Activity Index (ASAI): A standardized strategy for measuring interpersonal heterosexual behaviors among youth. Health Education Research. 1999;14:485–490. doi: 10.1093/her/14.4.485. [DOI] [PubMed] [Google Scholar]
- Harrell AV. Research Monograph No. 167. Rockville, MD: National Institute on Drug Abuse; 1997. The validity of self-reported drug use data: The accuracy of responses on confidential self-administered answered sheets; pp. 37–58. [PubMed] [Google Scholar]
- Herman-Giddens M, Slora E, Wasserman R, Bourdony C, Bhapkar M, Koch G, et al. Secondary sexual characteristics and menses in young girls seen in office practice: A study from the Pediatric Research in Office Settings network. Pediatrics. 1997;99:505–512. doi: 10.1542/peds.99.4.505. [DOI] [PubMed] [Google Scholar]
- Hipwell AE, Loeber R, Stouthamer-Loeber M, Keenan K, White H, Kroneman L. Characteristics of girls with early onset disruptive and antisocial behaviour. Criminal Behaviour and Mental Health. 2002;12:99–118. doi: 10.1002/cbm.489. [DOI] [PubMed] [Google Scholar]
- Hipwell AE, Stepp S, Chung T, Loeber R, Keenan K. Brief Report: Parsing the psychosocial heterogeneity of adolescent sexual behaviors. Journal of Adolescence. 2011;34:589–592. doi: 10.1016/j.adolescence.2010.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jemmott J, Jemmott L, Fong G. Abstinence and safer sex HIV risk-reduction interventions for African American adolescents. Journal of the American Medical Association. 2006;279:1529–1536. doi: 10.1001/jama.279.19.1529. [DOI] [PubMed] [Google Scholar]
- Johnson P, Richter L, Kleber H, McLellan A, Carise D. Telescoping of drinking-related behaviors: Gender, racial/ethnic, and age comparisons. Substance Use & Misuse. 2005;40:1139–1151. doi: 10.1081/JA-200042281. [DOI] [PubMed] [Google Scholar]
- Johnston L, O’Malley P, Bachman J, Schulenberg J. Teen drug use continues down in 2006, particularly among older teens; but use of prescription-type drugs remains high. Ann Arbor: University of Michigan News and Information Services; 2006. [Google Scholar]
- Kaestle C, Halpern C, Miller W, Ford C. Young age at first sexual intercourse and sexually transmitted infections in adolescents and young adults. American Journal of Epidemiology. 2005;161:774–780. doi: 10.1093/aje/kwi095. [DOI] [PubMed] [Google Scholar]
- Kahn J, Kaplowitz R, Goodman E, Emans S. The association between impulsiveness and sexual risk behaviors in adolescent and young adult women. Journal of Adolescent Health. 2002;30:229–232. doi: 10.1016/s1054-139x(01)00391-3. [DOI] [PubMed] [Google Scholar]
- Kane R, Khadduri R, Wellings K. Screening for chlamydia among adolescents in the UK: A review of policy and practice. Health Education. 2001;101:108–115. [Google Scholar]
- Keenan K, Hipwell A, Chung T, Stepp S, Stouthamer-Loeber M, McTigue K, et al. The Pittsburgh Girls Study: Overview and initial findings. Journal of Clinical Child and Adolescent Psychology. 2010;39:506–521. doi: 10.1080/15374416.2010.486320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerrigan D, Andrinopoulos K, Johnson R, Parham P, Thomas T, Ellen J. Staying strong: Gender ideologies among African-American adolescents and the implications for HIV/STI prevention. Journal of Sex Research. 2007;44:172–180. doi: 10.1080/00224490701263785. [DOI] [PubMed] [Google Scholar]
- Ku L, St Louis M, Farshy C, Aral S, Turner CF, Lindberg L, et al. Risk behaviors, medical care, and chlamydial infection among young men in the United States. American Journal of Public Health. 2002;92:1140–1143. doi: 10.2105/ajph.92.7.1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanza S, Collins L. Pubertal timing and the onset of substance use in females during early adolescence. Prevention Science. 2002;3:69–82. doi: 10.1023/a:1014675410947. [DOI] [PubMed] [Google Scholar]
- Leigh B. Alcohol and condom use: A meta-analysis of event-level studies. Sexually Transmitted Diseases. 2002;29:476–482. doi: 10.1097/00007435-200208000-00008. [DOI] [PubMed] [Google Scholar]
- Lightfoot M, Milburn N. HIV prevention and African American youth: Examination of individual-level behaviour is not the only answer. Culture, Health & Sexuality. 2009;11:731–742. doi: 10.1080/13691050903078824. [DOI] [PubMed] [Google Scholar]
- Locke T, Newcomb M. Correlates and predictors of HIV risk among inner-city African American female teenagers. Health Psychology. 2008;27:337–348. doi: 10.1037/0278-6133.27.3.337. [DOI] [PubMed] [Google Scholar]
- Lowry R, Holtzman D, Truman B, Kami L, Collins J, Kolbe L. Substance use and HIV-related sexual behaviors among U.S. high school students: Are they related? American Journal of Public Health. 1994;84:1116–1120. doi: 10.2105/ajph.84.7.1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald R, Ho MHR. Principles and practice in reporting structural equation analyses. Psychological Methods. 2002;7:64–82. doi: 10.1037/1082-989x.7.1.64. [DOI] [PubMed] [Google Scholar]
- Muthén B, Curran P. General longitudinal modeling of individual differences in experimental designs: A latent variable framework for analysis and power estimation. Psychological Methods. 1997;2:371–402. [Google Scholar]
- Muthén L, Muthén R. Mplus: The comprehensive modeling program for applied researchers, (version 6) Los Angeles: Authors; 2010. [Google Scholar]
- Niccolai L, Ethier K, Kershaw T, Lewis J, Meade C, Ickovics J. New sex partner acquisition and sexually transmitted disease risk among adolescent females. Journal of Adolescent Health. 2004;34:216–223. doi: 10.1016/S1054-139X(03)00250-7. [DOI] [PubMed] [Google Scholar]
- Pandina R, Labouvie E, White H. Potential contributions of the life span developmental approach to the study of adolescent alcohol and drug use: The Rutgers Health and Human Development Project, a working model. Journal of Drug Issues. 1984;14:253–268. [Google Scholar]
- Parsons J, Vicioso K, Kutnick A, Punzalan J, Halkitis P, Velasquez M. Alcohol use and stigmatized sexual practices of HIV seropositive gay and bisexual men. Addictive Behaviors. 2004;29:1045–1051. doi: 10.1016/j.addbeh.2004.03.001. [DOI] [PubMed] [Google Scholar]
- Petersen A, Crockett L, Richards M, Boxer A. A self-report measure of pubertal status: Reliability, validity, and initial norms. Journal of Youth and Adolescence. 1988;17:117–133. doi: 10.1007/BF01537962. [DOI] [PubMed] [Google Scholar]
- Poulin C, Graham L. The association between substance use, unplanned sexual intercourse and other sexual behaviours among adolescent students. Addiction. 2001;96:607–621. doi: 10.1046/j.1360-0443.2001.9646079.x. [DOI] [PubMed] [Google Scholar]
- Quinn T, Overbaugh J. HIV/AIDS in women: An expanding epidemic. Science. 2005;308:1582–1583. doi: 10.1126/science.1112489. [DOI] [PubMed] [Google Scholar]
- Santelli J, Kaiser J, Hirsch L, Radosh A, Simkin L, Middlestadt S. Initiation of sexual intercourse among middle school adolescents: The influence of psychosocial factors. Journal of Adolescent Health. 2004;34:200–208. doi: 10.1016/j.jadohealth.2003.06.004. [DOI] [PubMed] [Google Scholar]
- Shrout P, Bolger N. Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychological Methods. 2002;7:422–445. [PubMed] [Google Scholar]
- Soloff P, Lynch K, Moss H. Serotonin, impulsivity, and alcohol use disorders in the older adolescent: A psychobiological study. Alcoholism, Clinical and Experimental Research. 2000;24:1609–1619. [PubMed] [Google Scholar]
- Stanton B, Romer D, Ricardo I, Black M, Feigelman S, Galbraith J. Early initiation of sex and its lack of association with risk behaviors among adolescent African-Americans. Pediatrics. 1993;92:13–19. [PubMed] [Google Scholar]
- Stueve A, O’Donnell LN. Early alcohol initiation and subsequent sexual and alcohol risk behaviors among urban youths. American Journal of Public Health. 2005;95:887–893. doi: 10.2105/AJPH.2003.026567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarter RE, Vanyukov M, Giancola P, Dawes M, Blackson T, Mezzich A, et al. Etiology of early age onset substance use disorder: A maturational perspective. Development and Psychopathology. 1999;11:657–683. doi: 10.1017/s0954579499002266. [DOI] [PubMed] [Google Scholar]
- Thorburn S, Bogart L. Conspiracy beliefs about birth control: Barriers to pregnancy prevention among African Americans of reproductive age. Health Education & Behavior. 2005;32:474–487. doi: 10.1177/1090198105276220. [DOI] [PubMed] [Google Scholar]
- Toler N, Roona M, Ochshorn P, Marshall D, Streke A, Stackpole K. School-based adolescent drug prevention programs: 1998 meta-analysis. Journal of Primary Prevention. 2000;20:275–336. [Google Scholar]
- Turner C, Ku L, Rogers S, Lindberg L, Pleck J, Sonestein R. Adolescent sexual behavior, drug use, and violence: Increased reporting with computer survey technology. Science. 1998;280:867–873. doi: 10.1126/science.280.5365.867. [DOI] [PubMed] [Google Scholar]
- Upchurch D, Levy-Storms L, Sucoff C, Aneshensel C. Gender and ethnic differences in the timing of first sexual intercourse. Family Planning Perspectives. 1998;30:121–127. [PubMed] [Google Scholar]
- Upchurch D, Aneshensel C, Sucoff C, Levy-Storms L. Neighborhood and family contexts of adolescent sexual activity. Journal of Marriage & the Family. 1999;61:920–933. [Google Scholar]
- Wagenaar A, Komro K, McGovern P, Williams C, Perry C. Effects of a saliva test pipeline procedure on adolescent self-reported alcohol use. Addiction. 1993;88:199–208. doi: 10.1111/j.1360-0443.1993.tb00803.x. [DOI] [PubMed] [Google Scholar]
- Wallace J, Jr, Bachman J, O’Malley P, Schulenberg J, Cooper S, Johnston L. Gender and ethnic differences in smoking, drinking and illicit drug use among American 8th, 10th and 12th grade students, 1976–2000. Addiction. 2003;98:225–234. doi: 10.1046/j.1360-0443.2003.00282.x. [DOI] [PubMed] [Google Scholar]
- Whitaker D, Miller K, Clark L. Reconceptualizing adolescent sexual behavior: Beyond did they or didn’t they? Family Planning Perspectives. 2000;32:111–117. [PubMed] [Google Scholar]
- Winters K, Stinchfield R, Bukstein O. Assessing adolescent substance use and abuse. In: Kaminer Y, Bukstein O, editors. Adolescent substance abuse: Psychiatric comorbidity and high risk behaviors. New York: Routledge; 2008. pp. 53–86. [Google Scholar]
- Wright D, Aquilino W, Supple A. A comparison of computer-assisted and paper-and-pencil self-administered questionnaires in a survey on smoking, alcohol and drug use. Public Opinion Quarterly. 1998;62:331–353. [Google Scholar]
- Zimmer-Gembeck M, Helfand M. Ten years of longitudinal research on U.S. adolescent sexual behavior: Developmental correlates of sexual intercourse, and the importance of age, gender and ethnic background. Developmental Review. 2008;28:153–224. [Google Scholar]
- Zimmer-Gembeck M, Siebenbruner J, Collins W. A prospective study of intraindividual and peer influences on adolescents’ heterosexual romantic and sexual behavior. Archives of Sexual Behavior. 2004;33:381–394. doi: 10.1023/B:ASEB.0000028891.16654.2c. [DOI] [PubMed] [Google Scholar]