Abstract
HIV-related stigma has a damaging effect on health outcomes among people living with HIV (PLWH), as studies have associated it with poor HIV medication adherence and depressive symptoms. We investigated whether depressive symptoms mediate the relationship between stigma and medication adherence. In a cross-sectional study, 720 PLWH completed instruments measuring HIV-related stigma, depressive symptoms, and HIV medication adherence. We used structural equation modeling (SEM) to investigate associations among these constructs. In independent models, we found that poorer adherence was associated with higher levels of stigma and depressive symptoms. In the simultaneous model that included both stigma and depressive symptoms, depression had a direct effect on adherence, but the effect of stigma on adherence was not statistically significant. This pattern suggested that depressive symptoms at least partially mediated the association between HIV-related stigma and HIV medication adherence. These findings suggest that interconnections between several factors have important consequences for adherence.
Keywords: adherence, antiretroviral treatment, stigma, depression, HIV/AIDS
INTRODUCTION
HIV-related stigma interferes with effective treatment and positive health outcomes for people living with HIV.(1) HIV-related stigma has been associated with low self-esteem, depression, anxiety, and poor health related quality of life.(1–4) Furthermore, HIV-related stigma has been associated with poor HIV medication adherence and low service utilization, which have direct negative impacts on morbidity and mortality.(5, 6)
Stigma is defined as negative attitudes held by members of the public.(7, 8) HIV-related stigma occurs in the social environment, where it may be sensed or experienced by a person living with HIV (PLWH), who may subsequently internalize this stigma.(9) HIV-related stigma that is internalized can contribute to poor medication adherence that in turn, affects health outcomes for PLWH.(6, 10) Our previous investigations have shown that PLWH may be non-adherent to HIV medications to conceal their HIV status.(6)
Like HIV-related stigma, depressive symptoms are a significant barrier to HIV medication adherence.(11, 12) Prevalence rates of major depressive disorder among PLWH have been reported to be as high as 37%, three times the rate found in general populations.(13, 14) One study found that depressive symptoms, side effects, self-efficacy, and social support distinguished between people who exhibited good and poor HIV medication adherence.(15) In our own investigations, we found that depressive symptoms were associated with poor HIV medication adherence among PLWH in China.(16) While HIV-related stigma is associated with HIV medication adherence and depression, and depression is associated with HIV medication adherence, studies have not simultaneously investigated the relationship among depressive symptoms, HIV-related stigma, and HIV medication adherence.
The purpose of this study was to examine associations between HIV-related stigma, depressive symptoms, and HIV medication adherence among PLWH in routine clinical care. We were chiefly interested in examining whether depressive symptoms would mediate (act as a mechanism that could explain) the relationship between HIV-related stigma and HIV medication adherence.
METHODS
Study Setting
This cross-sectional study was conducted among a convenience sample of patients in the University of Washington (UW) HIV Cohort, a longitudinal observational study of PLWH who receive primary care in the UW Harborview Medical Center HIV Clinic. Harborview is an urban public hospital and the HIV clinic is the largest single provider of HIV care in the Pacific Northwest region of the US. This study was approved by the UW Institutional Review Board.
Participants
PLWH aged 18 years and above who attended the clinic for a routine clinical care appointment between February and November of 2009 and were receiving antiretroviral therapy were eligible for the study. Patients were not compensated for participation. Patients unable to provide informed consent (e.g. participants with severely impaired cognitive functioning) or those who could not understand English or Spanish were excluded from the study.
Data sources
As part of routine clinic proceedings, English or Spanish-speaking patients use tablet personal computers with touch screens to complete a self-administered web-based assessment including measures of depressive symptoms, adherence, risk behaviors, physical functioning, and quality of life.(17) We added a measure of HIV-related stigma for the present study. Data were also obtained from the UW HIV Information System (UWHIS), which integrates comprehensive data on the UW HIV cohort from all outpatient and inpatient encounters including demographic, clinical, laboratory, medication, and socioeconomic information. Key data included socio-demographic and clinical characteristics such as self-reported race/ethnicity, sex, age, and recent CD4+ cell count.
HIV-related stigma
We assessed HIV-related stigma using 4 items from the Stigma Scale for Chronic Illness (SSCI).(18) Based on exploratory and confirmatory factor analyses from the initial study that evaluated the validity of the SSCI,(18) we chose 2 items that assessed enacted (i.e. experienced) stigma (“Because of my illness, some people avoided me”, “Some people acted as though it was my fault I have this illness”) and 2 items that assessed internalized stigma (“Because of my illness, I felt left out of things”, “I felt embarrassed about my illness””). Although the 4 items come from a larger scale, they stand alone as a single construct in our analysis. All four items used “lately” as the recall period. Each of these items had five response options ranging from “never” to “always”. Since the items refer to ‘my illness’, respondents were instructed to reference their HIV infection with the question “How often have the following statements regarding your HIV infection been true for you lately?” In addition, we calculated the percentage of participants who experienced “some HIV-related stigma”, which refers to a nonzero total score on the 4 items of the stigma scale.
Depressive symptoms
The 9-item Patient Health Questionnaire (PHQ-9) from the Primary Care Evaluation of Mental Disorders (PRIME-MD)(19, 20) was used to assess depressive symptoms. For each PHQ-9 item, patients are asked how often they experienced a depression symptom during the previous 2 weeks. Each item had four response options ranging from “not at all” to “nearly every day.” Standard PHQ-9 scores range from 0 to 27 and are categorized as: none (0–4 points), mild (5–9 points), moderate (10–14 points), moderately-severe (15–19) and severe (≥20 points) depressive symptom severity.(21)
HIV medication adherence
Participants self-reported HIV medication adherence by responding to 5 items. Three items were modified from the Adult AIDS Clinical Trial Group (AACTG) adherence assessment,(22, 23) including the number of doses missed in the previous 4 days (response options ranged from “0” to “more than 4”), missed doses on the previous weekend (“yes” or “no”), and time of last missed dose (response options ranged from “within the past week” to “never skip medication”). Patients were asked to rate their ability to take their HIV medications over the previous 4 weeks (response options ranged from “very poor” to “excellent”). Finally, patients were asked to rate their HIV medication adherence over the past month on a visual analog scale that ranged from 0% to 100%.(24, 25) Perfect adherence refers to 100% adherence on the visual analog scale.
Data Analyses
We used Structural Equation Modeling (SEM) techniques, which can include both continuous and discrete observed variables as indicators that measure unobservable latent variables (constructs). We used latent variables with multiple indicators for adherence, depressive symptoms, and HIV-related stigma. Latent variables differ from observed sum-scores of the indicators in that they account for measurement error in the items and items are allowed differential weights in estimating the latent construct.(26) We collapsed some categories of the adherence items because of sparse data and used exploratory and confirmatory factor analyses to recode HIV medication adherence variables to ensure that information was not being lost in the process of collapsing categories. We converted responses for the visual analog scale HIV medication adherence item to a four-category ordinal scale. We used a logistic link function (proportional-odds model) for ordinal variables.
Mediation Models
We used a mediation model to test the hypothesis that the relationship of HIV-related stigma and HIV medication adherence could be explained by depressive symptoms.(27) Such models can help to suggest mechanisms by which one variable may impact another and provide a nuanced understanding of processes that link behavior and health.(28)
Estimation and missing data
We used robust mean- and variance-adjusted weighted least squares estimation (WLSMV), implemented in Mplus 5 to estimate the statistical models. The WLSMV estimator is robust to deviations from model assumptions.(29) WLSMV utilizes a multi-step process that allows the researcher to use all available data, without either imputing values or deleting cases, based on the assumption that, conditional on covariates, the missing data are non-informative and missing completely at random.(29, 30) WLSMV also gives overall fit statistics for model testing. These include a chi square statistic, which tends to be over-sensitive to minor misfit with large sample sizes,(31) as well as some measures that are not sensitive to sample size, including the comparative fit index (CFI), the Tucker-Lewis index (TLI), and the root mean square error of approximation (RMSEA). The CFI and TLI suggest good fit if they are close to or greater than 0.95; the RMSEA suggests adequate fit when it is close to or less than 0.06.(31)
RESULTS
During the study period, 720 participants completed the assessment. Demographic characteristics of these individuals are shown in Table 1. Most participants were male (86%) and just under half were men who have sex with men (48%). The majority of the participants were white (62%), and most were 40 or older (73%). Cronbach’s alpha for the 4 items that made up the stigma construct was 0.84. Overall, 76% of the participants reported experiencing some HIV-related stigma, with slightly higher proportions among certain subgroups including those under age 30 and those with nadir CD4+ cell counts greater than 350 cells/mm3. Only 160 (22%) reported perfect adherence. Participants reported no (49%), mild (25%), moderate (22%), or severe (5%) depressive symptoms. Details on socio-demographic characteristics by level of stigma are listed in Table 1.
Table 1.
Sample Characteristics and Stigma Sum-Score Tertiles
| Participants | Overall Freq. (%) | Stigma Freq. (%) | ||
|---|---|---|---|---|
| Total | None/Mild | Moderate | Severe | |
| 720 (100) | 225 (31) | 261 (36) | 234 (33) | |
| Sex | ||||
| Female | 103 (14) | 26 (12) | 36 (14) | 41 (18) |
| Male | 617 (86) | 199 (88) | 225 (86) | 193 (82) |
| Race | ||||
| White | 447 (62) | 153 (68) | 171 (66) | 123 (53) |
| Black | 147 (20) | 40 (18) | 49 (19) | 58 (25) |
| Other | 126 (18) | 32 (14) | 41 (16) | 53 (23) |
| Transmission risk factor | ||||
| MSM | 344 (48) | 120 (53) | 138 (53) | 86 (37) |
| Injection drug user | 186 (26) | 61 (27) | 50 (19) | 75 (32) |
| Heterosexual | 117 (16) | 32 (14) | 40 (15) | 45 (19) |
| Other or unknown | 73 (10) | 12 (5) | 33 (13) | 28 (12) |
| Recent CD4+ cell count (cells/mm3) | ||||
| ≤200 | 89 (12) | 28 (12) | 31 (12) | 30 (13) |
| 201–350 | 146 (20) | 48 (21) | 46 (18) | 52 (22) |
| ≥351 | 485 (67) | 149 (66) | 184 (70) | 152 (65) |
| Nadir CD4+ Count (cells/mm3) | ||||
| ≥200 | 370 (51) | 131 (58) | 113 (43) | 126 (54) |
| 201–350 | 212 (29) | 59 (26) | 91 (35) | 62 (26) |
| ≥351 | 138 (19) | 35 (16) | 57 (22) | 46 (20) |
| Age (in years) | ||||
| < 30 | 65 (9) | 14 (6) | 30 (11) | 21 (9) |
| 30–39 | 139 (19) | 39 (17) | 52 (20) | 48 (21) |
| 40–49 | 311 (43) | 105 (47) | 111 (43) | 95 (41) |
| 50 or older | 205 (28) | 67 (30) | 68 (26) | 70 (30) |
All statistical models were adjusted for self-reported race/ethnicity, sex, and age. In separate models, we found that poorer HIV medication adherence was associated with higher levels of HIV-related stigma and depressive symptom levels (standardized estimates: β = −0.21, p < 0.01 for HIV-related stigma, β = −0.23, p < 0.01 for depression), and that higher depressive symptom levels were associated with greater HIV-related stigma (β = 0.51, p < 0.01). The interpretation of these standardized coefficients is as follows: every standard deviation difference in HIV-related stigma was associated with a 0.21 standard deviation drop in HIV medication adherence.
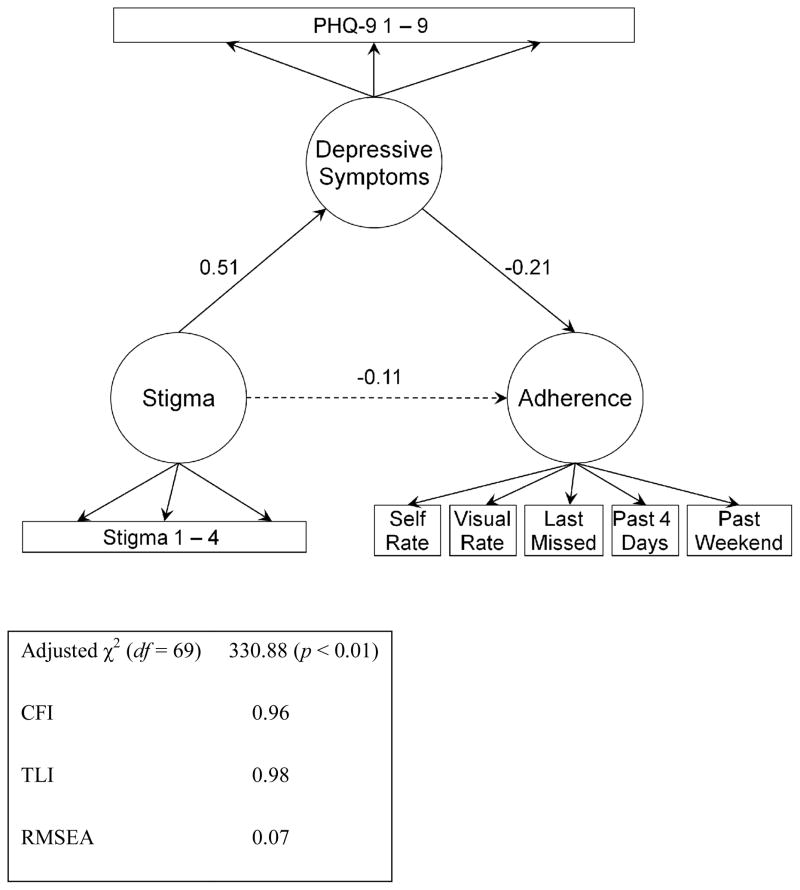
In the final model, we simultaneously estimated coefficients for all three latent variables together, as shown in Figure 1. The final model fit the data well (summarized in Figure 1). Coefficient estimates are shown in Table 2 and Figure 1. In the final model, HIV-related stigma had a strong association with depressive symptoms (standardized β = 0.51, p < 0.01). In turn, depressive symptoms had a moderate effect on HIV medication adherence (standardized β = −0.17, p < 0.01). Furthermore, in the final model, the standardized association between HIV-related stigma and HIV medication adherence (represented by the dotted line in Figure 1) was β = −0.11, p = 0.07. This value is just over half the β of −0.21 we found for the strength of association between HIV-related stigma and HIV medication adherence when depressive symptoms were omitted from the model. These findings suggest that much of the effect of stigma on adherence is mediated by depressive symptoms. In the final model, the total estimated standardized effect of stigma on adherence, including the direct effect and the indirect effect through depression, was −0.19 (p < .01); each standard deviation higher in HIV-related stigma was associated with a 1/5 standard deviation drop in HIV medication adherence.
Figure 1.
Path Diagram
Figure 1 depicts the relationships between latent variables analyzed in the model. The latent variables are depicted as circles and the observed variables (i.e. items) as squares (questionnaire items labeled Depressive symptoms 1–9 and Stigma 1–4). Stigma is associated with depressive symptoms, which in turn is associated with adherence. The path coefficients, which can be interpreted as standardized beta weights in a regression model, are shown next to each arrow. The arrow with the dotted line represents the effect between stigma and adherence that is diminished when depressive symptoms are included in the model, indicating that depressive symptoms partially mediate the relationship between stigma and adherence. Models were adjusted for age, sex, and race.
Table 2.
Parameter Estimates from Final Mediation Model
| Parameter | Coefficient (SE) | Wald | p | Standardized |
|---|---|---|---|---|
| Adherence on | ||||
| Stigma | −0.14 (0.08) | −1.80 | 0.07 | −0.11 |
| Depressive symptoms | −0.22 (0.06) | −3.89 | < 0.01 | −0.21 |
| Age (in years) | < −0.01 (< 0.01) | −0.63 | 0.53 | −0.03 |
| Sex | 0.08 (0.12) | 0.66 | 0.51 | 0.03 |
| Race | −0.23 (0.08) | −2.74 | < 0.01 | −0.13 |
| Depressive symptoms on | ||||
| Stigma | 0.67 (0.05) | 13.34 | < 0.01 | 0.51 |
| Age | < −0.01 (< 0.01) | −0.31 | 0.75 | −0.01 |
| Sex | −0.13 (< 0.10) | −1.30 | 0.19 | −0.05 |
| Race | −0.01 (0.07) | −0.10 | 0.92 | < −0.01 |
DISCUSSION
We found that depressive symptoms partially mediated the relationship between HIV-related stigma and HIV medication adherence. Increased levels of HIV-related stigma were associated with more severe depressive symptoms that, in turn, were associated with poorer HIV medication adherence. These results are consistent with the notion that depressive symptoms may be a mechanism by which HIV-related stigma impacts HIV medication adherence. To our knowledge, these are the first analyses to simultaneously examine HIV-related stigma, depressive symptoms, and HIV medication adherence. Results of this study support our hypothesis that depressive symptoms may play a role in explaining the previously observed relationship between HIV-related stigma and HIV medication adherence.(6, 10)
The findings of this study have important implications. First, poor adherence to antiretroviral medications can be traced to many readily observed factors, such as regimen complexity, desire to avoid unpleasant side effects,(32) substance use,(33) and housing stability.(34) Our results highlight the association between adherence and two interconnected, factors: stigma and depression. Our findings suggest further investigation is warranted to understand interconnected factors associated with adherence, namely, how factors interplay with one another to affect adherence and the combined impact of all these factors on adherence. Optimal medication adherence is necessary for long-term AIDS-free survival among PLWH,(35, 36) and as such, increasing awareness and targeting of factors such as stigma and depression together may ultimately lead to improved outcomes.
Second, these findings suggest a specific mechanism—depressive symptoms—by which stigma may affect adherence. Experiencing and internalizing stigma may exacerbate levels of fatigue, diminished ability to concentrate, or feelings of worthlessness—all symptoms of depression. These factors are necessary components for optimal adherence: one must have good concentration skills to remember when and how to take complex medication regimens, for example. Thus, understanding and addressing stigma may more fully address root causes of depressive symptoms and poor adherence among PLWH. Interventions to reduce HIV-related stigma could impact adverse psychological responses early, before depressive symptoms develop or have an impact on HIV medication adherence.
Understanding these factors and their impact on PLWH’s lived reality offers an opportunity to effectively intervene in potentially adherence-hindering behaviors. Further results, such as those we found here, would suggest specific strategies for intervention (e.g. teaching coping skills and cognitive behavioral techniques, providing social support). Additionally, it may be useful to address internalizations of stigma, which may manifest as PLWH believing that negative stereotypes apply to them (e.g. I am promiscuous), challenging stereotypes, increasing social support, and empowerment techniques. Our results suggest that depression could interact and exacerbate any of these factors as well as having a direct affect on adherence. Therefore, studies that design, implement, and test strategies to alleviate depressive symptoms along with the impact of stigma among PLWH are needed to comprehensively improve adherence.
The strengths of our study include collection of comprehensive clinical data, including routine assessment of HIV-related stigma, depression, and HIV medication adherence in a large clinical cohort of PLWH in clinical care. Furthermore, our study used SEM techniques to analyze item-level data. As such, we were able to examine interconnections between factors impacting HIV medication adherence in one parsimonious statistical model.
The present study was conducted using cross-sectional data. As such, we cannot presume causality in any relationships between variables studied. We are currently collecting longitudinal data that may further illuminate these relationships. Future longitudinal studies may provide more evidence regarding causal associations between HIV-related stigma, depressive symptoms, and HIV medication adherence. In addition, other potential variables, such as social support, could play an important role in HIV medication adherence. Our study was designed to be parsimonious and minimize participant burden, and as such, we could not inquire about several potentially important variables. Similarly, although our study was based on prior research on associations between stigma and depression, other arrangements of the model are certainly feasible. A final limitation is that patients were recruited from a single HIV clinic, and thus findings may not be generalizable to all PLWH, especially those from other ethnic/racial backgrounds or people not in routine care.
In all, we found strong relationships between HIV-related stigma, depressive symptoms, and HIV medication adherence and evidence to suggest that depressive symptoms represent a mechanism by which HIV-related stigma affects poor HIV medication adherence. Further research will explore whether interventions to limit the internalized effects of HIV-related stigma and depressive symptoms improve HIV medication adherence.
Acknowledgments
The present study was funded by National Institutes of Mental Health grant number K23 MH 084551 (PI: Rao) and R01 MH 084759 (PI: H. Crane). Initial results from this study were presented at the 5th International Conference on HIV Treatment Adherence, May 23–25, 2010, Miami, Florida.
References
- 1.Lee RS, Kochman A, Sikkema KJ. Internalized stigma among people living with HIV-AIDS. AIDS and Behavior. 2002 Dec;6(4):309–319. [Google Scholar]
- 2.Rao D, Chen W-T, Pearson C, Simoni J, Fredriksen-Goldsen K, Nelson K, et al. Social Support Mediates the Relationship between HIV Stigma, Depression, and Quality of Life among People Living with HIV in Beijing, China. International Journal of STD & AIDS. doi: 10.1258/ijsa.2009.009428. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Murphy DA, Austin EL, Greenwell L. Correlates of HIV-related stigma among HIV-positive mothers and their uninfected adolescent children. Women Health. 2006;44(3):19–42. doi: 10.1300/J013v44n03_02. [DOI] [PubMed] [Google Scholar]
- 4.Wu DY, Munoz M, Espiritu B, Zeladita J, Sanchez E, Callacna M, et al. Burden of depression among impoverished HIV-positive women in Peru. J Acquir Immune Defic Syndr. 2008;48(4):500–4. doi: 10.1097/QAI.0b013e31817dc3e9. [DOI] [PubMed] [Google Scholar]
- 5.Pulerwitz J, Michaelis AP, Lippman SA, Chinaglia M, Díaz J. HIV-related stigma, service utilization, and status disclosure among truck drivers crossing the Southern borders in Brazil. AIDS Care. 2008;20(7):764–70. doi: 10.1080/09540120701506796. [DOI] [PubMed] [Google Scholar]
- 6.Rao D, Kekwaletswe TC, Hosek S, Martinez J, Rodriguez F. Stigma and Social Barriers to Medication Adherence with Urban Youth Living with HIV. AIDS Care. 2007;19(1):28–33. doi: 10.1080/09540120600652303. [DOI] [PubMed] [Google Scholar]
- 7.Goffman E. Stigma: Notes on the Management of Spoiled Identity. New York: Simon and Schuster Inc; 1963. [Google Scholar]
- 8.Corrigan P, Watson A. The paradox of self-stigma and mental illness. Clinical Psychology: Science and Practice. 2002 Feb;9(1):35–53. [Google Scholar]
- 9.Nyblade LC. Measuring HIV stigma: existing knowledge and gaps. Psychology Health & Medicine. 2006 Aug;11(3):335–45. doi: 10.1080/13548500600595178. [DOI] [PubMed] [Google Scholar]
- 10.Sayles J, Wong M, Kinsler J, Martins D, Cunningham W. The Association of Stigma with Self-Reported Access to Medical Care and Antiretroviral Therapy Adherence in Persons Living with HIV/AIDS. Journal of General Internal Medicine. 2009 doi: 10.1007/s11606-009-1068-8. epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Singh N, Squier C, Sivek C, Wagener M, Nguyen MH, Yu VL. Determinants of compliance with antiretroviral therapy in patients with human immunodeficiency virus: prospective assessment with implications for enhancing compliance. AIDS Care. 1996;8(3):261–9. doi: 10.1080/09540129650125696. [DOI] [PubMed] [Google Scholar]
- 12.Gordillo V, del Amo J, Soriano V, GonzÃ!lez-Lahoz J. Sociodemographic and psychological variables influencing adherence to antiretroviral therapy. AIDS. 1999;13(13):1763–9. doi: 10.1097/00002030-199909100-00021. [DOI] [PubMed] [Google Scholar]
- 13.Bing EG, Burnam MA, Longshore D, Fleishman JA, Sherbourne CD, London AS, et al. Psychiatric disorders and drug use among human immunodeficiency virus-infected adults in the United States. Arch Gen Psychiatry. 2001;58(8):721–8. doi: 10.1001/archpsyc.58.8.721. [DOI] [PubMed] [Google Scholar]
- 14.Valente SM. Depression and HIV disease. J Assoc Nurses AIDS Care. 2003;14(2):41–51. doi: 10.1177/1055329002250993. [DOI] [PubMed] [Google Scholar]
- 15.Catz SL, Kelly JA, Bogart LM, Benotsch EG, McAuliffe TL. Patterns, correlates, and barriers to medication adherence among persons prescribed new treatments for HIV disease. Health Psychol. 2000;19(2):124–33. [PubMed] [Google Scholar]
- 16.Rao D, Simoni J, Nelson K, Chen W, Zhao H, Zhang F. Depressive symptoms predict adherence to ART in people living with HIV in Beijing, China. 5th International Conference on HIV Treatment Adherence; May 23–25, 2010; Miami, Florida2010. [Google Scholar]
- 17.Crane H, Lober W, Webster E, Harrington R, Crane P, Davis T, et al. Routine collection of patient-reported outcomes in an HIV clinic setting: the first 100 patients. Current HIV Research. 2007;5:109–18. doi: 10.2174/157016207779316369. [DOI] [PubMed] [Google Scholar]
- 18.Rao D, Choi S, Victorson D, Bode R, Heinemann A, Peterman A, et al. Measuring Stigma Across Neurological Conditions: The Development of the Stigma Scale for Chronic Illness (SSCI) Quality of Life Research. 2009;18:585–95. doi: 10.1007/s11136-009-9475-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. Journal Of General Internal Medicine. 2001;16(9):606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA: The Journal Of The American Medical Association. 1999;282(18):1737–44. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 21.Kroenke K, Spitzer R, Williams J. The Patient Health Questionnaire-2: validity of a two-item depression screener. Medical Care. 2003;41(11):1284–92. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 22.Chesney M, Ickovics J, Chambers D, Gifford A, Neidig J, Zwickl B, et al. Self-reported adherence to antiretroviral medications among participants in HIV clinical trials: the AACTG Adherence Instruments. AIDS Care. 2000;12(3):255–66. doi: 10.1080/09540120050042891. [DOI] [PubMed] [Google Scholar]
- 23.Simoni J, Kurth A, Pearson C, Pantalone D, Merrill J, Frick P. Self-report measures of antiretroviral therapy adherence: a review with recommendations for HIV research and clinical management. AIDS and Behavior. 2006;10:227–245. doi: 10.1007/s10461-006-9078-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lu M, Safren S, Skolnik P, Rogers W, Coady W, Hardy H, et al. Optimal recall period and response task for self-reported HIV medication adherence. AIDS and Behavior. 2008;12:86–94. doi: 10.1007/s10461-007-9261-4. [DOI] [PubMed] [Google Scholar]
- 25.Amico K, Fisher W, Cornman D, Shuper P, Redding C, Konkle-Parker D, et al. Visual analog scale of ART adherence: association with 3-day self-report and adherence barriers. J Acquir Immune Defic Syndr. 2006;42:455–9. doi: 10.1097/01.qai.0000225020.73760.c2. [DOI] [PubMed] [Google Scholar]
- 26.Skrondal A, Rabe-Hesketh S. Generalized linear latent and mixed models with composite links and exploded likelihoods. In: Biggeri A, Dreassi E, Lagazio C, Marchi M, editors. Statistical Modelling. Firenze: Firenze University Press; 2004. pp. 27–39. [Google Scholar]
- 27.MacKinnon DP, Fairchild AJ, Fritz MS. Mediation Analysis. Annual Review of Psychology. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Structural equations with latent variables, (1989).
- 29.Muthén LK, Muthén BO. Mplus User’s Guide. 6. Los Angeles, CA: Muthén & Muthén;; pp. 1998–2010. [Google Scholar]
- 30.Little RJA. Modeling the drop-out mechanism in repeated-measures studies. Journal of the American Statistical Association. 1995;90(431):1112–21. [Google Scholar]
- 31.Hu L, Bentler P. Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological methods. 1998;3:424–53. [Google Scholar]
- 32.Glass TR, Battegay M, Cavassini M, De Geest S, Furrer H, Vernazza PL, et al. Longitudinal Analysis of Patterns and Predictors of Changes in Self-Reported Adherence to Antiretroviral Therapy: Swiss HIV Cohort Study. J Acquir Immune Defic Syndr. 2009 Dec 23; doi: 10.1097/QAI.0b013e3181ca48bf. [DOI] [PubMed] [Google Scholar]
- 33.Golin CE, Liu H, Hays RD, Miller LG, Beck CK, Ickovics J, et al. A prospective study of predictors of adherence to combination antiretroviral medication. J Gen Intern Med. 2002 Oct;17(10):756–65. doi: 10.1046/j.1525-1497.2002.11214.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kidder D, Wolitski R, Campsmith M, Nakamura G. Health status, health care use, medication use, and medication adherence among homeless and housed people living with HIV/AIDS. Am J Public Health. 2007;97(12):2238–45. doi: 10.2105/AJPH.2006.090209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Singh N, Berman SM, Swindells S, Justis JC, Mohr JA, Squier C, et al. Adherence of human immunodeficiency virus-infected patients to antiretroviral therapy. Clin Infect Dis. 1999 Oct;29(4):824–30. doi: 10.1086/520443. [DOI] [PubMed] [Google Scholar]
- 36.Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squier C, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med. 2000;133(1):21–30. doi: 10.7326/0003-4819-133-1-200007040-00004. [DOI] [PubMed] [Google Scholar]