Abstract
Objective
We examined whether individual-level social capital--the intangible resources in a community available through membership in social networks or other social structures and perceived trust in the community—was associated with acculturation; depression and anxiety symptoms; and perceived access to services among women of Mexican ancestry.
Method
Recruited through venue-based targeted sampling in King County, WA, 205 women of Mexican descent age 18 to 64 years who differed in socioeconomic status and nativity completed a cross-sectional survey. Half completed the survey in Spanish and half in English. Structural equation modeling was used for model testing.
Results
Social capital increased with level of acculturation and was negatively related to depression and anxiety; it had no direct association with perceived access to services. Social capital mediated the relation between acculturation and both depression and anxiety symptoms. Acculturation had no direct association with psychological distress but was directly associated with perceived access to services. This community sample of women reported high levels of psychological distress, with 20–26% of women meeting diagnostic criteria for depression or anxiety.
Conclusions
Social capital can be assessed at the individual level, increases with acculturation, and may be a potential target for interventions to improve mental health among Mexican American women residing in the U.S.
Keywords: social capital, depression, anxiety, Mexican American women, acculturation, perceived access to services, structural equation modeling
Introduction
Latinos constitute 15% of the total population in the United States (U.S.) and are one of the fastest growing racial/ethnic groups in the country; by the year 2050, Latinos will constitute approximately 25% of the total U.S. population (Pew Hispanic Center, 2010). Latinos in the U.S. hail from 43 Spanish-speaking countries, with most (67%) of Mexican origin (Pew Hispanic Center, 2010). Latinos face multiple social and economic risks that may negatively impact their mental health and access to care, including low education levels, residence in poor neighborhoods, language barriers, lack of or inadequate health care, poverty, isolation, discrimination, and segregation (Carter-Pokras & Zambrana, 2001). Research specifically focusing on Mexican Americans has documented greater language and cultural barriers, poverty, high school drop-out rates, lack of college achievement (Zambrana & Zoppi, 2002), and teenage pregnancy compared to the general U.S. population and to other Latino subgroups (Kaiser Family Foundation, 2004). Of all the racial/ethnic groups in the U.S., Latinos are the most likely to be uninsured and the least likely to use health care services for preventive care (Carter-Pokras & Zambrana, 2001). Indeed, Latinos are at greater risk than the general U.S. population of experiencing cultural barriers when interacting with the health care system (Kaiser Family Foundation, 2004; Zambrana & Zoppi, 2002), and their mental health problems are more likely to be addressed by a physician than a mental healthcare provider (Vega & Alegría, 2001).
Among Latinos, women, compared to men, are especially vulnerable to adverse mental health outcomes. Latinas are at greater risk for and experience higher rates of anxiety and depression (Elder, Broyles, Brenna, et al., 2005; Gonzalez, Haan, & Hinton, 2001). Being an ethnic minority woman in the U.S. and having limited income are salient factors in the lives of many Latinas, who may live with few or fragile resources as well as face ethnic and immigrant-related structural barriers (Carter-Pokras & Zambrana, 2001). These risk factors may be associated with worse mental health outcomes and barriers to services among Mexican American women.
Social capital may be a resource through which mental health and service use outcomes may be improved among Mexican American women despite the socioeconomic and institutional barriers they face. The construct of social capital refers to the intangible resources in a community available through membership in social networks or other social structures (Granovetter, 1973; Putnam, 2000). Like other forms of capital (i.e., human, financial, physical), social capital is productive, providing material benefits to individuals who are connected to other individuals and groups (Bourdieu, 1986; Coleman, 1990; Putnam, 1993). Communities characterized by high levels of social capital are likely to have higher educational achievement, better performing public institutions, faster economic growth, and less crime and violence (Putnam, 2000). Social capital may influence these outcomes through improved social networks and relationships which serve to accommodate and facilitate the exchange of material goods, services, information, and money as well as less tangible support such as mutual assistance and emotional support (Baum & Ziersch, 2003; Granovetter, 1973; Kawachi & Berkman, 2001).
The relation between social capital and mental health in Mexican American populations may be influenced by factors that have not yet been identified, given the different social, economic, cultural and political environments of Latinos compared to White Americans (Almedon, 2005; Segura et al., 2001). The present study examined the construct of social capital and its association with acculturation, psychological distress (depression and anxiety symptoms) and perceived access to mental health services among women of Mexican ancestry. Social capital, shown to have positive health effects (Putnam, 2000), may help explain how acculturation is associated with mental health outcomes among Latinos.
Acculturation is the multidimensional process of change in behaviors, attitudes, and beliefs in both a newly arrived group and the dominant culture with which it interacts (Berry, 2003; Schwartz, Unger, Zamboanga, & Szapocznik, 2010). While some studies have found that acculturation has a negative impact on Latino’s mental health (Alegría et al., 2007; Vega et al., 1998); others have found partial or no effects of acculturation on health (Abraido-Lanza et al., 2005).
Although there is much literature examining the direct relation between acculturation and mental health as well as studies on social capital and mental health, we did not find any studies examining the relations among social capital, acculturation, and mental health. Social capital’s cognitive aspects, which are the focus of this paper, include people’s attitudes and beliefs about norms, values, interpersonal trust, and sense of belonging (Fujiwara & Kawachi, 2008; Kawachi & Berkman, 2000). Fujiwara and Kawachi (2008) found that individuals with higher levels of cognitive social capital were at lower risk of developing major depression. Some researchers have further suggested that increasing social capital and community involvement may be a way to decrease inequalities related to race/ethnicity, income, gender, and geographic location (Cheadle, Wagner, Walls, et al., 2001). Additionally, social capital may be a way to increase service use in ethnic minority populations by addressing issues of trust in healthcare providers and promoting a sense of community belonging.
In the present study, we surveyed a community sample of 205 women of Mexican ancestry living in the Northwest. We hypothesized that women with higher levels of social capital would report better mental health (lower depression and anxiety symptoms) and would also perceive greater access to services in their community. We sought to examine whether social capital would mediate the relationship between acculturation and psychological distress (depression and anxiety symptoms) in this population.
Method
Procedures
Venue-based targeted sampling (Lemp, Jones, Kellogg, & Nieri, 1995) was used to recruit a non-clinical community sample. Members of a Community Advisory Board as well as focus group participants from an earlier, qualitative phase of the study assisted study personnel in identifying appropriate venues. We selected venues that would allow us to target women with a range of incomes, educational levels, and employment backgrounds (e.g., health fairs, community centers, colleges and universities, beauty salons, banks, and Latino-identified stores). Additionally, we identified several Latino-oriented e-mail listservs. Study personnel contacted shop owners, managers, and listserv coordinators to assess the appropriateness of the site (e.g., Latino density) and elicit cooperation. Afterwards, study fliers were posted on-site and information sent to the listservs. The flyers invited women of Mexican ancestry to participate in a study regarding community issues and health among women; they mentioned the monetary incentive, described eligibility criteria, and instructed interested women to call or e-mail the study office.
Women who were recruited in-person at targeted events were given a study flier and if interested were given the option to be screened at that moment or to call or e-mail the study office at their convenience. All screening and recruitment was done by the principal investigator or Latina undergraduate research assistants in Spanish or English (based on the participants’ choice). Eligibility criteria were: woman of Mexican origin (i.e., they themselves or their ancestors originated from Mexico); 18 years of age or older; able to read either English or Spanish; and resided in the area of King County, Washington. In recruitment, a pseudo-quota technique was employed to ensure representation with respect to Spanish or English language preference, U.S. or foreign nativity, income, and length of time in the U.S. The majority (64%) of participants completed the survey at a community location; 36% completed the survey at a university campus. Survey completion time ranged from 25 to 60 minutes, and women were offered $20 for their participation.
Measures
Selected measures were used from the National Latino and Asian American Survey (NLAAS; Alegría, Takeuchi, Canino et al., 2004) based on validity, reliability, and availability of Spanish/English versions. NLAAS is a large, comprehensive study that examined psychiatric disorders with soci-culturally appropriate measures among a nationally representative sample of Latinos and Asians residing in the U.S. The NLAAS provides national information on the similarities and differences in mental illness and service use of Latinos and Asian Americans (Alegría, Takeuchi, Canino et al., 2004). Other survey measures available only in English were translated by three bilingual research staff using back translation to ensure linguistic and cultural equivalency (Marín & Marín, 1991) and were pre-tested with members of the community advisory board. Only measures that were used in the SEM analysis are described in this paper.
Demographic information collected included date of birth, nativity, age of migration to the U.S., and employment status. Generational status was based on birthplace of both the participant and her parents/grandparents (Cuéllar, Arnold, & Maldonado, 1995). Level of education was measured by the highest level of education completed in the U.S. or equivalent elsewhere. Household income was defined as income (before taxes) from all family members from all sources in a typical month.
Acculturation was assessed with three factors: length of time in the U.S., language preference, and voter registration. Language preference was measured with 3 items assessing preferred language when speaking with friends, family, and when thinking (Félix-Ortiz, Newcomb, & Meyers, 1994). Responses were based on a 5-point likert-type scale and ranged from 1 (Spanish all of the time) to 5 (English all of the time). Current sample α = .91. Voter registration was assessed by the question, “Are you currently registered to vote?” Responses were coded as 0 (not eligible to vote), 1 (no), or 2 (yes). Participants were then divided into one of three acculturation categories based on the work of Vega et al. (1998): U.S. born, born in Mexico and living in the U.S. for less than 13 years, or born in Mexico and living in the U.S. for greater than 13 years.
Social capital was assessed with two measures of trust and one measure of volunteerism. The first measure of trust (Neighborhood Trust) was based on 3 dichotomous items from Kawachi et al., (1997), which were adapted into an 8-item scale with likert-type responses. The revised scale required participants to rate from 1(strongly disagree) to 4 (strongly agree) items such as “In my neighborhood, most people try to be helpful” or “If people in my neighborhood had the opportunity, most people would try to take advantage of me.” Current sample α =.75. The second trust measure (Trust in People) involved having respondents rate from 1 (never have contact with them) to 5 (trust people a lot) how much they trusted different groups of people in their community (e.g., “most people in your neighborhood,” “doctors or nurses”); it was adapted from the Tomas Rivera Policy Institute, Social Capital Survey, 1997. Current sample α =.80. Volunteering was assessed with one item: “In the past year, how much time have you volunteered in any groups or organizations?” (also adapted from the Tomas Rivera Policy Institute, Social Capital Survey, 1997). Possible responses ranged from 1 (none) to 4 (a lot).
Depression was assessed with the Patient Health Questionnaire (PHQ9; Spitzer et al., 1999), items from the Kessler Psychological Distress Scale (K-10; Kessler & Mroczek, 1994), and Major Depressive Disorder (MDD) questions from the Composite International Diagnostic Interview, Short Form (CIDI-SF, World Health Organization, 1998). Using the PHQ9, participants were asked, “In the last 2 weeks, how often have you been bothered by any of the following problems?” They then rated 9 depressive symptoms using a likert-type scale ranging from 0 (not at all) to 3 (nearly every day). Current sample α=.91. Six of the 10 items of the K-10 scale were used to assess depressive symptoms. Participants were asked to indicate, during the last 30 days, how often they felt “tired for no good reason, hopeless, depressed, so depressed that nothing could cheer you up, that everything was an effort, worthless.” The likert-type scale ranged from 1 (none of the time) to 5 (all of the time). Current sample α = .92. For MDD, participants were asked a series of questions based on DSM-IV criteria and received either a 0 (did not meet diagnostic criteria) or 1 (met diagnostic criteria) based on responses (see CIDI-SF, Nelson et al., 1998 for detailed scoring guidelines).
Anxiety was measured using questions from the CIDI-SF Generalized Anxiety Disorder section and participants received a 0 (did not meet diagnostic criteria) or 1 (met diagnostic criteria) (see CIDI-SF, Nelson et al., 1998 for detailed scoring guidelines). Ataque de nervios, a common culture-bound syndrome found in many Latin American countries was assessed using a 15-item scale (per NLAAS). Participants who endorsed a stem question of ever having an episode or nervous attack were asked to indicate whether or not they felt any of the 15 symptoms during an episode (e.g., shout a lot, become hysterical, have a period of amnesia, break things or become aggressive). Participants were categorized as either 0 (did not meet diagnostic criteria) or 1(met diagnostic criteria) based on symptom cut-off score criteria (see Guarnaccia, Lewis- Fernandez, Martinez et al., 2010). Current sample α = .65. Four of the 10 items of the K-10 scale were used to assess for anxiety symptoms. Participants were asked to indicate, during the last 30 days, how often they felt nervous, so nervous that nothing could calm them down, restless of fidgety, and so restless that they could not sit still. The likert-type scale ranged from 1 (none of the time) to 5 (all of the time). Current sample α =.88.
Perceived access to services was assessed with two items and a service use barrier scale. The first yes/no item assessed whether participants had current health insurance coverage. The second question assessed how much they agreed with the following statement: “In general, there are adequate services in my community to assist me with problems with my emotions or nerves” (see NLAAS). Response items ranged from 1 (strongly disagree) to 4 (strongly agree). A 22-item scale was employed to measure perceived barriers to service use (per NLAAS). Participants were asked to indicate whether each item was a barrier to service use by answering yes/no; items included “I was unsure about where to go or who to see” and “There was no Spanish speaking provider within my area.” The “no” responses were summed, with higher scores indicated more access to services. Current sample α = .88.
Statistical Analysis
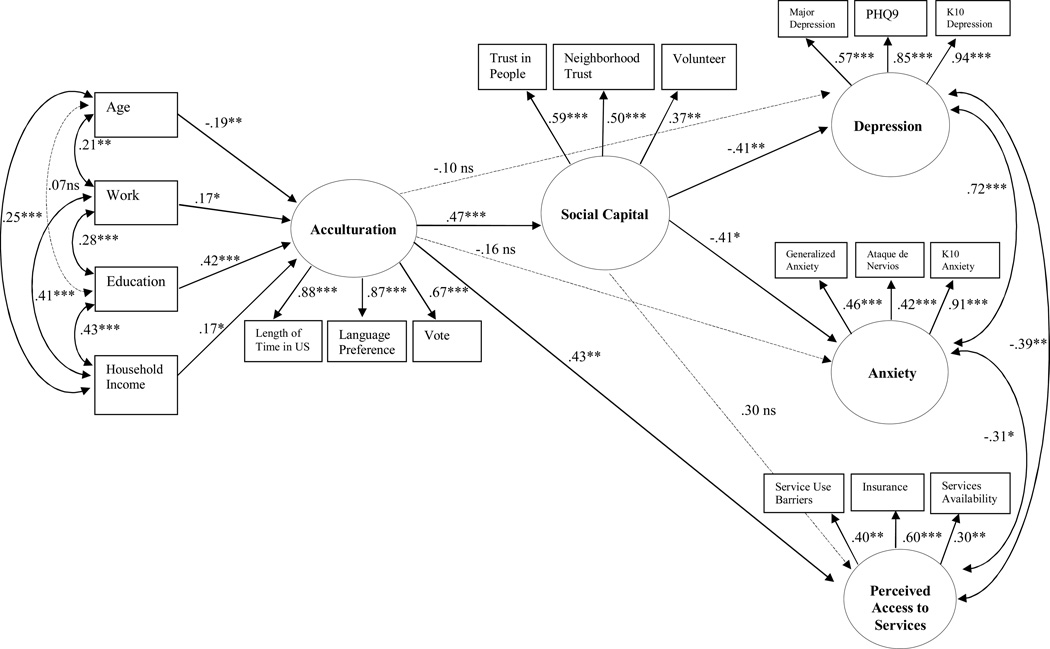
A confirmatory factor analysis (CFA) and structural equation modeling (SEM) analyses were used for model testing. SEM is theory driven and uses multiple measures for each latent construct to reduce measurement error in individual indicators, which increases the accuracy of the results (Kline, 2005). Given our a priori model, confirmatory SEM analysis assisted with model fit. A CFA was conducted first on five latent variables: acculturation, social capital, depression, anxiety, and perceived access to services to confirm and test the measurement of the theoretical constructs. In order to obtain a well fitting parsimonious model, only variables with significant factor loadings were retained in the final CFA for the five latent constructs (see Figure 1). Second, SEM was employed to test specific hypothesized directional relations among the latent constructs for overall model fit. While several good fitting models were run, the most parsimonious model using our specified indicators was used as the final model. A sample size of 200 was determined as sufficient to detect the relatively conservative estimates using SEM (Bollen, 1989; Kline, 2005).
Figure 1. Results of the Structural Equation Model.
A structural equation model of four latent constructs. Household Income = Monthly household income; Vote = Currently registered to vote; PHQ9= Patient Health Questionnaire for Depression; K-10 Depression = Kessler Psychological Distress Scale, Depression items; K-10 Anxiety = Kessler Psychological Distress Scale, Anxiety items; Services Availability = Perceived availability to mental health services in the community. *p < .05. **p < .01. *** p < .001.
Given that the standard chi-square statistic has been discussed as a nonsufficient guide to model fit (see Kline, 2005), the present model was assessed using various model fit indices recommended by Hu and Bentler (1998; 1999) for Maximum Likelihood (ML) based models including Tucker-Lewis Index (TLI) values close to or greater than .95, Comparative Fit Index (CFI) values close to or greater than .95, Standardized Root Mean Square Residuals (SRMR) values close to .08, and Root Mean Square Error of Approximation (RMSEA) less than or equal to .06.
Results
Participants
A total of 356 women were either recruited in person or contacted the study (via phone or e-mail) about their interest in participation. Seventeen women who contacted the study were not able to be reached for screening. Of the 339 women who were screened, 30 (9%) were ineligible because they were not of Mexican ancestry. Of the 309 (91%) who were screened and found to be eligible, 205 (66%) completed the paper-pencil survey (the other 104 (34%) could not be re-contacted or scheduled). We found no significant differences based on age or language preference of survey between those who completed the survey and those who did not.
As seen in Table 1, the final sample consisted of 205 women of Mexican ancestry between the ages of 18 to 64 years (M = 31.42, SD = 10.83). They self-identified as Mexican/Mexicana (46%), Latina (24%), Mexican American (15%), Hispanic (8%), Chicana (7%), American (1%) and other (1%). Language preference was evenly divided, with 103 women choosing to complete the survey in Spanish and 102 in English. Fifty-two percent of women indicated that they were not a legal U.S. resident, 39.5% indicated that they were, and 8% refused to answer the question.
Table 1.
Participant Demographic Characteristics Stratified by Language (N = 205)
| Variable | English (n = 102) | Spanish (n = 103) | ||
|---|---|---|---|---|
| n | % | n | % | |
| Currently in a primary relationship | ||||
| Yes | 65 | 64 | 70 | 68 |
| No | 37 | 36 | 33 | 32 |
| Generation in the U.S.*** | ||||
| First (Born in Mex.) | 27 | 27 | 97 | 94 |
| Second (U.S. Born, either parent born in Mex.) | 52 | 51 | 5 | 5 |
| Third and beyond (U.S. Born, both parents or grandparents born in U.S.) | 23 | 23 | 1 | 1 |
| Poverty Threshold *** | ||||
| Met | 34 | 33 | 65 | 63 |
| Not Met | 68 | 67 | 38 | 37 |
| Employment ** | ||||
| Working (FT/PT) | 67 | 66 | 47 | 46 |
| No Paid Employed | 35 | 34 | 56 | 54 |
| Education Level *** | ||||
| Less than high school | 5 | 5 | 48 | 47 |
| High school | 16 | 16 | 19 | 18 |
| Some college or more | 81 | 80 | 36 | 35 |
| Religious Preference | ||||
| Catholic | 61 | 69 | 78 | 80 |
| Other Religion | 11 | 12 | 11 | 11 |
| No Religion | 17 | 19 | 8 | 8 |
| Political Affiliation *** | ||||
| Democrat | 73 | 71 | 32 | 31 |
| Republican | 8 | 8 | 1 | 1 |
| Independent | 2 | 2 | 7 | 7 |
| No Preference | 16 | 16 | 60 | 58 |
| Other | 3 | 3 | 3 | 3 |
| Mean | SD | Mean | SD | |
| Age *** | 28.22 | 10.71 | 34.24 | 9.69 |
| Age at Migration for First Generation *** | 5.85 | 4.77 | 23.40 | 9.09 |
Note.
p < .05.
p < .01.
p < .001.
There were several important socio-demographics differences by language of survey completion (see Table 1). Specifically, compared to women who completed the survey in Spanish, those who completed it in English were more likely to have paid employment, had higher household incomes, were more educated, were less likely to meet poverty criteria (based on income and family size), and were younger. As expected, of the non-U.S. born women, those who completed the survey in English had a significantly younger age of migration (M=5.85 vs. M=23.40) than those who completed the survey in Spanish.
Descriptive Findings
As seen in Table 2, respondents varied in length of time in the U.S.; half of the sample was registered to vote in U.S. elections. The majority (62%) of participants indicated some form of health insurance coverage. Participants generally perceived that there were available services in their community to assist them with mental health needs, and barriers to seeking help appeared moderately low (see Table 2).
Table 2.
Descriptive Statistics for Latent Variable Indicators
| Continuous Measures | M | SD | Range |
|---|---|---|---|
| Language Preference | 7.55 | 3.8 | 3 – 15 |
| Trust in People | 39.89 | 7.38 | 11 – 55 |
| Neighborhood Trust | 22.65 | 4.52 | 8 – 32 |
| Volunteer | 2.42 | 1.16 | 1 – 4 |
| PHQ9 - Depression Scale | 5.92 | 5.70 | 0 – 27 |
| K10 - Depression Subscale | 11.18 | 5.36 | 6 – 30 |
| K10 - Anxiety Subscale | 7.51 | 3.34 | 4 – 20 |
| Service Use Barriers | 15.88 | 4.87 | 0 – 22 |
| Perceived Availability of Services | 2.76 | .79 | 1 – 4 |
| Dichotomized Measures | N | % | |
| Major Depression Disorder | |||
| Caseness Met | 40 | 20 | |
| Caseness Not Met | 165 | 80 | |
| Generalized Anxiety Disorder | |||
| Caseness Met | 53 | 26 | |
| Caseness Not Met | 152 | 74 | |
| Ataque de nervios | |||
| Criteria Met | 43 | 21 | |
| Criteria Not Met | 162 | 79 | |
| Insurance Coverage | |||
| Current Coverage | 127 | 62 | |
| No Current Coverage | 78 | 38 | |
| Categorical Measures | N | % | |
| Time in the U.S. | |||
| U.S. Born | 81 | 39.5 | |
| Mexico Born, In U.S. < 13 years | 69 | 34 | |
| Mexico Born, In U.S. > 13 years | 55 | 27 | |
| Registered to Vote | |||
| Registered | 103 | 50 | |
| Not Registered | 70 | 34 | |
| Not Eligible | 32 | 16 | |
Note.
p < .05.
p < .01.
p < .001.
Dichotomized measures of depression and anxiety indicated that 20–26% of participants met diagnostic criteria for these disorders according to standard cut-offs. Specifically, 53 (26%) of participants met diagnostic criteria for GAD, 40 (24%) for MDD, and 19 (9%) for moderate to severe depression based on the PHQ-9. Additionally, 80 (39%) of the sample met the cut-off criteria for the K-10 scale on psychological distress, and 43 (21%) met criteria for ataque de nervios.
Model Testing
CFA analysis yielded three significant indicators per latent variable (see Table 3 for correlations of the measured variables in the model). All 3 indicators had significant loadings (p < .01) on the respective latent variable with coefficients ranging from .30 to .94 (see Figure 1). Acculturation was measured by 3 factors including length of time in the U.S. (.88, p < .001), language preference (.87, p < .001) and voter registration (.67, p < .001). Social capital was measured by trust in people (.59, p < .001), neighborhood trust (.50, p < .001), and volunteering (.37, p < .01). Depression was measured with MDD (.57, p < .001), the PHQ-9 (.85, p < .001), and the K-10 depression items (.94, p < .001). Anxiety was measured with 3 scales, GAD (.46, p < .001), ataque de nervios (.42, p < .001), and K-10 anxiety items (.91, p < .001). Last, perceived access to services latent variable was measured by 3 factors including barriers to service use (.40, p < .01), insurance coverage (.60, p < .001), and perceived availability of services in the community (.30, p < .01).
Table 3.
Correlations of Measured Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| 1. Age | --- | ||||||||
| 2. Work | .21** | --- | |||||||
| 3. Education | .07 | .28*** | --- | ||||||
| 4. Household Income | .25*** | .41*** | .43*** | --- | |||||
| 5. US Time | −.07 | .26*** | .45*** | .27*** | --- | ||||
| 6. Language Preference | −.13 | .30*** | .47*** | .34*** | .77*** | --- | |||
| 7. Vote | .00 | .17* | .39*** | .31*** | .61*** | .55*** | --- | ||
| 8. Trust in People | .01 | .04 | .17* | .13 | .23*** | .23*** | .23*** | --- | |
| 9. Neighborhood Trust | .18* | .22** | .21** | .29*** | .18* | .21** | .22*** | .29*** | --- |
| 10. Volunteer | −.10 | .08 | .12 | .09 | .14* | .13 | .08 | .28*** | .12 |
| 11. MDD | .02 | −.06 | .03 | −.16* | −.06 | −.02 | −.15* | −.17* | −.06 |
| 12. PHQ- Depression | −.01 | −.18* | −.17* | −.31*** | −.13 | −.16* | −.26*** | −.17* | −.25*** |
| 13. K-10 Depression | −.03 | −.19* | −.15* | −.30*** | −.24*** | −.25*** | −.27*** | −.23*** | −.27*** |
| 14. GAD | .17* | .01 | .12 | −.06 | −.00 | −.01 | −.17* | −.18* | −.11 |
| 15. ADN | .04 | −.05 | −.03 | −.12 | −.04 | .00 | −.15* | −.11 | −.21* |
| 16. K-10 Anxiety | −.05 | −.13 | −.17* | −.28*** | −.30*** | −.28*** | −.28*** | −.22*** | −.25*** |
| 17. Service Use Barriers | .09 | .02 | .03 | .21** | .13 | .11 | .16* | .13 | .21** |
| 18. Insurance | .10 | .31*** | .25*** | .28*** | .36*** | .37*** | .36*** | .12 | .16* |
| 19. Services Availability | .23*** | .10 | −.01 | .06 | .06 | .04 | −.01 | .09 | .10 |
| Variable | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 |
|---|---|---|---|---|---|---|---|---|---|
| 10. Volunteer | --- | ||||||||
| 11. MDD | −.04 | --- | |||||||
| 12. PHQ - Depression | −.10 | .50*** | --- | ||||||
| 13. K-10 Depression | −.15* | .53*** | .80*** | --- | |||||
| 14. GAD | −.14* | .30*** | .39*** | .39*** | --- | ||||
| 15. ADN | −.10 | .29*** | .37*** | .38*** | .24*** | --- | |||
| 16. K-10 Anxiety | −.15* | .48*** | .72*** | .81*** | .42*** | .37*** | --- | ||
| 17. Service Use Barriers | .03 | −.21** | −.32*** | −.34*** | −.23*** | −.88** | −.29*** | --- | |
| 18. Insurance | .17* | −.17* | −.29*** | −.32*** | −.11 | −.11 | −.30*** | .17* | --- |
| 19. Services Availability | .03 | −.13 | −.15* | −.19** | −.09 | −.02 | −.17* | .18** | .26*** |
Note. U.S. Time = Length of time in the U.S.; Vote = Currently registered to vote; MDD = Major Depression Disorder; PHQ-Depression= Patient Health Questionnaire for Depression; K-10 Depression = Kessler Psychological Distress Scale, Depression items; GAD = Generalized Anxiety Disorder; ADN = Ataque de nervios; K-10 Anxiety = Kessler Psychological Distress Scale, Anxiety items; Services Available = Perceived access to mental health services in the community.
p < .05.
p < .01.
p < .001
Of particular interest, during SEM analysis the indicator “vote” (assessing voter registration) which was originally theorized to load on the social capital latent construct was moved as an indicator to the acculturation latent construct with a factor loading of .67. This decision was first made based on statistical findings using the values from the modification indices of the CFA data, changes to the chi-square value, as well as the correlation matrix outcomes. While we did not initially propose to measure voting registration as an indicator of acculturation, theoretically, it fits. Correlation coefficients (see Table 3) also indicate significant correlations (p < .05) between the variable “vote” and the two other acculturation indicators (U.S. Time and Language Preference; r = .61 and r = .55, respectively) and weaker associations between “vote” and the Social Capital indicators (Trust in People, Neighborhood Trust, and Volunteer; r = .23, r = .22, r = .08, respectively). Furthermore, the final model accounted for 22% of the variance in the social capital items, 36% of the variance in the acculturation items, 22% of the variance in the depression items, 25% of the variance in the anxiety items, and 40% of the variance in the perceived access to service items.
The final model solution (Figure 1) included standardizing coefficients for all significant paths and indicated that the five latent factors were measured adequately by their respective indicators with high factor loadings. The five indices used for overall model fit indicated that the model fit the data well. The chi-square value was within the acceptable range [χ2 (136, N = 205) = 208.90]. The CFI (.94) and TLI (.92) values were close to the benchmark criteria of .95. RMSEA (.05, 90% CI .04 to .06) and SRMR (.07) were within the range of good fit.
Acculturation was a main component in the model with 4 direct significant paths which were all positive except for age (see Figure 1). Higher acculturation scores were associated with younger age (β = −.19, p < .01), being employed (β = .17, p < .05), higher levels of education (β = .42, p < .001), and higher household incomes (β = .17, p < .05). There was a positive and significant path from acculturation to social capital (β = .47, p < .001) and to perceived access to services (β = .43, p < .001) but not to depression (β = −.10, p > .05) or anxiety (β = −.16, p > .05). Social capital, in turn, was associated with a decrease in depression (β = −.41, p < .01) and anxiety (β = −.41, p < .05) symptoms but not with perceived access to services (β = .30, p > .05). As expected, the model results showed that social capital mediated the relation between socio-demographic factors/acculturation and the outcomes of both depression and anxiety symptoms as well as perceived access to services.
Discussion
In this study of 205 women of Mexican descent living the in U.S. Northwest, we found that social capital increased along with acculturation and that greater social capital was associated with fewer depression and anxiety symptoms. Structural equation modeling confirmed our a priori assumption that social capital would mediate the relation between acculturation and psychological distress (depression and anxiety symptoms). However, our assumption that it would mediate the relation between acculturation and perceived access to services was not supported. To our knowledge, this is the first study to examine the relations among these latent variables, using social capital as a mediator, and testing associations with depression and anxiety, and perceived access to services. The study findings highlight the importance of social capital in mediating the relation between acculturation and psychological distress suggesting that social capital may have a significant impact on individual-level factors that influence this outcome.
Putnam (2000) may have been correct in suggesting that social capital may indeed improve health. He refers to social capital as the “social glue” that holds communities together and argues that countries, regions or communities with greater social capital are better positioned to take advantage of economic and social opportunities. Accordingly, the study results indicated that greater social capital was associated with better mental health outcomes, but not with better perceived access to services. Higher levels of social capital in the more acculturated women in our sample may have protective qualities for mental illness in this population that we have not yet thoroughly explored. This study examined cognitive elements of social capital and therefore the nonsignificant relation found between social capital and perceived access to services in this study may be a function of the measures. Future studies should examine structural elements of social capital and their impact on perceived access to services.
In line with previous studies (Hu & Covell, 1986; Wells et al., 1989), our results indicated that the more acculturated women had higher perceived access to services. Women with higher incomes, higher education, who have paid employment, may indeed have more perceived access to services (perceive and have less barriers) and have higher rates of insurance. The final model was able to explain 40% of the variance in perceived access to services. While we recruited a diverse sample based on nativity and time in the U.S., it is important to highlight that many of the women in our study may have had high rates of acculturation, such that 81 women in our sample were born in the U.S. and an additional 69 had been living in the U.S. for greater than 13 years.
Theories of social capital (see Putnam, 2000) indicate that voting is an important part of civic participation and is linked to social capital. Results from this study indicate that voting registration was associated with acculturation and not with social capital. Apparently, voter registration is associated more with participants’ perceptions of acculturation or integration into U.S. mainstream society than other cognitive elements of social capital (trust or volunteering). Our findings further suggest that voting registration, a central concept to social capital among Caucasian groups, may hold different meanings and associations across ethnic groups. Among Mexican American women, voting may be more relevant as an indicator of U.S. acculturation and sense of empowerment than to the concept of social capital.
Social capital may be an important resource through which mental health outcomes may be improved among Mexican American women despite the socioeconomic and institutional barriers faced by this population. Few studies have examined how the association between social capital and health may vary by acculturation or immigration-status. Improving social capital, especially for communities with few economic and political resources, may be a cost-efficient and highly effective way to enhance economic and political performance and improve quality of life for this population (Almedon, 2005; Segura et al., 2001). Michael and colleagues (2008) developed a community-based participatory intervention to increase social capital among a sample of African Americans and Latinos and found that their intervention was able to increase social support, self-rated physical health, and improve symptoms of depression. However, the intervention did little to increase reciprocity and civic engagement (two main elements of social capital). While this study shows promising results, interventions targeting social capital need to be better defined.
While the present findings highlight important contributions, there are several limitations that warrant discussion. Both English- and Spanish-speaking participants were included as one group in the SEM analysis due to sample size limitations, therefore direct group comparisons based on language was not possible. Future studies should examine if social capital has the same mediating effect on English- and Spanish- speaking Latino populations residing in the U.S. As with any study which employs a cross-sectional design, the proposed study is limited in making inferences regarding the direction of causality. Measures of social capital, mental health, and perceived access to services were all based on retrospective self-report and therefore the precise temporal sequence of events cannot be determined. Our recruitment strategy, venue based targeted sampling, is a type of convenience sampling which may decrease our ability to generalize beyond our study sample. The construct and measurement of acculturation may also be a limitation given the measures used in the present study. However, we used various measures from respected investigators in the field (see Vega and Alegria, 2001) to measure the latent construct of acculturation for our SEM analysis. Last, while voting registration was used as a factor measuring acculturation it may perhaps be a better proxy of immigration status as non-U.S. citizens cannot register to vote, regardless of degree of acculturation.
While the concept of social capital has recently received much attention, certain critical issues deserve particular attention in future studies: (1) there is no consensus regarding a definition for social capital (see Hawe & Shiell, 2000; Portes, 1998); and (2) there is controversy over whether social capital should be measured at an individual or group level (Baum & Ziersch, 2003; Bourdieu, 1986; Kawachi & Berkman, 2000; Putnam, 2000). Moreover, while our data could not address causation, the present model allows us to explore meaningful pathways that may address health disparities among ethnic minority populations. Future studies need to better address the methodological and measurement flaws in social capital in order to capture its true potential – as “social glue” that brings communities together and enhances health (Putnam, 2000).
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/ccp
Contributor Information
Dellanira Valencia-Garcia, University of Washington, Department of Psychology.
Jane M. Simoni, University of Washington, Department of Psychology
Margarita Alegría, Harvard University, Department of Psychiatry.
David T. Takeuchi, University of Washington, Department of Sociology and School of Social Work
REFERENCES
- Abraido-Lanza AF, Chao MT, Florez KR. Do healthy behaviors decline with greater acculturation? Implications for the Latino mortality paradox. Social Science & Medicine. 2005;61(6):1243–1255. doi: 10.1016/j.socscimed.2005.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Mulvaney-Day N, Woo M, Torres M, Gao S, Oddo V. Correlates of Past-Year Mental Health Service Use Among Latinos: Results From the National Latino and Asian American Study. American Journal of Public Health. 2007;97(1):76–83. doi: 10.2105/AJPH.2006.087197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Canino G, Shrout PE, Woo M, Duan N, Vila D, Torres M, Chen C, Meng X. Prevalence of mental illness in immigrant and non-immigrant US. Latino groups. Am J Psychiatry. 2008;165:359–369. doi: 10.1176/appi.ajp.2007.07040704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Cao A, McGuire TG, Ojeda VD, Sribney B, Woo M, Takeuchi D. Health insurance coverage for vulnerable populations: contrasting Asian Americans and Latinos in the United States. Inquiry. 2006;43(3):231–254. doi: 10.5034/inquiryjrnl_43.3.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Takeuchi D, Canino G, Duan N, Shrout P, Meng X-L, et al. Considering Context, Place, and Culture: the National Latino and Asian American Study. International Journal of Methods in Psychiatric Research. 2004;13(4):208–220. doi: 10.1002/mpr.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almedon AM. Social capital and mental health: An interdisciplinary review of primary evidence. Social Science & Medicine. 2005;61:943–964. doi: 10.1016/j.socscimed.2004.12.025. [DOI] [PubMed] [Google Scholar]
- Baum FE, Ziersch AM. Social capital. Journal of Epidemiology and Community Health. 2003;57:320–323. doi: 10.1136/jech.57.5.320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry JW. Conceptual approaches to acculturation. In: Chun KM, Organista PB, Marin G, editors. Acculturation: Advances in theory, measurement, and applied research. Washington, DC: American Psychological Association; 2003. pp. 17–37. [Google Scholar]
- Bourdieu P. The forms of capital. In: Richardson JG, editor. Handbook of Theory and Research for the Sociology of Education. New York: Greenwood Press; 1986. pp. 241–258. [Google Scholar]
- Carter-Pokras O, Zambrana RE. Latino health status. In: Aguirre-Molina M, Molina C, Zambrana R, editors. Health Issues in the Latino Community. Jossey-Bass Publishing; 2001. pp. 23–54. [Google Scholar]
- Cheadle A, Wagner E, Walls M, Diehr P, Bell M, Anderman C, et al. The effect of neighborhood-based community organizing: Results from the Seattle Minority Youth Health Project. Health Sciences Research. 2001;36(4):671–689. [PMC free article] [PubMed] [Google Scholar]
- Coleman JS. Foundations of Social Theory. Cambridge: Belknap Press of Harvard University Press; 1990. [Google Scholar]
- Cuellar I, Arnold B, Maldonado R. Acculturation rating scale for Mexican Americans-II: A revision of the original ARSMA scale. Hispanic Journal of Behavioral Sciences. 1995;17(3):275–304. [Google Scholar]
- Elder JP, Broyles SL, Brennan JJ, Zuniga de Nuncio ML, Nader PR. Acculturation, parent-child acculturation differential, and chronic disease risk factors in a Mexican-American population. Journal of Immigrant Health. 2005;7(1):1–9. doi: 10.1007/s10903-005-1385-x. [DOI] [PubMed] [Google Scholar]
- Fujiwara T, Kawachi I. A prospective study of individual-level social capital and major depression in the United States. J Epidemiol Community Health. 2008;62:627–633. doi: 10.1136/jech.2007.064261. [DOI] [PubMed] [Google Scholar]
- González HM, Haan MN, Hinton L. Acculturation and the prevalence of depression in older Mexican Americans: Baseline results of the Sacramento area Latino study on aging. JAGS. 2001;49:948–953. doi: 10.1046/j.1532-5415.2001.49186.x. [DOI] [PubMed] [Google Scholar]
- Granovetter MS. The strength of weak ties. American Journal of Sociology. 1973;78(6):1360–1380. [Google Scholar]
- Guarnaccia PJ, Lewis-Fernandez R, Martinez I, Shrout P, Guo J, Torres M, Canino G, Alegría M. Ataque de nervios as a marker of social and psychiatric vulnerability results from the NLAAS. International Journal of Social Psychiatry. 2010;56:298–309. doi: 10.1177/0020764008101636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawe P, Shiell A. Social capital and health: A review. Soc Sci Med. 2000;51(6):871–885. doi: 10.1016/s0277-9536(00)00067-8. [DOI] [PubMed] [Google Scholar]
- Hu DJ, Covell RM. Health care usage by Hispanic outpatients as function of primary language. West. J. Med. 1986;144(4):490–493. [PMC free article] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods. 1998;3(4):424–453. [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indices in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Kawachi I, Berkman LF. Social ties and mental health. Journal of Urban Health. 2001;78(3):458–467. doi: 10.1093/jurban/78.3.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I, Berkman LF. Social cohesion, social capital and health. In: Berkman L, Kawachi I, editors. Social Epidemiology. New York: Oxford University Press; 2000. pp. 171–190. [Google Scholar]
- Kawachi I, Kennedy B, Lochner K, Prothrow SD. Social capital, income inequality, and mortality. American Journal of Public Health. 1997;87:1491–1498. doi: 10.2105/ajph.87.9.1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R, Mroczek D. Ann Arbor (MI): Survey Research Center of the Institute for Social Research, University of Michigan; 1994. Final versions of our non-specific psychological distress scale. [Google Scholar]
- Kessler RC, Andrews G, Mroczek D, Üstun TB, Wittchen HU. The World Health Organization Composite International Diagnostic Interview Short-Form (CIDI-SF) Int J Methods Psychiatr Res. 1998;7:171–185. [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. 2nd ed. New York: Guilford Press; 2005. [Google Scholar]
- Lemp GF, Jones M, Kellogg TA, Nieri GN. HIV seroprevalence and risk behaviors among lesbians and bisexual women in San Francisco and Berkeley, California. American Journal of Public Health. 1995;85(11):1549–1552. doi: 10.2105/ajph.85.11.1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marín G, Marín BV. Research with Hispanic populations. Thousand Oaks, CA: Sage Publications, Inc.; 1991. [Google Scholar]
- Michael YL, Farquhar SA, Wiggins N, Green MK. Findings from a community-based participatory prevention research intervention designed to increase social capital in Latino and African American communities. Journal of Immigrant and Minority Health. 2008;10(3):281–289. doi: 10.1007/s10903-007-9078-2. [DOI] [PubMed] [Google Scholar]
- Mitchell CU, LaGory M. Social capital and mental distress in an impoverished community. City & Community. 2002;1(2):195–215. [Google Scholar]
- Nelson CB, Kessler RC, Mroczek D. Scoring the World Health Organization’s Composite International Diagnostic Interview Short Form. 1998 Web site: http://www.who.int/msa/cidi/cidi-sf.
- Pew Hispanic Center. Web site: http://pewhispanic.org.
- Portes A. Social capital: Its origins and applications in modern sociology. Annual Review of Sociology. 1998;24:1–24. [Google Scholar]
- Putnam RD. Making democracy work: Civic traditions in modern Italy. Princeton, NJ: Princeton University Press; 1993. [Google Scholar]
- Putnam RD. Bowling Alone. The Collapse and Revival of American Community. New York: Simon and Schuster; 2000. [Google Scholar]
- Schwartz SJ, Unger JB, Zamboanga BL, Szapocznik J. Rethinking the concept of acculturation: Implications for theory and research. American Psychologist. 2010;65(4):237–251. doi: 10.1037/a0019330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segura GM, Pachon H, Woods ND. Hispanics, social capital, and civic engagement. National Civic Review. 2001;90(1):85–96. [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW the Patient Health Questionnaire Primary Care Study Group. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. JAMA. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Vega WA, Alegría M. Latino mental health and treatment in the United States. In: Aguirre-Molina M, Molina C, Zambrana RE, editors. Health Issues in the Latino Community. Jossey-Bass Publishing; 2001. pp. 179–208. [Google Scholar]
- Vega WA, Lopez SR. Priority Issues in Latino Mental Health Services Research. Mental Health Services Research. 2001;3(4):189–200. doi: 10.1023/a:1013125030718. [DOI] [PubMed] [Google Scholar]
- Vega WA, Kolody B, Aguilar-Gaxiola S, Alderate E, Catalano R, Carveo-Anduaga J. Lifetime prevalence of DSM-III-R psychiatric disorders among urban and rural Mexican Americans in California. Archives of General Psychiatry. 1998;55:771–778. doi: 10.1001/archpsyc.55.9.771. [DOI] [PubMed] [Google Scholar]
- Wells KB, Golding JM, Hough RL, Burnam MA, Karno M. Factors affecting the probability of use of general and medical health and social/community services for Mexican Americans and non-Hispanic whites. Medical Care. 1988;26(5):441–452. doi: 10.1097/00005650-198805000-00001. [DOI] [PubMed] [Google Scholar]
- Zambrana RE, Zoppi IM. Latina students: Translating cultural wealth into social capital to improve academic success. Journal of Ethnic & Cultural Diversity in Social Work. 2002;11(1–2):33–53. [Google Scholar]