Abstract
Purpose
By adversely affecting family functioning and stability, poverty constitutes an important risk factor for children’s poor mental health functioning. This study examines the impact of a comprehensive microfinance intervention, designed to reduce the risk of poverty, on depression among AIDS-orphaned youth.
Methods
Children from 15 comparable primary schools in Rakai District of Uganda, one of those hardest hit by HIVAIDS in the country, were randomly assigned to control (n=148) or treatment (n=138) conditions. Children in the treatment condition received a comprehensive microfinance intervention comprising of matched savings accounts, financial management workshops, and mentorship. This was in addition to traditional services provided for all school-going orphaned adolescents (counseling and school supplies). Data were collected at wave 1 (baseline), wave 2 (10-months postintervention), and wave 3 (20-months post-intervention). We used multilevel growth models to examine the trajectory of depression in treatment and control conditions, measured using Children’s Depression Inventory (Kovacs).
Results
Children in the treatment group exhibited a significant decrease in depression whereas their control group counterparts showed no change in depression.
Conclusion
The findings indicate that over and above traditional psychosocial approaches used to address mental health functioning among orphaned children in sub-Saharan Africa, incorporating poverty alleviation-focused approaches, such as this comprehensive microfinance intervention, has the potential to improve psychosocial functioning of these children.
Introduction and Background
The relationship between poverty and mental health functioning is well documented.1–5 Poverty affects not only families’ ability to physically care for children, but also families’ stability, functioning, and psychosocial wellbeing.6, 7 Thus, family poverty, by adversely affecting family functioning, constitutes an important risk factor for children’s poor mental health functioning. In particular, children in poverty, with no real hope for a future, are more likely to be depressed.8
In this paper we examine the impact of a comprehensive microfinance intervention, intended to reduce the risk of poverty, on depression among adolescent youth who have lost either one or both parents to AIDS. Studies indicate that AIDS-affected children often suffer recurrent trauma, starting with the illness and deaths of their first line of defense—the parents. A child who has been affected by AIDS is more likely to have increased levels of anxiety, depression and reduced self-esteem. 8, 9–12 Depression among this group of children is particularly worrisome as it may severely undermine their future development, social functioning, and risk taking behaviors, and reproductive health choices.13 In Uganda, a country heavily affected by HIV/AIDS, orphaned children exhibit significantly higher depressive symptoms compared to non-orphan children.8, 11 Similar findings were reported in Tanzania,14 Mozambique,15 and Namibia.16
To date, few interventions aimed at enhancing mental health and psychosocial functioning of orphaned children have addressed family poverty. Most interventions, especially in sub-Saharan Africa the epicenter of HIV/AIDS, are limited in that they primarily focus on counseling with some including food, shelter and clothing.17, 18 Although these usual forms of care may provide temporary relief, they often fall short of providing long-term care, support, and economic opportunities—including the realistic hope necessary to address emotional distress and to break the vicious cycle of hopelessness and helplessness.
Asset theory19 posits that access to economic opportunities will have important psychological and socio-economic benefits for individuals and families. Thus, poverty reduction interventions over and above the traditional approaches of care may help AIDS-orphaned children’s psychosocial functioning, and enhance their family and individual stability. In addition, resiliency theory 20 predicts that individual capacities and family resources, including access to economic assets (in this case, the microfinance intervention detailed below), balance the effect of life adversities, including AIDS-induced orphanhood. With appropriate economic resources and support, poor AIDS-orphaned children may overcome their disadvantaged experiences.
Against that background, we hypothesize that AIDS-orphaned adolescents provided with a comprehensive microfinance program, consisting of matched savings accounts, training in financial management and small business development, and mentorship, would have improved mental health functioning. We specifically address two questions: 1) Would a comprehensive microfinance intervention reduce depression among AIDS-orphaned children?; 2) What are the lessons and key insights that would inform future microfinance interventions aimed at impacting mental health functioning of AIDS-orphaned adolescents?
The Intervention
Suubi (hope)-Uganda Project
This paper is based on a pilot study of a comprehensive microfinance intervention (MH076475-01) funded by the National Institute of Mental Health (NIMH) (2005– 2008). The study received IRB approval from Columbia University (AAA5337), and the Uganda National Council of Science and Technology (SS 1540).
The intervention served AIDS-orphaned adolescents who were in their last year or two prior to the transition to secondary school, as this is the time when children begin to be at risk of dropping out of school. Specifically, children who met the following criteria were eligible to participate in the study: (1) an AIDS-orphaned child, defined as having lost one or both parents to AIDS; and (2) enrolled in primary school, specifically in primary six or primary seven (the equivalent of 7th and 8th grade in the U.S education system). Study participants were recruited through the school system from 15 rural primary schools in Rakai District over a 3-month period. The schools included in the study have similar socioeconomic characteristics, including overall performance on the national standardized Primary Leaving Examinations (PLEs), and they attract students from similar socioeconomic backgrounds. Each of the 15 primary schools was randomly assigned to the experimental or control condition, such that all selected children from a particular school received the same intervention. During the study design phase, individual-level randomization was considered because it could improve power for hypothesis testing, but school-level randomization was selected to reduce the possibility of contamination of control participants by intervention participants. Because of geographic distance between schools, participants assigned to different conditions did not know each other
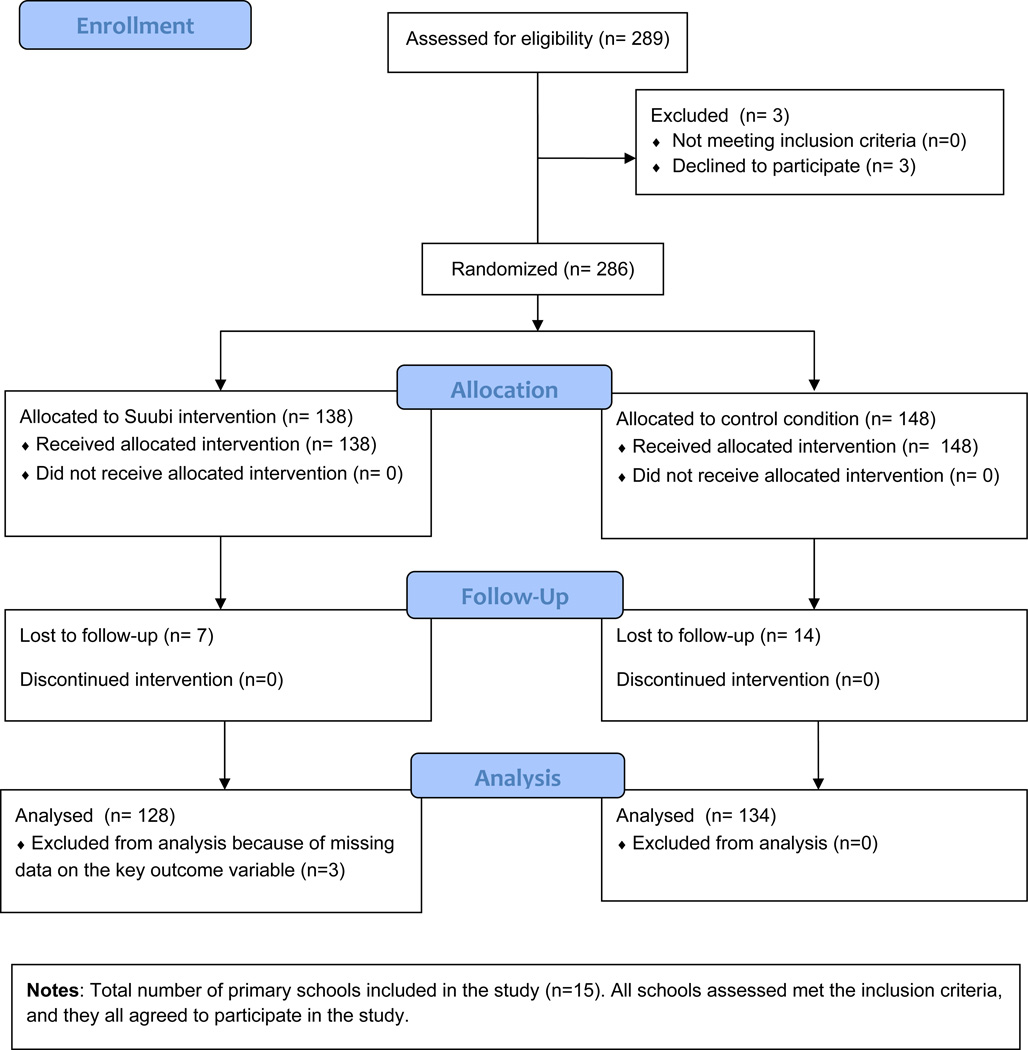
The recruitment process involved the following: School-going children meeting the inclusion criteria outlined above were given flyers written in Luganda (the local language) and English (the instructional language used in all Ugandan schools) outlining the key features of the study. Children who expressed interest in the study were required to participate in an in-person meeting where the research team explained in detail the proposed study. Following these in-person meetings, children interested in the study were asked to bring their caregivers who were given the same study details. Throughout the meetings, it was emphasized that participation in the study was voluntary. Only three participants decided not to participate, saying that the microfinance intervention as designed seemed “too good to be true”. (See figure 1 for CONSORT Flow Diagram).
Figure 1.
CONSORT 2010 Flow Diagram
The treatment condition (also known as Suubi intervention group) had 138 children. The control condition (also known as usual care) had 148 children (N = 286 total). RMASS 21 was used to generate the minimum detectable effect size d representing the standardized mean difference between groups for continuous, normal primary outcomes for the original study (e.g, HIV knowledge) in a two-group repeated measures design. Inputs were alpha = .05, power = .80, three time points, baseline N = 300, attrition = 10%, and repeated measures covariance structure based on pilot data, followed by several design effect (DEFF) adjustment scenarios for clustering of students within schools. At DEFF = 1.0, d = .32; at DEFF = 2.0, d = .46, which fall between a small (d = .20) and a medium (d = .50) difference. 22 The actual baseline N of 286 was slightly less than 300, but attrition was only 8%, so useable N was close to the original target.
Participants assigned to the control condition received the usual care for orphaned children, consisting of counseling and educational related supplies (including textbooks—kept by the participating schools at the end of the study). Further, by virtue of being in school, all participants received health education (including AIDS-focused education) provided through the nationwide primary school curriculum.
Participants assigned to the experimental condition (the Suubi intervention group) received the usual care plus a comprehensive microfinance intervention designed to reduce poverty. Specifically, the Suubi intervention had three key components. First, it promoted monetary savings, through support for matched savings accounts, which could be used for educational opportunities for adolescent children or for small business opportunities for youth and their families. In a matched savings account, for every dollar that a child and his/her family contributes (up to a specified limit), the program contributes a match. In this intervention, the match rate was 2:1 and the match cap was $10/month, so for every dollar that a child or family contributed to the child’s savings account (up to the cap of $10/month), the program contributed an additional two dollars. The account was held in the child’s name and the matching funds in the account could only be used to pay for the child’s secondary education or to invest in a family business. This component of the intervention was designed to reduce the long-run risk of poverty by raising the likelihood that a child would stay in school and by raising family income through income-generating small businesses. It was intended to reduce child depression by raising a child’s hopes and aspirations for the future, by raising the chance that a child would see him/herself as being able to go on in school, and by reducing financial hardship. Second, the program offered financial management classes and classes on small businesses, intended to support savings and the establishment of family-level income generating projects for orphaned children and their caregiving families. We expected this component to raise family incomes and reduce child depression by enhancing economic stability, providing a long-run source of income for families, and enhancing family protective processes. Third, the intervention provided an adult mentor to children. An ongoing caring relationship with an adult is one of the most important sources for resilience in children and can protect their mental health when they experience stress and adversity.23–24 In addition, we expected the provision of a mentor to boost the effectiveness of the other components of the intervention, by encouraging youth to save, supporting them in developing career aspirations, and providing further support and guidance about starting small businesses. See Ssewamala and colleagues 25–28 for a more detailed description of the intervention.
Data were collected at wave 1 (baseline), wave 2 (10–12 months after baseline), and wave 3 (20–24 months after baseline). A 90-minute survey was administered by trained Ugandan research assistants blind to study assignment and matched to the participants by gender. The surveys were administered individually at the child’s home or in a private office space at the school during non-school days. Surveys were administered in English, since all children in year 6 and 7 are proficient in English, but all measures were also available in Luganda (the native language) in the event that a child did not appear to fully comprehend the questions in English. There were no reported adverse effects of the intervention on study participants.
Measures
The outcome variable – children’s depressive symptoms -- was measured using the Children’s Depression Inventory (CDI) developed by Kovacs.29 The study utilized a short version of CDI that contains 10 items, whose psychometric properties are comparable to the long version of the same measure.30 The CDI is a widely utilized standardized measure of children’s depressive symptoms and has been previously tested by the investigators and other researchers with AIDS-orphaned children in sub-Saharan Africa.16, 31–33 For each question asked, children were required to choose one of three statements that best described their feelings in the past two weeks (e.g., “I am sad once in a while”; “I am sad many times”; “I am sad all the time”). Statements indicating no symptoms of depression (e.g., “I am sad once in a while”) were coded as 0, statements representing moderate depressive feelings (e.g., I am sad many times) were coded as 1, and statements representing higher levels of depression (e.g., “I am sad all the time”) were coded as 2. The total score was computed by summing up the score across all the ten items. The hypothetical score range was 0 to 20, with a higher score indicating higher levels of depression. The CDI index demonstrated moderate internal consistency for the current sample (Cronbach’s alpha at baseline = .65).
The socio-demographic covariates included in the study are: gender of the child, child’s orphanhood status (coded as double orphan [both parents not living], maternal orphan [a biological mother not living], or paternal orphan [a biological father not living]), employment status of primary caregiver, education-level attained by primary caregiver, age, number of people in the household, family cohesion, child-parent/caregiver relationship, and level of comfort between the child and parent talking (see Table 1).
Table 1.
Socio-demographic Characteristics of Suubi Participants (N=283)
| Percent or Mean, % [95% Confidence Interval] | ||||||
|---|---|---|---|---|---|---|
| Variable | Total (N=283) |
Treatment Group (N=128) |
Control Group (N=132) |
Design- based F |
p | Design Effect (DEFF) |
| Female childa | 56.89 [47.28,66.01] | 60.58 [44.25,74.85] | 53.42 [43.05,63.51] | 0.65 | .44 | 2.23 |
| Orphanhood Statusa | ||||||
| Double orphan | 39.07 [33.41, 45.04] | 36.76 [30.8, 43.16] | 41.26 [32.44, 50.67] | 1.19 | .32 | 0.82 |
| Maternal orphan | 19.00 [14.52, 24.45] | 22.06 [14.21, 32.59] | 16.08 [13.94, 18.48] | |||
| Paternal orphan | 41.94 [36.45, 47.63] | 41.18 [36.63, 45.88] | 42.66 [33.05, 52.86] | |||
| Employment status of primary caregivera | ||||||
| Self-employed | 62.99 [55.96, 69.51] | 56.93 [48.99, 64.54] | 68.75 [59.46, 76.74] | 4.51 | .052 | 0.90 |
| Formally employed | 37.01 [30.49, 44.04] | 43.07 [35.46, 51.01] | 31.25 [23.26, 40.54] | |||
| Female caregiver education (years)b | 2.92 [2.68, 3.15] | 2.88 [2.60, 3.16] | 2.96 [2.58, 3.33] | 0.13 | .72 | 1.44 |
| Male caregiver education (years)b | 3.71 [3.55, 3.88] | 3.76 [3.46, 4.07] | 3.67 [3.56, 3.77] | 0.42 | .53 | 0.76 |
| Age in yearsb | 13.71 [13.37, 14.05] | 13.82 [13.21, 14.42] | 13.6 [13.31, 13.89] | 0.47 | .50 | 4.04 |
| Number in householdb | 6.66 [6.08, 7.24] | 7.10 [6.33, 7.86] | 6.25 [5.72, 6.79] | 3.74 | .07 | 1.51 |
| Family cohensionb | 20.16 [19.54, 20.78] | 20.22 [19.03, 21.41] | 20.10 [19.65, 20.56] | 0.04 | .85 | 1.45 |
| Parent relationshipb | 7.09 [6.86, 7.30] | 7.00 [6.60, 7.40] | 7.17 [7.01, 7.32] | 0.69 | .42 | 1.61 |
| Talk with parentsb | 14.22 [13.04, 15.41] | 14.23 [12.20, 16.27] | 14.21 [12.94, 15.49] | 0.01 | .99 | 2.30 |
| Comfort in talkingb | 16.03 [13.63, 18.43] | 14.64 [11.42, 17.91] | 17.31 [13.70, 20.91] | 1.37 | .26 | 4.97 |
Notes:
Percent and 95% CI;
Mean and 95% CI. N = 279 for orphanhood status; N = 281 for caregiver employment status; N = 282 for parent relationship.
Data Analysis
Statistical analysis was performed using Stata 11 and SAS 9.2. We utilized survey procedures in Stata34 for frequency tables to obtain confidence intervals and test statistics that are appropriately adjusted for participants being nested within schools. We used a linear multilevel growth curve model to investigate the impact of the Suubi intervention on depression. Due to a baseline difference in depression between the control and intervention groups, described below, the overall analysis focused on within-group changes in depression over time. To facilitate interpretation the model was parameterized to contain group-specific intercepts and slopes with the default constant term omitted. Planned comparisons tested group depression differences at three key time points: baseline, the study midpoint (10 months), and at the end of the study (20 months). Random effects included participant-specific intercepts and slopes and a random intercept term for school membership to account for within-school correlation of participants’ responses. The resulting model was a three-level multilevel model with measurements of depression at each time point (level 1) being nested within participants (level 2) who were in turn nested within schools (level 3). Follow-up analyses employed double robust estimation methods to compute mean population-level differences between groups’ depression scores at 10 months and at 20 months under the assumption of pseudo-balance of the baseline depression score and other potential confounders.35 The Stata command - dr- was used to perform doubt robust estimation analyses.36
Results
Descriptive results
As indicated in Table 1, the mean age for the youth in the study was 13.71 years. Girls represented 57% of the study sample. Thirty-nine percent of the children were double orphans (with no biological father or mother living), 19% maternal orphans (without a biological mother living), and 42% paternal orphans (with no biological father living). Only 37% of the children’s primary caregivers reported some form of formal employment. The rest (63%) were self-employed or worked in the informal sector. Parental education in this Ugandan sample was modest: the mean years of education was 2.92 for female caregivers and 3.71 years for male caregivers. On average, children reported between six and seven persons living in their households. The depression score at baseline ranged from 0 to 15 points with an average score of 3.29 (95% CI=2.73, 3.85).
Table 2 displays sample means and 95% confidence intervals for depression at each measurement occasion and unadjusted comparisons of the intervention and control group means at each time point. At baseline, there were no significant differences between the treatment and control groups on the depression score, yet significant differences between the two groups were found at 10 months and 20 months (Table 2).
Table 2.
Mean Depression Levels of SUUBI Participants (N=283)
| Mean [95% Confidence Interval] | |||||
|---|---|---|---|---|---|
| Depression Mean | Treatment Group (N=128) |
Control Group (N=132) |
F | p | Design Effect (DEFF) |
| Sample-Based | |||||
| Wave 1 (N=283) | 2.82 [2.12, 3.52] | 3.73 [3.08, 4.39] | 4.20 | .06 | 2.29 |
| Wave 2 (N=274) | 2.31 [2.00, 2.63] | 4.08 [3.52, 4.64] | 34.72 | <.001 | 1.04 |
| Wave 3 (N=260) | 2.16 [1.75, 2.57] | 3.45 [3.20, 3.69] | 33.31 | <.001 | 0.63 |
| Model-Based | |||||
| Wave 1 | 2.73 [2.19, 3.26] | 3.86 [3.13, 4.59] | 6.15 | .014 | — |
| Wave 2 | 2.39 [2.06, 2.72] | 3.73 [3.30, 4.17] | 23.14 | <.001 | — |
| Wave 3 | 2.05 [1.75, 2.35] | 3.61 [3.25, 3.97] | 42.51 | <.001 | — |
Notes: Sample means were tested for equality using a design-based F-statistic corrected for clustering of respondents within schools. Model-based estimated means were compared within a three-level linear mixed model with random intercepts and slopes capturing within-person variability and an additional random intercept for school ID. F-tests for model-based estimates were computed based on the HC3 heteroskedastic-consistent “sandwich” variance estimator available in SAS PROC GLIMMIX.
Table 2 also displays model-based means, 95% confidence intervals, and p-values testing equality of the model-based means arising from the multilevel model described below. Using the model-based approach, statistically significant differences in depression between the intervention and control groups were obtained at each measurement occasion, including baseline. At each time point, the intervention group estimated mean was lower than the control group’s mean.
Multilevel Model Results
Results from the multilevel model (in Table 3) show that the Suubi intervention group had a statistically significant reduction in depression over time (B = −.34, t(256) = −2.41, p = .02; 95% CI = −.61, −.06), but the control group’s slope for the depression change over time was not statistically significant (B = −.13, t(256) = −0.68, p = .50; 95% CI = −.50, .24; the two slopes were not statistically different, however: B = −.21, t(256) = −0.88, p = .38; 95% CI = −.67, .26). Turning to planned comparisons of model-implied depression means, baseline depression means for intervention (M = 2.73) and control (M = 3.86) were significantly different (t(256) = 2.48, p = .01), as were intervention (M = 2.39) and control (M = 3.73) groups’ means at 10 months (t(256) = 4.81, p < .0001) and intervention (M = 2.05) and control groups’ (M = 3.61) means at 20 months (t(256) = 6.52, p < .0001). These results indicate that over the period of the intervention, depression was significantly reduced among the treatment group, but not among the controls.
Table 3.
Mean Depression Levels of SUUBI Participants (N=283)
| Effect | B [95% Confidence Interval] | Test Statistic | p |
|---|---|---|---|
| Fixed | |||
| Intercept - Intervention | 2.73 [2.19, 3.26] | 10.10 | <.0001 |
| Intercept - Control | 3.86 [3.13, 4.59] | 10.43 | <.0001 |
| Slope - Intervention | −0.34 [−0.61, −0.06] | −2.41 | .02 |
| Slope - Control | −0.13 [−0.50, 0.24] | −0.68 | .50 |
| Random (Level) | |||
| Level 2 | |||
| Person Intercept | 0.93 [0.39, 4.39] | 1.75 | .04 |
| Person Slope | 0.33 [0.10, 7.27] | 1.11 | .13 |
| Covariance: Person Intercept - Person Slope | 0.09 [−0.55, 0.73] | 0.28 | .78 |
| Level 3 | |||
| School Intercept | 0.06 [0.01, 11.69] | 0.82 | .21 |
| Residual | 4.49 [3.82, 5.36] | 11.56 | <.0001 |
Notes: Model-based estimated intercepts and slopes were compared within a three-level linear mixed model with random intercepts and slopes capturing within-person variability and an additional random intercept for school ID. The test statistic for fixed effects is a t-test with 256 degrees of freedom. The test statistic for random effects is a Wald z-test. All test statistics were computed based on the HC3 heteroskedastic-consistent “sandwich” variance estimator available in SAS PROC GLIMMIX.
Double Robust Estimation Results
Due to the difference in groups’ baseline depression means, it is difficult to determine whether the significant differences in the groups’ post-intervention depression means arose from the intervention. Ideally, randomization would have yielded equivalent depression means at baseline, but such was not the case. Thus, a logical follow-up question to explore is whether post-baseline depression scores would differ in a hypothetical or counterfactual scenario in which depression means at baseline were in fact equivalent and all participants could have received the Suubi intervention or all participants could have received usual care. This question can be investigated using double robust estimation. Double robust estimation methods estimate group differences controlling for potential confounder influences on (a) the outcome and (b) study group membership and will yield pseudo-balance on baseline depression. 37 Ten and 20-month depression scores may then be compared under the assumption of pseudo-balance of baseline depression (and any other potential confounders included in the analysis).
Table 4 presents the results from the double robust analysis. For comparison purposes, the top half of the table displays the results from an unadjusted analysis comparing the two groups on depression at each wave. The bottom half of the table shows the corresponding adjusted double robust estimated mean differences that are generated under the assumption of pseudo-balance of baseline depression and other baseline covariates shown in Table 1. As expected, the mean differences are reduced, but they are still statistically significant, which suggests that even if baseline depression had been equivalent across the two study groups, depression levels following the Suubi intervention would have been significantly lower than depression levels under usual care.
Table 4.
Double Robust Estimates of Group Differences in Depression
| Mean | |||||
|---|---|---|---|---|---|
| Depression Mean | Treatment | Control | Difference [95% CI] | Z | p |
| Unadjusted | |||||
| Wave 1 (N=283) | 2.82 | 3.73 | −0.92 [−1.76, −0.02] | −2.07 | .039 |
| Wave 2 (N=274) | 2.31 | 4.08 | −1.77 [−2.31, −1.19] | −6.04 | <.001 |
| Wave 3 (N=260) | 2.16 | 3.45 | −1.29 [−1.75, −0.88] | −5.74 | <.001 |
| Adjusted | |||||
| Wave 1 (N=283) | 3.11 | 3.30 | −0.19 [−0.72, 0.23] | −0.72 | .47 |
| Wave 2 (N=274) | 2.25 | 3.91 | −1.66 [−2.20, −1.16] | −6.04 | <.001 |
| Wave 3 (N=260) | 2.32 | 3.41 | −1.09 [−1.67, −0.72] | −4.80 | <.001 |
Notes: All estimates were generated using the Stata command -dr- with clustering of adolescents nested within schools handled via the cluster bootstrap with 5001 bootstrap replications. Confidence intervals for differences are based on the bias-corrected (BC) bootstrap-based confidence interval. Adjusted analyses controlled for the effects of all potential confounders listed in Table 1 on both group membership and depression outcome scores. Also, baseline depression was included as a predictor of group membership at all three waves and as a predictor of depression outcome scores at wave 2 and wave 3.
Discussion
This study reports the results of a comprehensive microfinance intervention which provided AIDS orphans in Uganda with a matched savings account they could use to pay for secondary schooling or to invest in family businesses, financial and business training workshops, and a mentorship program.
Participants in the Suubi intervention group showed a significant reduction in depression over time whereas participants in the control group did not. One potential concern is that, in spite of randomization, participants in the Suubi group had lower mean levels of depression at baseline than children in the control group. However, the significant differences in mean levels of depression persisted even after double robust estimation was used to attain pseudo-balance of baseline depression and other potential confounders, suggesting that the intervention did reduce depression among these high-risk youth.
These results support the hypothesis that a combined microfinance intervention, including matched savings accounts, workshops to support savings and business development, and mentorship, could be effective in reducing depression among AIDS orphaned youth in Uganda. Because the intervention was delivered as a package, we are not able to determine which component(s) of the intervention played the most important role in improving children’s mental health functioning. On the one hand, we expect that the matched savings component would play a primary role, by giving children hope that they could continue on to secondary school and by raising family incomes and reducing financial hardship. On the other hand, it is likely that the role of those matched savings accounts was augmented by children receiving the workshops and the mentorship. It is also likely that having a mentor may have had a direct effect on youth mental health. However, our study was not designed to tease apart the effects of different components and thus we can only speculate about this.
As mentioned, an important limitation to these findings is that baseline levels of depression were different across the two groups, most likely due to the small numbers of schools in this intervention pilot study. Double robust and related methods that pseudo-balance otherwise imbalanced groups are helpful to address this issue, but they are not as robust as having groups that are actually balanced at the outset of the study. This is especially true in the current study where the number of available potential confounders to include in the double robust estimation was quite limited.
Also, while levels of depression were significantly reduced in the Suubi intervention group over time while the control group’s were not, the groups’ depression slopes were not statistically different from each other, which could suggest the possibility of modest naturalistic depression reduction among Uganda AIDS-orphaned adolescents as they age. However, it is important to note that the baseline depression difference was in the same direction as the follow-up depression differences (lower mean levels of depression in the intervention group at all time points), so regression to the mean was less likely to play a role in the significant differences observed post-baseline. Moreover, the mean difference in depression scores between the groups increased over time.
Thus, despite the limitations noted above, we regard these findings as sufficiently intriguing to merit additional study of comprehensive microfinance interventions as a vehicle to reduce depression among youth in resource-poor settings. An important element of future studies will be to measure a wide array of potential mechanisms of change, with each mechanism linked to a specific element of the intervention. The current pilot study was not scaled to investigate such issues, nor did it include separate arms where children received one component of the intervention but not others. Thus, it was not possible to separate out the effects of the matched savings accounts vs. the workshops vs. the mentorship program. Future studies that include such measures linked to specific intervention components and coupled with a larger sample (more participants and especially more schools, and ideally different intervention arms), employing stratified randomization to ensure depression balance across study groups at baseline, will enable researchers to shed more light on the role such interventions might play in improving mental health functioning among these at risk youth. 38
Even with the above-mentioned limitations, our findings are suggestive and have implications relevant for researchers, pediatricians and health care practitioners. The findings indicate that over and above the traditional psychosocial approaches used to address mental health functioning among orphaned children in sub-Saharan Africa, poverty alleviation-focused approaches, such as the comprehensive microfinance intervention studied here, may play a role in lowering depression. This finding is significant, given the multidimensional nature of poverty in sub-Saharan Africa, and in light of the fact that the region is the epicenter of HIV/AIDS. While not conclusive, our results suggest that a larger randomized trial is in order. Overall, the findings of this study complement earlier studies 39, 40 that point to the role of comprehensive microfinance programs in health-promoting interventions in low resource countries.
Acknowledgement
Funding for the Suubi-Uganda study came from the National Institute of Mental Health (R21 MH076475-01). The study received IRB approval from Columbia University (AAA5337), and the Uganda National Council of Science and Technology (SS 1540). We are grateful to Ms. Proscovia Nabunya (at the University of Chicago), Reverend Fr. Kato Bakulu, and Ms. Stacey Alicea for monitoring the study implementation process. We thank all the children and their caregiving families who agreed to participate in the Suubi-Uganda study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Fred M. Ssewamala, Email: fs2114@columbia.edu, Associate Professor of Social Work and International Affairs, Columbia University.
Torsten B. Neilands, Email: Torsten.Neilands@ucsf.edu, Associate Professor, Center for AIDS Prevention, University of California, San Francisco.
Jane Waldfogel, Email: jw205@columbia.edu, Professor of Social Work and Public Policy, Columbia University.
Leyla Ismayilova, Email: li61@columbia.edu, Post-Doctoral Fellow, Columbia University School of Social Work.
References
- 1.Costello E, Compton S, Keeler G, Angold A. Relationships between poverty and psychopathology: A natural experiment. JAMA. 2003;290(15):2023. doi: 10.1001/jama.290.15.2023. [DOI] [PubMed] [Google Scholar]
- 2.Lipman E, Offord D, Boyle M. What if we could eliminate child poverty? Social Psychiatry and Psychiatric Epidemiology. 1996;31(5):303–307. doi: 10.1007/BF00787925. [DOI] [PubMed] [Google Scholar]
- 3.McLeod J, Shanahan M. Trajectories of poverty and children's mental health. Journal of Health and Social Behavior. 1996;37(3):207–220. [PubMed] [Google Scholar]
- 4.Pollitt E. Poverty and child development: Relevance of research in developing countries to the United States. Child Development. 1994;65(2):283–295. [PubMed] [Google Scholar]
- 5.Duncan G, Brooks-Gunn J. Family poverty, welfare reform, and child development. Child Development. 2000;71(1):188–196. doi: 10.1111/1467-8624.00133. [DOI] [PubMed] [Google Scholar]
- 6.Foster G. Children who live in communities affected by AIDS. The Lancet. 2006;367(9511):700–701. doi: 10.1016/S0140-6736(06)68273-1. [DOI] [PubMed] [Google Scholar]
- 7.Case A, Paxson C, Ableidinger J. Orphans in Africa: parental death, poverty, and school enrollment. Demography. 2004;41(3):483–508. doi: 10.1353/dem.2004.0019. [DOI] [PubMed] [Google Scholar]
- 8.Sengendo J, Nambi J. The psychological effect of orphanhood: a study of orphans in Rakai district. Health Transition Review. 1997;7:105–124. [PubMed] [Google Scholar]
- 9.Cluver L, Gardner F. The mental health of children orphaned by AIDS: a review of international and southern African research. Journal of Child and Adolescent Mental Health. 2007;19(1):1. doi: 10.2989/17280580709486631. [DOI] [PubMed] [Google Scholar]
- 10.Cluver L, Gardner F. The psychological well-being of children orphaned by AIDS in Cape Town, South Africa. Annals of General Psychiatry. 2006;5(1):8. doi: 10.1186/1744-859X-5-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Atwine B, Cantor-Graae E, Bajunirwe F. Psychological distress among AIDS orphans in rural Uganda. Social Science & Medicine. 2005;61(3):555–564. doi: 10.1016/j.socscimed.2004.12.018. [DOI] [PubMed] [Google Scholar]
- 12.Rotheram-Borus M, Stein J. Problem behavior of adolescents whose parents are living with AIDS. American Journal of Orthopsychiatry. 1999;69:228–239. doi: 10.1037/h0080424. [DOI] [PubMed] [Google Scholar]
- 13.Patel V, Flisher A, Hetrick S, McGorry P. Mental health of young people: a global public-health challenge. The Lancet. 2007;369(9569):1302–1313. doi: 10.1016/S0140-6736(07)60368-7. [DOI] [PubMed] [Google Scholar]
- 14.Makame V, Grantham-Mcgregor S. Psychological well-being of orphans in Dar El Salaam, Tanzania. Acta Paediatrica. 2002;91(4):459–465. doi: 10.1080/080352502317371724. [DOI] [PubMed] [Google Scholar]
- 15.Manuel P. Assessment of orphans and their caregivers' psychological well-being in a rural community in central Mozambique. London, Institute of Child Health. 2002 [Google Scholar]
- 16.Ruiz-Casares M, Thombs B, Rousseau C. The association of single and double orphanhood with symptoms of depression among children and adolescents in Namibia. European Child & Adolescent Psychiatry. 2009;18(6):369–376. doi: 10.1007/s00787-009-0739-7. [DOI] [PubMed] [Google Scholar]
- 17.Deininger K, Garcia M, Subbarao K. AIDS-induced orphanhood as a systemic shock: Magnitude, impact, and program interventions in Africa. World Development. 2003;31(7):1201–1220. [Google Scholar]
- 18.UNICEF. Africa's Orphaned and Vulnerable Generations: Children affected by AIDS. 2003 http://www.unicef.org/publications/files/Africas_Orphaned_and_Vulnerable_Generations_Children_Affected_by_AIDS.pdf.
- 19.Sherraden M. Stakeholding: Notes on a theory of welfare based on assets. The Social Service Review. 1990;64(4):580–601. [Google Scholar]
- 20.Fergus S, Zimmerman M. Adolescent resilience: a framework for understanding healthy development in the face of risk. 2004 doi: 10.1146/annurev.publhealth.26.021304.144357. [DOI] [PubMed] [Google Scholar]
- 21.Hedeker D, Gibbons RD, Waternaux C. Sample Size Estimation for Longitudinal Designs with Attrition: Comparing Time-Related Contrasts Between Two Groups. Journal of Educational and Behavioral Statistics. 1999;24(1):70–93. [Google Scholar]
- 22.Cohen J. Statistical Power Analysis for the Behavioral Sciences. Hillsdale, New Jersey: Lawrence Erlbaum Associates; 1987. [Google Scholar]
- 23.Garmezy N. Stress-resistant children: The search for protective factors. Recent research in developmental psychopathology. 1985;4:213–233. [Google Scholar]
- 24.Garmezy N, Rutter M. Stress coping and development in children. New York: McGraw-Hill; 1983. [Google Scholar]
- 25.Ssewamala F, Han C, Neilands T. Asset ownership and health and mental health functioning among AIDS-orphaned adolescents: Findings from a randomized clinical trial in rural Uganda. Social Science & Medicine. 2009 doi: 10.1016/j.socscimed.2009.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ssewamala F, Han C, Neilands T, Ismayilova L, Sperber E. Effect of Economic Assets on Sexual Risk-Taking Intentions Among Orphaned Adolescents in Uganda. American Journal of Public Health. 2010;100(3):483. doi: 10.2105/AJPH.2008.158840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ssewamala F, Ismayilova L. Integrating Children's Savings Accounts in the Care and Support of Orphaned Adolescents in Rural Uganda. Social Service Review. 2009;83(3):453–472. doi: 10.1086/605941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ssewamala F, Ismayilova L, McKay M, Sperber E, Bannon W, Jr, Alicea S. Gender and the Effects of an Economic Empowerment Program on Attitudes Toward Sexual Risk-Taking Among AIDS-Orphaned Adolescent Youth in Uganda. Journal of Adolescent Health. 2009 doi: 10.1016/j.jadohealth.2009.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kovacs M. The children’s depression inventory (CDI) Psychopharmacology Bulletin. 1985;21(4):995–998. [PubMed] [Google Scholar]
- 30.Kovacs M. The Children's Depression Inventory (CDI): Technical Manual Update. Toronto, ON: Multi-Health Systems; 2003. [Google Scholar]
- 31.Cluver L, Gardner F, Operario D. Psychological distress amongst AIDS-orphaned children in urban South Africa. J Child Psychol Psychiatry. 2007 Aug;48(8):755–763. doi: 10.1111/j.1469-7610.2007.01757.x. [DOI] [PubMed] [Google Scholar]
- 32.Wallis A, Dukay V. Project MUSE Journals Journal of Health Care for the Poor and Underserved Volume 20, Number 4, November 2009 Supplement Learning How to Measure the Well-Being of OVC in a Maturing HIV/AIDS Crisis. Journal of Health Care for the Poor and Underserved. 2009;20(4) doi: 10.1353/hpu.0.0230. [DOI] [PubMed] [Google Scholar]
- 33.Ssewamala FM, Alicea S, Bannon W, Ismayilova L. A Novel Economic Intervention to Reduce HIV Risks among School-going AIDS-Orphaned Children in Rural Uganda. Journal of Adolescent Health. 2008;42(1):102–104. doi: 10.1016/j.jadohealth.2007.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rabe-Hesketh S, Skrondal A. Multilevel and longitudinal modeling using Stata. Stata Corp; 2008. [Google Scholar]
- 35.Robins J, Rotnitsky A, Zhao LP. Analysis of semiparametric regression models for repeated outcomes in the presence of missing data. Journal of the American Statistical Association. 1995;90:106–121. [Google Scholar]
- 36.Lunt M, Emsley R, Pickles A, Dunn G. Implementing double-robust estimators of causal effects. Stata Journal. 2008;8(3):334–353. [Google Scholar]
- 37.Kurth T, Walker AW, Glynn RJ, Chan KA, Gaziano JM, Berger K, Robins JM. Results of multivariable logistic regression, propensity matching, propensity adjustment, and propensity-based weighting under conditions of nonuniform effect. American Journal of Epidemiology. 2006;163:262–270. doi: 10.1093/aje/kwj047. [DOI] [PubMed] [Google Scholar]
- 38.Hayes RJ, Moulton LH. Cluster Randomised Trials. Boca Raton, FL: Chapman and Hall; 2009. [Google Scholar]
- 39.Pronyk P, Hargreaves J, Kim J, et al. Effect of a structural intervention for the prevention of intimate-partner violence and HIV in rural South Africa: a cluster randomised trial. The Lancet. 2006;368(9551):1973–1983. doi: 10.1016/S0140-6736(06)69744-4. [DOI] [PubMed] [Google Scholar]
- 40.Pronyk P, Hargreaves J, Morduch J. Microfinance programs and better health: prospects for sub-Saharan Africa. JAMA. 2007;298(16):1925. doi: 10.1001/jama.298.16.1925. [DOI] [PubMed] [Google Scholar]