Abstract
Objective
To assess the feasibility of using birth attendants instead of bereaved mothers as perinatal verbal autopsy respondents.
Methods
Verbal autopsy interviews for early neonatal deaths and stillbirths were conducted separately among mothers (reference standard) and birth attendants in 38 communities in four developing countries. Concordance between maternal and attendant responses was calculated for all questions, for categories of questions and for individual questions. The sensitivity and specificity of individual questions with the birth attendant as respondent were assessed.
Findings
For early neonatal deaths, concordance across all questions was 94%. Concordance was at least 95% for more than half the questions on maternal medical history, birth attendance and neonate characteristics. Concordance on any given question was never less than 80%. Sensitivity and specificity varied across individual questions, more than 80% of which had a sensitivity of at least 80% and a specificity of at least 90%.
For stillbirths, concordance across all questions was 93%. Concordance was 95% or greater more than half the time for questions on birth attendance, site of delivery and stillborn characteristics. Sensitivity and specificity varied across individual questions. Over 60% of the questions had a sensitivity of at least 80% and over 80% of them had a specificity of at least 90%. Overall, the causes of death established through verbal autopsy were similar, regardless of respondent.
Conclusion
Birth attendants can substitute for bereaved mothers as verbal autopsy respondents. The questions in existing harmonized verbal autopsy questionnaires need further refinement, as their sensitivity and specificity differ widely.
Résumé
Objectif
Évaluer la faisabilité du recours aux sages-femmes (au lieu des mères endeuillées) pour répondre aux questions de l’autopsie verbale périnatale.
Méthodes
Des entretiens d’autopsie verbale en cas de décès néonataux précoces et de mort à la naissance ont été menés séparément chez des mères (norme de référence) et chez des sages-femmes dans 38 communautés de 4 pays en voie de développement. La concordance entre les réponses des mères et des sages-femmes a été calculée pour l’ensemble des questions, pour les catégories de questions et pour les questions individuelles. On a évalué la sensibilité et la spécificité des questions individuelles aux sages-femmes en tant que personnes interrogées.
Résultats
Pour les décès néonataux précoces, la concordance sur toutes les questions a atteint 94%. Elle était d’au moins 95% pour plus de la moitié des questions sur les antécédents médicaux maternels, l’accouchement et les caractéristiques du nouveau-né. La concordance sur une question donnée n’a jamais été inférieure à 80%. La sensibilité et la spécificité variaient selon les questions individuelles, et 80% d’entre elles présentaient une sensibilité d’au moins 80% et une spécificité d’au moins 90%.
Pour les enfants morts-nés, la concordance sur l’ensemble des questions était de 93%. Elle était supérieure ou égale à 95%, plus de la moitié du temps, pour les questions sur l’accouchement, le lieu de la naissance et les caractéristiques de l’enfant mort-né. La sensibilité et la spécificité variaient selon les questions individuelles. Plus de 60% des questions présentaient une sensibilité d’au moins 80%, et plus de 80% d’entre elles une spécificité d’au moins 90%. Dans l’ensemble, les causes de la mort établies par autopsie verbale étaient similaires, quelle que soit la personne interrogée.
Conclusion
Les sages-femmes peuvent replacer les mères endeuillées et répondre aux questions de l’autopsie verbale. Les questions des questionnaires d’autopsie verbale harmonisés existants nécessitent une amélioration supplémentaire, car généralement, leur sensibilité et leur spécificité diffèrent grandement.
Resumen
Objetivo
Evaluar la viabilidad de utilizar matronas como encuestadas en autopsias verbales perinatales en lugar de madres que han perdido un hijo/a.
Métodos
Las entrevistas para las autopsias verbales de muertes neonatales prematuras y alumbramientos mortinatos se realizaron por separado entre madres (estándar de referencia) y matronas en 38 comunidades de cuatro países en desarrollo. Se calculó la concordancia entre las respuestas maternas y las respuestas de las matronas para todas las preguntas, tanto para las categorías de preguntas como para las preguntas individuales. Se evaluaron la sensibilidad y especificidad de las preguntas individuales con la matrona como encuestada.
Resultados
En las muertes neonatales prematuras, la concordancia en todas las preguntas fue del 94%. La concordancia fue de al menos el 95% para más de la mitad de las preguntas sobre el historial médico materno, atención en el parto y características neonatales. La concordancia de cualquier pregunta determinada no fue en ningún caso inferior al 80%. La sensibilidad y la especificidad variaron en las preguntas individuales. En este caso, más del 80% de las preguntas presentaron una sensibilidad de al menos el 80% y una especificidad de al menos el 90%.
En cuanto a los alumbramientos mortinatos, la concordancia en todas las preguntas fue del 93%. La concordancia fue del 95% o más durante más de la mitad del tiempo para preguntas relacionadas con la atención en el parto, el centro de parto y las características de la mortinatalidad. La sensibilidad y especificidad variaron en las preguntas individuales. Más del 60% de las preguntas presentaron una sensibilidad de al menos el 80%. En este caso, más del 80% de las preguntas presentaron una especificidad de al menos el 90%. Globalmente, las causas de muerte establecidas mediante autopsia verbal fueron similares, independientemente de la persona encuestada.
Conclusión
Las matronas pueden sustituir a las madres que han perdido un hijo/a como encuestadas en autopsias verbales. Es necesario perfeccionar las preguntas de los cuestionarios de autopsia verbal armonizados existentes, ya que su sensibilidad y especificidad difieren ampliamente.
ملخص
الغرض
تقييم جدوى الاستعانة بالقابلات بدلاً من الأمهات اللاتي فقدن مواليدهن كمستجيبات للتشريح الشفوي في الفترة المحيطة بالولادة.
الطريقة
تم إجراء مقابلات التشريح الشفوي لحالات الوفاة المبكرة للمواليد والمواليد الموتى على نحو منفصل بين الأمهات (المعيار المرجعي) والقابلات في 38 مجتمعًا محليًا في أربعة بلدان نامية. تم حساب التوافق بين استجابات الأمهات والقابلات بالنسبة لجميع الأسئلة، وبالنسبة لفئات الأسئلة، وبالنسبة للأسئلة الفردية. وتم تقييم حساسية وخصوصية الأسئلة الفردية مع القابلة كمستجيبة.
النتائج
بالنسبة لحالات الوفاة المبكرة، بلغ التوافق عبر جميع الأسئلة 94 %. وبلغ التوافق 95 % على الأقل لما يزيد عن نصف الأسئلة الخاصة بالتاريخ الطبي للأم والقبالة وخصائص حديثي الولادة. ولم يقل التوافق على أي سؤال محدد عن 80 % على الإطلاق. وتنوعت الحساسية والخصوصية عبر الأسئلة الفردية، حيث كان لدى أكثر من 80 % منها حساسية بنسبة 80 % على الأقل وخصوصية بنسبة 90 % على الأقل.
وبالنسبة للمواليد الموتى، بلغ التوافق عبر جميع الأسئلة 93 %. وبلغ التوافق 95 % أو أعلى أكثر من نصف الوقت فيما يتعلق بالأسئلة الخاصة بالقبالة ومكان الولادة وخصائص المولود الميت. وتنوعت الحساسية والخصوصية عبر الأسئلة الفردية. وكانت لدى ما يزيد عن 60 % من الأسئلة حساسية بنسبة 80 % على الأقل وكانت لدى ما يزيد عن 80 % منها خصوصية بنسبة 90 % على الأقل. بشكل عام، تشابهت أسباب الوفاة التي تم تحديدها من خلال التشريح الشفوي، بغض النظر عن المستجيبة.
الاستنتاج
من الممكن أن تحل القابلات محل الأمهات اللاتي فقدن مواليدهن كمستجيبات للتشريح الشفوي. وتحتاج الأسئلة الواردة في استبيانات التشريح الشفوي المنسقة الحالية إلى مزيد من التنقيح، نظرًا للاختلاف الواسع بين الحساسية والخصوصية فيما بينها.
摘要
目的
评估让接生员而非丧生母亲作为围产期口头尸检调查对象的可行性。
方法
在四个发展中国家的 38 个社区的母亲(参考标准)和接生员中展开早期新生儿死亡和死产的口头尸检面谈。计算母亲和接生员对所有问题、各类问题和各个问题的回答之间的一致性。评估接生员调查对象各个问题的敏感度和特异性。
结果
对于早期新生儿死亡,所有问题的一致性为 94%。半数以上有关母亲病史、接生员和婴儿特征的问题的一致性不低于 95%。任何给定问题的一致性不低于 80%。各个问题的敏感度和特异性不同,其中超过 80% 问题的敏感度至少为 80%,特异性至少为 90%。
对于死产,所有问题的一致性为 93%。半数以上有关接生员、分娩地点和死产特征的问题的一致性不低于 95%。各个问题的敏感度和特异性不同。超过 60% 的问题的敏感度至少为 80%,超过 80% 的问题特异性至少 90%。 总体而言,无论谁是调查对象,通过口头尸检确定的死亡原因相似。
结论
接生员可以替代丧生母亲作为口头尸检调查对象。因为敏感度和特异性差异很大,需要进一步提炼现有经过协调的口头尸检问卷调查中的问题。
Резюме
Цель
Оценить возможность использования акушерок вместо лишившихся детей матерей, для проведения вербальной аутопсии в случаях перинатальной смертности.
Методы
Интервью для проведения вербальной аутопсии в случаях ранней неонатальной смертности и мертворождений проводились отдельно среди матерей (образец для сравнения) и акушерок в 38 общинах 4-х развивающихся стран. Был рассчитан процент соответствия ответов матерей и акушерок для всех вопросов, категорий вопросов и отдельных вопросов. Были оценены параметры чувствительности и специфичности отдельных вопросов для акушерок, участвующих в опросе.
Результаты
Для случаев неонатальной смертности, соответствие по всем вопросам составило 94%. Соответствие составило минимум 95% для более чем половины вопросов, относящихся к данным медицинской карты матери, ходу родов и характеристикам новорожденного. Соответствие при ответах все вопросы ни разу не составляло менее 80%. Для отдельных вопросов уровни чувствительности и специфичности варьировались, для более чем 80% вопросов уровень чувствительности составил не менее 80%, а уровень специфичности – не менее 90%.
Для случаев мертворождений, соответствие по всем вопросам составило 93%. Для более чем половины случаев соответствие достигало уровня 95% и выше при ответах на вопросы о родовспоможении, месте родов и характеристиках мертворожденных детей. Уровни чувствительности и специфичности варьировались в зависимости от индивидуальных вопросов. Более 60% вопросов имело уровень чувствительности не менее 80% и более 80% вопросов имело уровень специфичности не менее 90%. В целом, причины смерти, установленные путем вербальной аутопсии, были схожи, независимо от того, кто отвечал на вопросы.
Вывод
Акушерки могут заменить потерявших детей матерей в качестве респондентов при проведении вербальной аутопсии. Вопросы в существующих унифицированных анкетах по вербальной аутопсии нуждаются в дальнейшей доработке, так как показатели уровней чувствительности и специфичности ответов отличаются друг от друга.
Introduction
Of the approximately 8.8 million deaths that occur annually in children under 5 years of age, 41% occur in neonates.1 A child is 45 times more likely to die within the first 28 days of life than in the entire period from 28 days to 5 years of age.2 Three quarters of all neonatal deaths, or approximately 2.7 million deaths annually, occur during the first seven days of life and are termed early neonatal deaths.3 In addition, an estimated 2.7 million stillbirths occur annually.4–6 Early neonatal deaths and stillbirths, which together comprise what are termed perinatal deaths, account for the highest proportion of deaths among children less than 15 years of age. In this age group, they account for twice as many deaths as malaria and human immunodeficiency virus (HIV) infection combined.7 Over 98% of perinatal deaths occur in low- and middle-income countries and more than two thirds occur in community settings, frequently at home.8,9 These deaths that take place outside the formal health-care system are rarely included in the vital registers.10,11 In fact, vital registration data are unavailable for over 97% of perinatal deaths, yet such data are necessary for designing measures to reduce perinatal mortality. A coherent health policy based on accurate information needs to be developed to address the most common causes of perinatal death.7,12
Verbal autopsy is one of various techniques that have been developed to compensate for the lack of data on the causes of deaths that occur in community settings.13 It is an indirect method of ascertaining the cause of death where civil registration and health systems are weak.14 During a verbal autopsy conducted to investigate the causes of a perinatal death, a systematic description of the signs, symptoms and circumstances preceding the death is obtained through an interview with the primary caregiver, traditionally the mother, of a lost fetus or child who has died.15 In most cases a physician panel uses the data thus obtained to ascertain the cause of death. Less commonly, the cause of death is established by using algorithms, neural networks or probabilistic approaches to interpret these data.16–18 Verbal autopsy has been validated against more conventional methods for establishing the cause of death and it is used in large surveillance programmes and vital registration systems.19
Traditionally, the perinatal verbal autopsy respondent is the mother whose neonate or fetus has died. However, birth attendants could make better verbal autopsy respondents than mothers for several reasons: (i) they may be more aware than mothers of the circumstances surrounding the birth; (ii) they are often the first to attempt resuscitation and often have greater insight than the mother into the events that led to the death. Often the circumstances surrounding such deaths become embedded in the memory of birth attendants who live in the same community as the mother. For these reasons, our group undertook a prospective study to investigate whether birth attendants could be a suitable alternative to mothers as respondents during perinatal verbal autopsies. Our a priori hypothesis was that mothers’ and birth attendants’ responses to selected close-ended items on the verbal autopsy questionnaire would show more than 80% concordance.
Methods
Study design, setting and subjects
This prospective observational study based on verbal autopsy was an ancillary study to the FIRST BREATH Trial, conducted by the Eunice Kennedy Shriver National Institute of Child Health and Human Development’s Global Network for Women’s and Children’s Health Research. 20 The FIRST BREATH Trial was a cluster-randomized, controlled trial that investigated the effects of implementing a package of neonatal care practices and neonatal resuscitation in community settings.
Our verbal autopsy study included 38 communities in the Democratic Republic of the Congo (Equateur province), Guatemala (Chimaltenango province), Pakistan (Thatta district) and Zambia (Kafue district). Each community was a geographically defined area consisting of a cluster of villages with approximately 300 to 500 deliveries per year. For every birth enrolled in the FIRST BREATH Trial, birth attendants collected data on fetal monitoring, birth weight, APGAR score, any resuscitation required, and the use of bag or mask ventilation. The data were then reviewed for correct procedure by trained nurses (with 3 to 4 years of health training) or community health workers (high school graduates with 18 months of health training), who were designated as community coordinators.
Within one week of the occurrence of an early neonatal death or stillbirth in a community, birth attendants notified community coordinators, who then visited the family, determined its eligibility for participation in our study, and requested consent from eligible mothers. The family was excluded from participating in the study if: the birth or death took place in hospital; the delivery occurred without the presence of a birth attendant; the mother was unavailable for any reason (including peripartum death); or the mother could not be enrolled in the study within seven days of the perinatal death. A seven day enrolment window was chosen to reduce the possibility of recall bias.15,19,21 Because the mother is traditionally the respondent during perinatal verbal autopsies, we included only cases in which the mothers were available for interview. Because this study was community-based, hospital-based deliveries were excluded. Informed consent was obtained from mothers in a private and confidential setting. The consent form was read to all mothers, who were asked to sign it or, if illiterate, to affix their thumbprints. Community birth attendants participated in the study also. In addition to the mothers, birth attendants also participated in the study. They included untrained traditional birth attendants, certified traditional birth attendants, nurses and nurse midwives. Physicians were excluded from the study.
Uniform data describing the circumstances surrounding a perinatal death were collected separately from each mother and from each birth attendant using a standardized verbal autopsy questionnaire developed specifically for this study from a validated verbal autopsy tool.2,22,23 Broadly, the questionnaire covered the following categories: (i) maternal medical history; (ii) parturition history; (iii) birth attendance and site of delivery; (iv) characteristics of the neonate or stillborn, and (v) early neonatal period. The order of interviewing birth attendants and mothers was alternated in each community to reduce potential bias. The interview responses were then analysed by two local physicians who independently assigned an underlying cause of death. Discrepancies between physicians in the assigned cause of death were resolved through discussion and the cause of death was established by consensus. Interview responses provided by the birth attendants were validated by comparing them with those provided by the mothers, which were treated as a gold standard.
Respondents included in this analysis
During the verbal autopsy interview, the mother and birth attendant were asked whether the baby was dead or alive when born (i.e. whether a stillbirth or an early neonatal death had occurred). Because the interview included detailed questions about the circumstances that existed before and during the death, the perceived time of death (i.e. before or after birth) may have influenced participant responses. To avoid the difficulty of interpreting results when the mother and the birth attendant had a different perception of the time of death, we restricted our analyses to the subset of deaths on whose timing the mother and the birth attendant were in agreement.
Data collection and analysis
Data were entered and transmitted electronically to the data coordinating centre (Research Triangle Institute, Durham, United States of America), where data edits, including inter- and intra-form consistency checks, were performed. The study was reviewed and approved by the institutional ethics review committees of the Research Triangle Institute, the University of North Carolina at Chapel Hill and in-country institutional review boards. Data were analysed using SAS version 9.2 (SAS Institute, Cary, USA).
Responses were defined as concordant when both the mother and the birth attendant answered yes, no or don’t know. For all non-missing responses, the percentage of concordance between the mothers’ and birth attendants’ responses to the individual questions posed during the interviews was calculated. Overall concordance was estimated by adding the percentage of concordant responses on all individual questions and dividing the result by the number of questions. The mothers’ responses were viewed as the reference standard for calculating the sensitivity (proportion of true positives correctly identified as such) and specificity (proportion of true negatives correctly identified as such) of each question when the birth attendant was the respondent. These measures were calculated using conventional two-by-two table analysis. Responses of don’t know by the mother were excluded from the sensitivity and specificity calculation, as they would only lead to an inconclusive diagnosis. Responses of don’t know by the birth attendant to questions to which the mother replied either yes or no were considered incorrect (i.e. either a false positive or a false negative).
Results
The FIRST BREATH trial was conducted between March 2005 and August 2008, and this verbal autopsy study took place from May 2007 to June 2008. A total of 9461 births occurred in the designated communities during this period. There were 518 perinatal deaths among these births, and 81 of them were ineligible for the study because the delivery occurred in a hospital (79) or the birth attendant was absent at the time of delivery (2). Of the 437 eligible deaths, 185 were not enrolled in the study because the mother was not available for interview within seven days after the death (145) or did not provide consent (40). This left a total of 252 perinatal deaths (from 241 deliveries, some of them multiple) that were eligible for participation and for which consent was granted. Our final sample for this analysis included the 234 deliveries (245 perinatal deaths: 134 stillbirths and 111 early neonatal deaths) for which there was concordance between the mother and the birth attendant as to the time of the death (i.e. stillbirth versus early neonatal death). Seven deaths were omitted due to discordance in this respect.
Table 1 provides the sociodemographic characteristics of the mothers by birth outcome. Mothers that experienced an early neonatal death or a stillbirth were similar in terms of age, parity, education and marital status. Mothers who experienced a stillbirth had a breech delivery significantly more often than those who experienced a neonatal death (P = 0.04). The place of delivery and type of birth attendant were similar in both groups.
Table 1. Characteristics of mothers, deliveries and pregnancies in study of perinatal verbal autopsy, by birth outcomea.
| Characteristic | No. early neonatal death (%)b | No. stillbirth (%)b | Total (%)b |
|---|---|---|---|
| No. of mothers | 106 | 128 | 234 |
| Age (years) | 104 | 123 | 227 |
| < 20 | 18 (17.3) | 17 (13.8) | 35 (15.4) |
| 20–35 | 76 (73.1) | 91 (74.0) | 167 (73.6) |
| > 35 | 10 (9.6) | 15 (12.2) | 25 (11.0) |
| Parity (excluding current pregnancy), mean and SD | 2.6 (2.9) | 3.1 (2.9) | 2.9 (2.9) |
| Formal schooling completed | 105 | 127 | 232 |
| None, illiterate | 56 (53.3) | 67 (52.8) | 123 (53.0) |
| None, literate/primary | 38 (36.2) | 48 (37.8) | 86 (37.1) |
| Some secondary/university | 11 (10.5) | 12 (9.4) | 23 (9.9) |
| Mother with partner or spouse | 98 (92.5) | 122 (96.1) | 220 (94.4) |
| Mother received prenatal carec | 97 (91.5) | 107 (84.3) | 204 (87.6) |
| Mode of delivery | 106 | 128 | 234 |
| Vaginal vertex | 99 (93.4) | 108 (84.4) | 207 (88.5) |
| Vaginal breech | 7 (6.6) | 20 (15.6) | 27 (11.5) |
| Location of delivery | 106 | 128 | 234 |
| Home | 55 (51.9) | 71 (55.5) | 126 (53.8) |
| Clinic | 27 (25.5) | 28 (21.9) | 55 (23.5) |
| Birth attendant’s home | 24 (22.6) | 28 (21.9) | 52 (22.2) |
| En route to hospital | 0 (0.0) | 1 (0.8) | 1 (0.4) |
| Birth attendant | 106 | 128 | 234 |
| Nurse or midwife | 28 (26.4) | 28 (21.9) | 56 (23.9) |
| Traditional birth attendant, certified | 61 (57.5) | 79 (61.7) | 140 (59.8) |
| Traditional birth attendant, untrained | 17 (16.0) | 21 (16.4) | 38 (16.2) |
| Current pregnancy | 106 | 128 | 234 |
| Woman had twins/triplets | 7 (6.6) | 6 (4.7) | 13 (5.6) |
| Deaths among twins/triplets | 7 | 6 | 13 |
| All babies died | 3 (42.9) | 3 (50.0) | 6 (46.2) |
| One baby died | 4 (57.1) | 3 (50.0) | 7 (53.8) |
SD, standard deviation.
a All values in the table are absolute numbers and percentages unless otherwise indicated.
b The denominator used to derive each percentage is the total number of women in the particular category. For example, the denominator used to derive the percentage of illiterate women who experienced a stillbirth (52.8%) is the total number of women who experienced a stillbirth and whose educational level is known (i.e. 127). Denominators vary because missing and don’t know responses for specific items are excluded from the denominators.
c Other than from a traditional birth attendant.
Note: The table is restricted to the subset of deaths for which maternal and birth attendant responses to questions on the time of death (i.e. stillbirth versus early neonatal death) were concordant.
Early neonatal death
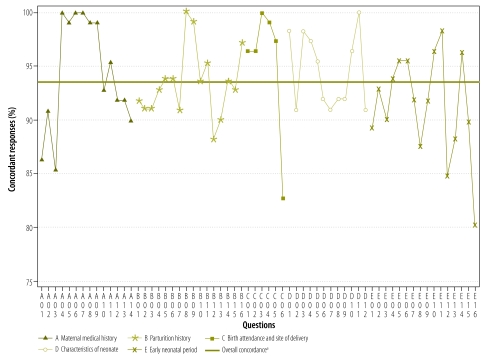
Fig. 1 provides a graphical summary of the percentage of concordant responses to individual interview questions, with the mothers’ responses used as the reference standard. Questions A1–14, B1–16, C1–6, D1–12 and E1–16 marked along the x-axis correspond to the questions and responses presented in Appendix A (available at: http://gn.rti.org/literature/index.cfm?fuseaction=pubDetail&ID=1563). Concordance across all questions was 91%, 94% and 95% among nurses/nurse midwives, certified traditional birth attendants and untrained traditional birth attendants, respectively. Since beyond this level of analysis the sample size for each type of birth attendant became too small to permit stratification and further statistical analyses, henceforth we combine birth attendants of all types when reporting concordance. Concordance across all questions was 94%. Concordance was 95% or greater for at least half of the questions in the categories for maternal medical history, birth attendance and neonate characteristics. Concordance varied most widely for responses to questions pertaining to the early neonatal period (80–95%), whereas it varied the least for responses to questions about the characteristics of the neonate (92–99%). Concordance was 80% for one question (E16: baby was cold to the touch) and greater than 80% for all other questions.
Fig. 1.
Concordance between responses to individual verbal autopsy questions given by birth attendants and by mothers who experienced an early neonatal death
a Overall concordance was calculated by adding the percentages of concordant responses to individual questions and dividing the result by the number of questions.
Note: The figure is restricted to the subset of deaths for which maternal and birth attendant responses to questions on the time of death (i.e. stillbirth versus early neonatal death) were concordant. Questions A1–14, B1–16, C1–6, D1–12 and E1–16 correspond to responses presented in Appendix A.
Appendix A compares the responses given by the mothers and the birth attendants to the verbal autopsy questions. The shaded cells show concordant responses to specific questions. Sensitivity (in parentheses) is provided for each characteristic in the top left cell (where the column for a maternal yes response overlaps with a yes response by the birth attendant). Sensitivity ranged from 0.33 for Question D2 (i.e. the baby had an odour at birth) to 1.00 for 16 of the 60 questions to which at least one mother answered yes. Of the total of 60 questions, 50 had a sensitivity of 80% or more. Specificity is provided for each characteristic in the middle cell (where the column for a maternal no answer overlaps with a no answer by a birth attendant). Specificity ranged from 0.52 for Question C6 (i.e. the mother had received tetanus toxoid when first pregnant) to 1.00 for 12 of the 64 questions to which at least one mother answered no. Of the total of 64 questions, 52 had a specificity of 90% or more.
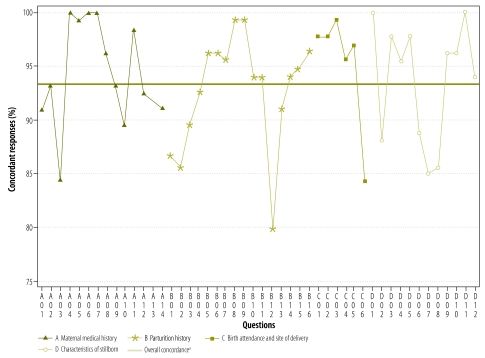
Stillbirth
Fig. 2 provides a graphical summary of the percentage of concordant responses to individual interview questions, with the mothers’ responses used as the reference standard. Questions A1–14, B1–16, C1–6, and D1–12 marked along the x-axis correspond to the questions and responses presented in Appendix B (available at: http://gn.rti.org/literature/index.cfm?fuseaction=pubDetail&ID=1563). As was the case for early neonatal deaths, we hypothesized that the birth attendant’s response would be concordant with the mother’s more than 80% of the time. Concordance across all questions was 92%, 93%, and 96% for nurses/nurse midwives, certified traditional birth attendants and untrained traditional birth attendants, respectively. Since beyond this level of analysis the sample size for each type of birth attendant became too small to permit stratification and further statistical analyses, henceforth we combine birth attendants of all types when reporting concordance. Concordance across all questions was 93%. Concordance was 95% or greater for at least half of the questions in the categories for birth attendance and site of delivery and characteristics of the stillborn. Concordance varied most widely for responses to questions pertaining to parturition history (80–99%), whereas it varied the least for responses to questions about the characteristics of the stillborn (85–100%). Concordance was less than 80% for Question A13 (i.e. baby moved in womb before birth) and 75% for question B12 (i.e. vaginal odour present), but it was greater than 80% for all other questions.
Fig. 2.
Concordance between responses given to individual verbal autopsy questions by birth attendants and by mothers who experienced a stillbirth
a Overall concordance was calculated by adding the percentages of concordant responses to individual questions and dividing the result by the number of questions.
Note: The figure is restricted to the subset of deaths for which maternal and birth attendant responses to questions on the time of death (i.e. stillbirth versus early neonatal death) were concordant. Questions A1–14, B1–16, C1–6 and D1–12 correspond to responses presented in Appendix B.
Appendix B compares the responses given by the mothers and the birth attendants to the verbal autopsy questions. Sensitivity ranged from 0.29 for Question A8 (i.e. mother had suffered abdominal trauma or accident) to 1.00 for 8 of the 44 questions to which at least one mother answered yes. Of the total of 48 questions, 31 had sensitivities of 80% or more. Question D9 (i.e. the child’s arms/legs had strength) also had poor sensitivity (0.33). Specificity ranged from 0.69 for Question A12 (i.e. mother had received antenatal care other than from a traditional birth attendant) to 1.00 for 9 of the 47 questions to which at least one mother replied no. Of the total of 48 questions, 40 had a specificity of 90% or more.
Discussion
Our results show that the responses given by mothers and birth attendants to nearly all questions on the perinatal verbal autopsy questionnaire are highly concordant (80% or greater agreement) when the interviews take place within seven days after the perinatal death. This suggests that interviewing birth attendants instead of mothers may be a suitable alternative for collecting data for verbal autopsy. Using birth attendants instead of mothers as perinatal verbal autopsy respondents has potential advantages from the public health, economic, logistical, emotional and ethical perspectives. Current perinatal verbal autopsy methods are such that interviewers sometimes have to travel long distances to collect information for verbal autopsy from bereaved mothers living outside their communities.13,15,19 The process can take months, is relatively expensive and involves extensive logistical planning.18,24 Additionally, in the early stages of planning, community leaders often have to attend sessions where they learn about verbal autopsy, which is generally unfamiliar to them. All of this increases the logistical and economic burden of conducting perinatal verbal autopsy.19 Using birth attendants instead of mothers as respondents shortens the verbal autopsy process and hence decreases costs and minimizes logistical planning. For example, birth attendants from the same region could all be interviewed in a single location within a given time period. This would allow verbal autopsy interviews to be conducted at scale in resource-constrained countries. One limitation to this approach is that perinatal verbal autopsy can only be conducted for deliveries occurring in the presence of a birth attendant, and in rural communities not all deliveries are attended.
Some authors have discussed the pros and cons of using bereaved parents as verbal autopsy respondents. In many rural settings strong cultural beliefs (e.g. that the deceased child was a “spirit child”) preclude any discussion of the deceased neonate.25 Furthermore, because many children have not been given a name before they die, such children are not considered born in a social or cultural sense. Hence, people fear that discussing them will invoke malevolent spirits who will become manifest in subsequent deliveries.2,26,27 Other authors have reported that in areas with weak medical services and poor service uptake by community members, bereaved mothers are reluctant to complete lengthy questionnaires because they fail to see their utility.28,29 It has also been reported that although mothers are able to retrospectively report the signs and symptoms of an infant’s illness, they may be unable to gauge their severity.27 These are some of the reasons that highlight the potential role of birth attendants as verbal autopsy respondents.
When concordance was examined by question category, it was found to be 95% or more for at least half of the questions on birth attendance and site of delivery and on stillborn/neonate characteristics. This is not surprising, since these categories cover the period when the birth attendant is usually present. By contrast, a concordance of 95% was found much less often on the questions on parturition history, perhaps because birth attendants may have arrived after the onset of labour. Nonetheless, it is clear that concordance varied widely for different categories of questions.
In our study, individual questions were found to vary in their sensitivity and specificity when the respondent was the birth attendant. Certain questions had high sensitivity and specificity. This was true of the questions on sepsis: “Did waters break one or more days before delivery?” “Did the mother have a fever?” and “Was there a vaginal odour”? By contrast, the following questions had low sensitivity: “Was the child coughing?” and “Did eye colour change to yellow”? These findings suggest that in harmonized verbal autopsy tools, each question can be “weighted” both for its importance in establishing the cause of death and for its sensitivity and specificity when birth attendants are used as verbal autopsy respondents. Alternatively, the perinatal verbal autopsy questionnaire could be further refined by eliminating questions with low response concordance and using only questions with high sensitivity and specificity when the respondent is a birth attendant.
New verbal autopsy tools have been introduced since this study was conducted. They include, for example, harmonized verbal autopsy tools recently published by the World Health Organization and the Institute for Health Metrics and Evaluation.30 We believe that if these tools, which are broadly similar to ours, were used, they would yield results very similar to those obtained in this study.
This study has several strengths. Verbal autopsy interviewers received standardized training, and the use of the same interviewer for the mother and the birth attendants reduced the likelihood of interviewer bias. Bias was also reduced by alternating the order of the interviews with the mothers and birth attendants. Mothers and birth attendants were interviewed within seven days of a perinatal death to preclude recall bias. We reiterate that this particular study was not designed to establish the cause of death, which we address in a separate publication.23 The objective of this study was to find out how birth attendant responses compare with mothers’ responses on verbal autopsy interviews, and to this end we applied very stringent inclusion and exclusion criteria. The study also has limitations. The stringent inclusion and exclusion criteria and the use of currently accepted verbal autopsy tools may limit the widespread applicability of the findings. Only cases in which mothers and birth attendants agreed on the time of death (stillbirth versus early neonatal death) were included in our study, but disagreement was minimal (only 7 of 245 cases). Respondent bias may have confounded the results because respondents may have given answers that reduced their culpability in a death. We addressed this in the trial by systematically emphasizing during all phases of training and during the interview that accurate reporting of the facts surrounding each perinatal death was critical to the successful completion of the study and that there would be no incrimination by truthful disclosure. It is possible, since no two communities are alike, that the use of birth attendants as verbal autopsy respondents will be more successful in some communities than in others.
Conducting verbal autopsy interviews with the frequency required to capture perinatal deaths within seven days of delivery may pose logistical challenges to a health system. Further research is needed to determine whether similar results would be obtained if interviews were conducted more than one week after a perinatal death. Finally, our results are only applicable to cases of stillbirth and early neonatal death in which a birth attendant was present during the birth.
Conclusion
In settings where most deaths occur outside the health system, verbal autopsy is used as a real-world, data information system and may be the only practical, available tool for describing the cause of death. Our results suggest that during perinatal verbal autopsy birth attendants can be used as surrogates for bereaved mothers. This has important implications for low-income countries from a public health, economic and logistical perspective. Although it may be premature to recommend widespread use of birth attendants as perinatal verbal autopsy respondents, we recommend, based on our findings, that further research be performed using existing harmonized perinatal verbal autopsy questionnaires to assess whether our findings would be replicable if the interviews were conducted more than seven days after a perinatal death.
Funding:
Funding was provided by grants from the National Institutes of Child Health and Human Development (U01 HD043475, U01 HD040636, U01 HD043464, U01 HD040607, U01 HD040657 and U01 HD043475-03S1).
Competing interests:
None declared.
References
- 1.Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, Bassani DG, et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet. 2010;375:1969–87. doi: 10.1016/S0140-6736(10)60549-1. [DOI] [PubMed] [Google Scholar]
- 2.Engmann C. Improving neonatal mortality in sub-Saharan Africa: any cause for optimism? J Perinatol. 2011;31:745–748. doi: 10.1038/jp.2011.53. [DOI] [PubMed] [Google Scholar]
- 3.Lawn JE, Cousens S, Zupan J. 4 million neonatal deaths: When? Where? Why? Lancet. 2005;365:891–900. doi: 10.1016/S0140-6736(05)71048-5. [DOI] [PubMed] [Google Scholar]
- 4.Lawn J, Shibuya K, Stein C. No cry at birth: global estimates of intrapartum stillbirths and intrapartum-related neonatal deaths. Bull World Health Organ. 2005;83:409–17. [PMC free article] [PubMed] [Google Scholar]
- 5.Lawn JE, Lee AC, Kinney M, Sibley L, Carlo WA, Paul VK, et al. Two million intrapartum-related stillbirths and neonatal deaths: where, why, and what can be done? Int J Gynaecol Obstet. 2009;107:S5–18. doi: 10.1016/j.ijgo.2009.07.016. [DOI] [PubMed] [Google Scholar]
- 6.Lawn JE, Blencowe H, Pattinson R, Cousens S, Kumar R, Ibiebele I, et al. Stillbirths: Where? When? Why? How to make the data count? Lancet. 2011;377:1448–63. doi: 10.1016/S0140-6736(10)62187-3. [DOI] [PubMed] [Google Scholar]
- 7.Lopez AD, Mathers CD. Measuring the global burden of disease and epidemiological transitions: 2002-2030. Ann Trop Med Parasitol. 2006;100:481–99. doi: 10.1179/136485906X97417. [DOI] [PubMed] [Google Scholar]
- 8.Mathers CD, Fat DM, Inoue M, Rao C, Lopez AD. Counting the dead and what they died from: an assessment of the global status of cause of death data. Bull World Health Organ. 2005;83:171–7. [PMC free article] [PubMed] [Google Scholar]
- 9.Darmstadt GL, Lee AC, Cousens S, Sibley L, Bhutta ZA, Donnay F, et al. 60 Million non-facility births: who can deliver in community settings to reduce intrapartum-related deaths? Int J Gynaecol Obstet. 2009;107(Suppl 1):S89–112. doi: 10.1016/j.ijgo.2009.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lawn JE, Osrin D, Adler A, Cousens S. Four million neonatal deaths: counting and attribution of cause of death. Paediatr Perinat Epidemiol. 2008;22:410–6. doi: 10.1111/j.1365-3016.2008.00960.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Setel PW, Macfarlane SB, Szreter S, Mikkelsen L, Jha P, Stout S, et al. A scandal of invisibility: making everyone count by counting everyone. Lancet. 2007;370:1569–77. doi: 10.1016/S0140-6736(07)61307-5. [DOI] [PubMed] [Google Scholar]
- 12.Engmann C, Matendo R, Kinoshita R, Ditekemena J, Moore J, Goldenberg RL, et al. Stillbirth and early neonatal mortality in rural Central Africa. Int J Gynaecol Obstet. 2009;105:112–7. doi: 10.1016/j.ijgo.2008.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Garenne M, Fauveau V. Potential and limits of verbal autopsies. Bull World Health Organ. 2006;84:164. doi: 10.2471/BLT.05.029124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thatte N, Kalter HD, Baqui AH, Williams EM, Darmstadt GL. Ascertaining causes of neonatal deaths using verbal autopsy: current methods and challenges. J Perinatol. 2009;29:187–94. doi: 10.1038/jp.2008.138. [DOI] [PubMed] [Google Scholar]
- 15.Soleman N, Chandramohan D, Shibuya K. Verbal autopsy: current practices and challenges. Bull World Health Organ. 2006;84:239–45. doi: 10.2471/BLT.05.027003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Byass P, D'Ambruoso L, Ouedraogo M, Qomariyah SN. Assessing the repeatability of verbal autopsy for determining cause of death: two case studies among women of reproductive age in Burkina Faso and Indonesia. Popul Health Metr. 2009;7:6. doi: 10.1186/1478-7954-7-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.King G, Lu Y, Shibuya K. Designing verbal autopsy studies. Popul Health Metr. 2010;8:19. doi: 10.1186/1478-7954-8-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Murray CJ, Lopez AD, Feehan DM, Peter ST, Yang G. Validation of the symptom pattern method for analyzing verbal autopsy data. PLoS Med. 2007;4:e327. doi: 10.1371/journal.pmed.0040327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fottrell E, Byass P. Verbal autopsy: methods in transition. Epidemiol Rev. 2010;32:38–55. doi: 10.1093/epirev/mxq003. [DOI] [PubMed] [Google Scholar]
- 20.Carlo WA, Goudar SS, Jehan I, Chomba E, Tshefu A, Garces A, et al. Newborn-care training and perinatal mortality in developing countries. N Engl J Med. 2010;362:614–23. doi: 10.1056/NEJMsa0806033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee AC, Mullany LC, Tielsch JM, Katz J, Khatry SK, LeClerq SC, et al. Verbal autopsy methods to ascertain birth asphyxia deaths in a community-based setting in southern Nepal. Pediatrics. 2008;121:e1372–80. doi: 10.1542/peds.2007-2644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Engmann C, Jehan I, Ditekemena J, Garces A, Phiri M, Mazariegos M, et al. Using verbal autopsy to ascertain perinatal cause of death: are trained non-physicians adequate? Trop Med Int Health. 2009;14:1496–504. doi: 10.1111/j.1365-3156.2009.02395.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Engmann C, Jehan A, Ditekemena I, Phiri M, Mazariegos M.Causes of community stillbirths and early neonatal deaths in low-income countries using verbal autopsy: an international, multicenter study. J PerinatolEpub2011. Nov 10 10.1038/jp.2011.154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Joshi R, Kengne AP, Neal B. Methodological trends in studies based on verbal autopsies before and after published guidelines. Bull World Health Organ. 2009;87:678–82. doi: 10.2471/BLT.07.049288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Denham AR, Adongo PB, Freydberg N, Hodgson A. Chasing spirits: clarifying the spirit child phenomenon and infanticide in Northern Ghana. Soc Sci Med. 2010;71:608–15. doi: 10.1016/j.socscimed.2010.04.022. [DOI] [PubMed] [Google Scholar]
- 26.Adetunji JA. Preserving the pot and water: a traditional concept of reproductive health in a Yoruba community, Nigeria. Soc Sci Med. 1996;43:1561–7. doi: 10.1016/S0277-9536(96)00052-4. [DOI] [PubMed] [Google Scholar]
- 27.Winch PJ, Alam MA, Akther A, Afroz D, Ali NA, Ellis AA, et al. Local understandings of vulnerability and protection during the neonatal period in Sylhet District, Bangladesh: a qualitative study. Lancet. 2005;366:478–85. doi: 10.1016/S0140-6736(05)66836-5. [DOI] [PubMed] [Google Scholar]
- 28.Kaufman JS, Asuzu MC, Rotimi CN, Johnson OO, Owoaje EE, Cooper RS. The absence of adult mortality data for sub-Saharan Africa: a practical solution. Bull World Health Organ. 1997;75:389–95. [PMC free article] [PubMed] [Google Scholar]
- 29.Asuzu MC, Johnson OO, Owoaje EE, Rotimi CN, Kaufman JS, Cooper RS. Questions on adult mortality. World Health Forum. 1996;17:373–6. [PubMed] [Google Scholar]
- 30.Baiden F, Bawah A, Biai S, Binka F, Boerma T, Byass P, et al. Setting international standards for verbal autopsy. Bull World Health Organ. 2007;85:570–1. doi: 10.2471/BLT.07.043745. [DOI] [PMC free article] [PubMed] [Google Scholar]