Abstract
Objective
To estimate the global burden of cholera using population-based incidence data and reports.
Methods
Countries with a recent history of cholera were classified as endemic or non-endemic, depending on whether they had reported cholera cases in at least three of the five most recent years. The percentages of the population in each country that lacked access to improved sanitation were used to compute the populations at risk for cholera, and incidence rates from published studies were applied to groups of countries to estimate the annual number of cholera cases in endemic countries. The estimates of cholera cases in non-endemic countries were based on the average numbers of cases reported from 2000 to 2008. Literature-based estimates of cholera case-fatality rates (CFRs) were used to compute the variance-weighted average cholera CFRs for estimating the number of cholera deaths.
Findings
About 1.4 billion people are at risk for cholera in endemic countries. An estimated 2.8 million cholera cases occur annually in such countries (uncertainty range: 1.4–4.3) and an estimated 87 000 cholera cases occur in non-endemic countries. The incidence is estimated to be greatest in children less than 5 years of age. Every year about 91 000 people (uncertainty range: 28 000 to 142 000) die of cholera in endemic countries and 2500 people die of the disease in non-endemic countries.
Conclusion
The global burden of cholera, as determined through a systematic review with clearly stated assumptions, is high. The findings of this study provide a contemporary basis for planning public health interventions to control cholera.
Résumé
Objectif
Estimer le fardeau mondial du choléra en utilisant les rapports et les données d'incidence basés sur la population.
Méthodes
Les pays récemment affectés par le choléra ont été classés comme pays endémiques ou non endémiques, selon qu'ils avaient signalé des cas de choléra au cours d’au moins trois des cinq dernières années. Dans chaque pays, les pourcentages de la population n’ayant pas accès à des installations sanitaires améliorées ont été utilisés pour calculer les populations exposées au choléra, et les taux d'incidence tirés d’études publiées ont été appliqués à des groupes de pays afin d’évaluer le nombre annuel de cas de choléra dans les pays endémiques. Les estimations de cas de choléra dans les pays non endémiques étaient basées sur le nombre moyen de cas signalés de 2000 à 2008. Les estimations du taux de létalité (TL) du choléra basées sur la documentation disponible ont été utilisées pour calculer les TL du choléra moyens de variance pondérée afin d’évaluer le nombre de décès imputables au choléra.
Résultats
Environ 1,4 milliard de personnes sont exposées au choléra dans les pays endémiques. Environ 2,8 millions de cas de choléra se produisent chaque année dans ces pays (marge d'incertitude: 1,4−4,3), et quelque 87 000 cas de choléra sont enregistrés dans les pays non endémiques. On estime que l'incidence est supérieure chez les enfants de moins de 5 ans. Chaque année, environ 91 000 personnes (marge d'incertitude: 28 000 à 142 000) meurent du choléra dans les pays endémiques et 2 500 personnes en meurent dans les pays non endémiques.
Conclusion
Le fardeau mondial du choléra, tel que déterminé par une revue systématique sur la base d’hypothèses clairement énoncées, est élevé. Les résultats de cette étude fournissent une base actuelle pour la planification des interventions de santé publique afin de lutter contre le choléra.
Resumen
Objetivo
Calcular la carga global del cólera empleando los informes y datos sobre su incidencia en la población.
Métodos
Los países con unos antecedentes recientes de cólera se clasificaron como endémicos o no endémicos en función de si habían comunicado casos de cólera en al menos tres de los últimos cinco años. Se emplearon los porcentajes nacionales de población sin acceso a una sanidad moderna con el fin de calcular la población en riesgo de padecer el cólera y se aplicaron las tasas de incidencia de los estudios publicados a los grupos de países para calcular el número anual de casos de cólera en países endémicos. El cálculo aproximado del número de casos de cólera en países no endémicos se basó en las cifras medias de casos comunicados entre 2000 y 2008. Se utilizaron los cálculos aproximados de la tasa de mortalidad por cólera (TMC) procedentes de la documentación disponible para establecer la varianza ponderada de la TMC media para el cólera y calcular de este modo el número de defunciones por esta enfermedad.
Resultados
Aproximadamente 1,4 mil millones de personas están en riesgo de padecer el cólera en los países endémicos. Se ha calculado que en dichos países se registran aproximadamente 2,8 millones de casos de cólera al año (rango de incertidumbre: 1,4–4,3) así como unos 87 000 casos de cólera en los países no endémicos. Se estima que la incidencia más elevada se registra en los niños menores de 5 años. Cada año mueren unas 91 000 personas (rango de incertidumbre: 28 000 a 142 000) de cólera en los países endémicos y 2500 personas fallecen por esta enfermedad en los países no endémicos.
Conclusión
La carga global del cólera es elevada, según se ha determinado a través de una revisión sistemática con supuestos claramente definidos. Los resultados de este estudio ofrecen una base contemporánea para planificar las intervenciones de la sanidad pública dirigidas a controlar el cólera.
ملخص
الغرض
تقييم العبء العالمي للكوليرا باستخدام بيانات وتقارير الإصابة بالمرض المعتمدة على السكان.
الطريقة
تم تصنيف البلدان ذات التاريخ الحديث من الإصابة بالكوليرا إلى يتوطنها المرض أو لا يتوطنها المرض بناءً على ما إذا كانت قد أبلغت عن حالات إصابة بالكوليرا في ثلاثة على الأقل من الأعوام الخمسة الأخيرة. وتم استخدام النسب المئوية للسكان في كل بلد افتقر إلى الوصول إلى الخدمات الصحية المحسَّنة لحساب السكان المعرضين لخطر الإصابة بالكوليرا، وتم تطبيق معدلات الإصابة بالمرض من الدراسات المنشورة على مجموعات البلدان لتقييم العدد السنوي لحالات الكوليرا في البلدان التي يتوطنها المرض. واعتمدت تقديرات حالات الكوليرا في البلدان التي لا يتوطنها المرض على متوسط أعداد الحالات المبلغ عنها في الفترة ما بين عام 2000 إلى عام 2008. وتم استخدام تقديرات معدلات الوفاة بحالات الكوليرا (CFRs) المعتمدة على المراجع المنشورة لحساب متوسط التباين المرجح لمعدلات الوفاة بحالات الكوليرا لتقدير عدد حالات الوفاة بالكوليرا.
النتائج
1.4 مليار نسمة تقريبًا معرضون لخطر الإصابة بالكوليرا في البلدان التي يتوطنها المرض. ووفق التقديرات، تحدث 2.8 مليون إصابة بالكوليرا سنويًا في هذه البلدان (نطاق عدم اليقين: 1.4-4.3) وتحدث 87000 حالة إصابة بالكوليرا في البلدان التي لا يتوطنها المرض. ووفق التقديرات، بلغت الإصابة بالمرض أعلى مستوياتها لدى الأطفال الأقل من 5 أعوام. ويتعرض للوفاة سنويًا 91000 نسمة تقريبًا (نطاق عدم اليقين: 28000 إلى 142000) بسبب الكوليرا في البلدان التي يتوطنها المرض ويتعرض للوفاة 2500 نسمة بسبب هذا المرض في البلدان التي لا يتوطنها المرض.
الاستنتاج
العبء العالمي للكوليرا - وفق ما تم تحديده من خلال استعراض منهجي باستخدام افتراضات واضحة التحديد – مرتفع. وتقدِّم نتائج هذه الدراسة أساسًا معاصرًا لتخطيط تدخلات الصحة العامة للسيطرة على الكوليرا.
摘要
目的
使用基于人口的发病率数据和报告估计全球霍乱的负担。
方法
根据最近五年中是否至少三年报告霍乱病例,将最近有霍乱历史的国家分为地方流行性或非地方流行性霍乱国家。使用每个国家中缺乏改善的卫生环境的人口百分比计算霍乱风险人口,对多组国家使用已发布的研究得出的发病率估计地方流行性霍乱国家中每年霍乱病例的数量。基于 2000 至 2008 年报告的病例数量估计非地方流行性霍乱国家中的霍乱病例的数量。使用基于文献的霍乱致命病例率 (CFR) 估计来计算方差加权平均霍乱 CFR 用以估计霍乱死亡人数。
结果
在地方流行性霍乱国家中约有 14 亿人口面临霍乱风险。据估计,每年这些国家发生 280 万霍乱病例(不确定范围:140 万至 430 万),非地方流行性霍乱国家中估计发生 8.7 万霍乱病例。据估计,未满 5 岁的儿童发病率最高。地方流行性霍乱国家每年约有 9.1 万人(不确定范围:2.8 万至 14.2 万)口死于霍乱,非地方流行性霍乱国家每年 2500 人死亡。
结论
正如通过带有表述清晰的假设的系统性综述所确定的,全球霍乱负担高。此项研究的结果为规划控制霍乱的公共卫生干预提供时代基础。
Резюме
Цель
Оценить глобальное бремя холеры с использованием данных и отчетов о заболеваемости населения.
Методы
Страны с недавней историей заболеваемости холерой были классифицированы как эндемические и неэндемические, в зависимости от того, сообщали ли они о случаях заболевания холерой, по крайней мере, в течение трех из пяти последних лет. Процент населения в каждой стране, не имеющей доступа к улучшенным средствам санитарного надзора, был использован для вычисления групп населения с риском заболевания холерой, а показатели заболеваемости из опубликованных исследований были применены в отношении групп стран с целью оценки ежегодного количества заболеваний холерой в эндемических странах. Оценки случаев заболевания холерой в неэндемических странах были основаны на среднем количестве случаев, зарегистрированных с 2000 по 2008 гг. Основанные на полученных данных оценки частоты летального исхода (летальности) в случае заболевания холерой были использованы для вычисления значения средневзвешенной дисперсии уровня летальности, связанного с холерой, и оценки количества смертей в результате данного заболевания.
Результаты
В эндемических странах риску заболевания холерой подвержены около 1,4 миллиарда человек. По оценкам, в таких странах ежегодно регистрируется 2,8 миллиона случаев заболевания холерой (область неопределенности: 1,4-4,3), и примерно 87 000 случаев заболевания холерой регистрируется в неэндемических странах. Заболеваемость оценивается как самая высокая у детей в возрасте младше 5 лет. Каждый год около 91 000 человек (область неопределенности: 28 000-142 000) умирают от холеры в эндемических странах и 2500 человек умирают от данного заболевания в неэндемических странах.
Вывод
Уровень глобального бремени холеры, как определено посредством систематического обзора с четко заявленными предпосылками, является высоким. Результаты данного исследования представляют собой современную основу для планирования мер в области общественного здравоохранения для борьбы с холерой.
Introduction
Cholera is an important public health problem worldwide. Although most cholera infections are not detected, large cholera outbreaks, such as those seen in Haiti,1 Viet Nam2 and Zimbabwe3 in recent years, can occur. Industrialized countries have seen practically no cholera cases for over a century because of their good water and sewage treatment infrastructure. However, the causative agents (Vibrio cholerae O1 and O139) continue to thrive wherever crowded housing conditions exist and water and sanitation facilities are suboptimal.
The World Health Organization (WHO) maintains a public database of cholera cases and provides outbreak updates and an annual summary of aggregate national data in the Weekly Epidemiological Record. Owing to its rapid spread, cholera was one of three diseases requiring notification to the WHO in the 1969 International Health Regulations (IHR), and today, after the 2005 revision of the IHR, cholera outbreaks still require notification. Despite this, cholera notification remains incomplete because of inadequate laboratory and epidemiological surveillance systems and economic, social and political disincentives to case reporting.4–7 WHO estimates that the officially reported cases represent only 5–10% of the actual number occurring annually worldwide. Of the estimated 3 to 5 million cases that occur globally every year, about 100 000 to 120 000 die.8,9 In 2002, Lanata et al. calculated, using the fraction of diarrhoea cases estimated to be caused by cholera (0.05%), that 11 million cholera cases occur globally every year among children under 5 years of age.10 However, adults and older children can also get cholera, and mortality can be high in all age groups.11–13
One new generation oral cholera vaccine is pre-qualified by WHO for purchase by the United Nations (UN), and another, less expensive oral vaccine has recently been licensed and is undergoing evaluation for WHO pre-qualification.14 WHO recommends instituting cholera immunization, in conjunction with other prevention and control strategies, in endemic areas, and perhaps in areas at risk for cholera outbreaks.15 To plan interventions appropriately, policy-makers at all levels need to know the burden of disease and the population at risk.
In this paper we present age-specific estimates of the cholera burden in endemic and non-endemic countries and a global estimate. To derive our figures we used population-based incidence data and reports from WHO and supplementary sources.
Methods
Data sources and framework
To supplement the WHO cholera reports, we developed a framework based on literature searches and alternative disease monitoring systems, including the Program for Monitoring Emerging Diseases (ProMED), an online forum for infectious disease specialists, microbiologists and public health officials established in 1994 and administered by the International Society for Infectious Diseases since 1999.16 Although it is a passive reporting system, it complements the WHO reports by providing detailed data from media reports describing outbreaks. In an analysis of ProMED data, the number of cholera cases reported was found to be about five times higher than the number reported by the WHO.8,17 We used population-based cholera incidence data from a multi-country study that included Asian and African countries.18–20 In addition to these sources, we reviewed data from the Global Infectious Disease and Epidemiology Network (GIDEON) database, published articles listed in PubMed, and online government reports.
Country classification
In classifying countries, we used WHO’s division into five mortality strata, as follows: A, very low child and very low adult mortality; B, low child and low adult mortality; C, low child and high adult mortality; D, high child and high adult mortality; E, high child and very high adult mortality. Most developed countries in North America, Europe and the Western Pacific, which primarily report imported cholera cases, belong to stratum A. The Region of the Americas (AMR) and the European Region (ER) have very little cholera. Of the 35 countries in the AMR, only Brazil and Paraguay have reported non-imported cases over the last nine years (5 in Brazil in 2005 and 5 in Paraguay in 2009). Of the 52 countries in the ER, only Poland, the Russian Federation and the Ukraine have reported non-imported cholera cases (one case each) since 2005. We therefore classified the AMR and the ER as cholera-free. For the 148 remaining countries in the five mortality strata, we reviewed reported cholera incidence data for 2000–2008 to determine whether cholera was: (i) endemic; (ii) observed but not endemic, or (iii) not observed.
Endemic and non-endemic countries
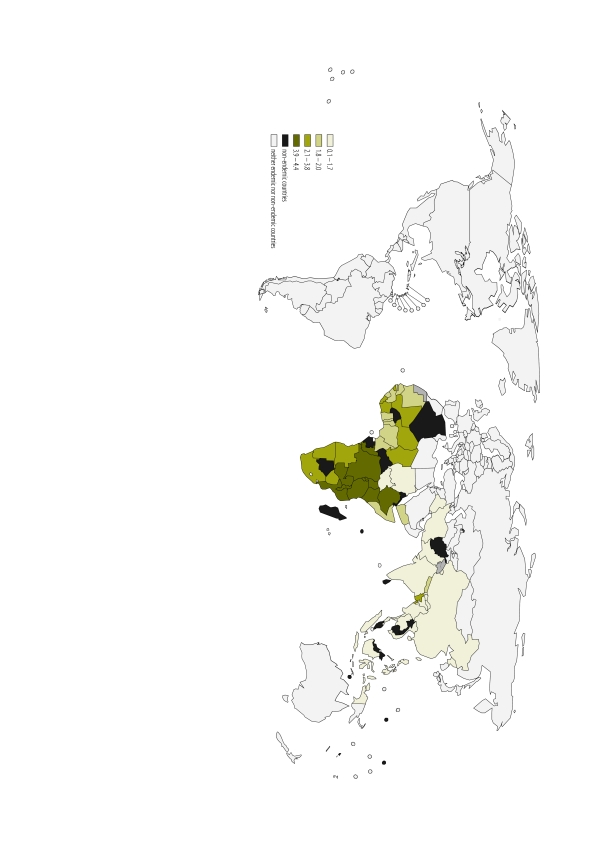
In classifying countries as endemic or non-endemic, we used the definitions recently applied by the WHO Strategic Advisory Group of Experts on Vaccines and Immunization (SAGE).15 Countries were classified as endemic if they had reported cholera cases in at least three of the five most recent years (either 2003–2007 or 2004–2008), as published in the Weekly Epidemiological Record. If a country had no cholera reports in the Weekly Epidemiological Record, we searched PubMed and the ProMED and GIDEON reporting systems using the terms acute watery diarrhoea (or diarrhoea), cholera (or cholerae) to identify endemic countries. Of the 148 countries, 51 were classified as cholera-endemic (Fig. 1). The reported cases, by country and year, are listed in Appendix A (available at: https://trdrdcsys.ivi.int/cic/appendixA.pdf); details on the references and methods used to obtain the reports are in Appendix B (available at: https://trdrdcsys.ivi.int/cic/appendixB.pdf).
Fig. 1.
Geographical patterns of the estimated cholera incidences for entire population in endemic countries
We identified another 18 countries that did not meet the criterion for endemic cholera but that had reported cholera cases sometime between 2000 and 2008. We classified these countries as non-endemic. Of these countries, those that had reported only imported cases (e.g. developed countries in North America, Western Europe and the Pacific) or very sporadic non-imported cases (e.g. countries of Eastern Europe or South America with five cases or fewer in non-consecutive years) were considered cholera-free and not included in the calculation.
Population at risk
We used the United Nations Development Programme population data21 for 2005 to estimate the population at risk of cholera in each country. Since not all the population of a cholera-endemic country is at risk for cholera, we used instead the percentage of the population of each country lacking access to improved sanitation, according to UN data from 2008.22 We made one exception: We considered the entire population of Bangladesh at risk, on advice from the country’s cholera experts, because of frequent and widespread flooding. For the three largest cholera-endemic countries – China, India and Indonesia – we only included the fraction of the population lacking access to improved sanitation in states and provinces that had reported cholera (2000–2007 in China23 and Indonesia24 and 1997–2006 in India25).
Disease burden estimation
In estimating cholera caseloads for both endemic and non-endemic countries, we focused on cholera episodes severe enough to require medical treatment.
Endemic countries
We obtained incidence rates from the Diseases of the Most Impoverished (DOMI) cholera surveillance programmes in Kolkata, India,18 Jakarta, Indonesia,19 and Beira, Mozambique20 (Table 1), since these population-based surveillance figures included both inpatient and outpatient cases of laboratory-confirmed cholera. We applied incidence rates from these studies to the at-risk populations of cholera-endemic countries by WHO mortality stratum. To be conservative, we assumed an incidence of zero in the population not at risk (i.e. the population with access to improved sanitation in countries other than Bangladesh). We grouped countries according to WHO region and WHO mortality stratum.26 An alphabetical list of the countries we included in our calculation, by WHO stratum, is given in Appendix C (available at: https://trdrdcsys.ivi.int/cic/appendixC.pdf).
Table 1. Cholera annual incidence rates (per 1000), by age group, in two Asian and one African site11.
| Age (years) | Kolkata, India (May 2003–Apr 2005) |
Jakarta, Indonesia (Aug 2001–Jul 2003) |
Beira, Mozambique (Jan–Dec 2004) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Population | Cases | Rate | Population | Cases | Rate | Population | Cases | Ratea | |||
| < 1 | 698 | 10 | 7.16 | 3 121 | 25 | 4.01 | – | – | – | ||
| 1–4 | 3 782 | 53 | 7.01 | 12 620 | 39 | 1.55 | 1 686b | 9 | 8.8 | ||
| 5–14 | 11 440 | 50 | 2.19 | 29 093 | 17 | 0.29 | 17 861c | 38 | 3.5 | ||
| > 14 | 42 143 | 78 | 0.93 | 115 423 | 62 | 0.27 | |||||
| Total | 58 063 | 191 | 1.64 | 160 257 | 143 | 0.45 | 19 547 | 47 | 4.0 | ||
a Rates were corrected for direct protection from cholera vaccination.
b Age group 2–4 years.
c Age group ≥ 5 years.
We assumed that the incidence rates observed in the DOMI studies were representative of the at-risk populations in the WHO mortality strata. This assumption was based on perceived similarities in cholera risk between the DOMI sites and the at-risk populations of the strata as a whole. For example, in the South-East Asia Region (SEAR), we applied Jakarta’s incidence rates to the at-risk population of Indonesia and other endemic countries in stratum B (SEAR-B), and we applied Kolkata’s incidence rates to India and all other cholera-endemic countries in stratum D (SEAR-D), except for Bangladesh. We also applied Kolkata’s incidence rates to countries of the Eastern Mediterranean Region (EMR) in WHO mortality stratum D (EMR-D), which includes Pakistan, Somalia and other countries with a large cholera burden. For Bangladesh we used a cholera incidence rate based on in-country expert interviews conducted for the Cholera Vaccine Investment Country Case Study: Bangladesh (B Maskery, personal communication).
In the African Region (AFR), we applied Beira’s incidence rates to the at-risk populations of cholera-endemic countries belonging to WHO’s mortality stratum E (AFR-E). In the absence of representative data for African countries in stratum D (AFR-D), we compared the mean and median estimates of cholera incidence reported in the Weekly Epidemiological Record for countries in AFR-D and AFR-E from 2000 up to 2008, since countries in the AFR report cholera cases to WHO more consistently than countries in other WHO regions. The average incidence rates reported in endemic countries in AFR-E were about 1.7 times higher than the rates reported in endemic countries in AFR-D. Thus, we assumed that incidence among the at-risk populations of countries in AFR-D would be approximately half as high as in Beira. In the absence of data for countries in the Western Pacific Region (WPR) and EMR-B, we assumed that the incidence of cholera in the at-risk populations would be low, about 0.1 cases per 1000 persons (Table 2).
Table 2. Cholera incidence rate (per 1000) and source of information by World Health Organization (WHO) mortality stratum.
| WHO stratum | Incidencea | Information source |
|---|---|---|
| AFR-D | 2.00 | Beira, Mozambique and WER data |
| AFR-E | 4.00 | Beira, Mozambique data |
| EMR-B | 0.10 | Assumption-based |
| EMR-D | 1.64 | Kolkata data |
| SEAR-B | 0.45 | Jakarta data |
| SEAR-D | 1.64 | Kolkata data |
| WPR-B | 0.10 | Assumption-based |
AFR-D, African Region, stratum D; AFR-E, African Region, stratum E; EMR-B, Eastern Mediterranean Region, stratum B; EMR-D, Eastern Mediterranean Region, stratum D; SEAR-B, South-East Asia Region, stratum B; SEAR-D, South-East-Asia Region, stratum D; WER, Weekly Epidemiological Record; WPR-B, Western Pacific Region, stratum B.
a Rate per 1000.
Note: Countries by WHO mortality strata are listed in Appendix A (available at: https://trdrdcsys.ivi.int/cic/appendixA.pdf).
Non-endemic countries
The number of cholera cases in non-endemic countries was estimated from the reported numbers of cases identified through the Weekly Epidemiological Record, ProMED, GIDEON and published articles in PubMed for the period from 2000 to 2008. The estimated number of cases is shown in Appendix B. We estimated the average number of cholera cases per year by adding all the reported cases identified in 2000–2008, careful to not repeat data from different articles for the same year, and dividing the total by nine (for the nine-year interval). Because most of the data included in this report were obtained from WHO’s Weekly Epidemiological Record, whose reporting efficiency WHO estimates as ranging from 5–10%,8 we assumed that the annual average numbers of reported cases represent approximately 10% of the cholera burden in non-endemic countries. We divided the average annual number of cases in 2000–2008 by this reporting efficiency rate to estimate the cholera burden in these countries.
Age-specific incidence rates
We estimated age-specific cholera incidence rates for each endemic country using WHO-region-specific overall incidence rates (Table 2) and the incidence age distribution from the Kolkata study (Table 1). We used the Kolkata age distribution because population-based age-specific incidence is generally unavailable by WHO mortality stratum. To account for differences between each country’s population age distribution and that of Kolkata, we normalized age-specific incidence rates such that the overall incidence for a given WHO mortality stratum matches the estimates in Table 2.
Estimation of cholera deaths
Cholera is distinctive among diarrhoeal diseases in that mortality is high among patients of all ages. Estimates of cholera mortality reported to WHO by Member States may be inaccurate. For example, during a cholera outbreak in several Kenyan villages in 2008, active, community-based case-finding showed much higher numbers of cases and deaths than reported: 37% more surviving cases and 200% more fatal cases were found, raising the estimated case-fatality rate (CFR) from 5.5% to 11.4%.27 Because in less-developed countries many deaths from cholera probably occur before patients reach the hospital for treatment, facility-based cholera mortality figures are very likely to be underestimates.
Drawing on reported CFRs from several published studies (Table 3, available at: http://www.who.int/bulletin/volumes/90/3/11-093427), we computed variance-weighted46 average cholera CFRs by WHO region. We took the sum of the product of CFR and weight and divided it by the sum of the weights (Appendix D, available at: https://trdrdcsys.ivi.int/cic/appendixD.pdf). No CFR estimates for AFR-D were available from peer-reviewed sources for the past 10 years, so instead we used the estimated CFRs for AFR-E, which we found to be about 20% lower.
Table 3. Summary of cholera cases and deaths reported in the literature, by date, country and World Health Organization (WHO) mortality stratum.
| Year/Date | Country | WHO stratum | Cholera cases | Deaths | CFR (%) | Variancea | Weight (1/variance) | Reference | Estimated CFR by WHO region | Per capita total expenditure on health (PPP dollars)27 |
|---|---|---|---|---|---|---|---|---|---|---|
| Oct 1994–Jan 1995 | Guinea-Bissau | AFR-D | 1 169 | 43 | 3.68 | 0.30 | 3.30 | 12 | 3.8 | 106 |
| Jan 1996–Dec 1996 | Nigeria | 1 384 | 92 | 6.65 | 0.45 | 2.23 | 13 | |||
| Jun 1997–Mar 1998 | Kenya | AFR-E | 14 275 | 547 | 3.83 | 0.03 | 38.74 | 28 | 3.8 | 146 |
| Nov 2003–Feb 2004 | Zambia | 4 343 | 154 | 3.55 | 0.08 | 12.70 | 29 | |||
| Aug 1990–Dec 1990 | Malawi | 1 931 | 68 | 3.52 | 0.18 | 5.68 | 30 | |||
| Aug 2005 | Islamic Republic of Iran | EMR-B | 560 | 7 | 1.28 | 0.20 | 4.96 | 31 | 1.3 | 689 |
| 15 Oct 2008 | Iraq | EMR-D | 500 | 8 | 1.60 | 0.31 | 3.18 | 32 | 3.2 | 68 |
| 24 Jul 1994 | Yemen | EMR-D | 150 | 17 | 11.33 | 6.70 | 0.15 | 33 | ||
| 5 Feb 2007 | Somalia | EMR-D | 110 | 15 | 13.64 | 10.71 | 0.09 | 34 | ||
| 21 Apr 2006 | Sudan | EMR-D | 5 369 | 180 | 3.35 | 0.06 | 16.57 | 35 | ||
| Sep 1991–Nov 1991 | Bangladesh | SEAR-D | 210 265–235 810 | 8 410–9 432 | 4.00 | 0.00 | 580.86 | 36 | 3.0 | 90 |
| 2002–2006 | India | SEAR-D | 164 100 | 705 | 0.31 | 0.00 | 207.11 | 37–45 | ||
| – | – | SEAR-B | – | – | – | – | – | – | 1.0 | 161 |
| – | – | WPR-B | – | – | – | – | – | – | 1.0 | 199 |
AFR-D, African Region, stratum D; AFR-E, African Region, stratum E; CFR, case-fatality rate; EMR-B, Eastern Mediterranean Region, stratum B; EMR-D, Eastern Mediterranean Region, stratum D; PPP, purchasing power parity; SEAR-B, South-East Asia Region, stratum B; SEAR-D, South-East Asia Region, stratum D; WPR-B, Western Pacific Region, stratum B.
a Variance = [CFR × (100 − CFR)] divided by the number of cholera cases.
Cholera CFR estimates were not available for any of the cholera-endemic countries in SEAR-B or WPR-B. We assigned these countries a CFR of 1.0% on the assumption that they had lower CFRs because their health expenditure per capita was higher than in AFR and SEAR-D countries (Table 3). Using these CFRs, we computed the expected annual number of deaths from cholera for all selected endemic and non-endemic countries except Bangladesh, for which we used a CFR of 1.5% provided by an expert (B Maskery, personal communication). Since age-specific mortality data were not available, we assumed that CFRs were the same across all age groups in each stratum.
Results
At-risk population
Table 4 shows the at-risk populations of endemic countries, aggregated by WHO mortality strata. An estimated 1.4 billion of the world’s population is at risk for cholera, and SEAR-D, which includes Bangladesh and India, has the largest populations at risk, followed in descending order by AFR-E and AFR-D. For country-specific at-risk population data, see Appendix C.
Table 4. Population at risk, estimated number of cholera cases and estimated annual incidence in endemic countries, by age group and World Health Organization (WHO) mortality stratum.
| WHO stratum | Total population at risk | Age group (in years) |
Incidence (per 1000 at risk) | ||||
|---|---|---|---|---|---|---|---|
| < 1 | 1–4 | 5–14 | 15+ | All | |||
| AFR-D | 196 462 691 | 45 062 | 159 118 | 99 714 | 89 035 | 392 929 | 2.0 |
| AFR-E | 254 606 241 | 115 374 | 410 737 | 259 704 | 232 709 | 1 018 524 | 4.0 |
| EMR-B | 11 817 550 | 93 | 330 | 292 | 459 | 1 174 | 0.1 |
| EMR-D | 114 459 890 | 19 099 | 70 711 | 46 951 | 50 858 | 187 619 | 1.6 |
| SEAR-B | 50 443 558a | 1 806 | 6 973 | 5147 | 8 760 | 22 686 | 0.4 |
| SEAR-D | 694 832 590b | 100 408 | 379 474 | 305 771 | 416 029 | 1 201 682 | 1.7 |
| WPR-B | 120 530 784c | 846 | 3 287 | 2785 | 5 137 | 12 055 | 0.1 |
| Total | 1 443 153 304 | 282 688 | 1 030 630 | 720 364 | 802 987 | 2 836 669 | 2.0 |
| Incidence (per 1000) | – | 7.3 | 7.0 | 2.2 | 0.9 | 2.0 | – |
AFR-D, African Region, stratum D; AFR-E, African Region, statum E; EMR-B, Eastern Mediterranean Region, stratum B; EMR-D, Eastern Mediterranean Region, stratum D; SEAR-B, South-East Asia Region, stratum B; SEAR-D, South-East Asia Region, stratum D; WPR-B, Western Pacific Region, stratum B.
a Provinces of Indonesia included West Java, Irian Jaya, Sumatra, Jakarta, Banten, Tangerang, Bogor and Maluku.
b States and territories of India included Andhra Pradesh, Assam, Goa, Gujarat, Haryana, Himachal Pradesh, Karnataka, Kerala, Madhya Pradesh, Maharashtra, Orissa, Punjab, Tamil Nadu, Uttar Pradesh, West Bengal, Andaman & Nicobar Island, Chandigarh and Delhi.
c Provinces of China included Guandong, Zhejiang, Shanghai, Fujian and Hainan.
Cholera cases
An estimated 2.8 million cholera cases occur each year in endemic countries (Table 4), and the average global annual incidence rate is 2.0 cases per 1000 people at risk (range: 0.10–4.0). If the population not at risk is counted, the estimated average incidence in cholera-endemic countries drops to about 1.15 cases per 1000 population. The countries with the highest incidence rates are in Africa and southern Asia (Fig. 1). Lower incidence rates were estimated for South-East Asia. Within Africa, western countries (primarily those in stratum D) were estimated to have lower incidence rates than countries in eastern Africa (primarily those in stratum E) because cholera incidence among at-risk populations in countries in AFR-D was assumed to be about 50% of the rate reported in Beira, based on the cholera incidence rates reported to WHO and other data sources. Only 1.2% of the estimated cases occur in SEAR-B, WPR-B and EMR-B, which is not surprising since these countries belong to lower mortality strata and have better infrastructure. Incidence rates are highest among children under 5. Overall, we estimate that about half of all cholera cases occur in this age group, and that the expected annual number of cholera cases in non-endemic countries is about 87 000 (Table 5). Estimates of the expected number of cholera cases by country and by age group are given in Appendix E (available at: https://trdrdcsys.ivi.int/cic/appendixE.pdf.).
Table 5. Estimated annual number of cholera cases in non-endemic countries.
| Country | WHO stratum | Cases | Deaths |
|---|---|---|---|
| Afghanistan | EMR-D | 17 157 | 549 |
| Algeria | AFR-D | 2 143 | 83 |
| Botswana | AFR-E | 51 | 2 |
| Burkina Faso | AFR-D | 17 129 | 651 |
| Cambodia | WPR-B | 16 805 | 168 |
| Central African Republic | AFR-E | 173 | 8 |
| Djibouti | EMR-D | 190 | 6 |
| Eritrea | AFR-E | 271 | 10 |
| Fiji | WPR-B | 377 | 3 |
| Gabon | AFR-D | 1 119 | 43 |
| Lao People's Democratic Republic | WPR-B | 5 426 | 54 |
| Madagascar | AFR-D | 23 180 | 881 |
| Malaysia | WPR-B | 2 293 | 24 |
| Marshall Islands | WPR-B | 18 | 0 |
| Micronesia (Federated States of) | WPR-B | 143 | 1 |
| Seychelles | AFR-D | 103 | 3 |
| Sri Lanka | SEAR-B | 10 | 0 |
| Timor-Leste | SEAR-D | 658 | 20 |
| Total | – | 87 246 | 2 506 |
AFR-D, African Region, stratum D; AFR-E, African Region, stratum E; EMR-B, Eastern Mediterranean Region, stratum B; EMR-D, Eastern Mediterranean Region, stratum D; SEAR-B, South-East Asia Region, stratum B; SEAR-D, South-East Asia Region, stratum D; WPR-B, Western Pacific Region, stratum B.
Cholera deaths
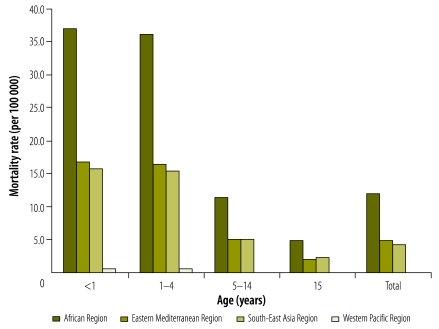
The estimated numbers of annual cholera deaths in endemic countries, by age and by WHO mortality stratum, are summarized in Table 6. Estimated numbers of country-specific cholera deaths are available in Appendix F (available at: https://trdrdcsys.ivi.int/cic/appendixF.pdf). Using population data from 2005, we estimated that cholera kills about 91 000 people annually, on average, in endemic countries, with about half of the deaths occurring in children under 5. This corresponds to a rate of 6.3 deaths per 100 000 people at risk. Mortality rates vary from 0.1 deaths per 100 000 people at risk in EMR-B and WPR-B to 15.2 deaths per 100 000 in AFR-E. Since we assumed that CFRs were the same across age groups, age-specific mortality rates, like age-specific incidence rates, were highest among young children (Fig. 2). In total, we estimated an average of about 2500 cholera deaths per year in a non-endemic country (Table 5).
Table 6. Estimated number of cholera deaths and annual mortality rate in endemic countries, by age group and World Health Organization (WHO) mortality stratum.
| WHO stratum | Age group (years) |
Mortalitya | ||||
|---|---|---|---|---|---|---|
| < 1 | 1–4 | 5–14 | 15+ | Total | ||
| AFR-D | 1 712 | 6 045 | 3 788 | 3 383 | 14 928 | 7.6 |
| AFR-E | 4 384 | 15 610 | 9 868 | 8 842 | 38 704 | 15.2 |
| EMR-B | 1 | 4 | 4 | 6 | 15 | 0.1 |
| EMR-D | 612 | 2 263 | 1 503 | 1 627 | 6 005 | 5.2 |
| SEAR-B | 18 | 70 | 52 | 88 | 228 | 0.5 |
| SEAR-D | 2 647 | 10 062 | 8 056 | 10 725 | 31 490 | 4.5 |
| WPR-B | 8 | 32 | 28 | 52 | 120 | 0.1 |
| Total | 9 382 | 34 086 | 23 299 | 24 723 | 91 490 | 6.3 |
| Mortalitya | 24.1 | 23.2 | 7.0 | 2.7 | 6.3 | – |
AFR-D, African Region, stratum D; AFR-E, African Region, stratum E; EMR-B, Eastern Mediterranean Region, stratum B; EMR-D, Eastern Mediterranean Region, stratum D; SEAR-B, South-East Asia Region, stratum B; SEAR-D, South-East Asia Region, stratum D; WER, WPR-B, Western Pacific Region, stratum B.
a Deaths per 100 000.
Fig. 2.
Age-specific mortality rates for at-risk populations by WHO stratum in cholera-endemic countries, 2005
Sensitivity analyses
We performed sensitivity analyses using different criteria to estimate: (i) the population at risk in endemic countries, (ii) cholera incidence rates, and (iii) CFRs. In the base-case analysis we assumed the population at risk in endemic countries to be the fraction lacking access to improved sanitation. We also conducted the analysis under a more restrictive assumption, namely, that the population at risk was the fraction lacking access to an improved water supply (smaller in most countries than the fraction lacking improved sanitation). When we applied the incidence rates from Table 1 to UN data on the population without an improved water source,47 the annual cholera burden decreased to 1.17 million cases and 41 000 deaths. We also applied the less restrictive assumption that in endemic countries (including all states and provinces of China, India and Indonesia) the entire population was at risk, whereupon the global cholera burden estimates increased to 5.1 million cases and 156 000 deaths.
When we assumed that incidence rate estimates were 50–150% of the base values for WHO mortality strata, the estimated annual number of cases and deaths ranged from 1.42 to 4.26 million and from 46 000 to 137 000, respectively. Finally, we found that CFRs generally vary between 1% and 5%, depending on access to appropriate treatment (Table 3). When these CFRs were applied across all mortality strata, the expected number of cholera deaths ranged from 28 000 to 142 000.
Discussion
Our study shows that the global burden of cholera is large, particularly in developing countries. Every year an estimated 2.8 million cases of cholera (uncertainty range: 1.2–4.3 million) and about 91 000 deaths (uncertainty range: 28 000–142 000) occur in endemic countries, and another 87 000 cases and 2500 deaths occur in non-endemic countries. The burden of cholera is greatest in Africa and southern Asia, with about 99% of the cases occurring in AFR-D, AFR-E, SEAR-D and EMR-D. About half of the cases and deaths occur in children under 5. Because most cholera cases occur in poor communities, few systematic studies of endemic cholera incidence have been conducted. In addition, since embargos from trading partners and tourism losses usually follow confirmation of cholera outbreaks,48,49 many countries are reluctant to conduct cholera surveillance or to officially report cholera cases or deaths. Finally, many cholera deaths occur before patients can reach treatment facilities, which further complicates disease burden estimates.27
Our estimates are based on a framework using available endemic cholera incidence rates, identification of endemic countries based on WHO criteria and, for Bangladesh, interviews with in-country experts. Our estimated number of cases and cholera-attributable deaths were consistent with previous WHO estimates of underreporting of 3 to 5 million cases and 100 000 to 120 000 deaths every year.9,17 These estimates are much higher than the 317 534 cases and 7543 deaths reported worldwide in 2010, suggesting that cholera is substantially underreported. Even if the 500 000 to 700 000 cases of acute watery diarrhoea reported annually in some parts of Asia are counted as cholera cases,50 the resulting numbers are still lower than our estimates. However, our estimated burden is substantially lower than the 11 million cases found among children under 5 in 2002 by Lanata et al., who used different methods and included published studies from 1990–2002.10
There are limitations to our study. First, we obtained some incidence rates from systematic surveillance over a two-year period in three research settings and applied them to cholera-endemic countries by WHO mortality stratum. Such settings may not be representative of each region. In addition, cholera incidence varies from year to year, even in endemic countries. Thus, two years of surveillance data may not be enough to estimate the average cholera burden. Second, supplemental data from WHO and other sources were also included to adjust incidence rates within the AFR; however, few countries outside this region report cholera consistently. To overcome the data limitations, we carefully evaluated every country setting and used our best judgment to attribute incidence rates by WHO mortality stratum. Third, we generalized data from Kolkata, in SEAR-D, to estimate the age distribution of cases in regions other than SEAR-D. We did this because Kolkata was the only site for which current data on the age-specific incidence of cholera in all age groups were available.
A further limitation of our study is that we treated Bangladesh, China, India and Indonesia differently from the way we treated other countries. We assumed the entire population of Bangladesh to be at risk because, unlike other cholera-endemic countries, Bangladesh has a low elevation and experiences tropical monsoons that undermine the benefits of improved sanitation. China, India and Indonesia were treated differently for three reasons: (i) they had large populations capable of greatly influencing estimates; (ii) their risk of cholera is heterogeneous, and (iii) they report data by state or province. In addition, we excluded certain parts of these countries after carefully reviewing the literature on cholera in 2003–2008. The inclusion of the entire populations of these countries could artificially increase the estimated at-risk population and cholera incidence.
We tried to be conservative in our estimates by defining the population at risk of cholera using the UN Millennium Development Goals Indicators database on country-specific access to improved sanitation and assuming zero incidence in the population not at risk. To address the impact of these limitations, we performed sensitivity analyses and calculated ranges for the total numbers of cholera cases and deaths.
On the positive side, we made transparent assumptions for generalizing data to the global population, and we estimated the global burden of cholera based on cholera incidence rates obtained from population-based surveillance studies. Our cholera burden estimates are in line with WHO’s lesser estimate. We did not include the recent major epidemic of cholera in Haiti in our study because it occurred after the time frame for our analysis and cholera had not been reported in Haiti for more than 100 years. If, as some predict, cholera becomes endemic in Haiti, then Haiti’s cholera burden should be included in future analyses.
Epidemic cholera is a disease of great local importance, as evidenced by large, recent outbreaks in Haiti and Zimbabwe. However, the burden of cholera in endemic areas, which appears to dwarf the burden in non-endemic areas, is often overlooked. At two district hospitals in rural Bangladesh, cholera was the most common cause of severe dehydration from acute watery diarrhoea among children less than 5 years of age; it was 1.8 times more common than rotavirus diarrhoea as a cause of severe dehydration.51 In another study from a hospital in Kolkata, V. cholerae O1 was the pathogen most commonly isolated from admitted patients who had diarrhoea and the one most often identified in fatal cases over a two-year period.52
Our estimate of the global burden of cholera may direct efforts to develop strategies for mitigating endemic and epidemic cholera in the face of climatic and environmental changes and slow progress towards improving water and sanitation in endemic countries. We need adequate prevention, preparedness and control measures to mitigate the impact of cholera.6 Poor case reporting is problematic because it can lead to insufficient allocation of resources to effectively deal with cholera. The data we present may help policy-makers and the WHO’s Global Task Force on Cholera Control to determine how much investment future cholera control interventions will require. They also underscore the need to improve cholera surveillance, especially among at-risk populations in endemic countries.
Acknowledgements
We are grateful to Deok Ryun Kim and to the members of the Cholera Vaccine Investment Case Technical Advisory Committee for their valuable contributions.
Funding:
Financial support was provided by the Bill and Melinda Gates Foundation through the Cholera Vaccine Initiative (CHOVI) programme, administered by the International Vaccine Institute (IVI), Seoul, Republic of Korea. Current donors providing unrestricted support to IVI include the Governments of Kuwait, Republic of Korea and Sweden.
Competing interests:
None declared.
References
- 1.Chao DL, Halloran ME, Longini IM., Jr Vaccination strategies for epidemic cholera in Haiti with implications for the developing world. Proc Natl Acad Sci USA. 2011;108:7081–5. doi: 10.1073/pnas.1102149108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization Outbreak news – severe acute watery diarrhoea with cases positive for Vibrio cholerae, Viet Nam. Wkly Epidemiol Rec. 2008;83:157–8. [PubMed] [Google Scholar]
- 3.Zimbabwe: OCHA Cholera Update Situation Report No. 22, 15 Jul 2009 New York: United Nations Office for the Coordination of Human Affairs; 2009. Available from: http://reliefweb.int/sites/reliefweb.int/files/resources/710BDD52303B8C47492575FA00051308-Full_Report.pdf [accessed 19 January 2012].
- 4.Sack DA. When should cholera vaccine be used in cholera-endemic areas? J Health Popul Nutr. 2003;21:299–303. [PubMed] [Google Scholar]
- 5.Griffith DC, Kelly-Hope LA, Miller MA. Review of reported cholera outbreaks worldwide, 1995–2005. Am J Trop Med Hyg. 2006;75:973–7. [PubMed] [Google Scholar]
- 6.Zuckerman JN, Rombo L, Fisch A. The true burden and risk of cholera: implications for prevention and control. Lancet Infect Dis. 2007;7:521–30. doi: 10.1016/S1473-3099(07)70138-X. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization Cholera in 1997. Wkly Epidemiol Rec. 1998;73:201–8. [PubMed] [Google Scholar]
- 8.World Health Organization [Internet]. Cholera surveillance and number of cases. Geneva: WHO; 2007. Available from: http://www.who.int/topics/cholera/surveillance/en/index.html [accessed 8 January 2012].
- 9.World Health Organization [Internet]. Cholera fact sheet. Geneva: WHO; 2010. Available from: http://www.who.int/mediacentre/factsheets/fs107/en/index.html [accessed 8 January 2012].
- 10.Lanata CF, Mendoza W, Black RE. Improving diarrhoea estimates Geneva: World Health Organization; 2002. [Google Scholar]
- 11.Deen JL, von Seidlein L, Sur D, Agtini M, Lucas MES, Lopez AL, et al. The high burden of cholera in children: Comparison of incidence from endemic areas in Asia and Africa. PLoS Negl Trop Dis. 2008;2:e173. doi: 10.1371/journal.pntd.0000173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gunnlaugsson G, Angulo FJ, Einarsdóttir J, Passa A, Tauxe RV. Epidemic cholera in Guinea-Bissau: the challenge of preventing deaths in rural West Africa. Int J Infect Dis. 2000;4:8–13. doi: 10.1016/S1201-9712(00)90059-6. [DOI] [PubMed] [Google Scholar]
- 13.Lawoyin TO, Ogunbodede NA, Olumide EAA, Onadeko MO. Outbreak of cholera in Ibadan, Nigeria. Eur J Epidemiol. 1999;15:367–70. doi: 10.1023/A:1007547117763. [DOI] [PubMed] [Google Scholar]
- 14.Sur D, Lopez AL, Kanungo S, Paisley A, Manna B, Ali M, et al. Efficacy and safety of a modified killed-whole-cell oral cholera vaccine in India: an interim analysis of a cluster-randomised, double-blind, placebo-controlled trial. Lancet. 2009;374:1694–702. doi: 10.1016/S0140-6736(09)61297-6. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization Cholera vaccines: WHO position paper. Wkly Epidemiol Rec. 2010;85:117–28. [PubMed] [Google Scholar]
- 16.Madoff LC, Woodall JP. The internet and the global monitoring of emerging diseases: Lessons from the first 10 years of ProMED-mail. Arch Med Res. 2005;36:724–30. doi: 10.1016/j.arcmed.2005.06.005. [DOI] [PubMed] [Google Scholar]
- 17.Global Task Force on Cholera Control. Cholera unveiled Geneva: World Health Organization; 2003. Available from: http://whqlibdoc.who.int/hq/2003/WHO_CDS_CPE_ZFK_2003.3.pdf [accessed 8 January 2012].
- 18.Sur D, Deen JL, Manna B, Niyogi SK, Deb AK, Kanungo S, et al. The burden of cholera in the slums of Kolkata, India: Data from a prospective, community-based study. Arch Dis Child. 2005;90:1175–81. doi: 10.1136/adc.2004.071316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Agtini MD, Soeharno R, Lesmana M, Punjabi NH, Simanjuntak C, Wangsasaputra F, et al. The burden of diarrhoea, shigellosis, and cholera in North Jakarta, Indonesia: findings from 24 months surveillance. BMC Infect Dis. 2005;5:89. doi: 10.1186/1471-2334-5-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lucas ME, Deen JL, von Seidlein L, Wang XY, Ampuero J, Puri M, et al. High-level effectiveness of a mass oral cholera vaccination in Beira, Mozambique. N Engl J Med. 2005;352:757–67. doi: 10.1056/NEJMoa043323. [DOI] [PubMed] [Google Scholar]
- 21.World population prospects: the 2008 revision New York: United Nations, Department of Economic and Social Affairs, Population Division; 2009. [Google Scholar]
- 22.World Health Organization [Internet]. Population with sustainable access to improved sanitation. Geneva: WHO; 2012. Available from: http://apps.who.int/whosis/data/ [accessed 8 January 2012].
- 23.National Bureau of Statistics of China. 2006 [Internet]. China National Census. Beijing: NBSC; 2007. Available from: http://www.stats.gov.cn/english/ [accessed 8 January 2012].
- 24.National Statistics Center. Indonesia Population Census. Jakarta: NSC; 2004. Available from: http://www.bps.go.id/eng/ [accessed 8 January 2012].
- 25.Central Bureau of Health Intelligence [Internet]. National health profile 2008. New Delhi: Ministry of Health and Family Welfare; 2008. Available from: http://www.cbhidghs.nic.in/index2.asp?slid=1000&sublinkid=706 [accessed 8 January 2012].
- 26.Shaping the future – list of Member States by WHO region and mortality stratum Geneva: World Health Organization, 2003. [Google Scholar]
- 27.Shikanga OT, Mutonga D, Abade M, Amwayi S, Ope M, Limo H, et al. High mortality in a cholera outbreak in western Kenya after post-election violence in 2008. Am J Trop Med Hyg. 2009;81:1085–90. doi: 10.4269/ajtmh.2009.09-0400. [DOI] [PubMed] [Google Scholar]
- 28.Shapiro RL, Otieno MR, Adcock PM, Phillips-Howard PA, Hawley WA, Kumar L, et al. Transmission of epidemic Vibrio cholerae O1 in rural western Kenya associated with drinking water from Lake Victoria: an environmental reservoir for cholera? Am J Trop Med Hyg. 1999;60:271–6. doi: 10.4269/ajtmh.1999.60.271. [DOI] [PubMed] [Google Scholar]
- 29.DuBois AE, Sinkala M, Kalluri P, Makasa-Chikoya M, Quick RE. Epidemic cholera in urban Zambia: hand soap and dried fish as protective factors. Epidemiol Infect. 2006;134:1226–30. doi: 10.1017/S0950268806006273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Swerdlow DL, Malenga G, Begkoyian G, Nyangulu D, Toole M, Waldman RJ, et al. Epidemic cholera among refugees in Malawi, Africa: treatment and transmission. Epidemiol Infect. 1997;118:207–14. doi: 10.1017/S0950268896007352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.At least 560 infected, 7 dead in Iran cholera outbreak. Khaleej Times Online 2005 Aug 17. Available from: http://findarticles.com/p/articles/mi_kmafp/is_200508/ai_n14881015/ [accessed 20 January 2012].
- 32.Iraq: Cholera deaths rise to eight as disease spreads. IRIN humanitarian news and analysis [Internet]. 2008 Oct 15. Available from: http://gorillasguides.com/2008/10/15/iraq-cholera-deaths-rise-to-eight-as-disease-spreads/ [accessed 20 January 2012].
- 33.Death toll from cholera rising in south Yemen City hit by war. International Herald Tribune 1994 July 24. Available from: http://www.nytimes.com/1994/07/24/world/death-toll-from-cholera-rising-in-south-yemen-city-hit-by-war.html [accessed 20 January 2012].
- 34.Somalia: Cholera kills 82 in central region. Reuters and AlertNet [Internet]. 2007 Feb 5. Available from: http://www.alertnet.org/thenews/newsdesk/IRIN/289d0e116c1f0700790157eb152ae7ca.htm [accessed 20 January 2012].
- 35.Sudan cholera update, 31 July 2006 Geneva: World Health Organization; 2006. Available from: http://www.emro.who.int/sudan/Media/PDF/Cholera%20Update%201Aug.pdf [accessed 20 January 2012].
- 36.Siddique AK, Zaman K, Baqui AH, Akram K, Mutsuddy P, Eusof A, et al. Cholera epidemics in Bangladesh: 1985-1991. J Diarrhoeal Dis Res. 1992;10:79–86. [PubMed] [Google Scholar]
- 37.Rudra S, Ramakrishnan R, Hutin Y, Gupte M. A cholera outbreak in a village of West Bengal, India, 2006: The danger of using ponds for soiled clothes disposal. In: Proceedings of the Fourth South-east Asia and Western Pacific Bi-Regional TEPHINET Scientific Conference, 26–30 November 2007, Taipei, Taiwan [Google Scholar]
- 38.Sisodiya R, Hutin Y, Murhekar M, Gupte M. Unsafe water source during an outbreak of cholera in Barwai village, Madhya Pradesh, India, 2006. In: Proceedings of the Fourth South-east Asia and Western Pacific Bi-Regional TEPHINET Scientific Conference, 26–30 November 2007, Taipei, Taiwan [Google Scholar]
- 39.Sur D, Dutta S, Sarkar BL, Manna B, Bhattacharya MK, Datta KK, et al. Occurrence, significance & molecular epidemiology of cholera outbreaks in West Bengal. Indian J Med Res. 2007;125:772–6. [PubMed] [Google Scholar]
- 40.Saha S. The danger of using dirty pond water for personal hygiene during a cholera outbreak, Kachua, South 24 Parganas district, West Bengal, India, 2004 In: Proceedings of the Fourth TEPHINET Global Conference, 3–7 November 2006, Brasilia, Brazil [Google Scholar]
- 41.Annual report 2004–2005 Kolkata: National Institute of Cholera and Enteric Diseases; 2005. [PubMed] [Google Scholar]
- 42.Swain SK, Das KK, Rao TV, Baral P, Gupte MD. Cholera caused by pirated connections on a rural water supply pipeline system, Orissa, India 2003 In: Proceedings of the Fourth TEPHINET Global Conference, 3–7 November 2006, Brasilia, Brazil [Google Scholar]
- 43.Taneja N, Kaur J, Sharma K, Singh M, Kalra JK, Sharma NM, et al. A recent outbreak of cholera due to Vibrio cholerae O1 Ogawa in & around Chandigarh, North India. Indian J Med Res. 2003;117:243–6. [PubMed] [Google Scholar]
- 44.Mohan A, Radhakrishnan R, Dhanapal MP, Gupte MD. Outbreaks of cholera in Central Tamil Nadu, 2002. In: Proceedings of the Third TEPHINET Global Scientific Conference, 8–12 November 2004, Beijing, China [Google Scholar]
- 45.Pradhan MM, Pal BB, Narayan S, Rao TV. Outbreak of cholera in Pitazodi village of Orissa-2002 In: Proceedings of the Joint Annual Conference of the Indian Society for Malaria and Other Communicable Diseases and the Indian Association of Epidemiologists, 9–11 November 2002, New Delhi, India [Google Scholar]
- 46.Grossman J, Grossman M, Katz K. The first systems of weighted differential and integral calculus Charleston: BookSurge; 2006. [Google Scholar]
- 47.United Nations Statistics Division [Internet]. Millennium Development Goal indicators. New York: UNSD; 2012. Available from: http://mdgs.un.org/unsd/mdg/Data.aspx [accessed 8 January 2012].
- 48.Kimball AM, Wong K-Y, Taneda K. An evidence base for international health regulations: quantitative measurement of the impacts of epidemic disease on international trade. Rev Sci Tech. 2005;24:825–32. [PubMed] [Google Scholar]
- 49.Suarez R, Bradford B. The economic impact of the cholera epidemic in Peru: an application of the cost of illness methodology Washington: United States Agency for International Development; 1993. [Google Scholar]
- 50.World Health Organization Cholera. Wkly Epidemiol Rec. 2011;86:325–39. [Google Scholar]
- 51.Siddique AK, Ahmed S, Iqbal A, Sobhan A, Poddar G, Azim T, et al. Epidemiology of rotavirus and cholera in children aged less than five years in rural Bangladesh. J Health Popul Nutr. 2011;29:1–8. doi: 10.3329/jhpn.v29i1.7560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nair GB, Ramamurthy T, Bhattacharya MK, Krishnan T, Ganguly S, Saha DR, et al. Emerging trends in the etiology of enteric pathogens as evidenced from an active surveillance of hospitalized diarrhoeal patients in Kolkata, India. Gut Pathogens. 2010;2:4. doi: 10.1186/1757-4749-2-4. [DOI] [PMC free article] [PubMed] [Google Scholar]