With the ever-expanding geographic reach and disease burden of the current cholera pandemic, as well as alarming fatality rates in newly affected regions, it is apparent that global cholera prevention strategies are failing.1 The established treatment methods – oral rehydration, antibiotics, enhanced water and sanitation infrastructure and vaccination – have performed well in selected local and regional settings. These measures are yet to be implemented on a global scale due to economic, logistic or other practical constraints.2–4 However, the disease burden could be significantly reduced if these preventive measures could be deployed ahead of time with an early warning system before an outbreak hits a particular region.
The existence of an environmental reservoir of Vibrio cholerae, the causative agent of the disease, is well established.5 Recent findings demonstrate the strong potential to predict impending cholera outbreaks using satellite remote monitoring of coastal and terrestrial ecosystems that harbour V. cholerae. For example, data on stream flows from the major rivers of the Bengal Delta and satellite-derived plankton abundance from coastal areas in the Bay of Bengal correlate with more than 80% of the cholera prevalence in Bangladesh.5 Such predictive capability could allow the use of an operational climate-based cholera warning system that would help identify vulnerable populations up to a few months in advance. Such a system would require minimal instrumentation and operating costs, yet allow for the timely implementation of preventive measures to contain the spread of outbreaks.
With the recent and devastating return of cholera to the Caribbean region, there has been a tremendous interest in the effectiveness of interventions since the Haitian outbreak. Vaccination appears to be the predominant response, with a call for health authorities to incorporate it into existing intervention methods to reduce infection rates and minimize future epidemics.1,4 With an increasing disease burden in endemic regions and high fatality rates in newly affected regions, there is a need to examine the efficacy of existing strategies and to explore the use of predictive technology to implement proactive intervention measures.
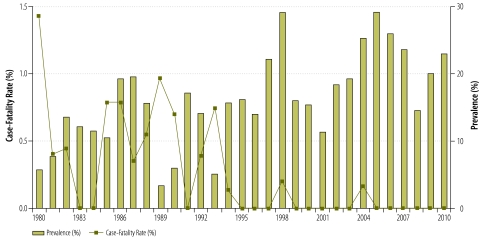
Are existing cholera intervention techniques effective in reducing the disease burden? Most cholera epidemiology, transmission, propagation and intervention literature are heavily influenced by long-term data sets generated by the International Center for Diarrhoeal Disease Research (ICDDR,B) in Bangladesh, where the disease is endemic. A closer look at the past 30 years (1980–2010) of surveillance data reveals some important trends of cholera occurrence in Dhaka, Bangladesh. Fig. 1 shows that the case-fatality rate has dropped substantially over the past three decades and death from cholera is now a rare occurrence in Bangladesh. This analysis poses a paradox – decreasing trends of fatality but increasing infection rates – and also generates questions about the efficacy of preventive measures in reducing the disease burden. Oral rehydration solution, an inexpensive and highly effective treatment, has been successfully used, backed up by aggressive information, education and outreach.2 In addition, epidemiological surveillance and health facility and laboratory-based reporting have significantly contributed to global cholera prevention and control.1,4
Fig. 1.
Average annual case-fatality rate (%) and prevalence (%) of cholera in Dhaka, Bangladesh from 1980 to 2010
Source: International Center for Diarrhoeal Disease Research, Bangladesh.
Yet, such treatment could not be translated to timely intervention in Haiti because of the inability to predict cholera outbreaks. With fatality rates less than 1% in south Asia, there is no reason for fatality rates to have exceeded 6% in Haiti.2,4 A decrease in case-fatality rate and overall reduction in disease burden can be potentially achieved by timely prediction and identification of communities at imminent risk, followed by proactive intervention. While Bangladesh and Haiti provide extreme examples of contemporary cholera epidemiology, they help identify a major knowledge gap in our understanding of the global problem. Despite having a history of successful cholera treatment, epidemic outbreaks are common in Bangladesh and prevalence shows a continuous increase over the past three decades. In Haiti, initial case-fatality rates were high, but were successfully brought down with increased access to safe water and sanitation.4 Similarly, epidemic cholera outbreaks in sub-Saharan countries in recent years have had high initial case-fatality rates, showing an urgent need for an advanced warning system to limit disease burden.4
What about primary prevention? Efforts at using vaccines to reduce infection and spread of cholera are still at an early stage of development.6 Shanchol, an affordable alternative of the well-known cholera vaccine Dukoral, is in the process of seeking WHO approval following trial studies.1,6 Meanwhile, more than a billion people in the world still lack access to clean water and remain vulnerable to cholera outbreaks.2,3 Manufacturers of the two vaccines, Dukoral and Shanchol, together produce about 2 million doses a year. Even if production and distribution was ramped up to 5 million doses a year, it would still take decades to vaccinate the approximately 100 million vulnerable people in Bangladesh alone; thus it would be very difficult to implement an effective mass vaccination programme in high-risk areas.
However, selective use of vaccination for vulnerable demographic groups – such as children and elderly people – ahead of impending outbreaks can be very effective in minimizing the impact of an epidemic.6 Evidence suggests that implementation of water, sanitation and hygiene infrastructures in vulnerable localities can also significantly reduce diarrhoeal disease prevalence.3 In Haiti, this was effective in reducing the case-fatality rate from 12% to less than 2%.4 However, before these infrastructures could be implemented, more than 3000 people had died. Arguably, many of these lives could have been saved if water and sanitation infrastructures and preventive vaccination had been administered proactively.
There is increasing evidence that proven intervention strategies would greatly benefit from the ability to predict imminent cholera outbreaks and to identify vulnerable population groups. Controlling endemic and epidemic cholera burden will require an integrated and proactive approach – a combination of prediction and prevention – based on recent advances in predictive capabilities and demonstrated successes in primary and tertiary prevention.2–5 A reliable and robust cholera prediction model will allow the mobilization of expert human (physicians and health workers) and material (vaccines, water purification and sanitation equipment, antibiotics, oral rehydration solution) resources to vulnerable areas to prepare for and implement carefully planned prevention approaches. Water and sanitation regulations and practices can be put in place and vulnerable demographic groups may be vaccinated in advance.6 Cholera outbreak warnings could be issued using the mass media and mobile-phone networks, which have been extremely successful in information dissemination during natural disasters and offer great potential to be used for epidemic warnings.
Time is a critical element for reducing cholera transmission. An early warning system based on a spatially explicit cholera prediction model can potentially provide critical lead-time to deploy human and material resources and establish preventive measures in vulnerable areas ahead of impending outbreaks.5 By combining prediction and prevention, we can reduce the cholera burden.
Acknowledgements
Shafiqul Islam is also director of Water Diplomacy, Fletcher School of Law and Diplomacy, Tufts University, MA, USA.
Funding:
This study was supported, in part, by a United States National Institutes of Health (NIH) research challenge grant (1RC1TW008587–01).
Competing interests:
None declared.
References
- 1.Ryan ET. The cholera pandemic, still with us after half a century: time to rethink. Negl Trop Dis. 2011;5:e1003. doi: 10.1371/journal.pntd.0001003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sack DA, Sack RB, Chaignat C-L. Getting serious about cholera. N Engl J Med. 2006;355:649–51. doi: 10.1056/NEJMp068144. [DOI] [PubMed] [Google Scholar]
- 3.Bartram J, Cairncross S. Hygiene, sanitation, and water: forgotten foundations of health. PLoS Med. 2010;7:e1000367. doi: 10.1371/journal.pmed.1000367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Harris JB, Larocque RC, Charles RC, Mazumder RN, Khan AI, Bardhan PK. Cholera’s western front. Lancet. 2010;376:1961–5. doi: 10.1016/S0140-6736(10)62172-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Akanda AS, Jutla AS, Alam M, de Magny GC, Kasem Siddique A, Sack RB et al. Hydroclimatic influences on seasonal and spatial cholera transmission cycles: implications for public health intervention in Bengal Delta. Water Resour. Res. 2011; 47(W00H07).
- 6.World Health Organization Cholera vaccines: WHO position paper. Weekly Epi. Rec. 2010;85:117–28. [PubMed] [Google Scholar]