Abstract
Background
The population of Germany is aging, i.e., the elderly currently make up an increasing percentage of the population from year to year. Furthermore, many common chronic diseases mainly affect the elderly. For these two reasons, the overall cost of health care in Germany is expected to increase. We studied the effect that population aging has had on the number of hospitalizations for major types of chronic disease in Germany since the year 2000.
Methods
This study is based on nationwide hospitalization statistics, classified by diagnosis, that were published by the German Federal Statistical Office. We analyzed data for three classes of diagnoses—malignant neoplasia, cardiovascular diseases, and diseases of the musculoskeletal system and connective tissue—which were further broken down into nine diagnostic subgroups. Changes in inpatient case numbers might be due either to population aging or to changing rates of hospitalization for individual diagnoses. We used index decomposition analysis to determine the relative influence of these two factors on changing case numbers.
Results
The author found that the aging of the population increased the number of hospitalizations for all of the diagnoses studied. This was particularly evident with respect to the large birth cohorts born in the 1920s (with the diagnosis of congestive heart failure) and in the period 1934–1944 (with the diagnoses ischemic heart disease, lung cancer, colorectal cancer, and osteoarthritis). On the other hand, changing rates of hospitalization for individual diagnoses increased the number of hospitalizations for some diagnoses (congestive heart failure, diseases of the spine and back) and decreased it for others (ischemic heart disease, cerebrovascular diseases, colorectal cancer, breast cancer).
Conclusion
The aging of the population and the changing rates of hospitalization for various diagnoses are exerting separate effects on the number of hospitalizations for chronic diseases in Germany. Predictions of hospital case numbers in the future must take both factors into account.
The consequences of the aging of the population in Germany are a subject of frequent debate. Population aging means that older age groups comprise a growing segment of the population as a whole as time goes by. Over the past 10 years, the proportion of the general population made up by those aged 65 or more has increased from 16.6% to 20.7% (calculated from data in [1]). The average age rose from 41 to 43 years (1). One of the reasons for this phenomenon, alongside persistently low birthrates and increasing life expectancy, is variation in the number of children born per year (2, 3). Fluctuations result from historical events; for example, fewer children were born directly after each of the two world wars, but rates rose again in the following years (see [e1] for details). Population “waves” are generated. Table 1 shows the birth cohorts that form the “crests” and “troughs” with their present ages.
Table 1. Demographic waves.
| Birth cohort | Age group | Demographic characteristic | Average number per birth year as of 31.12.2009) | ||
| 2000 | 2009 | Female | Male | ||
| 27 and earlier | 73 and older | 82 and older | Men killed in World War II | 152 | 75 |
| 1919–1930 | 70–81 | 79–90 | Increased birthrate after World War I | 254 | 131 |
| 1931–1933 | 67–69 | 76–78 | Low birthrate around time of world economic depression | 335 | 250 |
| 1934–1944 | 56–66 | 65–75 | High birthrate from 1934 | 501 | 443 |
| 1945–1947 | 53–55 | 62–64 | Low birthrate at end of World War II | 398 | 381 |
| 1948–1958 | 42–52 | 51–61 | Increased birthrate after World War II | 554 | 550 |
| 1959–1968 | 32–41 | 41–50 | Baby boomers | 681 | 709 |
| 1969–1975 | 25–31 | 34–40 | Reduced birthrate 1969–1975 | 523 | 540 |
Source: Population statistics of the German Federal Statistical Office (calculations by the author)
It seems plain that increasing demands may be placed on the health care system by the chronic diseases that are more common in the elderly.
Population aging is not a new phenomenon; on the contrary, it has been observed for many years. This leads to the question: What influence has population aging had on health care provision to date? The consequences for inpatient care can be analyzed in detail on the basis of the nationwide hospitalization statistics, classified by diagnosis, supplied by the German Federal Statistical Office. These figures have been published each year since 2000, permitting analysis of a 10-year period.
In this article I set out to show the influence of population aging on the numbers of patients treated in hospital for chronic diseases in selected diagnostic classes and subgroups since the year 2000.
Method
The data analyzed were the statistics provided by the German Federal Statistical Office (4), which break hospitalizations down by 5-year age cohort, sex, and diagnosis according to the 10th edition of the International Classification of Diseases (ICD-10), for the 10-year period from 2000 to 2009. It should be noted that hospitalization statistics count admissions, not patients. For example, a person treated several times in the same hospital will be counted anew each time.
The three diagnostic classes with the most cases were analyzed: malignant neoplasia (C00–C97, without C44), cardiovascular diseases (I00–I99), and diseases of the musculoskeletal system and connective tissue (M00–M99). Within these classes I analyzed particular diagnostic subgroups of chronic diseases that are important for inpatient care: ischemic heart disease (I20–I25), heart failure (I50), cerebrovascular diseases (I60–I69), colorectal cancer (C18–C21), lung cancer (C33–C34), breast cancer (C50), prostate cancer (C61), arthrosis (M15–M19), and dorsopathies (M40–M54).
The method of multiplicative index decomposition analysis was used to analyze the influence of aging. First, the number of hospital treatments in 2009 was divided by that in 2000. The resulting index was then multiplicatively split into two factors. The first factor quantified the change in case numbers as a consequence of change in the rate of hospitalization. The hospitalization rate depends not only on rates of incidence or prevalence, but also on other factors, such as altered “admission risks,” introduction of new diagnostic or therapeutic procedures, establishment of screening programs, and changes in coding behavior and practice, e.g., as a consequence of the introduction of the diagnosis-related groups (DRG) system for remuneration. This factor is comparable with the customary age standardization in epidemiology, in which differences related to age structure are filtered out. The second factor quantifies the influence of population aging (see eBox for details).
Results
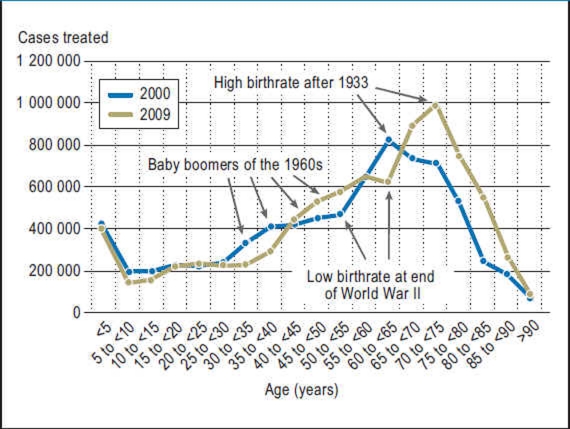
The results of index decomposition analysis are shown in Table 2, while Figure 1 presents the age structure of all hospital cases in the years 2000 and 2009.
Table 2. Index decomposition analysis: changes in inpatient treatment of selected chronic diseases between 2000 and 2009 (both sexes).
| Diagnostic class/subgroup | Case numbers | Index (change in %) | |||
| 2000 | 2009 | Total | Due to hospitalization rate | Due to population aging | |
| Both sexes | |||||
| A00–T98 All diseases and consequences of external factors | 16 723 761 | 17 567 310 | 1.050 | 0.990 | 1.061 |
| (+5.0) | (–1.0) | (+6.1) | |||
| Including | |||||
| I00–I99 Diseases of the circulatory system | 2 752 941 | 2 695 860 | 0.979 | 0.852 | 1.150 |
| (–2.1) | (–14.8) | (+15.0) | |||
| – I20–I25 Ischemic heart diseases | 895 016 | 661 317 | 0.739 | 0.641 | 1.152 |
| (–26.1) | (–35.9) | (+15.2) | |||
| – I50 Heart failure | 239 148 | 363 256 | 1.519 | 1.245 | 1.220 |
| (+51.9) | (+24.5) | (+22.0) | |||
| – I60–I69 Cerebrovascular diseases | 390 598 | 357 141 | 0.914 | 0.773 | 1.183 |
| (–8.6) | (–22.7) | (+18.3) | |||
| C00–C97 (without C44) Malignant neoplasms | 1 617 804 | 1 425 633 | 0.881 | 0.772 | 1.142 |
| (–11.9) | (–22.8) | (+14.2) | |||
| – C18–C21 Colorectal cancer | 248 352 | 173 455 | 0.698 | 0.613 | 1.139 |
| (–30.2) | (–38.7) | (+13.9) | |||
| – C33–C34 Lung cancer | 177 450 | 188 100 | 1.060 | 0.922 | 1.150 |
| (+6.0) | (–7.8) | (+15.0) | |||
| – C50 Malignant neoplasm of breast | 250 510 | 146 587 | 0.585 | 0.553 | 1.057 |
| (–41.5) | (–44.7) | (+5.7) | |||
| – C61 Malignant neoplasm of prostate | 80 088 | 83 868 | 1.047 | 0.845 | 1.239 |
| (+4.7) | (–15.5) | (+23.9) | |||
| M00–M99 Diseases of the musculoskeletal system and connective tissue | 1 239 222 | 1 641 564 | 1.325 | 1.244 | 1.065 |
| (+32.5) | (+24.4) | (+6.5) | |||
| – M15–M19 Arthrosis | 298 507 | 419 411 | 1.405 | 1.256 | 1.118 |
| (+40.5) | (+25.6) | (+11.8) | |||
| – M40–M54 Dorsopathies | 340 625 | 545 418 | 1.601 | 1.508 | 1.061 |
| (+60.1) | (+50.8) | (+6.1) | |||
Source: Hospitalization statistics of the German Federal Statistical Office (calculations by the author)
Figure 1.
Number of hospital treatments (ICD-10 codes A00 to T98) by age group in 2000 and 2009: men
The hospitalization rate for the diagnoses A00 to T98 increased by 5% from 2000 to 2009. Aging alone would have brought about an increase of 6.1%. In contrast, if only the risk had changed (with age structure constant as in 2009) the number of hospital treatments would have sunk by 1%. In the diagnostic subgroups there were particular noticeable decreases in treatments for ischemic heart disease (–26%) and colorectal cancer (–30%), while treatments for heart failure (+52%), dorsopathies (+60%), and arthrosis (+41%) showed an increasing tendency.
Division of the data by sex shows the same underlying trends for males and females, but with quantitative differences (eTable). For example, the increase in the number of treatments for heart failure was far greater in men than in women.
eTable. Index decomposition analysis: changes in inpatient treatment of selected chronic diseases between 2000 and 2009.
| Diagnostic class/subgroup | Case numbers | Index (change in %) | |||
| 2000 | 2009 | Total | Due to hospitalization rate | Due to population aging | |
| Female | |||||
| A00–T98 All diseases and consequences of external factors | 9 170 701 | 9 336 221 | 1.018 (+1.8) | 0.990 (–1.0) | 1.028 (+2.8) |
| Including | |||||
| I00–I99 Diseases of the circulatory system | 1 319 782 | 1 271 163 | 0.963 (–3.7) | 0.877 (–12.3) | 1.098 (+9.8) |
| – I20–I25 Ischemic heart disease | 320 415 | 223 830 | 0.699 (–30.1) | 0.636 (–36.4) | 1.099 (+9.9) |
| – I50 Heart failure | 138 201 | 191 660 | 1.387 (+38.7) | 1.217 (+21.7) | 1.139 (+13.9) |
| – I60–I69 Cerebrovascular diseases | 210 454 | 179 532 | 0.853 (–14.7) | 0.764 (–23.6) | 1.117 (+11.7) |
| C00–C97 (without C44) Malignant neoplasms | 816 776 | 651 119 | 0.797 (–20.3) | 0.731 (–26.9) | 1.090 (+9.0) |
| – C18–C21 Colorectal cancer | 114 767 | 74 443 | 0.649 (–35.1) | 0.597 (–40.3) | 1.087 (+8.7) |
| – C33–C34 Lung cancer | 45 758 | 60 134 | 1.314 (+31.4) | 1.215 (+21.5) | 1.081 (+8.1) |
| – C50 Malignant neoplasm of breast | 250 510 | 146 587 | 0.585 (–41.5) | 0.553 (–44.7) | 1.057 (+5.7) |
| M00–M99 Diseases of the musculoskeletal system and connective tissue | 687 012 | 933 669 | 1.359 (+35.9) | 1.286 (+28.6) | 1.057 (+5.7) |
| – M15–M19 Arthrosis | 190 041 | 259 962 | 1.368 (+36.8) | 1.256 (+25.6) | 1.089 (+8.9) |
| – M40–M54 Dorsopathies | 178 153 | 299 306 | 1.680 (+68.0) | 1.595 (+59.5) | 1.053 (+5.3) |
| Male | |||||
| A00–T98 All diseases and consequences of external factors | 7 553 060 | 8 231 089 | 1.090 (+9.0) | 0.991 (–0.9) | 1.100 (+10.0) |
| Including | |||||
| I00–I99 Diseases of the circulatory system | 1 433 159 | 1 424 697 | 0.994 (–0.6) | 0.830 (–17.0) | 1.198 (+19.8) |
| – I20–I25 Ischemic heart disease | 574 601 | 437 487 | 0.761 (–23.9) | 0.644 (–35.6) | 1.182 (+18.2) |
| – I50 Heart failure | 100 947 | 171 596 | 1.700 (+70.0) | 1.277 (+27.7) | 1.331 (+33.1) |
| – I60–I69 Cerebrovascular diseases | 180 144 | 177 609 | 0.986 (–1.4) | 0.783 (–21.7) | 1.260 (+26.0) |
| C00–C97 (without C44) Malignant neoplasms | 801 028 | 774 514 | 0.967 (–3.3) | 0.809 (–19.1) | 1.195 (+19.5) |
| – C18–C21 Colorectal cancer | 133 585 | 99 012 | 0.741 (–25.9) | 0.626 (–37.4) | 1.183 (+18.3) |
| – C33–C34 Lung cancer | 131 692 | 127 966 | 0.972 (–2.8) | 0.828 (–17.2) | 1.174 (+17.4) |
| – C61 Malignant neoplasm of prostate | 80 088 | 83 868 | 1.047 (+4.7) | 0.845 (–15.5) | 1.239 (+23.9) |
| M00–M99 Diseases of the musculoskeletal system and connective tissue | 552 210 | 707 895 | 1.282 (+28.2) | 1.193 (+19.3) | 1.075 (+7.5) |
| – M15–M19 Arthrosis | 108 466 | 159 449 | 1.470 (+47.0) | 1.257 (+25.7) | 1.169 (+16.9) |
| – M40–M54 Dorsopathies | 162 472 | 246 112 | 1.515 (+51.5) | 1.415 (+41.5) | 1.070 (+7.0) |
Source: Hospitalization statistics of the German Federal Statistical Office (calculations by the author)
In contrast, the two sexes show distinctly different trends for lung cancer. In men there was a slight decrease in treatments, in women a sharp increase.
The index partition showed that in the period analyzed, population aging increased the case numbers in all selected diagnostic subgroups. Particularly strong effects were observed for the diagnoses heart failure, cerebrovascular diseases, and prostate cancer. Basically, the aging effects were (sometimes much) greater in men than in women.
Equally, it could be seen that the effects of change in the hospitalization rate varied according to diagnostic subgroup. The number of treatments for ischemic heart disease went down by 36%—and for breast cancer by as much as 45%—because of the change in hospitalization rate alone. In other diagnostic subgroups, however, change in hospitalization rate increased the case numbers. This was observed particularly for dorsopathies (+51%), arthrosis (+26%), and heart failure (+24%).
Various combinations of the two factors were seen in different diagnostic subgroups:
Cumulative effects of the two factors were observed for arthrosis, dorsopathies, and heart failure, where the separate influences exerted by population aging and change in risk added up to an increase in case numbers of 40% or more.
For lung cancer and prostate cancer, the effects of aging more than compensated for the decrease in case numbers brought about by lowering of the hospitalization rate, resulting in a slight increase of around 5% in the number of cases.
In ischemic heart disease, cerebrovascular diseases, colorectal cancer, and breast cancer, the effects of the decreased rate of hospitalization more than compensated for those of aging, resulting in distinct decreases in case numbers of up to 41%.
Discussion
The wavelike changes in age structure brought about by population aging affect case numbers. Figure 1 shows how particular birth cohorts produce peaks and troughs that progress through the age structure of hospital cases. For example, the large number of births in the years following 1933 resulted in the peak of 60- to 65-year-olds in 2000 and the peak of 70- to 75-year-olds in 2009.
By means of index decomposition analysis, the changes in case numbers in the study period were split into two factors: an age structure-related factor, and a factor that identified the effects of the “risk” of receiving inpatient treatment, i.e., the hospitalization rate, for a given diagnosis. Each of these factors can both elevate and depress numbers of cases.
Sizable increases in case numbers were observed for the diagnostic subgroups heart failure and dorsopathies. These increases may have been the result of increasing prevalence. For example, the growth in the frequency of heart failure in the USA has been described as an epidemic (5, 6); the numbers of cases with heart failure as primary or secondary diagnosis tripled between 1979 and 2004 (7).
The strong aging effect seen in heart failure, particularly in men, was accompanied by a high average age. This corresponded to findings from analyses of hospital patients in other countries (7– 10). The reason for the aging effect lies in the age cohort born between 1919 and 1930. This population had crossed the threshold age of 60 years, after which the risk of suffering heart failure doubles with every additional decade (11) and the hospitalization rate for this diagnosis begins to increase steeply (12). In Germany, a considerable proportion of men born in that period died in World War II (Table 1). The proportion of the population made up by this birth cohort is steadily decreasing, and they are being replaced by later-born cohorts not affected by war losses.
Altogether, population aging and the growing hospitalization rate had cumulative effects on the frequency of the diagnosis heart failure.
Only a small part of the marked increase in the numbers of cases with the diagnosis dorsopathies was attributable to aging. A far greater role was played by the increased rate of hospitalization for this diagnosis. A study from the USA shows growing prevalence rates in the population (13). Increasing prevalence could also go at least some way towards explaining the rising hospitalization rate in Germany. The diagnostic subgroup arthrosis comprised mainly arthrosis of the knee and hip, and the increase in cases was plainly an expression of the higher rates of implantation of prostheses in these joints (Table 3).
Table 3. Operations for implantation of a knee- or hip-joint prosthesis.
| Hip | Knee | |
| 2005 | 194 453 | 128 932 |
| 2006 | 199 040 | 135 393 |
| 2007 | 204 018 | 146 562 |
| 2008 | 209 912 | 154 722 |
| 2009 | 213 174 | 159 137 |
Source: DRG statistics (hospital statistics based on case flat rates), operations and procedures performed to treat hospital inpatients, German Federal Statistical Office
The apparent stability of the number of cases with the diagnosis prostate cancer was illusory; a glance at the results of index decomposition analysis shows that the hospitalization rate went down, while the effects of aging increased case numbers. These effects were exerted by different age groups than was the case for heart failure; the risk of prostate cancer increases considerably from the 55- to 59-year age group onwards (14). During the study period this age was reached by those in the birth cohort 1934 to 1944, which was larger than those from the previous and following years, thus increasing the number of cases.
The number of cases with the diagnosis ischemic heart disease was dominated by opposing trends: An aging-associated increase was more than compensated by the decrease in hospital admissions. In the USA, researchers have noted a decline in the incidence of acute myocardial infarction (15), with a total fall of 24% between 1998 and 2008. Decreasing incidence has also been reported from the UK (e2). This decrease—together with the observed fall in mortality (e3)—is due to improvements in cardiovascular risk factors (16). The rates of hospitalization for acute myocardial infarction in the USA have been sinking since the mid-1990s (17). The diagnostic subgroup ischemic heart disease includes more than just myocardial infarction; however, the other diagnoses in the subgroup are all manifestations of the same underlying disease, namely arteriosclerosis of the coronary vessels. The number of patients discharged after a short hospital stay with the primary diagnosis of ischemic heart disease fell by 26% in the USA between 1997 and 2007 (18).
It can be affirmed that the mortality, incidence, and hospitalization rates have been decreasing for well over 10 years in the USA and the UK. With the exception of one analysis of mortality (e4), no studies of this nature have been carried out in Germany. It can be assumed, however, that the underlying trends are similar in this country. In this respect, the decrease in the number of cases with the diagnosis ischemic heart disease would (at least partially) reflect a decrease in incidence.
The situation is similar for cerebrovascular diseases. Falling rates of incidence and mortality have been reported from several countries (19– 22), together with decreasing rates of hospital treatment (18, 19, 23, 24).
As outlined above, the rate of hospitalization for a given diagnosis may depend not only on the incidence but also on other factors, as shown for cerebrovascular diseases. One such factor is the introduction of the DRG system for remuneration and the associated changes in coding behavior.
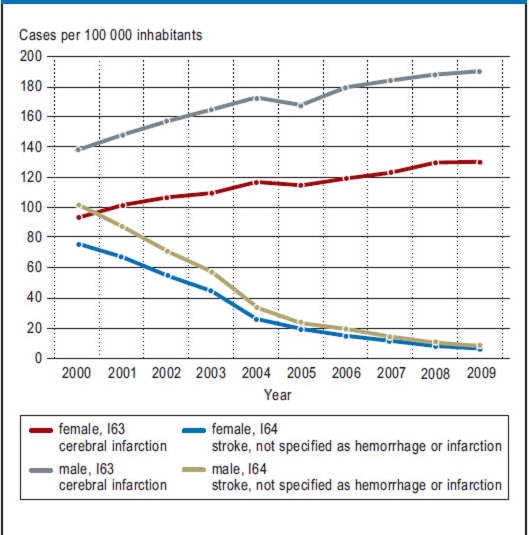
The most important disease in the diagnostic subgroup cerebrovascular diseases is stroke, for which there are several ICD codes. Of the 391 000 inpatient cases with the diagnosis cerebrovascular diseases in the year 2000 in Germany, 136 000 were coded as “cerebral infarction” (I63) and 112 000 as “stroke, not specified as hemorrhage or infarction” (I64). Together, these two codes made up 63% of all diagnoses in the code group I60 to I69. The DRG coding instructions specify that I64 is to be assigned only in cases where the codes I60 to I63 do not apply (e5). This ruling was put into practice gradually, as shown by the development of the age-standardized rates of treatment for the two principal diagnoses I63 and I64 (Figure 2). The treatment rates of cases coded with I64 are decreasing sharply, while those coded with I63 are on the increase. There has thus been a shift from one ICD code to another.
Figure 2.
Age-standardized treatment rates for the diagnoses ICD-10 I63 and I64 in 2000 and 2009 (cases per 100 000 inhabitants, standardized by age, old European standard population)
An interesting constellation can be observed on sex-specific analysis of the treatments for the diagnosis lung cancer. In both sexes the case numbers were increased by aging effects. The large birth cohort 1934 to 1944 reached the age of 65 to 80 years, at which the rate of hospitalization for lung cancer is greatest, during the study period. The hospitalization rate changed differently in men and women. In men it decreased considerably, while in women it increased. This finding corresponds with falling incidence rates for lung cancer in men and rising incidence in women (25). This contrasting development can be attributed to changes in smoking behavior in previous decades (e6, e7).
The reduction in the number of cases with the diagnosis colorectal cancer resulted from the decreasing rate of hospitalization. The latter parallels the (age-standardized) incidence of colorectal cancer, which rose in the final years of the 20th century but has been falling since (14). This decrease was partially compensated by the effects of aging.
Breast cancer showed a similar development. The reduction in hospitalization rate—which has also been described elsewhere, e.g., in Switzerland (e8)—was partially compensated by aging.
Limitations
When interpreting the data it is important to realize that changes in case numbers do not necessarily reflect changes in incidence or prevalence at the population level. Patients may be admitted for hospital treatment several times during a calendar year. However, the present analysis of data from various hospital entities shows that the nationwide hospitalization statistics, classified by diagnosis, can be used to identify trends in inpatient care that correspond to trends at population level.
Conclusions
The aging-related changes in case numbers are determined particularly by the large birth cohorts in the years 1934 to 1944 (diagnostic subgroups ischemic heart disease, lung cancer, colorectal cancer, and arthrosis) and 1948 to 1958, with the low-birthrate years of 1945 to 1947 (diagnostic subgroups cerebrovascular diseases, prostate cancer, and breast cancer) sandwiched in between. Those born in the years after World War I have strongly affected the development with regard to heart failure.
The strong aging effects in men arise above all from the fact that surviving members of the generation with a sex imbalance owing to the deaths in World War II are steadily becoming fewer. The following cohorts have a more balanced sex distribution and thus a higher proportion of men than the war generation. Another reason is a more pronounced increase in male compared to female life expectancy in recent years (e9).
The changes in hospital case numbers caused by aging can therefore be attributed to particular age groups and thus to particular birth cohorts. The wavelike evolution of age structure—the succession of “crests” and “troughs”—affects inpatient care in different ways at different times. It can be assumed that population aging will continue to have this kind of undulating effect on inpatient treatments of various chronic diseases in the future. Moreover, the hospitalization rate according to diagnostic subgroup has changed noticeably.
Predictions of future developments in hospital treatment must therefore take account of both population aging and possible changes in risk. Many prognoses in the field of health care are based exclusively on population aging (see [e10] for a selection). Needing to consider possible changes in risk places more strenuous demands on prognoses and makes their preparation more complex. The present research article is intended as a contribution to enabling such predictions.
Key Messages.
Population aging led to a 6% increase in inpatient case numbers in Germany between 2000 and 2009.
The influence of aging on treatment numbers for a given diagnostic subgroup may be amplified, attenuated, or canceled out by the change in rate of hospitalization. For the diagnoses heart failure and dorsopathies, for example, the effects of aging and increased hospitalization rate add up to an increase of 40% or more in numbers of admissions.
For other diagnoses (ischemic heart disease, cerebrovascular diseases, colorectal cancer, breast cancer), the effects of a reduced hospitalization rate more than compensated for the effects of aging. Case numbers for individual diagnostic subgroups went down by as much as 45%.
The wavelike evolution of the population age structure and the changes in hospitalization rates have exerted differentiated effects on hospital case numbers in the various diagnostic subgroups over the past 10 years.
Predictions of future developments must take both factors into account
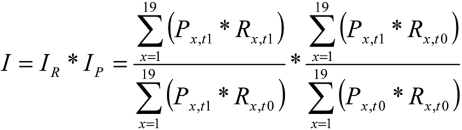
eBOX. Methods.
The data analyzed were derived from nationwide hospitalization statistics, classified by diagnosis (4). These statistics include all hospitals in Germany with the exception of prison hospitals and police hospitals. Army hospitals are included only if they provide services to civilian patients. The unit non-response rate was 0.2% (e11).
The data classify patients by 5-year age group, sex, and diagnosis. I analyzed the 10-year period 2000 to 2009, for which hospital data classified according to ICD-10 were available. When evaluating hospital diagnosis statistics it is important to note that they count cases, not patients. A person treated several times at the same hospital will be counted again each time.
The three diagnostic classes with the most cases were analyzed: malignant neoplasms (C00–C97, without C44), diseases of the circulatory system (I00–I99), and diseases of the musculoskeletal system and connective tissue (M00–M99). Within these classes I analyzed particular diagnostic subgroups of chronic diseases that are important for inpatient care: ischemic heart disease (I20–I25), heart failure (I50), cerebrovascular diseases (I60–I69), colorectal cancer (C18–C21), lung cancer (C33–C34), malignant neoplasm of breast (C50), malignant neoplasm of prostate (C61), arthrosis (M15–M19), and dorsopathies (M50–M54).
The influence of aging was evaluated using the Laspeyres method of index decomposition analysis. This simple procedure, named after German economist Étienne Laspeyres (1834–1913), is commonly used in economics (e12).
The utilization of the Laspeyres procedure is based on the fact that case numbers are the product of the total population and the rate of hospitalization for a given diagnosis (classified by age group and sex). First, the number of cases in 2009 was divided by that in 2000. The resulting quotient was termed the index (I). The value of I was 1 if no change had taken place, >1 if there had been an increase in case numbers, and <1 if there had been a decrease. The index was then multiplicatively split into two factors. One of these factors (IR; see equation below) quantified the change in case numbers as a consequence of the change in “risk of treatment” (i.e., hospitalization rate) for a given diagnosis. IR can be interpreted as a change in case numbers if only the hospitalization rate has changed, not the age structure of the population. The rate of hospitalization depends not only on rates of incidence or prevalence, but also on other aspects such as changed “admission risk”, introduction of new diagnostic or therapeutic procedures, establishment of screening programs, or alterations in coding behavior and practice, e.g., as a consequence of the diagnosis-related groups (DRG) system of remuneration. IR is comparable to the age standardization customary in epidemiology, by means of which age structure-related differences between parameters are eliminated.
The second factor (IP) expressed how the case numbers for a given diagnosis would have altered if only the age structure, not the rate of hospitalization, had changed. IP thus quantified the influence of population aging. Strictly speaking, IP is also affected by changes in the total population; this influence can be ignored in the present case, however, because the population of Germany changed very little (decreased by 0.6%) between 2000 and 2009.
P, population, by age group
R, risk of treatment, by age group
x, 5-year age group (with 90 and older as highest age group)
t0, 2000
t1, 2009
Acknowledgments
Translated from the original German by David Roseveare.
Footnotes
Conflict of interest statement
The author declares that no conflict of interest exists.
References
- 1.Statistisches Bundesamt. Bevölkerungsfortschreibung. Wiesbaden: Fachserie 1, Reihe 1.3; Bevölkerung und Erwerbstätigkeit; 2009a pp. [Google Scholar]
- 2.Dinkel RH. Was ist demographische Alterung? Der Beitrag der demographischen Parameter zur demographischen Alterung in den alten Bundesländern seit 1950. Was ist Alter(n)? Neue Antworten auf eine scheinbar einfache Frage. In: Häfner H, Staudinger UM, editors. Berlin: Springer; 2008. pp. 97–117. [Google Scholar]
- 3.Schwarz K. Bestimmungsgründe der Alterung einer Bevölkerung - Das deutsche Beispiel. Z Bevolkerungswiss. 1997;22:347–359. [Google Scholar]
- 4.Statistisches Bundesamt Diagnosedaten der Krankenhäuser ab 2000. (Thematische Recherche: Krankheiten/ Gesundheitsprobleme, Krankheiten allgemein; Dokumentart Tabellen) ( http://www.gbe-bund.de/) (last accessed on 19 October 2011)
- 5.Giamouzis G, Kalogeropoulos A, Georgiopoulou V, et al. Hospitalization epidemic in patients with heart failure: Risk factors, risk prediction, knowledge gaps, and future directions. Journal of Cardiac Failure. 2011;17:54–75. doi: 10.1016/j.cardfail.2010.08.010. [DOI] [PubMed] [Google Scholar]
- 6.Gheorghiade M, Sopko G, De Luca L, et al. Navigating the cross-roads of coronary artery disease and heart failure. Circulation. 2006;114:1202–1213. doi: 10.1161/CIRCULATIONAHA.106.623199. [DOI] [PubMed] [Google Scholar]
- 7.Fang J, Mensah GA, Croft JB, et al. Heart failure-related hospitalization in the US., 1979 to 2004. J Am Coll Cardiol. 2008;52:428–434. doi: 10.1016/j.jacc.2008.03.061. [DOI] [PubMed] [Google Scholar]
- 8.Nicol ED, Fittal B, Roughton M, et al. NHS heart failure survey: a survey of acute heart failure admissions in England, Wales und Northern Ireland. Heart. 2008;94:172–177. doi: 10.1136/hrt.2007.124107. [DOI] [PubMed] [Google Scholar]
- 9.Najafi F, Dobson AJ, Jamrozik K. Recent changes in heart failure hospitalisations in Australia. European Journal of Heart Failure. 2007;9:228–233. doi: 10.1016/j.ejheart.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 10.McMurray J, McDonagh T, Morrison CE, et al. Trends in hospitalization for heart failure in Scotland 1980-1990. European Heart Journal. 1993;14:1158–1162. doi: 10.1093/eurheartj/14.9.1158. [DOI] [PubMed] [Google Scholar]
- 11.Mohacsi P, Moschovitis G, Tanner H, et al. Prevalence, increase, and costs of heart failure. Heart and Metabolism. 2001;14:9–16. [Google Scholar]
- 12.Cleland JGF, Gemmell I, Khand A, et al. Is the prognosis of heart failure improving? European Journal of Heart Failure. 1999;1:229–241. doi: 10.1016/s1388-9842(99)00032-x. [DOI] [PubMed] [Google Scholar]
- 13.Freburger JK, Holmes GM, Agans RP, et al. The rising prevalence of chronic low back pain. Arch Intern Med. 2009;169:251–258. doi: 10.1001/archinternmed.2008.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Robert Koch-Institut. Entwicklung der Prävalenzen zwischen 1990 und 2010. Berlin: RKI; 2010. Verbreitung von Krebserkrankungen in Deutschland. [Google Scholar]
- 15.Yeh RW, Sidney S, Chandra M, et al. Population trends in the incidence and outcomes of acute myocardial infarction. New England Journal of Medicine. 2010;362:2155–2165. doi: 10.1056/NEJMoa0908610. [DOI] [PubMed] [Google Scholar]
- 16.Hardoon SL, Whincup PH, Lennon LT, et al. How much of the recent decline in the incidence of myocardial infarction in british men can be explained by changes in cardiovascular risk factors? Evidence from a prospective population-based study. Circulation. 2008;117:598–604. doi: 10.1161/CIRCULATIONAHA.107.705947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fang J, Alderman MH, Keenan NL, et al. Acute myocardial infarction hospitalization in the United States, 1979 to 2005. The American Journal of Medicine. 2010;123:259–266. doi: 10.1016/j.amjmed.2009.08.018. [DOI] [PubMed] [Google Scholar]
- 18.Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics-2011 update: A report from the American Heart Association. Circulation. 2011;123:e18–e209. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lewsey JD, Jhund PS, Gillies M, et al. Age- and sex-specific trends in fatal incidence and hospitalized incidence of stroke in Scotland, 1986 to 2005. Circulation: Cardiovascular Quality and Outcomes. 2009;2:475–483. doi: 10.1161/CIRCOUTCOMES.108.825968. [DOI] [PubMed] [Google Scholar]
- 20.Carandang R, Seshadri S, Beiser A, et al. Trends in incidence, lifetime risk, severity, and 30-day mortality of stroke over the past 50 years. JAMA. 2006;296:2939–2946. doi: 10.1001/jama.296.24.2939. [DOI] [PubMed] [Google Scholar]
- 21.Sutton CJ, Marsden J, Watkins CL, et al. Changing stroke mortality trends in middle-aged people: an age-period-cohort analysis of routine mortality data in persons aged 40 to 69 in England. Journal of Epidemiology and Community Health. 2010;64:523–529. doi: 10.1136/jech.2008.086785. [DOI] [PubMed] [Google Scholar]
- 22.Rothwell PM, Coull AJ, Giles MF, et al. Change in stroke incidence, mortality, case-fatality, severity, and risk factors in Oxfordshire, UK from 1981 to 2004 (Oxford Vascular Study) Lancet. 2004;363:1925–1933. doi: 10.1016/S0140-6736(04)16405-2. [DOI] [PubMed] [Google Scholar]
- 23.Béjot Y, Aouba A, de Peretti C, et al. Time trends in hospital-referred stroke and transient ischemic attack: Results of a 7-year nationwide survey in France. Cerebrovascular Diseases. 2010;30:346–354. doi: 10.1159/000319569. [DOI] [PubMed] [Google Scholar]
- 24.Fang J, Alderman MH, Keenan NL, et al. Declining US stroke hospitalization since 1997: National Hospital Discharge Survey, 1988-2004. Neuroepidemiology. 2007;29:243–249. doi: 10.1159/000112857. [DOI] [PubMed] [Google Scholar]
- 25.Robert Koch-Institut und die Gesellschaft der epidemiologischen Krebsregister in Deutschland e.V. Häufigkeiten und Trends. 7th edition. Berlin: RKI; 2010. Krebs in Deutschland 2005/2006. [Google Scholar]
- e1.Bundesinstitut für Bevölkerungsforschung. Wiesbaden: 2008. Bevölkerung. Daten, Fakten, Trends zum demographischen Wandel in Deutschland. [Google Scholar]
- e2.Davies AR, Grundy E, Nitsch D, et al. Constituent country inequalities in myocardial infarction incidence and case fatality in men and women in the United Kingdom, 1996-2005. Journal of Public Health. 2011;33:131–138. doi: 10.1093/pubmed/fdq049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e3.Ford ES, Ajani UA, Croft JB, et al. Explaining the decrease in US. deaths from coronary disease, 1980-2000. New England Journal of Medicine. 2007;356:2388–2398. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- e4.Müller-Riemenschneider F, Andersohn F, Willich S. Trends in age-standardised and age-specific mortality from ischaemic heart disease in Germany. Clinical Research in Cardiology. 2010;99:545–551. doi: 10.1007/s00392-010-0151-9. [DOI] [PubMed] [Google Scholar]
- e5.Zaiß AH. Deutsche Kodierrichtlinien mit Tipps, Hinweisen und Kommentierungen. Köln: Deutscher Ärzte-Verlag; 2009. DRG: Verschlüsseln leicht gemacht. [Google Scholar]
- e6.Donington J, Le Q-T, Wakelee H. Lung cancer in women: Exploring sex differences in susceptibility, biology, and therapeutic response. Clinical Lung Cancer. 2006;8:22–29. doi: 10.3816/CLC.2006.n.029. [DOI] [PubMed] [Google Scholar]
- e7.Deppermann KM. Epidemiologie des Lungenkarzinoms. Internist. 2011;52:125–129. doi: 10.1007/s00108-010-2695-1. [DOI] [PubMed] [Google Scholar]
- e8.Lippuner K, Grifone S, Schwenkglenks M, et al. Comparative trends in hospitalizations for osteoporotic fractures and other frequent diseases between 2000 and 2008. Osteoporos Int 2011. 2011 May 28; doi: 10.1007/s00198-011-1660-8. Epub Date. [DOI] [PubMed] [Google Scholar]
- e9.Robert Koch-Institut. Berlin: RKI; 2011. Sterblichkeit, Todesursachen und regionale Unterschiede. [Google Scholar]
- e10.Nowossadeck E. Morbiditätsprognosen auf Basis von Bevölkerungsprognosen. Welchen Beitrag kann ein Gesundheitsmonitoring leisten? Bundesgesundheitsblatt - Gesundheitsforschung - Gesundheitsschutz. 2010;53:427–434. doi: 10.1007/s00103-010-1048-5. [DOI] [PubMed] [Google Scholar]
- e11.Statistisches Bundesamt. Fachserie 12, Reihe 6. Wiesbaden: 2009. Gesundheit. Diagnosedaten der Patienten und Patientinnen in Krankenhäusern. [Google Scholar]
- e12.Rinne H. Erläuterungen - Erhebungen - Ergebnisse. München, Wien: R. Oldenbourg Verlag; 1996. Wirtschafts- und Bevölkerungsstatistik. [Google Scholar]