INTRODUCTION
Estimates of the incidence and impact of bacterial infective endocarditis (IE) have been limited by the infrequency of the disease. Administrative data analyses can provide important information across a broad range of hospitals and regions. We used a recent, nationally representative sample to estimate the incidence of hospitalizations for bacterial IE in the United States.
METHODS
We conducted a retrospective cohort study using the1999–2008 Nationwide Inpatient Sample (NIS), which is produced by the Agency for Healthcare Research and Quality. The NIS is the largest all-payer inpatient database in the United States(approximately8 million records per year).1 Admissions related to bacterial IE were identified by the presence of International Classification of Diseases, Ninth Edition codes 421.0, 421.1, 421.9 or 996.61, combining two previous strategies.2, 3 The etiological agent of IE was determined by the presence of organism-specific infection (e.g. 041.x) and bacteremia codes (038.x). Incidence was estimated using the rate of IE-related discharges per 100,000 US population-years. Rates were calculated quarterly based on discharge date; the denominator was adjusted annually based on the US population. Trends in admission rate were evaluated using joinpoint methods, allowing the trend to change over time.4 We measured the effect of organism on in-hospital mortality using logistic regression, adjusted for age, gender, payer, and comorbidities. The dataset was constructed in SAS System, version 9.22; analyses were performed in Stata/IC, version 11.2 and Joinpoint Regression Program, version 3.4.3, using the stratification and weighting data provided with the NIS to create nationally-representative estimates. Additional detail on study methods is available in an online appendix.
RESULTS
Of the 78.2 million records in the 1999–2008 NIS, 93,511 met inclusion criteria. Using weights, these records correspond to457,690 discharges nationwide. After exclusion of 9,538 admissions ending in inpatient transfer and 273 (0.3%) with unknown disposition, the main study sample consisted of 83,700 discharges (409,665 weighted). Most episodes involved patients who were male (59.3%), white (71.4%), and insured by Medicare (57.2%). Of those discharges for which an organism was identified, staphylococci were most common (57.5%), followed by streptococci/enterococci (33.3%).
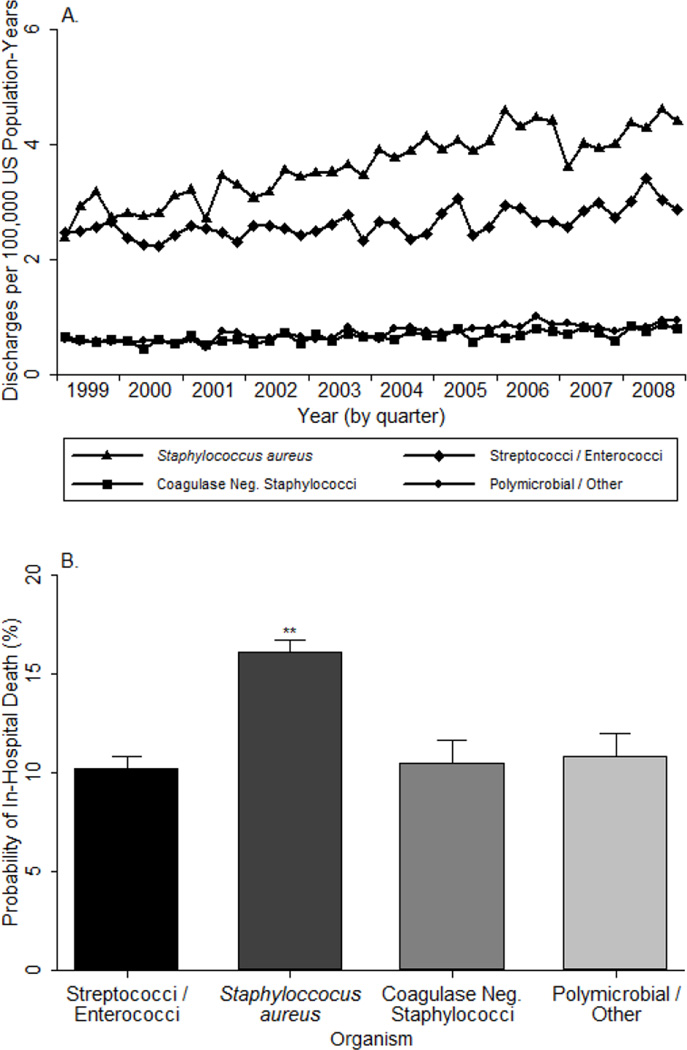
Between the first quarter of 1999 and the first quarter of 2006, the rate of bacterial IE-related hospitalizations increased from 11.4 per 100,000 population-years to 16.6 per 100,000 population-years (test of trend, p < 0.001). This trend corresponds to an average percent change (APC) of 1.1% per quarter (95% confidence interval (CI): 0.9% to 1.3%). After the first quarter of 2006, the rate stabilized, with an APC of 0.1% (95% CI: −0.6% to 0.8%). Substantial differences were evident in the rate of IE-related admissions caused by different organisms over the study period (Figure 1A). Admissions associated with staphylococcal IE grew at a rate of 1.1% per quarter (95% CI: 0.9% to 1.3%), rising from 3.3 to 5.4 cases per 100,000 person-years from first quarter 1999 to fourth quarter 2008 (test of linear trend, p < 0.001). Most of the increase in staphylococcal IE admissions was due to IE caused by S. aureus, which increased at a rate of 1.7% per quarter between first quarter 1999 and first quarter 2006 (95% CI: 1.3% to 2.0%). Interestingly, rates of S. aureus-associated IE stabilized between 2006 and 2008 (APC 0.1%, 95% CI: −1.1% to 1.2%).
Figure 1.
(A) Temporal trend in the total rate of bacterial infective endocarditis-associated hospitalizations in the United States: 1999–2008; (B) Covariate-adjusted in-hospital mortality
** Significantly different from streptococci/enterococci at 0.1% level.
We limited the cohort to 33,956 admissions(165,563 weighted) that occurred in 2002 or later, for which a etiologic organism was identified (excluding unknown organisms and unspeciated staphylococcus), and which had complete covariate data. Admissions for S. aureus-related IE were associated with higher probability of in-hospital mortality than streptococcal/enterococcal IE (17.5% versus 8.9%, p < 0.001). After adjustment, IE caused by S. aureus was associated with a 57.1% greater risk of in-hospital mortality (risk difference: 5.9% p < 0.001) when compared with streptococcal/enterococcal IE (Figure 1B).
DISCUSSION
This report estimates the current incidence and trends in hospitalizations due to bacterial IE in the United States at the beginning of the 21st Century. We found that the rate of IE-related hospitalizations grew markedly, and that this growth was driven primarily by increases in S. aureus IE. Patients with S. aureus IE were also more likely to die during the hospitalization. Since these findings were drawn from a representative sample of over 78 million hospitalizations, they are generalizable to contemporary medical practice.
Our finding that S. aureus is the predominant cause of IE in the 21st Century is consistent with results from the International Collaboration on Endocarditis.3 Our results contrast with those of Tleyjeh and colleagues, who found no significant change in IE rates or etiology during 1970–2000 in Olmstead County, Minnesota.5 The generalizability of that important study was limited by its small size (107 IE cases during the 30 year time period), small geographic scope, and lack of racial and ethnic diversity. By contrast, the current investigation involved a nationally-representative sample of contemporary US admissions.
This investigation has important strengths. Our study design employs a large, contemporary, and nationally representative dataset. Such a dataset avoids referral bias,6 ensures that our results are broadly generalizable, and allows for sufficient sample size for statistical inference. The study is limited by its use of ICD-9 diagnosis codes, which have been associated with both false positive and negative findings.7 However, others have reported good agreement between IE diagnosis codes and clinical criteria obtained from medical records.8 Our inability to access laboratory results resulted in a relatively high proportion of IE cases without organism identification (43.8%). However, the number of unidentified cases grew at a rate similar to that of identified cases (APC 1.1% versus 1.2%), suggesting that our findings are not due to improvements in coding.
Despite these limitations, our study is uniquely able to make a number of observations. We estimate the incidence of bacterial IE in the United States and document its increasing prevalence in the early 21st Century. This growth was attributed primarily to increased rates of IE related to S. aureus, which was associated with worse outcomes and higher costs compared to IE caused by other organisms.
Supplementary Material
ACKNOWLEDGEMENTS
We thank Tiffany Jewell, RHIA for her assistance with developing the coding criteria. Peter H. Gilligan, PhD assisted in formulating the research objectives and design. Any errors are solely the responsibility of the authors.
Financial Support. National Institute of General Medical Sciences (T32GM008719), National Institute on Aging (R01 AG025801), National Institute of Allergy and Infectious Diseases (R01-AI068804; K24 AI093969), National Heart, Lung, and Blood Institute (F30 HL110483), and American Heart Association (0675027N). None of the funding agencies had any role in the design and conduct of the study, the collection, management, analysis, and interpretation of the data, or the preparation, review or approval of the manuscript. Mr. Federspiel had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Financial Disclosures: J.J.F.: Mr. Federspiel is employed by the University of North Carolina at Chapel Hill and has received grant support from the National Institutes of Heath; S.C.S.: Dr. Stearns is employed by the University of North Carolina at Chapel Hill and has received grant support from the National Institutes of Health; A.F.P.: Dr. Peppercorn is employed by GlaxoSmithKline; V.H.C.: Dr. Chu has received research support from Merck and Pfizer and is employed by Duke University; V.G.F.: Dr. Fowler has served as a consultant for Astellas, Cubist, Inhibitex, Merck, Johnson & Johnson, Shire, Leo Pharmaceuticals, NovaDigm, The Medicines Company, Baxter Pharmaceuticals & Biosynexus; has received grant or research support from Astellas, Cubist, Inhibitex, Merck, Theravance, Cerexa, Pfizer, Novartis, Advanced Liquid Logic and National Institute of Health; has received honoraria from Arpida, Astellas, Cubist, Inhibitex, Merck, Pfizer, Targanta, Theravance, Wyeth, Ortho-McNeil, Novartis & Vertex Pharmaceuticals; has served on an advisory committee for Cubist; is employed by Duke University; and has served as a speaker's bureau for Cubist.
Preliminary data will be presented at the Interscience Conference on Antimicrobial Agents and Chemotherapy (Chicago, Illinois), September 17, 2011
REFERENCES
- 1.Agency for Healthcare Research and Quality. Washington, DC: 2010. [Accessed May 1, 2011]. Introduction to the HCUP nationwide inpatient sample (NIS) http://www.hcup-us.ahrq.gov/db/nation/nis/NIS_2008_INTRODUCTION.pdf. [Google Scholar]
- 2.Noskin GA, Rubin RJ, Schentag JJ, et al. The burden of Staphylococcus aureus infections on hospitals in the United States: an analysis of the 2000 and 2001 Nationwide Inpatient Sample Database. Arch Intern Med. 2005;165(15):1756–1761. doi: 10.1001/archinte.165.15.1756. [DOI] [PubMed] [Google Scholar]
- 3.Cabell CH, Heidenreich PA, Chu VH, et al. Increasing rates of cardiac device infections among Medicare beneficiaries: 1990–1999. Am Heart J. 2004 Apr;147(4):582–586. doi: 10.1016/j.ahj.2003.06.005. [DOI] [PubMed] [Google Scholar]
- 4.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000 Feb 15;19(3):335–351. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 5.Tleyjeh IM, Steckelberg JM, Murad HS, et al. Temporal trends in infective endocarditis: a population-based study in Olmsted County, Minnesota. JAMA. 2005;293(24):3022–3028. doi: 10.1001/jama.293.24.3022. [DOI] [PubMed] [Google Scholar]
- 6.Steckelberg JM, Melton LJ, 3rd, Ilstrup DM, Rouse MS, Wilson WR. Influence of referral bias on the apparent clinical spectrum of infective endocarditis. Am J Med. 1990 Jun;88(6):582–588. doi: 10.1016/0002-9343(90)90521-e. [DOI] [PubMed] [Google Scholar]
- 7.Austin PC, Daly PA, Tu JV. A multicenter study of the coding accuracy of hospital discharge administrative data for patients admitted to cardiac care units in Ontario. American heart journal. 2002 Aug;144(2):290–296. doi: 10.1067/mhj.2002.123839. [DOI] [PubMed] [Google Scholar]
- 8.Schneeweiss S, Robicsek A, Scranton R, Zuckerman D, Solomon DH. Veteran's affairs hospital discharge databases coded serious bacterial infections accurately. J Clin Epidemiol. 2007;60(4):397–409. doi: 10.1016/j.jclinepi.2006.07.011. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.