Abstract
The reconstruction of acquired mandibular defects due to ablative tumor surgery or traumatic injuries is still challenging. The gold standard in such treatment is application of reconstructive titanium plates, which should be contoured and adapted to the defect as much as possible because of their influence on postoperative functional and esthetic results. Traditionally, plate bending is achieved by trial and error intraoperatively. Use of stereolitography (STL) models potentially could reduce the risk of incorrect contouring as well as operating time. On the other hand, fabrication of STL is time-consuming and costly. However, we found only one experimental study dedicating to virtual plate bending in the literature. The aim of this article was to demonstrate clinical application of a method of virtual bending of reconstructive plate for mandibular defect bridging. No significant complications occurred, and satisfactory functional and esthetic results were achieved in all cases. We found this technique precise and applicable in cases of reconstruction of mandibular defects.
Keywords: Mandibular reconstruction, reconstructive titanium plate, virtual bending
Reconstruction of acquired defects and deformities is crucial in modern maxillofacial surgery. Commonly, these defects could be result of benign or malignant tumors, osteomyelitis, trauma, osteoradionecrosis, and so on. They have significant impact on anatomy, function, and esthetics, which can provoke deterioration of overall quality of life of the patient. However, it is challenging because of the complex functional anatomy of the maxillofacial region. The use of titanium reconstructive plates has become a routine method in treatment of acquired mandibular defects. The key point of this procedure is proper anatomic adaptation of the plate to the resected or defective site of the mandible, which has a direct influence on the success of the surgical reconstruction. Commonly, the plate's adaptation is achieved intraoperative by trial and error, which means multiple bends of the plate and use of a bent template.1 This procedure requires more extensive surgical exposure of the mandible and increases operating time.
Today, widely spread computer-assisted treatment planning allows surgeons to proceed quickly with very precise preoperative planning.2 This method is actually based on computed tomography (CT), which produces digital data in DICOM (Digital Imaging and Communication in Medicine [National Electrical Manufacturers Association]) format. Changing of Hounsfield units during computer processing provides the possibility to create 3-D reconstructions of certain anatomic structures, such as bones, muscles, or airways. The 3-D data also could be transferred into some software systems as polygon meshes (Mimics, Simplant CMF [Materialise, Leuven, Belgium], NobelGuide [Nobel Biocare, Göteborg, Sweden] and AMIRA [Visage Imaging Inc., San Diego, CA]), where some corrections, depending on software, can also be done.3,4 Therefore, reconstruction of acquired defects in the maxillofacial region as well as preoperative planning might be done virtually prior to surgery with the same 3-D geometry. Moreover, nowadays Medical Rapid Prototyping (MRP) technology provides surgeons with the possibility to print 3-D virtual models. This kind of preoperative planning decreases the time and morbidity of surgery because of the potential to perform preoperative osteotomies and resection, choose donor sites, prefabricate surgical templates, and virtually bend plates.5,6 However, we found only one experimental study dedicated to virtual bending of reconstructive plates in our literature review.7
The aim of present study was to virtually bend titanium plate in clinical practice and assess its accuracy and efficiency compared with conventional intraoperative plate bending.
MATERIALS AND METHODS
Study Design
Once acquired, CT data in DICOM format was burned onto a CD. An Acer personal computer with a 2.21-MHz Duel-Core Intel processor with 2 GB of random access memory (Acer Computer, Inc., Taipei, China) was used. DICOM data were then transferred to Mimics 10.01 software and 3-D volume-rendered reconstruction was done by appropriate Hounsfield threshold units (in a range of 226 to 3071 Hounsfield units). At the same time, a scanned and remeshed reconstruction plate (2.7-mm thick, 24 holes straight and 2.7-mm thick, 16 × 4 holes angled, Conmet, Moscow, Russia) was imported into Mimics software. After segmentation and repositioning of facial bones into proper position, an appropriate anatomy of the facial skeleton was achieved. By segmentation and independent repositioning of this model, a virtual reconstruction plate was prebent and adapted to the facial skeleton. The virtually prebent plate dimensions, especially distances from inner and outer aspects, were measured with Mimics software. Then, saved screenshots were printed on Canon MF 4018 laser printer (Canon Inc., Tokyo, Japan). The reconstruction plate was bent according to virtual measurements, using a digital caliper (Rohs Norm 2002/95/EC; Zhangjiagang Titan Impt. & Expt. Co., Ltd, China) with the standard bending irons. All prebent plates were sterilized 1 day prior to surgery. Study data were applied in three clinical cases in which mandibular bridging was planned. As confirmation of accuracy of the plate bending, postoperative CT scans with 3-D reconstruction and subsequent comparison of preoperative and postoperative virtual plates were chosen.
Case 1: Recurrent Ameloblastoma
Case 1 was a 57-year-old woman admitted to our hospital with complaints of enormous mass in the left mandible region. Upon anamnesis, the first signs of disease were noted in 2005 when she underwent extraction of teeth 37 and 38. Since then, she had an enlarging tumor in the left mandibular angle, which was excochleated in 2005 and 2008 due to recurrence of the tumor. She was admitted to our hospital in 2010 with signs of recurrent ameloblastoma, and hemimandibular resection was taken into account as a treatment option. During clinical investigation, the tumor mass was found in the region of the left mandibular body and angle (Fig. 1). Orthopantomography (OPG) and CT scans showed the mass spreading into the subtemporal fossa and submandibular regions (Figs. 2 and 3). Using Mimics software virtual simulation, as well as virtual resection and virtual Ti-Recon, the plate was prebent (Figs. 4–7). Data from the virtually prebent plate were transferred into the real plate by 2-D printing, and the real plate was bent (Fig. 8). The plate was sterilized prior to surgery. Surgical approach was achieved via extended submandibular and retromandibular access (Fig. 9). The tumor was resected, and the prebent plate was fixed with four screws on one side and one screw on the condylar side (Figs. 10 and 11). No bone transfer was used, as instructed by the patient. Postoperative CT scan and clinical appearance showed excellent plate and condyle positioning in the glenoid fossa (Figs. 12–15).
Figure 1.
Preoperative clinical picture of the patient (case 1), showing the mass in the left hemimandible.
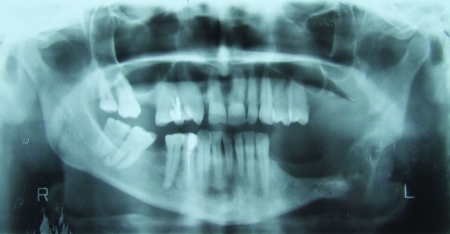
Figure 2.
Panoramic view, showing multilacunar radiolucent tumor (case 1).
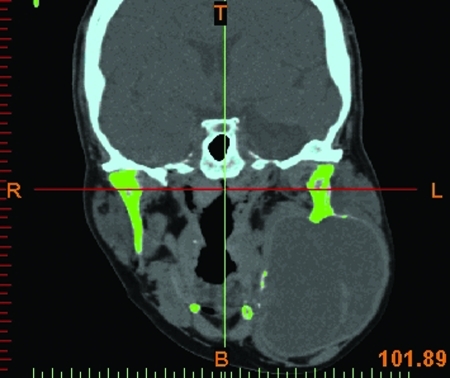
Figure 3.
Computed tomography scans of coronal section for virtual resection planning (case 1).
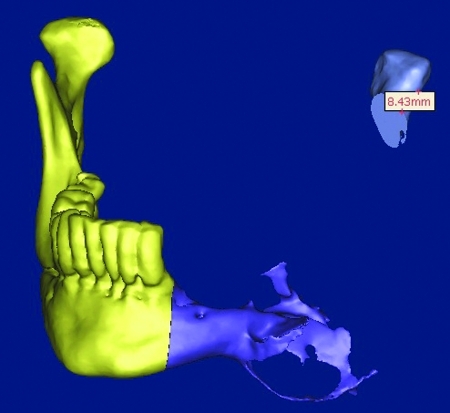
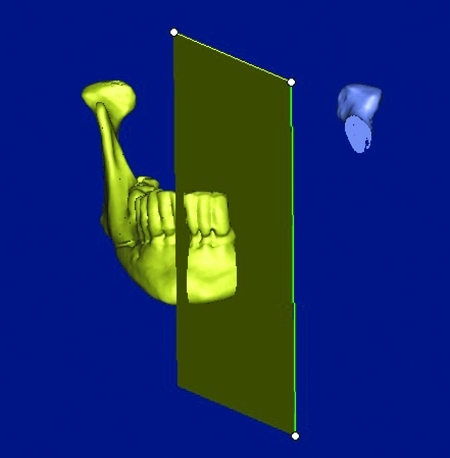
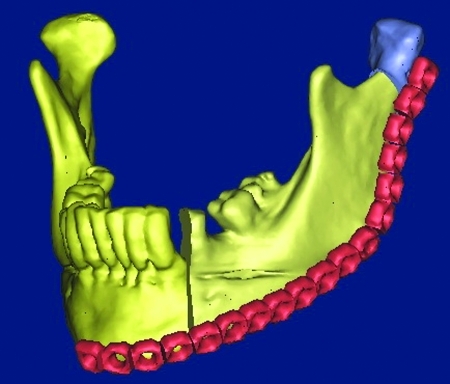
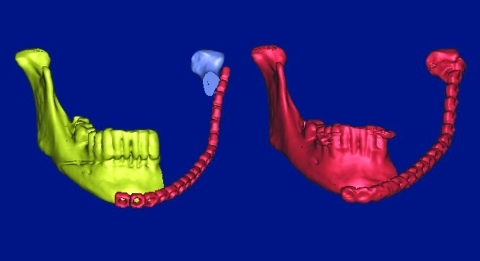
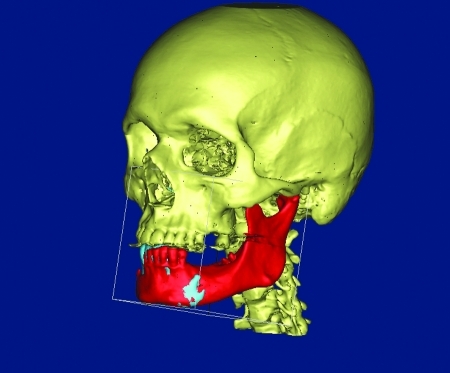
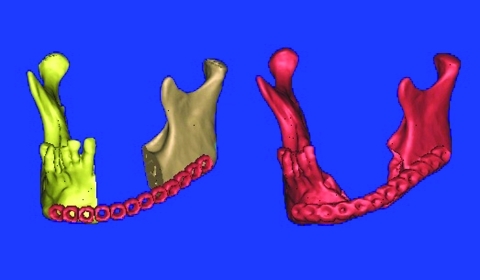
Figure 4.
Virtual resection and segmentation (case 1).
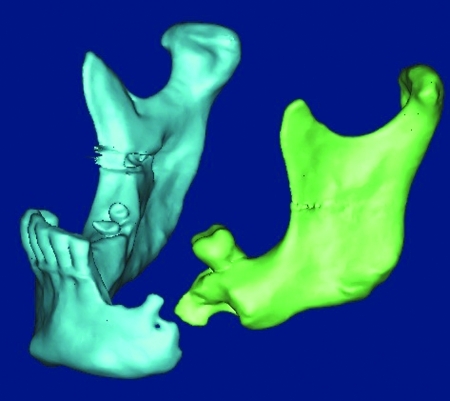
Figure 5.
Mirroring of normal side to defect region (case 1).
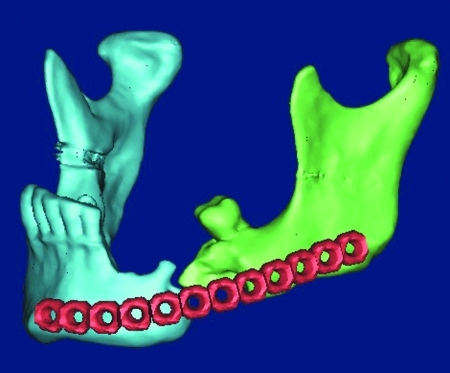
Figure 6.
Adaptation of virtual reconstructive plate to mirrored segment (case 1).
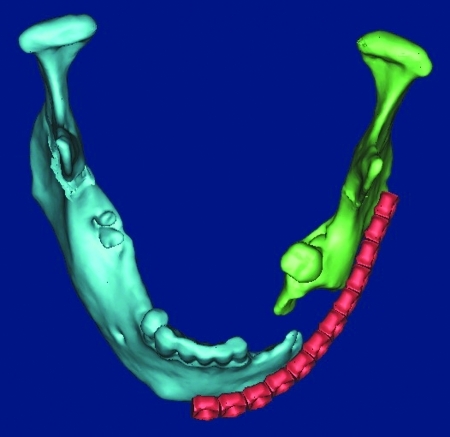
Figure 7.
Final plate adaptation (case 1).
Figure 8.
Prebent reconstructive plate (case 1).
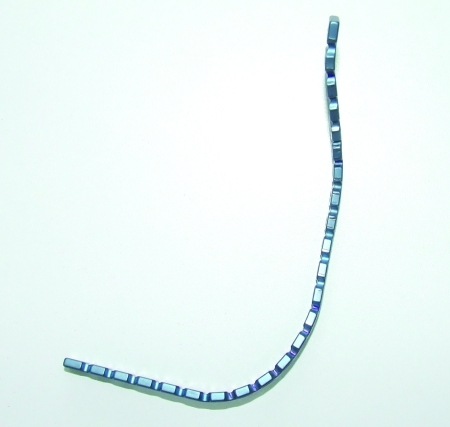
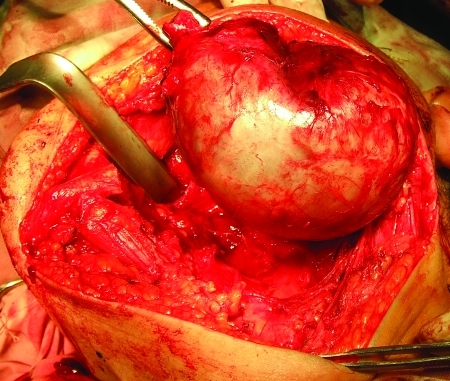
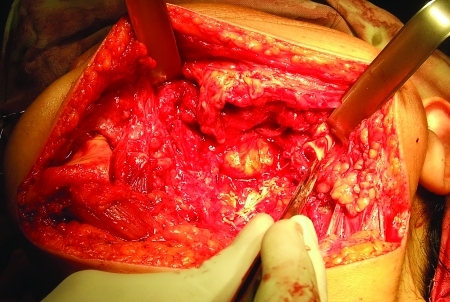
Figure 9.
Tumor resection (case 1).
Figure 10.
Resected site showing right hemimandible and preserved left condyle (case 1).
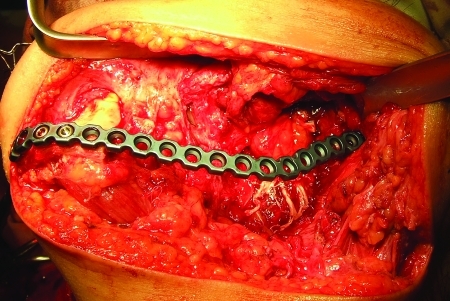
Figure 11.
Reconstruction plate adapted to remaining fragments (case 1).
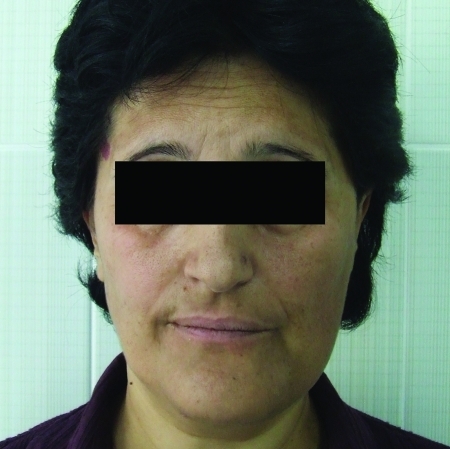
Figure 12.
Postoperative clinical picture of the patient, representing good facial symmetry (case 1).
Figure 13.
Postoperative computed tomography scan, showing adequate plate adaptation (case 1).
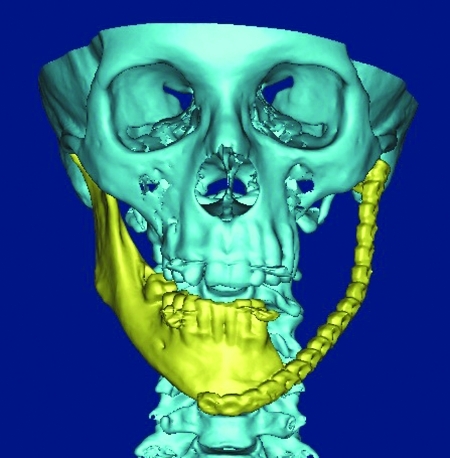
Figure 14.
Comparative 3-D pictures of virtually prebent and postoperative reconstruction plate (case 1).
Figure 15.
Comparative 3-D pictures of virtually prebent and postoperative reconstruction plate (case 1).
Case 2: Chronic Osteomyelitis
Case 2 was a 48-year-old man admitted to our hospital with complaints of pathological mobility in the left mandibular region. Upon anamnesis, he had trauma accident in 1992, which was treated surgically by internal wire fixation. Six months later, the intrafragmentary gap was infected and the patient underwent “wire extraction” under general anesthesia. Despite nonunion, the patient felt good up to 2010, when he experienced mandibular irregularity and pain in the left submandibular region. During clinical investigation, an infected bonny defect was found in the region of the left mandibular body. Lateralization of the occlusion was also noted during clinical investigation (Fig. 16). This defect has been confirmed by CT scan (Fig. 17). Virtual simulation, including virtual reposition and virtual Ti-Recon plate prebending, was done (Figs. 18–22). Subsequently, data from the virtually prebent plate were transferred to the real plate, which was sterilized before surgery (Fig. 23). Surgical approach was achieved via extended submandibular access. The nonunion side was exposed and the prebent plate fixed by three screws on each side (Fig. 24). Postoperative CT scan and clinical appearance showed excellent plate positioning and occlusion (Figs. 25–27).
Figure 16.
Preoperative clinical picture of the patient's occlusion, showing lateralization of occlusion to the left side (case 2).
Figure 17.
Virtual 3-D reconstructive imaging of defect region; convergence of fragments is notable (case 2).
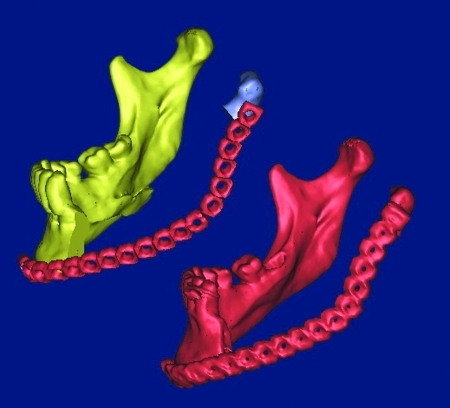
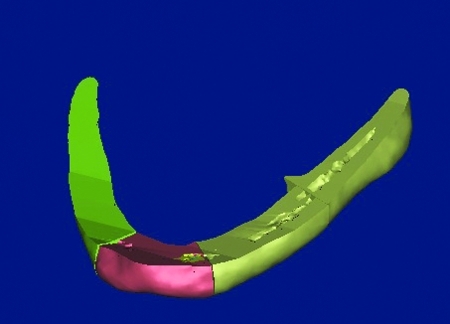
Figure 18.
Mirroring of normal side to defect region (case 2).
Figure 19.
Adaptation of mirrored fragment in glenoid fossa and distal fragment to mirrored fragment (case 2).
Figure 20.
New position of distal fragment; increasing intrafragment distance is notable (case 2).
Figure 21.
Adaptation of virtual reconstructive plate (case 2).
Figure 22.
Adaptation of virtual reconstructive plate (case 2).
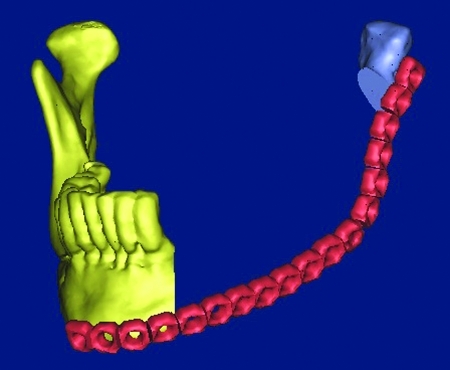
Figure 23.
Prebent reconstructive plate (case 2).
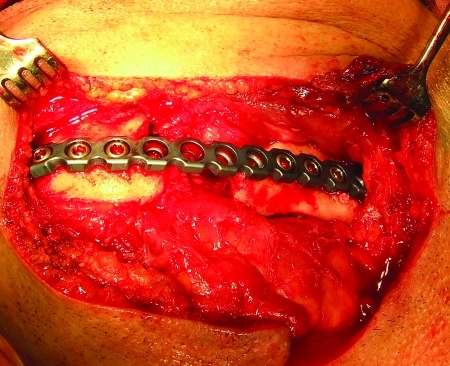
Figure 24.
Intraoperative adaptation of the plate (case 2).
Figure 25.
Postoperative occlusion; centralization of the intradental line (case 2).
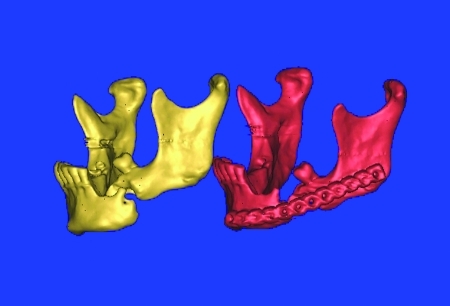
Figure 26.
Comparative 3-D pictures of virtually prebent and postoperative reconstruction plate (case 2).
Figure 27.
Comparative 3-D pictures of virtually prebent and postoperative reconstruction plate (case 2).
Case 3: Cementoma of the Left Side of the Mandible
Case 3 was a 58-year-old woman admitted to our hospital with complaints of mass in the left mandibular region. Anamnesis revealed the first signs of the disease in 2005 when she underwent extraction of tooth 34. During clinical investigation, boney tissue mass was found in the region of the left mandibular body. Orthopantomography (OPT) and CT scan showed spreading of the mass into the submandibular region (Figs. 28–30). By Mimics software virtual simulation, virtual resection and virtual Ti- Recon plate prebending was performed (Figs. 31–36); within the same software, data from the virtually prebent plate were transferred to the real plate, which was sterilized prior surgery (Fig. 37). Surgical approach was achieved via intraoral access. The tumor was resected and the prebent plate fixed by three screws on each side (Fig. 38). Postoperative CT scan and clinical appearance showed excellent plate positioning and facial couture (Figs. 39 and 40).
Figure 28.
Preoperative orthopantomography (OPT), showing spreading of the tumor along horizontal ramus (case 3).
Figure 29.
3-D virtual reconstruction; tumor expansion out to lingual and vestibular cortex (case 3).
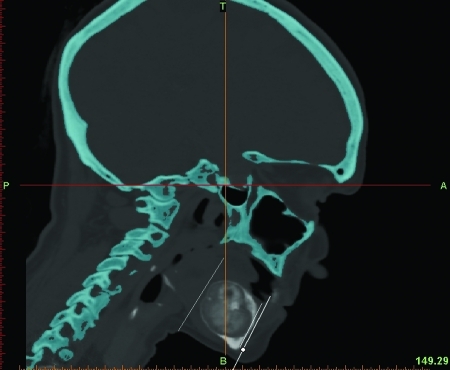
Figure 30.
Sagittal section for determining resection area (case 3).
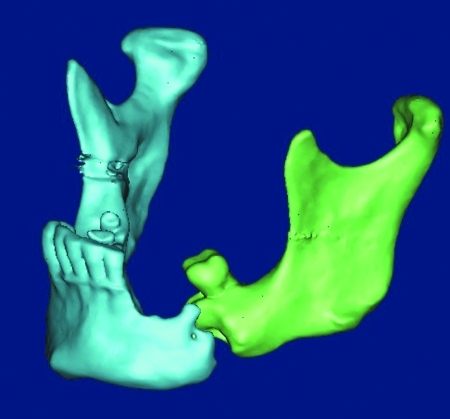
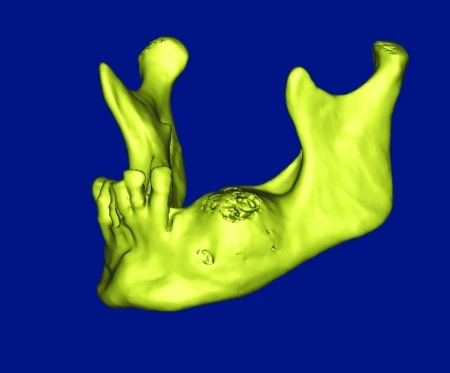
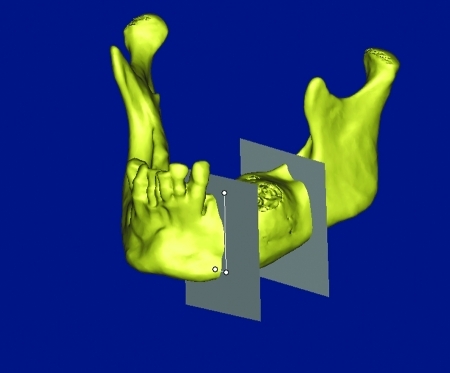
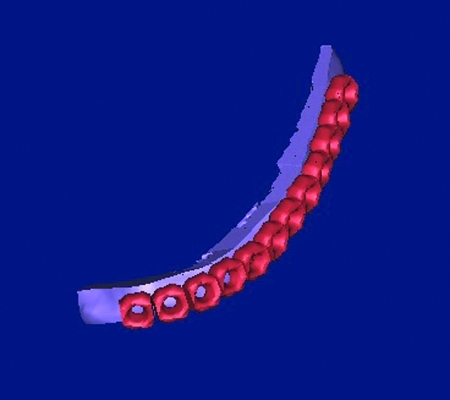
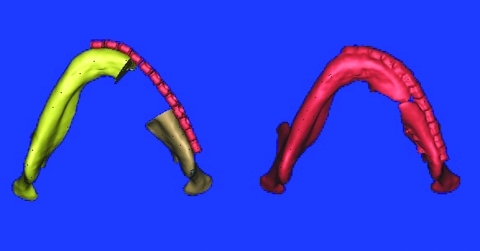
Figure 31.
Virtual resection (case 3).
Figure 32.
Virtual segmentation (case 3).
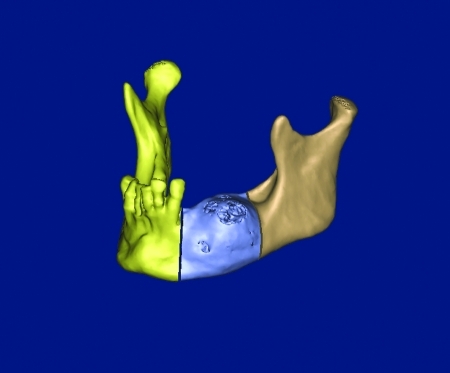
Figure 33.
Segmentation after mirroring of the normal site to defected one (case 3).
Figure 34.
Achievement of mandibular couture (case 3).
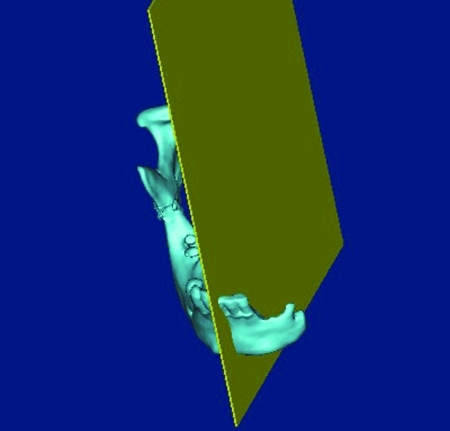
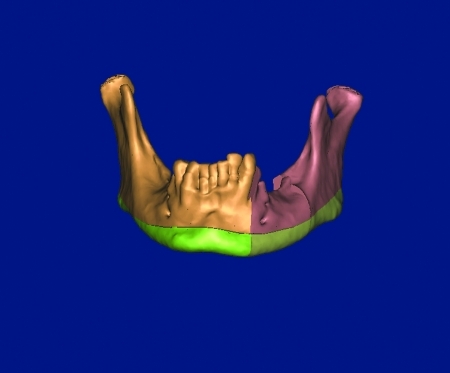
Figure 35.
Adaptation of virtual reconstructive plate to mirrored mandible (case 3).
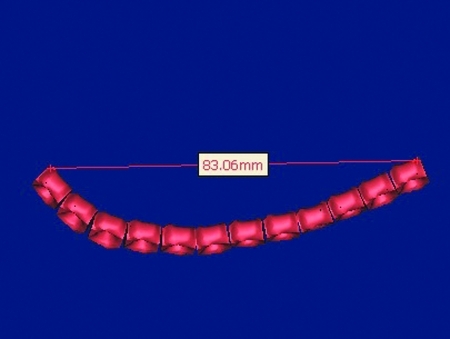
Figure 36.
Virtual measurements (case 3).
Figure 37.
Measurements of prebent reconstructive plate by caliper (case 3).
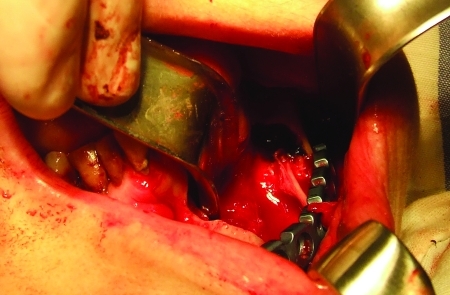
Figure 38.
Intraoperative positioning of prebent reconstructive plate via transoral approach (case 3).
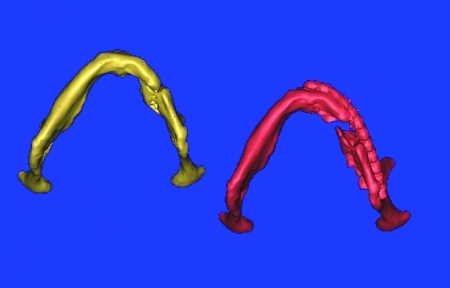
Figure 39.
Comparative 3-D pictures of virtually prebent and postoperative reconstruction plate (case 3).
Figure 40.
Comparative 3-D pictures of virtually prebent and postoperative reconstruction plate (case 3).
RESULTS
All prebent reconstructive plates were placed without difficulty and required minimal operative time for adaptation and fixation. However, MMF was used in each case for fragment stabilization during plate fixation. All cases demonstrated good postoperative occlusion, function, symmetry, and esthetics. Postoperative CT scan proved the plates were prebent appropriately. The mean surgical time estimated from 3 to 5 hours, and time for adaptation and fixation of the plate was significantly reduced and accounted for ~30 to 45 minutes. Notably, in all cases a distal fragment was free from occlusion, and its positioning was achieved only by the curvature of the plate. It is also important that in all cases the mandible could not be used as a template for intraoperative plate bending; in one case, this was impossible because of mandibular defect and fragment convergence, and in two cases, extensive growth of the tumor made it useless.
DISCUSSION
Within this clinical study, it was shown that reconstructive titanium plates (Conmet, RF, Moscow) could be prebent virtually prior to surgery with a reasonable degree of accuracy. This technique raises the possibility to significantly reduce surgical time and improve postoperative functional and esthetic result compared with conventional methods. However, prebent plates always could be corrected during surgery if some bending errors were found. Nevertheless, there were no incidences of incorrect contouring. Moreover, it is important to note that the virtual planning allows one to determine appropriate length of the plates and screws in advance, along with the direction and regions they could be used more effectively. It is also possible that virtually prebent and sterilized plates could be utilized as a surgical template for the bone graft shaping.
On the other hand, MRP technology and the use of stereolithographic models also could be used for preoperative plate bending.8 This technology was described first by Mankovich et al in 1990,9 and it is the method of choice in preoperative planning of reconstructive cases. It is very helpful when complex defects and deformities are to be reconstructed. Surgical templates could be prepared for intraoperative plate bending and bone graft shaping by using this method. In fact, stereolitography (STL) models could be sterilized and used as templates.10 On the other hand, the costs for MRP manufacturing in our country is ~200 to 300 € and it takes some time for fabrication of these models. Therefore, it is difficult to use this method in routine practice. In contrast, virtual plate bending requires only 2 to 3 hours for finalizing the plate before sterilization.
CONCLUSION
We found this technique precise and applicable in cases of mandibular bridging. This method raises the possibility of significantly reducing operational time with reduced risk of incorrect plate adaptation. Because of its simplicity and time saved, it can be successfully used in routine mandibular reconstruction procedures.
References
- Salgueiro M I, Stevens M R. Experience with the use of prebent plates for the reconstruction of mandibular defects. J Craniomaxillofac Trauma. 2010;3:201–208. doi: 10.1055/s-0030-1268520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen A, Laviv A, Berman P, Nashef R, Abu-Tair J. Mandibular reconstruction using stereolithographic 3-dimensional printing modeling technology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:661–666. doi: 10.1016/j.tripleo.2009.05.023. [DOI] [PubMed] [Google Scholar]
- Orentlicher G, Goldsmith D, Horowitz A. Applications of 3-dimensional virtual computerized tomography technology in oral and maxillofacial surgery: current therapy. J Oral Maxillofac Surg. 2010;68:1933–1959. doi: 10.1016/j.joms.2010.03.013. [DOI] [PubMed] [Google Scholar]
- Bell R B. Computer planning and intraoperative navigation in orthognathic surgery. J Oral Maxillofac Surg. 2011;69:592–605. doi: 10.1016/j.joms.2009.06.030. [DOI] [PubMed] [Google Scholar]
- Cunningham L L, Jr, Madsen M J, Peterson G. Stereolithographic modeling technology applied to tumor resection. J Oral Maxillofac Surg. 2005;63:873–878. doi: 10.1016/j.joms.2005.02.027. [DOI] [PubMed] [Google Scholar]
- Zhou L, He L, Shang H, Liu G, Zhao J, Liu Y. Correction of hemifacial microsomia with the help of mirror imaging and a rapid prototyping technique: case report. Br J Oral Maxillofac Surg. 2009;47:486–488. doi: 10.1016/j.bjoms.2009.05.001. [DOI] [PubMed] [Google Scholar]
- Dérand P, Hirsch J-M. Virtual bending of mandibular reconstruction plates using a computer-aided design. J Oral Maxillofac Surg. 2009;67:1640–1643. doi: 10.1016/j.joms.2009.03.039. [DOI] [PubMed] [Google Scholar]
- Fariña R, Plaza C, Martinovic G. New transference technique of position of mandibular reconstructing plates using stereolithographic models. J Oral Maxillofac Surg. 2009;67:2544–2548. doi: 10.1016/j.joms.2009.04.086. [DOI] [PubMed] [Google Scholar]
- Mankovich N J, Cheeseman A M, Stoker N G. The display of three-dimensional anatomy with stereolithographic models. J Digit Imaging. 1990;3:200–203. doi: 10.1007/BF03167610. [DOI] [PubMed] [Google Scholar]
- Sannomiya E K, Silva J VL, Brito A A, Saez D M, Angelieri F, Dalben GdaS. Surgical planning for resection of an ameloblastoma and reconstruction of the mandible using a selective laser sintering 3D biomodel. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:e36–e40. doi: 10.1016/j.tripleo.2008.01.014. [DOI] [PubMed] [Google Scholar]