Abstract
Cancer screening rates are lower among Asian Americans than the general USA population. While prior studies examined characteristics of Asian American patients as predictors of cancer screening, few investigated their health care providers. Asian American primary care physicians practicing in New York City were surveyed by questionnaire regarding their demographics, practice characteristics, and cancer screening of their Asian American patients. Of the 117 eligible respondents, 96% recommended mammograms to their Asian patients 50+ years of age and 70% to patients 40–49-year-old. Only 30% of respondents use both age and onset of sexual activity to determine when to recommend Pap smears. For colorectal cancer screening, the rates of performing fecal occult blood testing or recommending colonoscopy or sigmoidoscopy were 77% and 74%. About 70% recommend screening for hepatitis B. Gender and ethnicity of the physician were found to be significant predictors for cancer screening practice.
Keywords: Asian, Asian American, Cancer, Prevention, Screening, Physician
Introduction
Cancer is the second leading cause of death for Americans as a whole, but is the leading cause of death among Asian Americans. The mortality from several forms of cancers can be substantially reduced by interval screenings that allow for detection at an early stage of disease progression. Although the all-cancer mortality rate for Asian Americans (125/100,000) is not higher than other American ethnicities, there is substantial evidence that cancer screening is particularly deficient among Asian Americans and that greater gains from health promotion may be achieved in these communities [1].
The 2000 National Health Interview Survey (NHIS) revealed that Asian Americans have the lowest rates of Pap smear (68%) and endoscopy (i.e. sigmoidoscopy or colonscopy) (19%) compared to all other ethnic groups. Similarly, Asian Americans reported the second lowest rates of mammography (57%) [2]. Other surveys that focused on specific Asian American communities have reveal even lower screening rates, especially among South Asians, that are otherwise masked by the aggregation of ethnic subgroups [3–6].
Within New York City, the area of our study and a city well known for its ethnic diversity and sizeable immigrant population, recent health department surveys still indicate that only 70% of Asian American women have received a Pap smear in the last 3 years, compared to 80–85% for African Americans, Hispanics, and Caucasians. Asian American women in New York also have the lowest rate of mammography (75%) of all ethnicities, and only 51% of Asian American men and women over age 50 have ever received endoscopy for colon cancer screening [7].
The screening rates in Asian American communities carry substantial public health importance. Although census data indicate that American Asians and Pacific Islanders (AAPIs) constitute approximately 5% of the total USA population, far higher proportions of the population in our largest cities are AAPI, including San Francisco (33%), Los Angeles (11%) and New York (12%) [8]. Furthermore, a full third of the average 1.3 million new USA immigrants each year are from Asian countries [9]. Despite these numbers, availability of data on health indicators and behaviors for the various Asian American populations still lags substantially behind other American ethnic groups.
To better understand the barriers that Asian Americans must overcome to receive adequate cancer screening, we conducted a survey of Asian American physicians practicing within New York City. This approach differs from most published research in which the focus is on the recipients of cancer screening rather than the providers. However, in the National Health Interview Survey, the top reason cited for not obtaining cancer screening was the lack of a physician’s recommendation [10]. We focus on Asian American physicians, who in addition to serving larger proportions of Asian American patients, are likely to be influenced by many of the same cultural determinants that produce lower screening rates. This paper presents our results from a survey of cancer screening practices and attitudes of Asian American physicians in the New York City metropolitan area.
Methods
Study Sample
The surveyed population consisted of Asian American primary care physicians (i.e. Internal Medicine, Family Practice, Obstetrics-Gynecology, and Pediatrics) who practice in New York City. A two-pronged sampling method was utilized to recruit physicians during the time period of Fall 2002 to Spring 2004. First, the larger subject pool was extracted from the New York State Medical Licensing Board list of certified physicians. Selection of Asian physicians was based on the most common Chinese, Korean and South Asian surnames. The sensitivity and specificity of using surnames to identify Asian ethnicities in the USA has been reported previously [11]. To this contact list were added names from membership files for the Chinese American Medical Society of New York (CAMS) and the Bangladeshi Medical Association of North America, as well as from the attendance record of the CAMS Annual Conference. Physicians from this list were mailed a brief, anonymous survey, with telephone follow-up one month later. The second prong of sampling occurred by distribution of the survey in person to physicians at three conferences for South Asian American physicians held in New York City.
Survey Instrument
The study instrument was modeled from the survey used by Lee et al. [12], and included 32 questions on the physicians’ demographics, patient population and cancer screening practices and recommendations. Physicians were also asked to rank their agreement or disagreement with opinion statements regarding cancer screening on a five-point Likert scale. In addition to the Likert scale items on attitudes and beliefs about screening, physicians were asked to complete a table to identify reasons for not obtaining individual screening tests.
Data Analysis
Written survey responses were tabulated in a Microsoft Access database. Confidence intervals for single proportion estimates, univariate associations (χ2 test) and logistic regression were performed with SAS 9.1 for Windows (SAS Institute Inc., Cary, NC). In regression models, the predictor variables included physician gender, physician ethnicity, proportions of patients of Asian heritage, and proportion of patients lacking health insurance. Outcome variables were selected cancer screening practices. For greater statistical power physician ethnicity was grouped as either South Asian or East Asian. Other variables tested for association or effect modification in regression models included practice specialty, age, and practice setting (i.e. private, group, hospital-based, academic). Comparisons were made between reported clinical practice and guidelines for screening published by the American Cancer Society (ACS). Other commonly used guidelines from the National Cancer Institute (NCI), the American Gastroenterological Association, the American Academy of Family Physicians (AAFP), and the USA Preventive Service Task Force (USPSTF) were also referenced [13–17].
Results
A total of 1,374 physicians were invited to participate. From the respondents, (17% response rate), 117 were found to be eligible subjects, after exclusion of physicians who are non-Asian ethnicities, practice outside the study region, or practice non-applicable medical specialties (e.g. dermatology, psychiatry).
Physician Demographics and Practice Characteristics
The demographics and practice characteristics of the eligible respondents (N = 117) are shown in Table 1. The physician sample was 53% male and had a mean age of 45 years. Twenty percent were born in the United States and under half (43%) were graduates of USA medical schools. The average time since medical school graduation was 20 years. The three most frequent ethnicities were Chinese (47%), Indian (26%) and Korean (11%).
Table 1.
Characteristics of respondents: Asian physicians in New York city
| Total respondents |
n 117 |
% 100 |
|---|---|---|
| Demographic | ||
| Male (N = 116) | 61 | 53 |
| USA Born (N = 114) | 23 | 20 |
| Mean Age: 45 years | ||
| Ethnicity | ||
| Chinese | 55 | 47 |
| Indian | 30 | 26 |
| Korean | 13 | 11 |
| Bangladeshi | 10 | 9 |
| Pakistani | 9 | 8 |
| Medical education | ||
| Graduate of USA Medical School (N = 116) | 50 | 43 |
| Languages other than English spoken with patients | ||
| Chinese | 51 | 44 |
| Hindi | 17 | 15 |
| Gujarati | 17 | 15 |
| Bengali | 10 | 9 |
| Korean | 10 | 9 |
| Characteristics of patient population served | ||
| Greater than 30% Asian patients (N = 117) | 44 | 38 |
| Greater than 30% uninsured patients (N = 112) | 34 | 30 |
| Most patients understand preventive medicine (N = 113) | 50 | 44 |
| Most patients follow lifestyle recommendations (N = 110) | 25 | 23 |
| General cancer screening recommendations | ||
| Recommend smoking cessation to patients (N = 106) | 106 | 100 |
| Recommend healthy diets and exercise to patients (N = 109) | 109 | 100 |
| Offer patient education materials on cancer prevention (N = 99) | 69 | 70 |
More than a third (38%) of the physicians reported that a substantial fraction (>30%) of their patient population is Asian, and 23% serve mostly (>75%) Asian patients. Thirty percent of the physicians reported that many (>30%) of their Asian patients lack health insurance. Most (90%) of these Asian physicians communicate with their Asian patients in at least one language other than English.
Breast and Cervical Cancer Screening
Breast and cervical cancer screening practices of the surveyed physicians are shown in Table 2. The large majority of the physicians self-reported both teaching breast self-examinations (94%) and performing clinical breast exams (87%) for their Asian patients. The proportion of Asian physicians who reported ordering mammograms for their patients was 96%. The proportion was larger for East Asian physicians compared to South Asians (100% vs. 90%, P = 0.03). While almost all physicians reported ordering mammograms for their Asian patients, smaller proportions recommend mammograms start at age 40 years (70%) and be performed annually (68%).
Table 2.
Breast and cervical cancer screening practices among Asian physicians
| n | % | 95% Conf. interval | |
|---|---|---|---|
| Teach patients to do self breast exam (N = 100) | 94 | 94 | 86.9–97.5 |
| Perform clinical breast exams (N = 94) | 82 | 87 | 78.4–92.9 |
| Order mammograms for patients (N = 92) | 88 | 96 | 88.6–98.6 |
| Chinese (N = 44) and Korean (N = 9) | 53 | 100 | |
| Indian (N = 24), Pakistani (N = 8), and Bangladeshi (N = 7) | 35 | 90 | |
| Recommended interval for screening mammograms (N = 86) | |||
| Annual | 58 | 68 | 56.4–76.9 |
| Every two years | 24 | 28 | 19.0–38.8 |
| Recommended age to start screening mammograms (N = 89) | |||
| Age 35 years or older | 13 | 15 | 8.3–24.1 |
| Age 40 years or older | 60 | 70 | 56.6–76.8 |
| Age 50 years or older | 14 | 16 | 9.2–25.3 |
| Criteria used to determine when to begin Pap smears (N = 98) | |||
| When patient is 18 years or older | 54 | 54 | 44.8–65.1 |
| When patient is sexually active | 73 | 73 | 64.5–82.5 |
| Use both of above starting criteria | 29 | 29 | 21.0–39.8 |
Colorectal and Liver Cancer Screening
Colorectal and liver cancer screening practices are shown in Table 3. Fecal occult blood testing (FOBT) and colonoscopy were the most common screening modalities used (77% and 62%, respectively). Regarding hepatitis B infection, an important risk factor for hepatocellular carcinoma, a large majority (93%) of physicians recommend vaccination for their Asian patients. Approximately two-thirds of physicians screen their Asian patients for HBV surface antibody (immunity) and surface antigen (chronic carrier state). Fewer (44%) report screening for prior exposure with the anti-hepatitis B core antibody.
Table 3.
Colorectal and hepatic cancer screening among Asian physicians
| n | % | 95% Conf. interval | |
|---|---|---|---|
| Physician using selected colorectal cancer screening tests | |||
| Fecal occult blood test (FOBT) | 70 | 77 | 66.9–85.1 |
| Digital rectal exam | 56 | 62 | 50.8–71.6 |
| Either endoscopic study | 67 | 74 | 63.4–82.3 |
| Colonoscopy | 56 | 62 | 50.8–71.6 |
| Sigmoidoscopy | 23 | 25 | 16.8–35.5 |
| Barium enema | 3 | 3 | 0.7–9.3 |
| Interval for performing screening FOBT | |||
| Annual | 66 | 94 | 85.3–98.2 |
| Every 2–3 years | 4 | 6 | 1.8–14.7 |
| Interval for ordering screening colonoscopy | |||
| Annual or Every 2–3 years | 8 | 12 | 5.7–22.7 |
| Every 5 years | 34 | 51 | 38.4–63.1 |
| Every 10 years | 25 | 37 | 26.1–50.0 |
| Recommend HBV vaccine for patients | 94 | 93 | 85.8–96.9 |
| Proportion utilizing HBV screening tests | |||
| HBV surface antibody (HBsAb) | 55 | 70 | 58.1–79.2 |
| HBV surface antigen (HBsAg) | 64 | 70 | 59.7–79.2 |
| HBV core antibody (HBcAb) | 35 | 44 | 33.3–55.9 |
Physician Attitudes and Beliefs
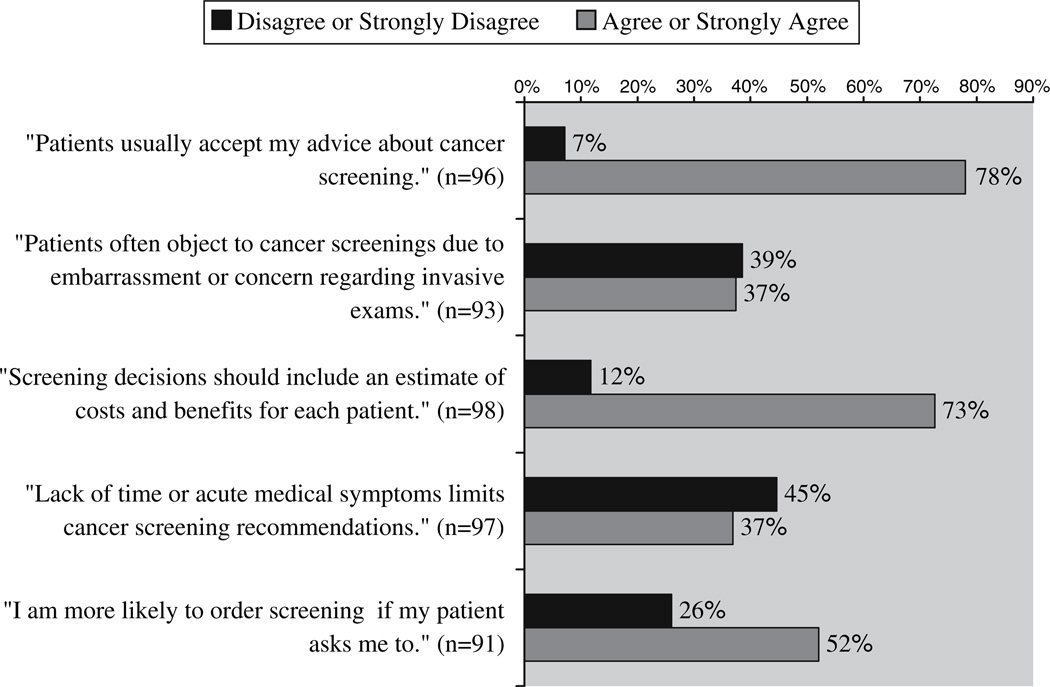
Physicians’ beliefs about cancer screening and prevention are shown in Fig. 1. The majority of physicians (78%) expressed belief that their Asian patients do follow their advice regarding cancer screening. Time constraints and patient embarrassment were identified as important obstacles, reported by roughly a third of the physicians. Most responding clinicians also considered an assessment of cost as important in the decision to screen or recommend screening. While half the physicians surveyed indicated that they are more likely to order a screening test if the patient requests it, they simultaneously indicated low expectations for their Asian patients to understand preventive medicine.
Fig. 1.
Asian American Physicians’ beliefs and attitudes regarding cancer screening
Determinants of Screening
The results from logistic regression analysis of the role of physician characteristics in predicting screening practices are shown in Table 4. Physicians who identified their ethnicity as East Asian were significantly more likely to screen for chronic hepatitis B (OR = 5.2; 95% confidence interval = 1.3–20) and use both age and sexual history criteria for starting Pap smears (OR = 6.4; 1.7–24), when compared to their South Asian counterparts. Male physicians were significantly less likely to perform clinical breast exams (OR = 0.07; 0.01–0.59) or recommend starting mammography at ages younger than 50 years (OR = 0.21; 0.05–0.90). Male physicians were also less likely to use both Pap smear initiation criteria in their recommendations than female physicians (OR = 0.31; 0.11–0.87). Physicians of both genders recommended chronic hepatitis B screening (HBsAg) with equal frequency.
Table 4.
Predictors in multivariate regression model for selected cancer screening practices
| Start mammograms at 35 or 40 y/o. Odds ratio (P-value) |
Use both Pap Smear Criteria |
Perform clinical breast exams |
Screen patients for HBsAg |
|
|---|---|---|---|---|
| Physician is male | 0.22 (0.04) | 0.31 (0.03) | 0.07 (0.01) | 1.43 (0.52) |
| Physician is East Asian (vs. South Asian) | 0.33 (0.19) | 6.36 (<0.01) | 1.38 (0.73) | 5.17 (0.02) |
| Patient population served is greater than 30% Asian | 3.60 (0.11) | 0.16 (<0.01) | 9.26 (0.08) | 3.07 (0.09) |
| Patient population served is greater than 30% uninsured | 0.23 (0.04) | 0.92 (0.90) | 0.27 (0.11) | 4.00 (0.04) |
Characteristics of the patient population served were also significant predictors in the regression model. Physicians with a larger proportion (>30%) of uninsured patients were less likely to recommend mammography for patients under 50-year-old (OR = 0.23; 0.05–0.94), but were more likely to recommend hepatitis B screening (OR = 4.0; 1.1–15), compared to physicians with fewer uninsured patients. Asian physicians who serve more Asian patients (>30%) were significantly less likely to use both criteria for starting Pap smears (OR = 0.16; 0.05–0.54) than physicians with fewer Asian patients.
Age of the physician, the physician’s practice setting, and the physician specialty were not significantly associated with screening practices in multivariate analysis. Most respondents did not complete the section regarding specific barriers to screening, therefore this section was removed from analysis. Individual responses included concern for patient discomfort, lack of a reminder system, and concerns regarding reimbursement.
Discussion
Minority communities in the United States have lower cancer screening rates than the majority Caucasian population. This disparity has been attributed to many causative factors, including low socioeconomic status and lack of health care access of the minority patient populations, as well as cultural barriers [4, 5, 18–20]. The variable of ethnicity, in particular, has the potential to act on both the recipient and the provider of preventive medicine. Yet, we found only one published study that has specifically examined the cancer screening practices of physicians belonging to a particular ethnic community [12]. Our survey expands upon the findings from this study of Chinese physicians in San Francisco by examining the practices of Asian physicians providing care in the New York City region.
Breast and Cervical Cancer Screening
The high proportion of physicians recommending mammography for their patients was consistent with results from the San Francisco study by Lee et al. However, among our participating physicians, there was less consistent conformance with ACS guidelines for the starting age and interval between mammograms. Differences of the starting age used by physicians may reflect underlying uncertainty in data supporting mammography in women age 40–49 years [14]. A recent Cochrane Review has also called into question the data supporting mammography at any age [21]. However, most major guidelines do currently recommend offering mammograms, including the 40–49-year-old age range, and this is generally considered the current standard of care [13–16, 22]. Practice guidelines also suggest that for women with a strong family history of breast cancer, earlier initiation of mammography should be recommended. Therefore, the physician respondents who reported starting mammography at 35 years of age may be accommodating these special cases, or may be obtaining a baseline image as recommended in older American Cancer Society literature. For the interval between mammograms, there is greater agreement in the published guidelines that the test should be performed annually—despite the failure of some insurance companies and federally funded programs to cover annual imaging. However, we found a large number of surveyed physicians recommend less frequent time intervals between screenings.
Similarly, a lack of uniformity in screening practice was observed in the starting criteria used for Pap smears. Some disagreement may have occurred with this question as our survey used “18 years or older” for the age criteria for starting Pap smears, while some (ACS, USPTF) guidelines have more recently switched to an initiation age of 21 years [15, 16]. Male physicians in this study were also less likely to follow cervical cancer screening guidelines, consistent the physician gender bias seen in published research from the general population [23, 24].
Colorectal and Liver Cancer Screening
For colorectal cancer screening, the rate of physician respondents performing fecal occult blood testing (FOBT) was lower than the rate (84%) seen in Lee et al. The proportion of physicians recommending any form of screening endoscopy was also lower than desired and there was wide variability in the screening intervals used. The ACS recommends that FOBT be performed annually, sigmoidoscopy every 5 years, and colonoscopy every 10 years [15]. Occult blood testing, like Pap smears, is likely to be especially sensitive to cultural barriers given the relatively invasive nature of the physical exam. Both require the ability of the physician to effectively communicate the utility and importance of an uncomfortable screening exam.
For the prevention of liver cancer caused by hepatitis virus, established guidelines do not address specific American ethnicities. For example, the USPTF does not recommend hepatitis screening of asymptomatic individuals (level D recommendation) due to the low prevalence in the total US population (0.3%) [16]. However, the prevalence of hepatitis B virus infection is 10 times higher in American-born Asian individuals, and reaches 10% in those who are foreign-born [25]. The liver is the third most common cancer site for Asian Americans, and the mortality rate for hepatic cancer in Asian Americans is more than double that for Caucasians [2, 25–27]. Hepatitis screening in Asian Americans could be substantially improved by ethnic-specific recommendations in screening guidelines. Unfortunately, the current national guidelines, which do not address the specific needs of minority communities, may instead reduce beneficial testing with false assurances of low risk. Clarifying the indications for hepatitis screening for Asian Americans is especially important given the recently improved treatment options for patients with chronic infection.
Determinants of Screening
A lack of health insurance was previously shown to predict low screening rates in surveys of Asian Americans [19]. Individuals without health insurance are postulated to have less access to health care providers and insufficient means to pay for the costly screening tests such as mammography. However, our findings suggest another reason may be differences in the practice of physicians who serve the uninsured community. We found that Asian American physicians serving more uninsured patients were less likely to recommend mammograms and perform clinical breast exams. These physicians may believe that tests such as mammograms will not be affordable to the uninsured patient. Substantial numbers of physicians in our study self-reported that cost considerations (73%) affect their cancer screening behaviors. Time constraint was also identified as an obstacle to recommending cancer screening by a sizeable fraction of respondents (37%). However, it is not known how the workloads of physicians serving large numbers of uninsured patients compared to other physicians.
English language ability has been shown to correlate with screening rates in studies of screening recipients. Given that 4.2 million Americans who speak an Asian language report that they do not speak English well, the language barrier is of substantial concern [8]. The large number of respondents who speak with patients in languages other than English are potentially able to overcome this barrier to cancer screening. Unfortunately, cancer screening often requires phlebotomy or radiography at a separate facility where the patient’s language may not be spoken. When available in the appropriate language, printed cancer education materials (which are readily available on the Internet) offer an effective and low-cost method for improving communication about cancer screening [28, 29]. The importance of disseminating cancer screening information is underscored by our study’s finding that 52% of the surveyed physicians reported that they are more likely to order cancer screening tests if the patient requests them.
Ethnicity, of both the patient and the physician, was significantly associated with screening rates in our study, although the details of the cultural interactions between the physicians and their patients are beyond the scope of this study. Such interactions have been investigated by others [20]. The physicians with more Asian American patients reported better practices for breast cancer screening but less desirable rates of cervical cancer screening. Possibly, there is greater attention to breast cancer due to awareness among Asian physicians that risk of breast cancer in Asian women rises significantly after immigration to America from Asia [30].
Limitations of our study include use of a convenience sample to maximize sample size given the expected low response rate. Our response rate was typical for surveys of physicians. Physicians who attend professional conferences and those who take time to complete research questionnaires may have significant differences in their beliefs, knowledge and clinical practice characteristics from nonresponders. Our results may also have limited generalizability due to the study’s regional nature. Although our results clearly support the physicians involvement in low screening rates within these communities, the exact barriers were not identified in this survey. Future studies should focus in more detail on the specific barriers Asian American physicians (especially South Asian) experience in screening their patients for cancer. Monitored interventions directed towards this community of providers and gatekeepers of screening, rather than just the recipients, are also needed.
Conclusions
Eliminating the health disparity for minorities is a major goal of government and non-governmental organization (NGO) initiatives [31]. Our survey reveals that cancer screening remains inadequate among Asian Americans and demonstrates that Asian American physicians should be included in any expansion of culturally competent cancer prevention programs.
Acknowledgment
This study was supported by a subcontract of the cooperative agreement #CA86322 of the National Cancer Institute with Dr. Moon Chen of the Asian American Network for Cancer Awareness, Research and Training (AANCART).
Contributor Information
Ethan E. Bodle, Email: eeb72@columbia.edu, Asian American Network for Cancer Awareness, Research, and Training (AANCART), Mailman School of Public Health, Columbia University, New York, NY, USA; Department of Emergency Medicine, St. Luke’s Roosevelt Hospital Center, New York, NY, USA; 515 West 59th Street, Apt 31J, New York, NY 10019, USA.
Nadia Islam, Asian American Network for Cancer Awareness, Research, and Training (AANCART), Mailman School of Public Health, Columbia University, New York, NY, USA.
Simona C. Kwon, Asian American Network for Cancer Awareness, Research, and Training (AANCART), Mailman School of Public Health, Columbia University, New York, NY, USA
Naseem Zojwalla, Asian American Network for Cancer Awareness, Research, and Training (AANCART), Mailman School of Public Health, Columbia University, New York, NY, USA.
Habibul Ahsan, Asian American Network for Cancer Awareness, Research, and Training (AANCART), Mailman School of Public Health, Columbia University, New York, NY, USA.
Ruby T. Senie, Asian American Network for Cancer Awareness, Research, and Training (AANCART), Mailman School of Public Health, Columbia University, New York, NY, USA
References
- 1.Ries L, Eisner M, Kosary C, Hankey B, Miller B, Clegg L, Mariotto A, Fay M, Feuer E. Edwards Be. SEER cancer statistics review, 1975–2000. Bethesda: National Cancer Institute; 2003. [Google Scholar]
- 2.American Cancer Society. Cancer facts and figures 2004. Atlanta: 2004. p. 28. [Google Scholar]
- 3.Ko CM, Sadler GR, Ryujin L, Dong A. Filipina American women’s breast cancer knowledge, attitudes, and screening behaviors. BMC Public Health. 2003;3:27. doi: 10.1186/1471-2458-3-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maxwell AE, Bastani R, Warda US. Demographic predictors of cancer screening among Filipino and Korean immigrants in the United States. Am J Prev Med. 2000;18:62–68. doi: 10.1016/s0749-3797(99)00110-5. [DOI] [PubMed] [Google Scholar]
- 5.Yu MY, Hong OS, Seetoo AD. Uncovering factors contributing to under-utilization of breast cancer screening by Chinese and Korean women living in the United States. Ethn Dis. 2003;13:213–219. [PubMed] [Google Scholar]
- 6.Chen JY, Diamant AL, Kagawa-Singer M, Pourat N, Wold C. Disaggregating data on Asian and Pacific Islander women to assess cancer screening. Am J Prev Med. 2004;27:139–145. doi: 10.1016/j.amepre.2004.03.013. [DOI] [PubMed] [Google Scholar]
- 7.Thorpe L, Mostashari F, Feldman G, Karpati A, Cobb L, Helgerson D, Frieden T. Cancer screening in New York city: we can do much better. NYC Vital Signs. 2003;2:1–4. [Google Scholar]
- 8.U.S. Census Bureau. [Accessed May 1];American community profile estimates. 2004 Available at: http://www.census.gov/acs/www/Products/Profiles/Single/2002/ACS/Tabular/160/16000US06440001.htm. [Google Scholar]
- 9.U.S. Census Bureau. [Accessed May 11, 2004];The foreign-born population in the United States: 2002. 2002 Available at: http://www.census.gov/prod/2003pubs/p20-539.pdf.
- 10.Hewitt M, Devesa SS, Breen N. Cervical cancer screening among U.S. women: analyses of the 2000 National Health Interview Survey. Prev Med. 2004;39:270–278. doi: 10.1016/j.ypmed.2004.03.035. [DOI] [PubMed] [Google Scholar]
- 11.Lauderdale DS, Kestenbaum B. Asian American ethnic identification by surname. Popul Res Policy Rev. 2000;19:283–300. [Google Scholar]
- 12.Lee MM, Lee F, Stewart S, McPhee S. Cancer screening practices among primary care physicians serving Chinese Americans in San Francisco. West J Med. 1999;170:148–155. [PMC free article] [PubMed] [Google Scholar]
- 13.American Academy of Family Physicians. Summary of policy recommendations for periodic health examinations, Revision 5.6. [Accessed November 3, 2004]; Available at: http://www.aafp.org/exam.xml. [Google Scholar]
- 14.National Cancer Institute. Bethesda: U.S. National Institutes of Health; 2002. NCI statement on mammography. [Google Scholar]
- 15.Smith RA, Cokkinides V, Eyre HJ. American Cancer Society guidelines for the early detection of cancer. CA Cancer J Clin. 2004;54:41–52. doi: 10.3322/canjclin.54.1.41. [DOI] [PubMed] [Google Scholar]
- 16.U.S. Preventive Services Task Force. Guide to clinical preventive services. Periodic updates. (3rd ed.) Available at: http://www.ahcpr.gov/clinic/gcpspu.htm.
- 17.Winawer SFR, Rex D, Bond J, Burt R, Ferrucci J, Ganiats T, Levin T, Woolf S, Johnson D, Kirk L, Litin S, Simmang C. Colorectal cancer screening and surveillance: clinical guidelines and rationale-update based on new evidence. Gastroenterology. 2003;124:544–560. doi: 10.1053/gast.2003.50044. [DOI] [PubMed] [Google Scholar]
- 18.Coughlin SS, Uhler RJ. Breast and cervical cancer screening practices among Asian and Pacific Islander women in the United States, 1994–1997. Cancer Epidemiol Biomarkers Prev. 2000;9:597–603. [PubMed] [Google Scholar]
- 19.Juon HS, Kim M, Shankar S, Han W. Predictors of adherence to screening mammography among Korean American women. Prev Med. 2004;39:474–481. doi: 10.1016/j.ypmed.2004.05.006. [DOI] [PubMed] [Google Scholar]
- 20.Lew AA, Moskowitz JM, Ngo L, Wismer BA, Wong JM, Ahn Y, Tager IB. Effect of provider status on preventive screening among Korean–American women in Alameda County, California. Prev Med. 2003;36:141–149. doi: 10.1016/s0091-7435(02)00039-7. [DOI] [PubMed] [Google Scholar]
- 21.Gotzsche PC, Nielsen M. Screening for breast cancer with mammography. Cochrane Database Syst Rev. 2006 doi: 10.1002/14651858.CD001877.pub2. CD001877. [DOI] [PubMed] [Google Scholar]
- 22.American College of Obstetricians and Gynecologists. 2nd ed. Washington DC: ACOG; 2002. Guidelines for women’s health care. [Google Scholar]
- 23.Bottorff JL, Balneaves LG, Sent L, Grewal S, Browne AJ. Cervical cancer screening in ethnocultural groups: case studies in women-centered care. Women Health. 2001;33:29–46. [PubMed] [Google Scholar]
- 24.Lurie N, Slater J, McGovern P, Ekstrum J, Quam L, Margolis K. Preventive care for women. Does the sex of the physician matter? N Engl J Med. 1993;329:478–482. doi: 10.1056/NEJM199308123290707. [DOI] [PubMed] [Google Scholar]
- 25.WHO Department of Communicable Disease Surveillance and Response. Hepatitis B. [Accessed May 3, 2005]; Available at: http://www.who.int/csr/disease/hepatitis/HepatitisB_whocdscsrlyo2002_2.pdf.
- 26.Centers for Disease Control and Prevention. Incidence of acute hepatitis B—United States, 1990–2002. MMWR Morb Mortal Wkly Rep. 2004;52:1252–1254. [PubMed] [Google Scholar]
- 27.Liaw YF, Leung N, Guan R, Lau GK, Merican I. Asian–Pacific consensus statement on the management of chronic hepatitis B: an update. J Gastroenterol Hepatol. 2003;18:239–245. doi: 10.1046/j.1440-1746.2003.03037.x. [DOI] [PubMed] [Google Scholar]
- 28.Kenny T, Wilson R, Purves I, Clark J, Newton L, Newton D, Moseley D. A PIL for every ill? Patient information leaflets (PILs): a review of past, present and future use. Fam Pract. 1998;15:471–479. doi: 10.1093/fampra/15.5.471. [DOI] [PubMed] [Google Scholar]
- 29.Asian American Network for Cancer Awareness Research and Training. AANCART: Resources. Available at: http://www.aancart.org/Resources.htm. [PMC free article] [PubMed] [Google Scholar]
- 30.Kliewer E, Smith K. Breast cancer mortality among immigrants in Australia and Canada. J Natl Cancer Inst. 1995;87:1154–1161. doi: 10.1093/jnci/87.15.1154. [DOI] [PubMed] [Google Scholar]
- 31.Fields CV. New York: Manhattan Borough President’s Office; 2004. Closing the health divide: what government can do to eliminate health disparities among communities of color in New York city. [Google Scholar]