For well over half a century, the link between insulin resistance and type 2 diabetes has been recognized. Insulin resistance is important. Not only is it the most powerful predictor of future development of type 2 diabetes, it is also a therapeutic target once hyperglycemia is present. In this issue of Diabetes, Morino et al. (1) report a series of studies that provide evidence of a genetic mechanism linking expression of lipoprotein lipase (LPL) to peroxisome proliferator–activated receptor (PPAR)-δ expression and mitochondrial function. This is likely to contribute to the muscle insulin resistance that predisposes to type 2 diabetes.
Observation of abnormal mitochondrial function in vitro in type 2 diabetes (2) was soon followed by in vivo demonstration of this abnormality in insulin-resistant, first-degree relatives of people with type 2 diabetes (3). Further reports of a modest defect in muscle mitochondrial function in type 2 diabetes were published shortly thereafter (4,5). These studies raised the question of whether type 2 diabetes could be a primary disorder of the mitochondria. However, the study of first-degree relatives tended to be misinterpreted as having shown a major defect in mitochondrial function in type 2 diabetes, although it had studied nondiabetic groups from the opposite ends of the insulin resistance–sensitivity spectrum. Indeed, other studies showed no defect in mitochondrial function in type 2 diabetes (6,7), which led to further confusion. Mitochondrial function was then shown to be acutely modifiable by changing fatty acid availability (8) and that it was affected by ambient blood glucose concentration (9). When ambient blood glucose levels were near normal in diabetes, no defect in mitochondrial function was apparent.
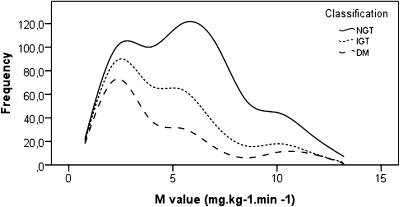
But if mitochondrial function in well-controlled type 2 diabetes is not abnormal, is a defect in insulin-resistant, first-degree relatives clinically relevant? The answer is provided in Fig. 1, which shows population distributions of insulin sensitivity for normoglycemia, impaired glucose tolerance, and type 2 diabetes. The wide range of insulin sensitivity in the normoglycemic population fully encompasses the range observed in type 2 diabetes. Even though mean insulin sensitivity in diabetes is lower than that of matched control subjects, values are drawn from the same distribution and, with matching for body weight and physical activity, differences will be relatively small. Differences in insulin sensitivity will be particularly evident when making comparisons between groups selected from the extreme ends of the population distribution (Fig. 1). When parameters directly linked to muscle insulin resistance are compared between groups selected in this way, any linked difference will be maximized, making this strategy entirely appropriate to investigate the pathophysiology of muscle insulin resistance.
FIG. 1.
Distribution curves of insulin sensitivity as measured by the euglycemic-hyperinsulinemic clamp showing that people with type 2 diabetes sit within the range of the nondiabetic distribution, but toward the lower range. Identification of factors underlying muscle insulin resistance itself can be investigated by comparing groups drawn from the extremes of the total population distribution. Such factors may not be clearly discernible when type 2 diabetic individuals are compared with normoglycemic control subjects matched for weight and physical activity. The data are from previously published population studies of normal glucose tolerance (n = 256), impaired glucose tolerance (n = 119), and type 2 diabetes (n = 194) (20,21).
Muscle insulin resistance as determined by the euglycemic-hyperinsulinemic clamp is clearly a risk factor for development of type 2 diabetes (10). However, the pathophysiology of hyperglycemia in established diabetes relates to hepatic not muscle insulin resistance. This distinction has been elegantly demonstrated in studies of moderate calorie restriction in type 2 diabetes, which resulted in a fall in liver fat, normalization of hepatic insulin sensitivity, and fasting plasma glucose, but no change in muscle insulin resistance (11). More recent work employing severe calorie restriction confirmed previous findings and also demonstrated a longer-term return of normal insulin secretion as intrapancreatic fat content fell (12). The fact that fasting and postprandial normoglycemia can be restored in type 2 diabetes without change in muscle insulin resistance should not be surprising. Mice totally lacking in skeletal muscle insulin receptors do not develop diabetes (13). People with inactive muscle glycogen synthase are not necessarily hyperglycemic (14), and many normoglycemic individuals maintain normal blood glucose with a degree of muscle insulin resistance identical to that among people who develop type 2 diabetes (Fig. 1). The relevance of muscle insulin resistance for development of type 2 diabetes is more subtle. Over many years and only in the presence of chronic calorie excess, hyperinsulinemia steadily brings about hepatic fat accumulation and hepatic insulin resistance. Onset of hyperglycemia is ultimately determined by failure of nutrient-stimulated insulin secretion (15). This new understanding is described by the twin cycle hypothesis (16). So what actually determines this critical primary insulin resistance in muscle?
Morino et al. (1) report analyses of mRNA in muscle biopsies to compare expression of genes involved in mitochondrial fatty acid oxidation. Their experiments compare data for subjects at opposite extremes of the insulin resistance spectrum. Findings were confirmed in independent groups selected in the same way and two genes were found to be consistently lower in expression. Using knock down of expression by appropriate inhibitory RNA, Western blotting showed that LPL was the important gene product. In both human rhabdomyosarcoma cells and L6 myocytes, such knock down of LPL induced a decrease in mitochondrial density. The function of LPL is to release fatty acids from triglyceride for direct cellular uptake. The biological relevance of the link between decreased mitochondrial numbers and RNA interference (RNAi) inhibition of LPL was confirmed by observing that the effect was only seen if fat was present in the extracellular media. To test the hypothesis that fatty acid flux into cells regulates mitochondrial biogenesis by a PPAR-dependent process, knock down of PPAR-δ was also shown to decrease mitochondrial density. Furthermore, limitation of fatty acid uptake by directly inhibiting the transmembrane fatty transporter CD36 was shown to achieve the same effect. Overall, these studies suggest that insulin resistance is related to decreased mitochondrial content in muscle due, at least in part, to reductions in LPL expression and consequent decreased PPAR-δ activation.
This important article establishes a biological mechanism whereby insulin resistance in muscle is causally linked to genetic influences that are measurable in the general population. It focuses on insulin resistance by comparing extremes of the distribution of this characteristic in the normal population. But does insulin resistance cause mitochondrial dysfunction, or vice versa? The former appears more likely on the basis of current evidence. Exercise can reduce insulin resistance and ameliorate mitochondrial dysfunction (17), whereas established mitochondrial dysfunction does not necessarily produce insulin resistance in animal models or in humans (18,19). Understanding the nature of common insulin resistance in muscle and its relationship to type 2 diabetes is long overdue. Future work should determine whether specific therapeutic manipulation can offset the effect of identifiable genetic influences and interrupt the long run-in to type 2 diabetes.
ACKNOWLEDGMENTS
No potential conflicts of interest relevant to this article were reported.
The author is grateful to Leif Groop of Lund University for permission to use combined data from the Botnia Study and the Malmö Prospective Study in Fig. 1 and to Jasmina Kravic of Lund University for replotting the data.
Footnotes
See accompanying original article, p. 877.
REFERENCES
- 1.Morino K, Petersen KF, Sono S, et al. Regulation of mitochondrial biogenesis by lipoprotein lipase in muscle of insulin-resistant offspring of parents with type 2 diabetes. Diabetes 2012;61:877–887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kelley DE, He J, Menshikova EV, Ritov VB. Dysfunction of mitochondria in human skeletal muscle in type 2 diabetes. Diabetes 2002;51:2944–2950 [DOI] [PubMed] [Google Scholar]
- 3.Petersen KF, Dufour S, Befroy D, Garcia R, Shulman GI. Impaired mitochondrial activity in the insulin-resistant offspring of patients with type 2 diabetes. N Engl J Med 2004;350:664–671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Szendroedi J, Schmid AI, Chmelik M, et al. Muscle mitochondrial ATP synthesis and glucose transport/phosphorylation in type 2 diabetes. PLoS Med 2007;4:e154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Phielix E, Schrauwen-Hinderling VB, Mensink M, et al. Lower intrinsic ADP-stimulated mitochondrial respiration underlies in vivo mitochondrial dysfunction in muscle of male type 2 diabetic patients. Diabetes 2008;57:2943–2949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.De Feyter HM, van den Broek NM, Praet SF, Nicolay K, van Loon LJ, Prompers JJ. Early or advanced stage type 2 diabetes is not accompanied by in vivo skeletal muscle mitochondrial dysfunction. Eur J Endocrinol 2008;158:643–653 [DOI] [PubMed] [Google Scholar]
- 7.Lim EL, Hollingsworth KG, Smith FE, Thelwall PE, Taylor R. Effects of raising muscle glycogen synthesis rate on skeletal muscle ATP turnover rate in type 2 diabetes. Am J Physiol Endocrinol Metab 2011;301:E1155–E1162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lim EL, Hollingsworth KG, Smith FE, Thelwall PE, Taylor R. Inhibition of lipolysis in Type 2 diabetes normalizes glucose disposal without change in muscle glycogen synthesis rates. Clin Sci (Lond) 2011;121:169–177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schrauwen-Hinderling VB, Kooi ME, Hesselink MK, et al. Impaired in vivo mitochondrial function but similar intramyocellular lipid content in patients with type 2 diabetes mellitus and BMI-matched control subjects. Diabetologia 2007;50:113–120 [DOI] [PubMed] [Google Scholar]
- 10.Lillioja S, Mott DM, Spraul M, et al. Insulin resistance and insulin secretory dysfunction as precursors of non-insulin-dependent diabetes mellitus. Prospective studies of Pima Indians. N Engl J Med 1993;329:1988–1992 [DOI] [PubMed] [Google Scholar]
- 11.Petersen KF, Dufour S, Befroy D, Lehrke M, Hendler RE, Shulman GI. Reversal of nonalcoholic hepatic steatosis, hepatic insulin resistance, and hyperglycemia by moderate weight reduction in patients with type 2 diabetes. Diabetes 2005;54:603–608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lim EL, Hollingsworth KG, Aribisala BS, Chen MJ, Mathers JC, Taylor R. Reversal of type 2 diabetes: normalisation of beta cell function in association with decreased pancreas and liver triacylglycerol. Diabetologia 2011;54:2506–2514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brüning JC, Michael MD, Winnay JN, et al. A muscle-specific insulin receptor knockout exhibits features of the metabolic syndrome of NIDDM without altering glucose tolerance. Mol Cell 1998;2:559–569 [DOI] [PubMed] [Google Scholar]
- 14.Savage DB, Zhai L, Ravikumar B, et al. A prevalent variant in PPP1R3A impairs glycogen synthesis and reduces muscle glycogen content in humans and mice. PLoS Med 2008;5:e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ferrannini E, Nannipieri M, Williams K, Gonzales C, Haffner SM, Stern MP. Mode of onset of type 2 diabetes from normal or impaired glucose tolerance. Diabetes 2004;53:160–165 [DOI] [PubMed] [Google Scholar]
- 16.Taylor R. Pathogenesis of type 2 diabetes: tracing the reverse route from cure to cause. Diabetologia 2008;51:1781–1789 [DOI] [PubMed] [Google Scholar]
- 17.Ritov VB, Menshikova EV, Azuma K, et al. Deficiency of electron transport chain in human skeletal muscle mitochondria in type 2 diabetes mellitus and obesity. Am J Physiol Endocrinol Metab 2010;298:E49–E58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zechner C, Lai L, Zechner JF, et al. Total skeletal muscle PGC-1 deficiency uncouples mitochondrial derangements from fiber type determination and insulin sensitivity. Cell Metab 2010;12:633–642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maassen JA, ‘t Hart LM, van Essen E, et al. Mitochondrial diabetes: molecular mechanisms and clinical presentation. Diabetes 2004;53(Suppl. 1):S103–S109 [DOI] [PubMed] [Google Scholar]
- 20.Groop L, Forsblom C, Lehtovirta M, et al. Metabolic consequences of a family history of NIDDM (the Botnia study): evidence for sex-specific parental effects. Diabetes 1996;45:1585–1593 [DOI] [PubMed] [Google Scholar]
- 21.Tripathy D, Eriksson KF, Orho-Melander M, Fredriksson J, Ahlqvist G, Groop L. Parallel manifestation of insulin resistance and beta cell decompensation is compatible with a common defect in Type 2 diabetes. Diabetologia 2004;47:782–793 [DOI] [PubMed] [Google Scholar]