Abstract
Objectives
We provide an overview of the Health Resources and Services Administration HIV/AIDS Bureau's Special Projects of National Significance Innovations in Oral Health Care Initiative, describe the models developed by the 15 demonstration sites and associated evaluation center, and present initial descriptive data about the characteristics of the multisite evaluation study sample.
Methods
Baseline data were collected from May 2007–August 2009 for 2,469 adults living with HIV/AIDS who had been without dental care, except for emergency care, for 12 months or longer. Variables included sociodemographic characteristics, HIV status, medical care, history of dental care and oral health symptoms, oral health practices, and physical and mental health quality of life. Descriptive statistics of baseline variables were calculated.
Results
The study sample included 2,469 adults who had been HIV-positive for a decade; most were engaged in HIV care. The majority (52.4%) of patients had not seen a dentist in more than two years; 48.2% reported an unmet oral health-care need since testing positive for HIV, and 63.2% rated the health of their teeth and gums as “fair” or “poor.”
Conclusions
This study is the largest to examine oral health care among people living with HIV/AIDS in more than a decade. The need for access to oral health care among members of this HIV-positive patient sample is greater than in the general population, following previous trends. Findings from our study reinforce the necessity for continued federal and statewide advocacy and support for oral health programs targeting people living with HIV/AIDS; findings can be extended to other vulnerable populations.
The Centers for Disease Control and Prevention (CDC) estimates that more than 1.1 million people are living with human immunodeficiency virus (HIV) infection in the U.S.,1 and the incidence rate for new U.S. HIV infections continues at approximately 50,000 cases annually.2 Over the past 30 years, efforts to prolong and improve the quality of patients' lives through medical care, pharmaceutical interventions such as combination antiretroviral therapy (cART), and support services have been successful. More people with HIV and acquired immunodeficiency syndrome (AIDS) are living longer productive lives.3 Amid all the advances in HIV/AIDS care and treatment, however, access to oral health care continues to be frequently cited by state and regional HIV/AIDS consumer needs assessments as the primary unmet need.4,5
The importance of oral health for people living with HIV has been documented. In the 2000 Surgeon General's report Oral Health in America, Surgeon General David Satcher described the mouth as the gateway to the body. It signals nutritional deficiencies and serves as an early warning system for diseases such as HIV/AIDS and other infections related to the immune system.5 Oral health problems can have a great impact on a patient's overall health, especially if that person has a compromised immune system and is thus more vulnerable to infection.6 In the early 1990s, studies estimated that up to 90% of HIV-positive patients would have at least one oral manifestation during the course of their disease.7,8 Due to the success of cART, the incidence of oral manifestations has decreased; however, the type of oral manifestations encountered by oral health providers is shifting.8 According to recent estimates, HIV-related oral conditions may occur at least once over the course of the disease in as few as 30% of HIV patients.9,10 Although the incidence of certain oral manifestations such as oral candidiasis and Kaposi's sarcoma has decreased,11 the rate of HIV salivary gland disease has increased. HIV salivary gland disease results in xerostomia (dry mouth), which is also frequently cited as a side effect of some HIV medications. This reduction in the volume of saliva, as well as chemical changes that lower the antimicrobial properties of saliva, can result in an increase in dental problems such as tooth decay and periodontal disease.12 The observance of an increase in certain oral manifestations such as oral warts11 and HIV salivary gland disease, coupled with a longer patient life expectancy after HIV diagnosis, strongly indicates the need for access to continuous oral health care for people living with HIV and AIDS (PLWHA).
Studies conducted in the last two decades suggest, however, that PLWHA have limited access to oral health care. The Surgeon General reported that 11% (16.7 million) of Americans needed oral health care but were not able to access it for a number of reasons, most commonly the cost of care.5 The HIV Cost and Services Utilization Study (HCSUS), conducted in 1996–1997 by the Agency for Healthcare Research and Quality and the RAND Corporation, included detailed oral health questions in a survey of PLWHA in the U.S. who were engaged in medical care. Based on this nationally representative study, researchers estimated that 40% of PLWHA needed oral health care in the past six months but did not get it.13 Other studies have reported an unmet need for oral health care among PLWHA ranging from 5% to 52% in the pre-cART era; the inability to pay for dental care was the primary reason for not receiving care.13–18 More than a decade since the HCSUS, barriers to dental care for PLWHA persist, in part due to lack of coverage through private insurance and the dwindling benefits provided by state Medicaid programs, as well as patients' inability to pay for dental services out-of-pocket. Other barriers to care include the inability to find an HIV-friendly dentist, fear of going to the dentist, and concerns about confidentiality.5
In 2006, the HIV/AIDS Bureau of the Health Resources and Services Administration (HRSA) funded an initiative under its Special Projects of National Significance (SPNS) program to address these issues and expand access to dental services for PLWHA. The Innovations in Oral Health Care Initiative (hereafter, Oral Health Initiative) comprised 15 sites across the U.S. serving both urban and rural populations, and a multisite evaluation and technical assistance center. The goals of the initiative were to (1) develop innovative models of comprehensive oral health-care services for PLWHA; (2) expand oral health services to new communities and populations; (3) implement models to maximize payment of services from all sources, including Medicaid and other community resources, and develop financing methods to sustain dental services; (4) establish linkages and referrals to HIV medical care and support services to ensure a continuum of care; and (5) provide appropriate training and support for clinical and other staff in developing the expertise to manage oral health care for PLWHA, and provide ongoing education in HIV care management.19
In addition to sponsoring sites to provide oral health care, the SPNS program established the Evaluation Center on HIV and Oral Health (ECHO). ECHO, convened by the Boston University School of Public Health, comprised a team of experts, including dentists, dental hygienists, policy analysts, and researchers. ECHO's goals were to (1) provide technical assistance to help oral health providers and programs improve access and adherence to high quality oral health care for underserved populations; (2) implement a mixed-methods multisite evaluation of the demonstration projects; (3) assist grantees in implementing both the multisite evaluation and their local evaluations; and (4) disseminate findings to a broad range of audiences including oral health-care providers, medical care providers, consumers, and policy makers. In collaboration with the demonstration grantees, ECHO implemented a longitudinal quantitative evaluation using patient survey and dental utilization data at all sites and a qualitative study involving two in-depth interviews with a small sample of patients at six sites. ECHO also provided clinical and programmatic technical assistance to all the sites.
The purpose of this initial article in the supplement is to provide an overview of the Oral Health Initiative, including information about the models developed by the 15 demonstration sites. We also discuss the approach developed to evaluate the demonstration sites and present baseline descriptive data of the characteristics of the 2,469 adult PLWHA who accessed dental care after not receiving any care in the prior 12 months other than for an emergency.
METHODS
Theoretical model
The design of the Oral Health Initiative evaluation was based on the Institute of Medicine's (IOM's) conceptual model of access to personal health-care services.20 The IOM model suggests that access to care is shaped by structural barriers, such as availability of services or transportation; financial barriers, such as a lack of health insurance coverage or inability to pay; and personal barriers, such as culture, language, and education. Use of services is further mediated by efficacy of treatment, quality of providers, and patient adherence to health-care treatment, leading to improvements in patient outcomes such as health status and reductions in patients' unmet needs. Using a participatory approach with sites, ECHO designed the evaluation and operationalized measures to reflect the IOM model domains.
Study design and recruitment
Fifteen oral health programs in 12 states and one U.S. territory participated in the study. The sites were located in San Francisco, California; Eugene, Oregon; Tyler, Texas; New Orleans, Lousiana; Green Bay, Wisconsin; Miami, Florida; Jefferson, South Carolina; Chapel Hill, North Carolina; Chester, Pennsylvania; New York, New York; Norwalk, Connecticut; Provincetown, Massachusetts; and St. Croix, U.S. Virgin Islands. The oral health programs were located at universities, hospitals, Community Health Centers, and AIDS service organizations. The sites recruited HIV-positive patients for the study through direct outreach to patients, collaboration with social-service organization and HIV case managers, and referrals from HIV clinics.
Staff at the Oral Health Initiative sites gathered quantitative baseline and follow-up data through structured interviews. Researchers developed survey instruments through a participatory process with staff at all sites, drawing from existing tools whenever possible. The baseline interview, guided by this survey, was conducted in person when a patient enrolled in the study. Follow-up interviews were conducted at six, 12, 18, and 24 months via phone or in person. Baseline interview data included sociodemographic characteristics, mode of HIV transmission, and access-to-care barriers as defined by the IOM model. Variables related to structural barriers included the patient's regular place for dental care, unmet dental need since testing positive for HIV, the last time the patient saw a dentist, and how long it took the patient to get to the first study-related dental appointment. Variables related to financial barriers included health insurance and dental insurance coverage. Variables to measure personal barriers included income, education level, language, patient hygiene practices, and risk behaviors such as past and current substance, tobacco, and alcohol use, which could impact oral health outcomes. The interview also included items from validated and reliable standardized measures including the SF-8™ Health Survey to measure health-related quality of life21 and a brief oral quality-of-life scale.22 Researchers pretested the baseline instrument at the sites and made slight modifications to items that needed more clarity. Follow-up interviews collected the same data except for sociodemographic characteristics that were not expected to change (e.g., age and race/ethnicity).
Data collection
Study eligibility criteria included (1) self-reported HIV infection, (2) 18 years of age or older, (3) no routine or preventive dental care within the past 12 months, and (4) an initial study-related oral health visit within 45 days after completing the baseline interview. Baseline data collection occurred from May 1, 2007, through August 31, 2009. Interviewers at each site participated in a standard training program conducted by ECHO. Interviews were repeated every six months for up to two years and were conducted in both English and Spanish. All participants gave informed consent to participate.
Each time an interview was conducted, staff collected patient clinical data, including the participant's most recent CD4 cell count (measured in cells per cubic millimeter [cells/mm3]) and viral load from laboratory reports or medical charts, as well as detailed clinic visit data, dental utilization data, and information about oral health-related referrals. At each patient visit, sites reported whether or not the Phase I treatment plan was completed. Phase I treatment was defined as prevention, maintenance, and/or elimination of oral pathology that results from dental caries or periodontal disease.23 All follow-up interview, clinic visit, and utilization data collection ended on August 31, 2010. Data from all 15 sites were entered into a Web-based database hosted by ECHO. ECHO then cleaned and merged the data into a single multisite database.
Analysis
We calculated descriptive statistics using SPSS® version 16.0.24 The results are categorized in the following manner: sociodemographics; description of HIV status and medical care and services; history of dental care and oral health symptoms; oral health practices; and physical, mental, and oral health status. Qualitative data collected about the program models were analyzed using case study methods.25
RESULTS
Program models
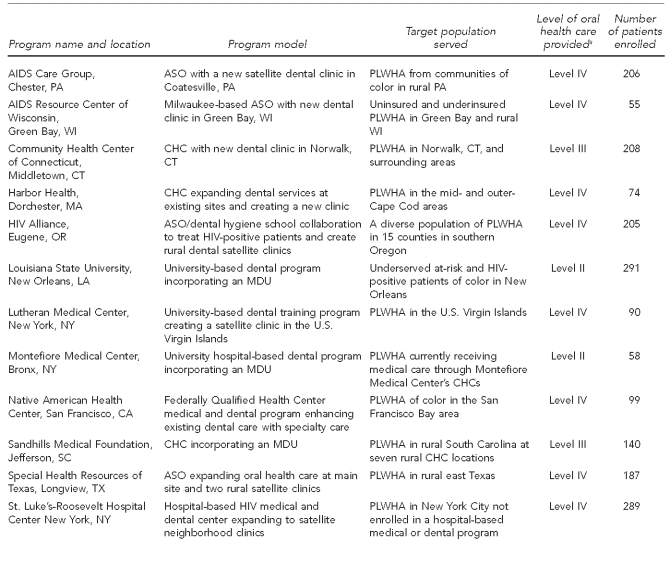
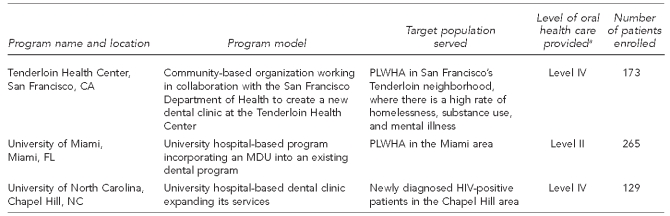
The Figure describes the program models, target populations served, level of oral health care provided, and number of patients enrolled in the multisite evaluation at each site. Five programs (33%) were AIDS service organizations or community-based organizations, and six programs (40%) were hospital-based programs. The remaining four programs were Community Health Centers. Six programs (40%) were located in major metropolitan cities, four programs (27%) served both urban and rural populations, and five programs served rural communities. To increase access to oral health-care services, four programs (27%) incorporated a mobile dental unit and nine programs (60%) employed a dental care coordinator or dental case manager as part of their model.26 All programs served patients living with HIV, with a majority of programs targeting low-income populations and communities of color.
Figure.
Health Resources and Services Administration HIV/AIDS Bureau's Special Projects of National Significance Oral Health Initiative: program models, May 2007–August 2010
aLevel I includes diagnostic and preventive services, such as oral exams, radiographs, dental prophylaxis (cleaning), and fluoride therapies. Level II is inclusive of all treatment in Level I as well as restorative procedures (fillings), simple extractions, nonsurgical periodontal care, night guards, management of common oral lesions associated with HIV disease, emergency care, and chair-side denture reline/repair. Level III is inclusive of Level II and adds removable prosthetics (complete and partial dentures), single-unit crowns, endodontic therapy (anterior and premolar root canals), cast post and core build-ups, and laboratory denture repair/reline. Level IV is inclusive of all procedures of Level III with the addition of fixed bridge work, periodontal surgery, biopsy of suspect lesions, molar endodontics, complex surgical extractions, implants, apicoectomy, and specialty care that is often referred to other providers.
HIV = human immunodeficiency virus
AIDS = acquired immunodeficiency syndrome
ASO = AIDS Service Organization
PLWHA = people living with HIV/AIDS
CHC = Community Health Center
MDU = mobile dental unit
Sites provided a range of dental services that were categorized into four levels for the purpose of this study. Level I includes diagnostic and preventive services, such as oral exams, radiographs, dental prophylaxis (cleaning), and fluoride therapies. Level II is inclusive of all treatment in Level I as well as restorative procedures (fillings), simple extractions, nonsurgical periodontal care, night guards, management of common oral lesions associated with HIV disease, emergency care, and chair-side denture reline/repair. Level III is inclusive of Level II and adds removable prosthetics (complete and partial dentures), single-unit crowns, endodontic therapy (anterior and premolar root canals), cast post and core build-ups, and laboratory denture repair/reline. Level IV includes all procedures of the previous level with the addition of fixed bridge work, periodontal surgery, biopsy of suspect lesions, molar endodontics, complex surgical extractions, implants, apicoectomy, and specialty care that is often referred to other providers. The total number of patients enrolled in the multisite evaluation study was 2,469.
Sociodemographics of the ECHO sample at baseline
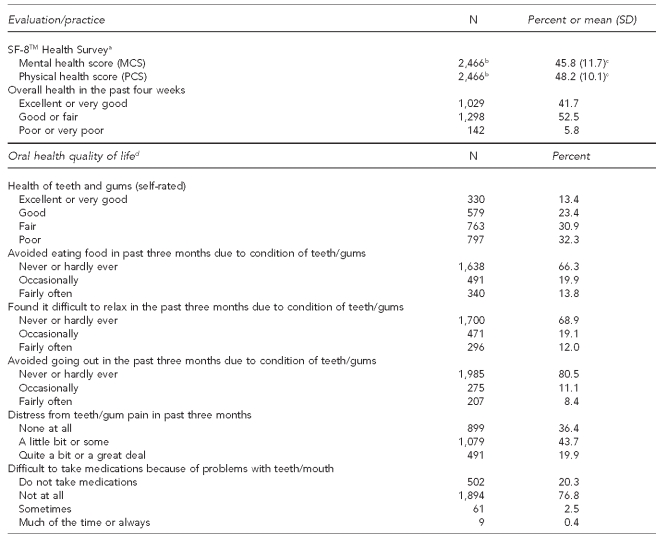
Table 1 describes the baseline demographic characteristics of the study sample at the time of enrollment. Participants ranged in age from 18 to 81 years with a mean age of 43.6 years. People who identified as black comprised 40.6% of the sample, followed by those who identified as white (33.2%). The majority of the sample was male (75.0%). Most study participants were born in the U.S. (81.8%) and reported English as their primary language (85.4%). The majority of patients (59.8%) reported living in their own home or apartment and had completed high school (33.4%) or schooling beyond high school (43.0%). More than half of the study participants reported either being unemployed (35.3%) or having a disability that prevented employment (32.8%). Most reported a monthly income of ≤$850 (55.7%); $850 per month was the federal poverty level for one person when this study began in 2006. When asked about current smoking status, 52.1% reported being current smokers. Regarding drug use, 39.9% reported having ever used crack/cocaine, while 3.3% reported using it in the past 30 days. In addition, 20.3% reported past use of crystal methamphetamine, with 2.7% reporting using it in the past 30 days. A minority (17.0%) of patients reported having some type of removable denture appliance at baseline.
Table 1.
Descriptive characteristics for the ECHO study sample (n=2,469): SPNS Oral Health Initiative, 15 U.S. sites, May 2007–August 2009
ECHO = Evaluation Center on HIV and Oral Health
SPNS = Special Projects of National Significance
SD = standard deviation
meth = methamphetamine
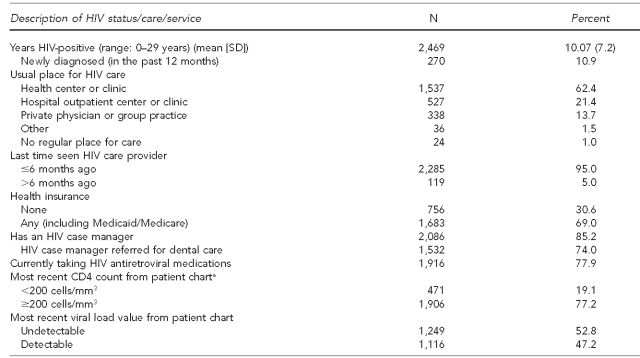
Description of HIV status and medical care and services
Among study participants, the mean number of years since testing HIV-positive was 10 years (Table 2). A small percentage of patients (10.9%) were newly diagnosed with HIV in the 12 months prior to their baseline interview. The majority of the study sample was engaged in HIV medical care at a health center or clinic (62.4%), a hospital or outpatient clinic (21.4%), or a private physician or group practice (13.7%), and 95.0% reported seeing their HIV clinician in the past six months. Values collected from laboratory reports or medical records indicated that 52.8% of the study sample had an undetectable viral load and 77.2% had a CD4 count of ≥200 cells/mm3. The range for a healthy CD4 count is 500–1,000 cells/mm3. A CD4 count of <200 cells/mm3 is an indicator of an AIDS diagnosis.27 In addition, 77.9% of the study participants reported taking HIV antiretroviral medications. A majority of the study sample had an HIV case manager (85.2%); of those patients, 74.0% had been referred to dental care by their HIV case manager. Health insurance coverage of this population varied. In total, 69.0% of participants reported having some sort of health-care coverage, either public (Medicaid or Medicare) or private. Medicaid was the primary insurance for 23.5% of the study sample (data not shown).
Table 2.
Description of HIV status and medical care and services for the ECHO study sample (n=2,469): SPNS Oral Health Initiative, 15 U.S. sites, May 2007–August 2009
aThe range for a healthy CD4 count is 500–1,000 cells/mm3. A CD4 count of <200 cells/mm3 is an indicator of an AIDS diagnosis. Source: Department of Health and Human Services (US). AIDS.gov: understand your test results: CD4 count [cited 2010 Dec 13]. Available from: URL: http://aids.gov/hiv-aids-basics/diagnosed-with-hiv-aids/understand-your-test-results/cd4-count
HIV = human immunodeficiency virus
ECHO = Evaluation Center on HIV and Oral Health
SPNS = Special Projects of National Significance
SD = standard deviation
mm3 = cubic millimeter
AIDS = acquired immunodeficiency syndrome
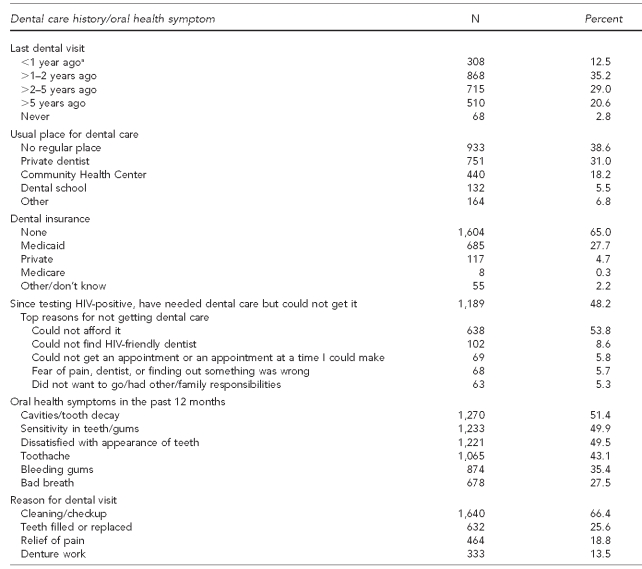
History of dental care and oral health symptoms
Table 3 shows the baseline responses to questions related to the participant's last dental visit, usual place for dental care, dental insurance, reasons for not getting dental care, oral health symptoms in the past 12 months, and presenting complaint at their first study-related oral health visit. Slightly more than half (52.4%) of the study participants reported being without oral health care for two or more years, and more than a third (38.6%) reported not having a regular place for dental care. Another third (31.0%) reported their usual place for dental care was a private dentist. When asked if there had been a time since testing HIV-positive during which they needed oral health care but were unable to get it, 48.2% responded “yes,” citing an inability to pay as the primary reason for not getting the oral health care (53.8% of those responding “yes”). Most participants (65.0%) had no dental coverage and 27.7% listed Medicaid as their dental coverage; dental coverage by Medicaid in some states is limited or does not exist.28
Table 3.
History of dental care and oral health symptoms for the ECHO study sample (n=2,469): SPNS Oral Health Initiative, 15 U.S. sites, May 2007–August 2009
aPatients had received only emergency oral health services in the past year.
ECHO = Evaluation Center on HIV and Oral Health
SPNS = Special Projects of National Significance
HIV = human immunodeficiency virus
Participants were also queried about their oral health symptoms in the past 12 months. About half of the sample reported cavities/tooth decay (51.4%), sensitivity in their teeth/gums (49.9%), and dissatisfaction with the appearance of their teeth (49.5%). Toothache (43.1%), bleeding gums (35.4%), and bad breath (27.5%) were also frequently reported. Conversely, when asked at their first oral health visit about their reason for the appointment, 66.4% cited a cleaning/checkup as opposed to a specific problem.
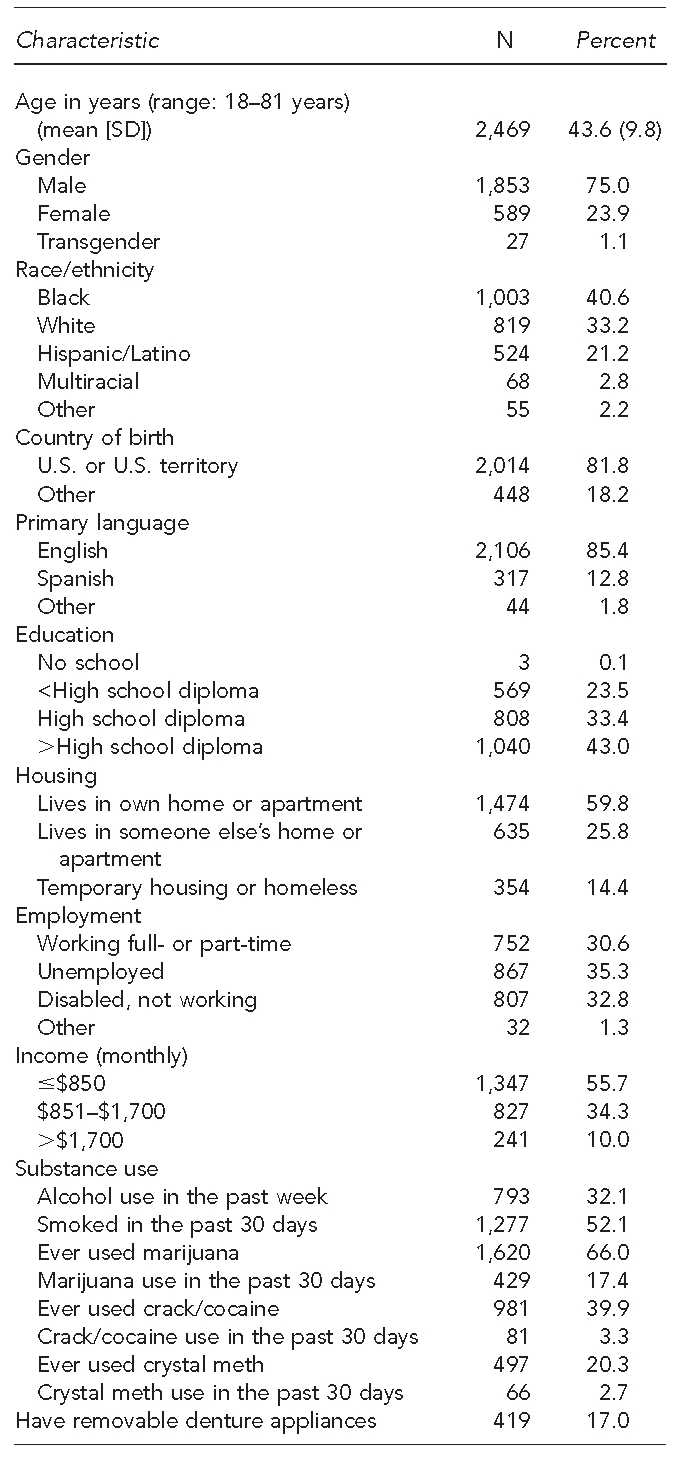
Quality of life and oral health practices
The SF-8™ Health Survey (which stands for Medical Outcomes Study Short Form 8) measures two domains: physical health (four items) and mental health (four items). It is a reliable and valid measure of health-related quality of life. The SF-8 items were included in the baseline patient interview. As part of the SF-8 survey, participants were asked to rate their overall health in the past four weeks.21 As shown in Table 4, slightly more than half of participants (52.5%) rated their overall health as “good or fair,” and an additional 41.7% rated their overall health as “excellent or very good.” The physical health score is derived from the patient's perception of his or her overall health, limitations due to physical health issues, difficulty with daily work due to physical health issues, and bodily pain in the prior four weeks. The mental health score is derived from the patient's perception of personal energy, the impact of physical or emotional problems on social activity, the extent of being bothered by emotional problems, and the impact of emotional problems on daily life activities. The mean physical and mental health scores for the SF-8 were 48.2 and 45.8, respectively. These scores were below the average score of 50.0 for each of the domains for the general population not living with a chronic illness.21
Table 4.
Quality of life and oral health practices for the ECHO study sample (n=2,469): SPNS Oral Health Initiative, 15 U.S. sites, May 2007–August 2009
aThe physical health score is derived from the patient's perception of his or her overall health, limitations due to physical health issues, difficulty with daily work due to physical health issues, and bodily pain in the prior four weeks. The mental health score is derived from the patient's perception of personal energy, the impact of physical or emotional problems on social activity, the extent of being bothered by emotional problems, and the impact of emotional problems on daily life activities. Source: Ware JE, Kosinski M, Dewey JE, Gandek B. How to score and interpret single-item health status measures: a manual for users of the SF-8 Health Survey. Lincoln (RI): Quality Metric Inc.; 2001.
bThree patients from the ECHO study sample did not complete the SF-8 Health Survey.
cThese scores were below the average score of 50 for each of the domains for the general population not living with a chronic illness. Source: Ware JE, Kosinski M, Dewey JE, Gandek B. How to score and interpret single-item health status measures: a manual for users of the SF-8 Health Survey. Lincoln (RI): Quality Metric Inc.; 2001.
dSource: Kressin NR, Jones JA, Orner MB, Spiro A 3rd. A new brief measure of oral quality of life. Prev Chronic Dis 2008;5:A43.
ECHO = Evaluation Center on HIV and Oral Health
SPNS = Special Projects of National Significance
SF-8™ = Short Form 8™
MCS = Mental Component Summary
PCS = Physical Component Summary
HIV = human immunodeficiency virus
Questions related to patient perception of their oral health were also included in the baseline survey using a brief measure of oral health quality of life designed by Kressin et al.22 This model includes six domains: (1) physical function, (2) impairment and disease, (3) role functioning, (4) distress, (5) worry, and (6) denture use. In this study, we used an adapted measure that excluded the worry item. Patients were asked to use a four- or five-point scale to define their experience in the five domains. Two-thirds of the sample reported the health of their teeth and gums as “fair” (30.9%) or poor (32.3%). A third of participants (33.7%) reported they occasionally or fairly often avoided eating food in the past three months and 31.1% occasionally or fairly often found it difficult to relax due to the condition of their teeth and gums. When asked about distress related to teeth/gum pain, 43.7% reported a little or some distress and an additional 19.9% reported quite a bit or a great deal of distress. The majority of participants (76.8%) reported that problems with their teeth and gums did not impact their ability to take any medications, while an additional 20.3% reported not taking any medications (Table 2).
When asked about practices that affect oral health, 82.1% reported brushing daily in the past 30 days, 18.7% reported flossing daily in the past 30 days, 28.1% ate sugary candy or chewed gum with sugar 15 or more times in the past 30 days, and 41.9% drank soda with sugar 15 or more times in the past 30 days (data not shown).
DISCUSSION
The Oral Health Initiative provides valuable data about access to oral health care from the largest sample of PLWHA since the HCSUS. In relation to the IOM theoretical model used to design this evaluation study, these baseline results highlight several of the structural, financial, and personal barriers encountered by the individuals in our sample of HIV-positive patients, as well as their oral health status in the post-cART era. Of the 2,469 study participants, many of whom had been HIV-positive for at least a decade, 48.2% reported a time since testing positive in which they needed dental care but could not get it, with the majority citing inability to pay for oral health care as the main reason they did not get care. In addition, more than a third of the sample reported not having a regular place for dental care and more than half reported their last dental visit occurred two or more years ago. These results are not so different from those reported by the HCSUS in which 35% of patients reported no usual source of dental care and 40% of the sample needed dental care but was unable to access it in the past six months. One difference is that only 24% of the HCSUS sample had not had a dental visit in two or more years.13,29
For a variety of reasons, PLWHA continue to face limited access to oral health care. Context for these findings can be provided by the 2009 National Health Interview Survey data, which show that 44% of U.S. adults had contact with a dentist in the past six months and an additional 17% in the past 12 months. Only 26% of the adult general population had not seen a dentist in two or more years.30 The two most influential factors limiting access to care in the current study appear to be a lack of dental coverage through either private insurance or public funding and the inability to pay for oral health care. A majority of the sample lives in poverty and is unemployed. Findings indicate that the majority of patients had no dental coverage and of those with dental coverage, 27.7% reported coverage through Medicaid, although adult dental coverage through Medicaid varies by state. For those patients who reported Medicaid as dental coverage, 20.9% resided in a state that had no adult dental Medicaid coverage or only provided emergency dental services through Medicaid.
The 2,469 HIV-positive adults enrolled in the study were largely engaged in medical care and taking antiretroviral medications, and the majority reported a visit with their HIV provider in the six months prior to their initial study interview. Almost two-thirds rated their oral health as “fair” or “poor” while rating their overall health as “good” or “excellent” (94.2%). It is interesting to note that some study patients appeared to discount their oral health status when rating their overall health. There is clearly a disconnect between how patients view their oral health status in relation to their overall health. Past oral health symptoms such as tooth decay and sensitivity were reported by half of the sample. This is a vulnerable patient population, yet these individuals had not accessed oral health care in the past year or longer.
Through the Oral Health Initiative, two primary reported barriers to care for PLWHA—lack of dental coverage and the inability to pay for oral health care—were mitigated as a result of the HRSA SPNS funding. The Oral Health Initiative enabled sites to enroll PLWHA into their programs to receive free oral health care. However, minimizing that barrier did not create an instant demand for oral health care. The funded sites had to rely on their innovative programs and staff to actively recruit PLWHA into care. These efforts included the incorporation of dental case managers at several sites to engage patients in care and provide personalized support to get patients to appointments. Four sites used mobile dental units to take oral health-care services to locations more convenient to PLWHA. And all sites reported building relationships with staff, clinicians, and case managers at local infectious disease clinics, Community Health Centers, and AIDS service organizations to assist them in educating and informing patients about the importance of oral health care in relation to HIV infection, as well as to make referrals into the oral health-care programs.
Limitations
Several study limitations should be noted. This was a cross-sectional study of data collected from a convenience sample of HIV-positive patients enrolling in oral health care at 15 HIV dental clinics. Sites varied by geographic location, type of dental program, level of dental care provided, and patient recruitment methods. Although the results of this study are not generalizable to HIV-positive individuals nationally, the geographic diversity of this sizable sample affirms the utility of results. An additional limitation was that the sample comprised people who had not seen a dentist in the preceding year; thus, the results may be more relevant to those who have delayed or never accessed care compared with those who have been receiving oral health care. These data were collected using an interview instrument that was created through a participatory process. Elements of the survey, such as the SF-8 and the oral health quality-of-life measures, have been tested for reliability and validity; however, such testing was not the case for the entire survey. Finally, these data were based on self-report rather than dental examination. Sites did not collect a clinical assessment of symptoms, dentition, and the patient treatment plan.
CONCLUSIONS
Having a usual source of oral health care or “dental home” is an important predictor of use of dental services.31 Many HCSUS authors argued that the findings of the HCSUS research, conducted more than 10 years prior to the beginning of this study, would inform the public health, HIV, community health, and oral health professions to better respond to the oral health needs of the HIV population and improve access to services. The baseline results of this study identify a persistent unmet need for oral health care among this sample of PLWHA, a group that had not been engaged in dental care in the previous 12 months or longer. In the face of Medicaid cuts, particularly to adult dental services,32,33 and uncertainty about funding for comprehensive HIV care in relation to health-care reform, it stands to reason that this unmet need for oral health care will continue to grow if left untended.
The availability of health care, inclusive of oral health care, is fundamental for the attainment of general health; for vulnerable populations such as PLWHA, this care is especially a priority.34 It is the collective responsibility of HIV care providers and the research community, as well as the public health dental community, to continue to support innovative models for increasing access to oral health care for HIV-positive patients—models that not only offer high-quality comprehensive oral health care, but also address the barriers to accessing oral health care identified in this article and in past studies. Comprehensive adult oral health care is a core component of quality HIV care and requires continued attention and funding from state and federal governments through Medicaid, the Ryan White HIV/AIDS Program,35 and Community Health Center programming.
The results presented in this article are from data collected at baseline interviews. This study was part of a larger longitudinal study, which also included collection of follow-up interview data and patient dental utilization data. Additional analyses will focus on findings related to the other domains of the IOM model, such as patient longitudinal changes and outcomes, as well as the types of oral health services provided. Future results will provide new insights into the implications for providing access to comprehensive oral health care to HIV patients as well as other vulnerable populations.
Footnotes
This study was supported by grant #H97HA07519 from the U.S. Department of Health and Human Services, Health Resources and Services Administration (HRSA). This grant is funded through the HRSA HIV/AIDS Bureau's Special Projects of National Significance program. The contents of this article are solely the responsibility of the authors and do not necessarily represent the views of the funding agencies or the U.S. government.
This multisite research project was approved by the Institutional Review Board (IRB) of the Boston University Medical Campus 2006–2011. The study was also approved by the following participating sites' IRBs: AIDS Care Group—Western IRB; AIDS Resource Center of Wisconsin—Human Research Review Committee with the Medical College of Wisconsin; Community Health Center, Inc.—Chesapeake Research Review, Inc.; Harbor Health—University of Massachusetts Medical School Committee for the Protection of Human Subjects in Research; HIV Alliance—Western IRB; Louisiana State University—Louisiana State University Health Sciences Center IRB; Lutheran Medical Center—Lutheran Medical Center Health System IRB; Montefiore Medical Center—Montefiore Medical Center IRB; Native American Health Center—Independent Review Consulting Inc.; Sandhills Medical Center—University of South Carolina IRB; Special Health Resources for Texas—Liberty IRB, Inc.; St. Luke's-Roosevelt Hospital Center—St. Luke's-Roosevelt Hospital Center, Institute for Health Sciences IRB; Tenderloin Health Center—Independent Review Consulting, Inc.; University of Miami—University of Miami, Social and Behavioral IRB; and University of North Carolina—University of North Carolina at Chapel Hill Biomedical IRB.
REFERENCES
- 1.HIV surveillance—United States, 1981–2008 [published erratum appears in MMWR Morb Mortal Wkly Rep 2011;60(25):852] MMWR Morb Mortal Wkly Rep. 2011;60(21):689–93. [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention (US). CDC fact sheet: estimates of new HIV infections in the United States, 2006–2009. [[cited 2012 Jan 5]]. Available from: URL: http://www.cdc.gov/nchhstp/newsroom/docs/HIV-Infections-2006-2009.pdf.
- 3.Broder S. The development of antiretroviral therapy and its impact on the HIV-1/AIDS pandemic. Antiviral Res. 2010;85:1–18. doi: 10.1016/j.antiviral.2009.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tobias C. Oral health care: the forgotten need for HIV-positive populations in the continuum of care. Presented at the American Public Health Association Annual Meeting; 2007 Nov 7; Washington, DC. [Google Scholar]
- 5.Kenagy GP, Linsk NL, Bruce D, Warnecke R, Gordon A, Wagaw F, et al. Service utilization, service barriers, and gender among HIV-positive consumers in primary care. AIDS Patient Care STDS. 2003;17:235–44. doi: 10.1089/108729103321655881. [DOI] [PubMed] [Google Scholar]
- 6.Department of Health and Human Services (US), Office of the Surgeon General. Oral health in America: a report of the Surgeon General. May 2000. [[cited 2010 Nov 23]]. Available from: URL: http://www.surgeongeneral.gov/library/oralhealth.
- 7.Weinert M, Grimes RM, Lynch DP. Oral manifestations of HIV infection. Ann Intern Med. 1996;125:485–96. doi: 10.7326/0003-4819-125-6-199609150-00010. [DOI] [PubMed] [Google Scholar]
- 8.McCarthy GM. Host factors associated with HIV-related oral candidiasis. A review. Oral Surg Oral Med Oral Pathol. 1992;73:181–6. doi: 10.1016/0030-4220(92)90192-s. [DOI] [PubMed] [Google Scholar]
- 9.Diz Dios P, Ocampo A, Miralles C, Limores J, Tomás I. Changing prevalence of human immunodeficiency virus-associated oral lesions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:403–4. doi: 10.1067/moe.2000.110030. [DOI] [PubMed] [Google Scholar]
- 10.Tappuni A, Fleming G. The effect of antiretroviral therapy on the prevalence of oral manifestation in HIV-infected patients: a UK study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:623–8. doi: 10.1067/moe.2001.118902. [DOI] [PubMed] [Google Scholar]
- 11.Patton LL, McKaig R, Strauss R, Rogers D, Eron JJ., Jr. Changing prevalence of oral manifestations of human immunodeficiency virus in the era of protease inhibitor therapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:299–304. doi: 10.1016/s1079-2104(00)70092-8. [DOI] [PubMed] [Google Scholar]
- 12.Reznik DA. Oral manifestations of HIV disease. Top HIV Med. 2005-2006;13:143–8. [PubMed] [Google Scholar]
- 13.Marcus M, Maida CA, Coulter ID, Freed JR, Der-Martirosian C, Liu H, et al. A longitudinal analysis of unmet need for oral treatment in a national sample of medical HIV patients. Am J Public Health. 2005;95:73–5. doi: 10.2105/AJPH.2003.025403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marx R, Katz MH, Park MS, Gurley RJ. Meeting the service needs of HIV-infected persons: is the Ryan White CARE Act succeeding? J Acquir Immune Defic Syndr Hum Retrovirol. 1997;14:44–55. doi: 10.1097/00042560-199701010-00008. [DOI] [PubMed] [Google Scholar]
- 15.Capilouto EI, Piette J, White BA, Fleishman J. Perceived need of dental care among persons living with acquired immunodeficiency syndrome. Med Care. 1991;29:745–54. doi: 10.1097/00005650-199108000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Fleishman JA, Schneider DA, Garcia I, Hardwick K. Dental service use among adults with human immunodeficiency virus infection. Med Care. 1997;35:77–85. doi: 10.1097/00005650-199701000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Shiboski CH, Palacio H, Neuhaus JM, Greenblatt RM. Dental care access and use among HIV-infected women. Am J Public Health. 1999;89:834–9. doi: 10.2105/ajph.89.6.834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Heslin KC, Cunningham WE, Marcus M, Coulter I, Freed J, Der-Martirosian C, et al. A comparison of unmet needs for dental and medical care among persons with HIV infection receiving care in the United States. J Public Health Dent. 2001;61:14–21. doi: 10.1111/j.1752-7325.2001.tb03350.x. [DOI] [PubMed] [Google Scholar]
- 19.Department of Health and Human Services, Health Resources and Services Administration (US). Rockville (MD): HHS, HRSA; 2006. Bureau HA, editor. Special Projects of National Significance (SPNS): Innovations in Oral Health Care Initiative: (1) demonstration models and (2) evaluation and support center. [Google Scholar]
- 20.Institute of Medicine. Washington: National Academy Press; 1993. Millman M, editor. Access to health care in America. [PubMed] [Google Scholar]
- 21.Ware JE, Kosinski M, Dewey JE, Gandek B. Lincoln (RI): Quality Metric, Inc.; 2001. How to score and interpret single-item health status measures: a manual for users of the SF-8 Health Survey. [Google Scholar]
- 22.Kressin NR, Jones JA, Orner MB, Spiro A., 3rd A new brief measure of oral quality of life. Prev Chronic Dis. 2008;5:A43. [PMC free article] [PubMed] [Google Scholar]
- 23.Health Resources and Services Administration (US), HIV/AIDS Bureau. HAB HIV performance measures: oral health. [[cited 2010 Dec 13]]. Available from: URL: http://hab.hrsa.gov/deliverhivaidscare/habperformmeasures.html.
- 24.SPSS, Inc. SPSS®: Version 16.0. Chicago: SPSS, Inc.; 2008. [Google Scholar]
- 25.Yin RK. Case study research: design and methods. 4th ed. Thousand Oaks (CA): Sage Publications, Inc.; 2009. [Google Scholar]
- 26.Rajabiun S, Bachman SS, Fox JE, Tobias C, Bednarsh H. A typology of models for expanding access to oral health care for people living with HIV/AIDS. J Public Health Dent. 2011;71:212–9. [PubMed] [Google Scholar]
- 27.Department of Health and Human Services (US). AIDS.gov: understand your test results: CD4 count. [[cited 2010 Dec 13]]. Available from: URL: http://aids.gov/hiv-aids-basics/diagnosed-with-hiv-aids/understand-your-test-results/cd4-count.
- 28.Henry J. Kaiser Family Foundation. Medicaid benefits: online database. Benefits by service: dental services (October 2006) [[cited 2010 Dec 13]]. Available from: URL: http://medicaidbenefits.kff.org/service.jsp?yr=3&cat=6&nt=on&sv=6&so=0&tg=0.
- 29.Freed JR, Marcus M, Freed BA, Der-Martirosian C, Maida CA, Younai FS, et al. Oral health findings for HIV-infected adult medical patients from the HIV Cost and Services Utilization Study [published erratum appears in J Am Dent Assoc 2006;137:156] J Am Dent Assoc. 2005;136:1396–405. doi: 10.14219/jada.archive.2005.0053. [DOI] [PubMed] [Google Scholar]
- 30.Pleis JR, Ward BW, Lucas JW. Summary of health statistics for U.S. adults: National Health Interview Survey, 2009. Vital Health Stat 10 2010(249) [PubMed] [Google Scholar]
- 31.Davidson PL, Cunningham WE, Nakazono TT, Anderson RM. Evaluating the effect of usual source of dental care on access to dental services: comparisons among diverse populations. Med Care Res Rev. 1999;56:74–93. doi: 10.1177/107755879905600105. [DOI] [PubMed] [Google Scholar]
- 32.Henry J. Kaiser Family Foundation, Kaiser Commission on Medicaid and the Uninsured. Hoping for economic recovery, preparing for health reform: a look at Medicaid spending, coverage and policy trends. [[cited 2010 Dec 13]]. Available from: URL: http://www.kff.org/medicaid/8105.cfm.
- 33.Brown LJ, Wall TP, Manski RJ. The funding of dental services among U.S. adults aged 18 years and older: recent trends in expenditures and sources of funding. J Am Dent Assoc. 2002;133:627–35. doi: 10.14219/jada.archive.2002.0238. [DOI] [PubMed] [Google Scholar]
- 34.American Dental Education Association. ADEA policy statement on health care reform: oral health care: essential to health care reform. J Dent Educ. 2009;73:856–9. [Google Scholar]
- 35.Health Resources and Services Administration (US). Ryan White HIV/AIDS Program. [[cited 2010 Nov 23]]. Available from: URL: http://hab.hrsa.gov/abouthab/aboutprogram.html.