Abstract
Objectives
We analyzed the characteristics of people living with HIV/AIDS (PLWHA) who reported unmet oral health needs since testing positive and compared those characteristics with people reporting no unmet health needs. We also identified barriers to accessing oral health care for PLWHA.
Methods
We collected data from 2,469 HIV-positive patients who had not received oral health care in the previous 12 months and who had accessed care at Health Resources and Service Administration-funded Special Projects of National Significance Innovations in Oral Health Care Initiative demonstration sites. The outcome of interest was prior unmet oral health needs. We explore barriers to receiving oral health care, including cost, access, logistics, and personal factors. Bivariate tests of significance and generalized estimating equations were used in analyses.
Results
Nearly half of the study participants reported unmet dental care needs since their HIV diagnosis. People reporting unmet needs were more likely to be non-Hispanic white, U.S.-born, and HIV-positive for more than one year, and to have ever used crack cocaine or crystal methamphetamine. The top three reported barriers to oral care were cost, access to dental care, and fear of dental care. Additional reported barriers were indifference to dental care and logistical issues.
Conclusion
Innovative strategies are needed to increase access to and retention in oral health care for PLWHA. Key areas for action include developing strategies to reduce costs, increase access, and reduce personal barriers to receiving dental care, particularly considering the impact of poor oral health in this population.
Oral health status affects a person's general health and overall well-being throughout the life cycle. This impact is particularly important in vulnerable populations, such as people living with human immunodeficiency virus (HIV) and acquired immunodeficiency syndrome (AIDS) (PLWHA).1 Vulnerable populations experience greater barriers to accessing oral health care because of a lack of coverage or inability to pay for dental care, as well as a lack of awareness regarding the importance of oral health care. This lack of access, coupled with physical and psychosocial health problems, can lead to a greater oral health disease burden.1 More than a decade ago, the unmet need for oral health care in the general U.S. population was estimated at 8.5%; however, for households whose income was ≤150% of the federal poverty level, the need was 16.4%, and more than 22% of uninsured people reported oral health-care needs.2 Data published more recently, from the 2009 National Health Interview Survey, indicated 26% of U.S. adults had not seen a dentist in two or more years. In addition, only 33% of adults aged 65 years or younger with Medicaid coverage and 18% of adults who were uninsured reported a dental visit in the prior six months.3 However, it should be noted that oral health service utilization could be affected by numerous additional factors, such as the low number of states with comprehensive (not just emergency) adult dental care covered by Medicaid and the minimal advertisement of adult dental care coverage as part of the Medicaid program in some states; the potential lack of knowledge regarding the need for dental care; and basic problems of inaccessibility, such as finding a Medicaid dentist, getting an appointment, and finding a dentist with whom they are comfortable or whom they believe can provide care in a nondiscriminatory manner.4–6
The deleterious impact of oral health care is of particular importance among PLWHA.7–11 Complications of oral health problems associated with HIV are well documented in the literature.12–16 Oral manifestations, such as oral ulcers, dental caries, salivary gland disease, oral warts, Kaposi's sarcoma, necrotizing ulcerative periodontitis, oral hairy leukoplakia, and candidiasis, can be strongly associated with HIV infections and may be present in up to 50% of people with HIV infection and up to 80% of people diagnosed with AIDS.12,13 PLWHA are more likely to experience oral health problems compared with non-HIV-infected people.13–16 Once oral health is compromised, PLWHA may experience difficulty in maintaining salivary flow, which can affect chewing, swallowing, and tasting foods, and, ultimately, their ability to take HIV medications and maintain an optimal quality of life.14
The HIV Cost and Services Utilization Study (HCSUS), conducted more than a decade ago, examined dental care use among a nationally representative sample of PLWHA engaged in medical care; 35% of patients reported no usual source of dental care, and 40% needed dental care but were unable to access it in the past six months. The unmet need for dental care was twice as prevalent as the unmet need for medical care in this study. In addition, the HCSUS found that 24% of the sample had not had a dental visit in two or more years.4,5 The reported unmet need for dental services among PLWHA is frequently related to a lack of dental coverage, either through private dental insurance or state Medicaid programs, and an inability to pay out-of-pocket for care.9,10
Since the HCSUS, no data have been published on the unmet oral health needs of PLWHA in the U.S. The data reported in this article are from an evaluation study that was designed using the Institute of Medicine's (IOM's) conceptual model of access to personal health-care services.11 The IOM model suggests that access to care is shaped by structural barriers, including availability of services or transportation; financial barriers, such as insurance coverage or reimbursement; and personal barriers, such as culture, language, and education. Use of services is further mediated by efficacy of treatment, quality of providers, and patient adherence, leading to improvements in patient outcomes, such as health status and reduction in patients' unmet needs.11
This article analyzes the characteristics of PLWHA reporting unmet oral health needs since testing positive from a sample of 2,469 HIV patients accessing oral health care from 15 demonstration sites. The sites were funded through the Health Resources and Services Administration HIV/AIDS Bureau's Special Projects of National Significance Innovations in Oral Health Care Initiative (hereafter, Oral Health Initiative), which is aimed at increasing access to oral health care for PLWHA.
METHODS
Study participants (n=2,469) were recruited from 15 distinct oral health programs in 12 states and one U.S. territory. The sites were located in San Francisco, California (two sites); Norwalk, Connecticut; Miami, Florida; New Orleans, Louisiana; Provincetown, Massachusetts; Chapel Hill, North Carolina; New York, New York (two sites); Eugene, Oregon; Chester, Pennsylvania; Jefferson, South Carolina; Tyler, Texas; St. Croix, U.S. Virgin Islands; and Green Bay, Wisconsin. The oral health programs were located in universities, hospitals, Community Health Centers, and AIDS service organizations. Approval was obtained from the Institutional Review Boards at each participating site and the Evaluation Center for HIV and Oral Health at Boston University; the multisite center maintained human subjects approval for the overall and individual studies.
Oral health program innovations included funding for additional dental chairs at underserved clinics, vans that could bring people to care in rural areas where dental care was not available locally, vans that transported portable dental care equipment to remote areas where dental equipment was not available, and mobile dental clinics providing care. Each site recruited and enrolled adult HIV-positive patients who had not received dental care, with the exception of emergency care, in the previous 12 months. PLWHA were referred to oral health programs by case managers serving PLWHA, social-service organizations providing care to PLWHA, HIV clinic managers, and other study participants. Once enrolled, participants were followed for up to 24 months. For the analyses in this article, we only use data collected as part of the baseline assessment.
Data collection
The baseline interview collected data on sociodemographic characteristics; mode of HIV transmission; past substance, tobacco, and alcohol use; barriers to accessing oral health care since testing HIV-positive; and oral health-care habits. The interview also included standardized measures, including the SF-8™ Health Survey,17 to measure health-related quality of life, and a brief oral health quality-of-life scale.18 Interviews were conducted in both English and Spanish, and all participants gave informed consent to participate. Baseline data collection occurred from May 2007 to August 2009. Interviewers at each site participated in a standardized training module conducted by the multisite evaluation staff. Data from all 15 sites were entered into a Web-based database hosted by the multisite coordinating center, where the data were then cleaned and merged into a single multisite database.
Measures
The outcome of significance for the current analysis was perceived unmet oral health-care needs since testing positive for HIV. Specifically, participants were asked, “Since you tested positive for HIV, was there a time when you needed dental treatment but did not get it?” For those participants who answered “yes,” the follow-up question asked was, “What was the most important reason you did not get the dental care you needed?” Responses were grouped into the following barrier-related categories for the purpose of this analysis: cost (e.g., could not afford it or had no insurance), access to dental care (e.g., did not know where to find a dentist or could not get an appointment), logistical issues (e.g., did not have transportation or had competing responsibilities), indifference to dental care, and fear of dental care.
The independent variables used in this analysis were age, gender, education (<high school, high school degree, or >high school), race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, or other for participants self-reporting belonging to a race/ethnicity other than the three predefined categories), birth location, years since HIV diagnosis, and lifetime illicit drug use (crack cocaine or crystal methamphetamine [meth]).
Analysis
Frequencies and percentages of independent variables by each dependent variable, unstratified by site, are shown in Table 1, with a Chi-square statistic for association and an effect size measure, Cramer's V. For multivariable analyses, we used generalized estimating equation (GEE) modeling methods with a logit link. Because the multisite study had various modalities of intervention delivery, we clustered by site in the multivariable GEE models to adjust for potential site differences.
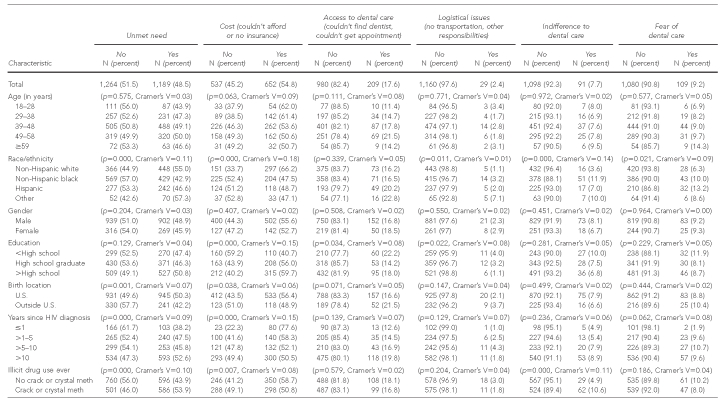
Table 1.
Unclustered bivariable associations between demographic characteristics and unmet need, and reasons for unmet need: Health Resources and Services Administration HIV/AIDS Bureau's Special Projects of National Significance Oral Health Initiative, 2006–2009 (n=2,469)
HIV = human immunodeficiency virus
AIDS = acquired immunodeficiency syndrome
crack = crack cocaine
meth = methamphetamine
RESULTS
The sample was largely male (77.0%), born in the U.S. or a U.S. territory (81.8%), and spoke English as their primary language (85.4%). A majority of the sample had completed either high school (31.8%) or education beyond high school (45.1%) (data not shown).
Unmet need
Nearly half of study participants (48.5%) reported unmet dental care needs (Table 1). Unmet needs were reported by 55.0% of non-Hispanic white participants, 42.9% of non-Hispanic black participants, and 46.6% of Hispanic participants. Participants who had used illicit drugs were much more likely to report unmet needs than nonusers (53.9% of crack/crystal meth users vs. 43.9% of nonusers). Reported reasons for unmet needs included cost (54.8%), access to dental care (17.6%), logistical issues (2.4%), indifference to dental care (7.7%), and fear of dental care (9.2%).
Characteristics of those reporting barriers
Multivariable regression results are presented in Table 2. Non-Hispanic black participants had nearly 30% lower adjusted odds (adjusted odds ratio [AOR] = 0.701; 95% confidence interval [CI] 0.567, 0.868) of reporting an unmet dental care need since testing HIV-positive than non-Hispanic white participants. Similarly, participants born outside of the U.S. had 27% lower adjusted odds (AOR=0.728; 95% CI 0.618, 0.857) of reporting unmet dental care needs than U.S.-born participants. Each additional year of having been diagnosed with HIV was positively associated with a 1.5% increase in unmet dental care needs (AOR=1.015; 95% CI 1.004, 1.027). History of illicit drug use was also positively associated with report of unmet dental care needs (AOR=1.265; 95% CI 1.077, 1.487).
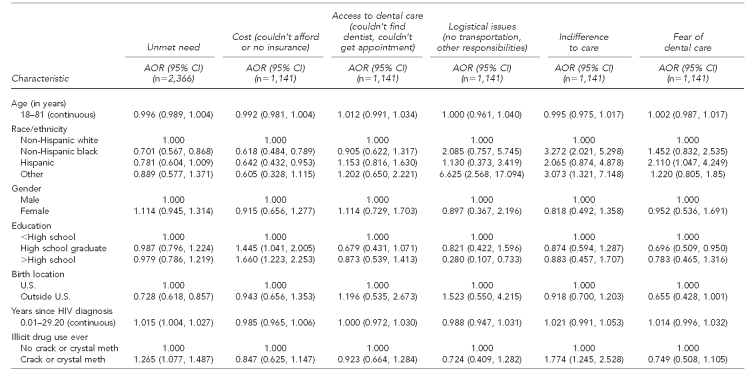
Table 2.
Clustered multivariable generalized estimating equation of unmet need and reasons for unmet need: Health Resources and Services Administration HIV/AIDS Bureau's Special Projects of National Significance Oral Health Initiative, 2006–2009 (n=2,469)
HIV = human immunodeficiency virus
AIDS = acquired immunodeficiency syndrome
AOR = adjusted odds ratio
CI = confidence interval
crack = crack cocaine
meth = methamphetamine
Non-Hispanic black participants had 38% lower adjusted odds (AOR=0.618; 95% CI 0.484, 0.789) and Hispanic participants had 36% lower adjusted odds (AOR=0.642; 95% CI 0.432, 0.953) of reporting cost-related barriers to dental care than their non-Hispanic white counterparts. High school graduates (AOR=1.445; 95% CI 1.041, 2.005) and those with >high school education (AOR=1.660; 95% CI 1.223, 2.253) had greater adjusted odds of reporting cost-related barriers to dental care than those who did not complete high school. No independent variables were significantly associated with the dependent variable of access-related barriers to dental care. Other race/ethnicity was significantly positively associated with logistical barriers to dental care (AOR=6.625; 95% CI 2.568, 17.094) compared with non-Hispanic white race/ethnicity.
Participants with >high school education had a 72% greater negative association (AOR=0.280; 95% CI 0.107, 0.733) with logistical barriers to dental care than those with <high school education. Non-Hispanic black participants (AOR=3.272; 95% CI 2.021, 5.298) and participants reporting other race/ethnicity (AOR=3.073; 95% CI 1.321, 7.148) had much greater adjusted odds of reporting indifference to dental care as a reason for their unmet need than their non-Hispanic white counterparts. Participants reporting a history of illicit drug use (crack cocaine or crystal meth) had higher statistically significant adjusted odds (AOR=1.774; 95% CI 1.245, 2.528) of reporting indifference to care as a reason for their unmet need than nonusers.
Hispanic participants had more than two times the adjusted odds (AOR=2.110; 95% CI 1.047, 4.249) of reporting fear of dental care as a reason for unmet needs than their non-Hispanic white counterparts. High school graduates (AOR=0.696; 95% CI 0.509, 0.950) and participants with >high school education (AOR=0.783; 95% CI 0.465, 1.316) were less likely to report fear of dental care as a reason for unmet need than participants who did not complete high school.
DISCUSSION
This study provided an opportunity to more fully investigate reasons for unmet dental care needs among a large, racially/ethnically diverse group of PLWHA who had not received oral health care for the past year. Study findings demonstrate that nearly half (48.5%) of the HIV-positive patients recruited by the 15 Oral Health Initiative sites reported unmet dental care needs since their HIV diagnosis. In our study, non-Hispanic black participants were less likely than participants of other races/ethnicities to report unmet dental care needs since learning of their HIV-positive status. This finding is counterintuitive to the HCSUS finding that non-Hispanic black PLWHA had significantly higher perceived unmet oral health-care needs than their non-Hispanic white counterparts. In addition, 31% of our study sample reported having no health coverage.19 In contrast, only 19.7% of the HCSUS sample reported no health coverage, suggesting underlying differences in study samples.
Additionally, foreign-born study participants were less likely to report an unmet need for dental care than their U.S.-born counterparts. The literature has shown that being of Latino(a) origin but not born in the U.S. has been protective of oral health-care needs, even when compared with people identifying as Latino(a) and born in the United States.20 Of the Hispanic sample reporting unmet dental needs, only 30% were foreign-born, supporting the previous literature. However, it must be noted that these findings may be indicative of a difference in what is considered unmet need by foreign-born people. Further research is needed to clarify this finding.
The likelihood of an unmet dental care need increased as the number of years since HIV diagnosis increased. It is likely that the longer period of time since HIV diagnosis may increase the chance that people might experience unmet dental care needs.
Participants reporting a history of crack cocaine or crystal meth use reported greater unmet needs; there is well-established literature documenting the impact of crack cocaine and crystal meth use on oral health.21–24
Participants with ≥high school education were more likely to report cost as a barrier. This finding may be because people with <high school education might be more likely to have lower incomes and, therefore, might be eligible for income-based discounted oral health-care benefits. Participants with >high school education were less likely to report logistical barriers to dental care than those with less education. It is plausible that people possessing >high school -education have more resources to address competing life responsibilities, such as work, children, or family, that may prevent them from easily accessing dental care.
Non-Hispanic black participants and those reporting other race/ethnicity, as well as participants with a history of illicit drug use, were more likely to report indifference as a reason for their unmet dental care need. It should be noted that unmet need in the present case is a perceived unmet need. The participant must have desired dental care in the past (for a variety of possible reasons) but then encountered obstacles to obtaining that care. Regarding the desire for care, there must be a perception of need based on prevention concerns, such as preventing caries or loss of teeth, or symptomatic concerns, such as appearance. As such, the perception of unmet need is likely to vary among different individuals, so that what one person considers an unmet need for a specific dental issue may be seen as unimportant to another person.
Despite the deleterious effects that poor oral health can have on general health, unmet dental needs, such as oral infections, mouth ulcers, and other severe dental conditions associated with HIV infections, often go untreated more than twice as often as other health problems related to the disease.25,26 Unmet dental care needs among PLWHA persist despite the availability and accessibility of dental services in many communities that are specifically designated for low-income HIV-positive people and funded through the Ryan White HIV/AIDS Program.24,27 Key areas for action include developing strategies to reduce cost, increase access, and reduce personal (indifference and fear) barriers to receiving dental care, particularly considering the impact of poor oral health in this population.
More than half of the participants reporting an unmet oral health need at some point since being diagnosed as HIV-positive (exact time point is not established) stated that cost was the most important barrier. Given the availability of Ryan White Program funding for dental care services among low-income PLWHA, it is important that each time HIV primary care is accessed, medical personnel (i.e., case managers, nurses, and/or physicians) take the opportunity to reinforce the availability and accessibility of dental care services. Successful community-based models have sought to increase access to care by increasing the number of providers and locations, case management, and linkage to care. Mofidi and Gambrell reported on the impact of the Community-Based Dental Partnership Program, a federal program designed to reduce dental disparities among PLWHA through the education and training of dental students and residents in underserved communities. The number of dental providers who delivered oral health services to PLWHA through the program grew from 766 in 2004 to 1,474 in 2007.26 Additional interventions could include the design and implementation of strategies such as increased attendance at health fairs and community outreach to engage individuals, which could increase awareness of the importance of oral health care and provide a venue to address barriers to oral health care. Dental clinics providing care to PLWHA could shift their working schedules to provide dental services during off times, such as after 5 p.m. or during the weekend, making dental care services available to people who have work conflicts or other competing responsibilities. These innovative models could engage and target special-needs populations in their own communities, especially low-income and marginalized individuals who have greater unmet needs for oral care.
Limitations
Several study limitations should be recognized. First, these data are from a convenience sample of HIV-positive patients recruited from HIV primary care clinics. Enrollment in the study was voluntary and by referral, and may have been vulnerable to selection bias. Additionally, information could not be collected on people who refused to participate in the study, so we do not know if these individuals were significantly different from recruits. Also, these data reflect perceived unmet oral health-care needs, which may be defined differently by each individual being assessed. Finally, the sample comprised people who had not seen a dentist in the past year; while the results reported in this article may not be generalizable to people who receive dental care more frequently, they are relevant to those who have delayed or never accessed care.
CONCLUSION
Despite the availability and accessibility of dental services specifically designated for low-income HIV-positive individuals, unmet dental care needs persist among PLWHA. The identification of barriers to oral health-care services for PLWHA is not only an important component of the overall management of this disease, it will also help inform future interventions, social programs, and public resource allocation. HIV primary care settings, health fairs, and community outreach are opportunities for providers to impress upon their patients the importance of maintaining regular dental care appointments and overall oral health. This study suggests the need for continued, increased focus on reducing unmet oral health-care needs for PLWHA.
Footnotes
This study was supported by grant #H97HA07519 from the U.S. Department of Health and Human Services, Health Resources and Services Administration. This grant is funded through the HIV/AIDS Bureau's Special Projects of National Significance program. The contents of this article are solely the responsibility of the authors and do not necessarily represent the views of the funding agencies or the U.S. government.
The Institutional Review Boards of the Boston University Medical Campus and the University of Miami approved this research study.
REFERENCES
- 1.Department of Health and Human Services (US); Office of the Surgeon General. Oral health in America: a report of the Surgeon General. 2000. May, [cited 2011 Jun 30]. Available from: URL: http://www.surgeongeneral.gov/library/oralhealth.
- 2.Mueller CD, Schur CL, Paramore LC. Access to dental care in the United States. J Am Dent Assoc. 1998;129:429–37. doi: 10.14219/jada.archive.1998.0241. [DOI] [PubMed] [Google Scholar]
- 3.Pleis JR, Lucas JW, Ward BW. Summary health statistics for U.S. adults: National Health Interview Survey, 2008. Vital Health Stat. 2009;10(242) [PubMed] [Google Scholar]
- 4.Schrimshaw EW, Siegel K, Wolfson NH, Mitchell DA, Kunzel C. Insurance-related barriers to accessing dental care among African American adults with oral health symptoms in Harlem, New York City. Am J Public Health. 2011;101:1420–8. doi: 10.2105/AJPH.2010.300076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Okunseri C, Pajewski NM, Jackson S, Szabo A. Wisconsin Medicaid enrollees' recurrent use of emergency departments and physicians' offices for treatment of nontraumatic dental conditions. J Am Dent Assoc. 2011;142:540–50. doi: 10.14219/jada.archive.2011.0224. [DOI] [PubMed] [Google Scholar]
- 6.Quiñonez C, Ieraci L, Guttmann A. Potentially preventable hospital use for dental conditions: implications for expanding dental coverage for low income populations. J Health Care Poor Underserved. 2011;22:1048–58. doi: 10.1353/hpu.2011.0097. [DOI] [PubMed] [Google Scholar]
- 7.Marcus M, Maida CA, Coulter ID, Freed JR, Der-Martirosian C, Liu H, et al. A longitudinal analysis of unmet need for oral treatment in a national sample of medical HIV patients. Am J Public Health. 2005;95:73–5. doi: 10.2105/AJPH.2003.025403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Heslin KC, Cunningham WE, Marcus M, Coulter I, Freed J, Der-Martirosian C, et al. A comparison of unmet needs for dental and medical care among persons with HIV infection receiving care in the United States. J Public Health Dent. 2001;61:14–21. doi: 10.1111/j.1752-7325.2001.tb03350.x. [DOI] [PubMed] [Google Scholar]
- 9.Freed JR, Marcus M, Freed BA, Der-Martirosian C, Maida CA, Yamamoto JM, et al. Oral health findings for HIV-infected adult medical patients from the HIV Cost and Services Utilization Study. J Am Dent Assoc. 2005;136:1396–405. doi: 10.14219/jada.archive.2005.0053. [DOI] [PubMed] [Google Scholar]
- 10.Badner VM. Ensuring the oral health of patients with HIV. J Am Dent Assoc. 2005;136:1415–7. doi: 10.14219/jada.archive.2005.0055. [DOI] [PubMed] [Google Scholar]
- 11.Millman M, editor. Institute of Medicine. Access to health care in America. Washington: National Academy Press; 1993. [PubMed] [Google Scholar]
- 12.Coogan MM, Greenspan J, Challacombe SJ. Oral lesions in infection with human immunodeficiency virus. Bull World Health Organ. 2005;83:700–6. [PMC free article] [PubMed] [Google Scholar]
- 13.Reznik DA. Oral manifestations of HIV disease. Top HIV Med. 2005;13:143–8. [PubMed] [Google Scholar]
- 14.Weinert M, Grimes RM, Lynch DP. Oral manifestations of HIV infection. Ann Intern Med. 1996;125:485–96. doi: 10.7326/0003-4819-125-6-199609150-00010. [DOI] [PubMed] [Google Scholar]
- 15.Patton LL, McKaig R, Strauss R, Rogers D, Eron JJ., Jr Changing prevalence of oral manifestations of human immunodeficiency virus in the era of protease inhibitor therapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:299–304. doi: 10.1016/s1079-2104(00)70092-8. [DOI] [PubMed] [Google Scholar]
- 16.Department of Health and Human Services (US), Health Resources and Services Administration, HIV/AIDS Bureau. Dental programs (part F) [cited 2012 Jan 12]. Available from: URL: http://hab.hrsa.gov/abouthab/partfdental.html.
- 17.Ware JE, Kosinski M, Dewey JE, Gandek B. How to score and interpret single-item health status measures: a manual for users of the SF-8 Health Survey. Lincoln (RI): Quality Metric Inc; 2001. [Google Scholar]
- 18.Kressin NR, Jones JA, Orner MB, Spiro A., 3rd A new brief measure of oral quality of life. Prev Chronic Dis. 2008;5:A43. [PMC free article] [PubMed] [Google Scholar]
- 19.Fox JE, Tobias CR, Bachman SS, Reznik DA, Rajabiun S, Verdecias N. Increasing access to oral health care for people living with HIV/AIDS in the U.S.: baseline evaluation results of the Innovations in Oral Health Care Initiative. Public Health Rep. 2012;127(Suppl 2):5–16. doi: 10.1177/00333549121270S203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sanders AE. A Latino advantage in oral health-related quality of life is modified by nativity status. Soc Sci Med. 2010;71:205–11. doi: 10.1016/j.socscimed.2010.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shetty V, Mooney LJ, Zigler CM, Belin TR, Murphy D, Rawson R. The relationship between methamphetamine and increased dental disease. J Am Dent Assoc. 2010;141:307–18. doi: 10.14219/jada.archive.2010.0165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Curtis EK. Meth mouth: a review of methamphetamine abuse and its oral manifestations. Gen Dent. 2006;54:125–9. [PubMed] [Google Scholar]
- 23.Brand HS, Gonggrijp S, Blanksma CJ. Cocaine and oral health. Br Dent J. 2008;204:365–9. doi: 10.1038/sj.bdj.2008.244. [DOI] [PubMed] [Google Scholar]
- 24.Blanksma CJ, Brand HS. Cocaine abuse: orofacial manifestations and implications for dental treatment. Int Dent J. 2005;55:365–9. doi: 10.1111/j.1875-595x.2005.tb00047.x. [DOI] [PubMed] [Google Scholar]
- 25.Institute of Medicine. Advancing oral health in America. Washington: National Academies Press; 2011. [Google Scholar]
- 26.Mofidi M, Gambrell A. Community-based dental partnerships: improving access to dental care for persons living with HIV/AIDS. J Dent Educ. 2009;73:1247–59. [PubMed] [Google Scholar]
- 27.Health Resources and Services Administration (US) Ryan White HIV/AIDS Program. [cited 2010 Nov 23]. Available from: URL: http://hab.hrsa.gov/abouthab/aboutprogram.html.