Abstract
Objective
We identified factors associated with improved self-reported health status in a sample of people living with HIV/AIDS (PLWHA) following enrollment in oral health care.
Methods
Data were collected from 1,499 enrollees in the Health Resources and Services Administration HIV/AIDS Bureau's Special Projects of National Significance Innovations in Oral Health Care Initiative. Data were gathered from 2007–2010 through in-person interviews at 14 sites; self-reported health status was measured using the SF-8™ Health Survey's physical and mental health summary scores. Utilization records of oral health-care services provided to enrollees were also obtained. Data were analyzed using general estimating equation linear regression.
Results
Between baseline and follow-up, we found that physical health status improved marginally while mental health status improved to a greater degree. For change in physical health status, a decrease in oral health problems and lack of health insurance were significantly associated with improved health status. Improved mental health status was associated with a decrease in oral health problems at the last available visit and no pain or distress in one's teeth or gums at the last available visit.
Conclusion
For low-income PLWHA, engagement in a program to increase access to oral health care was associated with improvement in overall well-being as measured by change in the SF-8 Health Survey. These results contribute to the knowledge base about using the SF-8 to assess the impact of clinical interventions. For public health practitioners working with PLWHA, findings suggest that access to oral health care can help promote well-being for this vulnerable population.
Studies suggest that the widely used standardized measure of health status developed through the Medical Outcomes Study, the Short Form (SF), is a reliable and valid measure of health status for diverse groups of people infected with the human immunodeficiency virus (HIV).1–6 A range of factors has been shown to be associated with health status for people who are HIV-positive.3,4 For example, lower mental health status has been associated with depression and drug use, while lower physical health status has been associated with older age, lower socioeconomic status, and more advanced disease stage.7 Abstinence from alcohol and drugs has also been shown to be associated with better physical heath, better mental health, and lower levels of depression among individuals who are HIV-positive.8
The SF has also been used to examine the association between self-reported health status and factors associated with the state of an individual's HIV disease.9 Results suggest an inverse relationship between HIV symptoms and well-being.10 Studies have also found a relationship between health status and engagement in care or interruption of antiretroviral therapy.7,9,11
Other studies suggest that the SF may lack sensitivity to the health status of individuals who are HIV-positive, especially for people who are asymptomatic,12 and that it is difficult to predict causality with respect to health status.9 Self-reported health status has been shown to explain little variance in disease outcomes13 and to be mediated by health literacy.14 The great diversity of functional status among individuals who are HIV-positive may indicate that a global health status measure does not adequately capture individual health status variation.15
Although the Surgeon General's 2000 report Oral Health in America16 called for greater awareness of the connection between oral health and systemic health, research about the impact of access to oral health care on health status among people living with HIV/AIDS (PLWHA) has been limited. Results of the nationally representative HIV Cost and Services Utilization Study (HCSUS) suggested that PLWHA receive regular medical care but not the dental care they need.17 More recently, an Institute of Medicine (IOM) report, “Advancing Oral Health in America,” continued to call for greater awareness and understanding of the connection between oral health and health outcomes.18 We found one study that suggested that dental care had no significant impact on self-reported health status among a sample of 376 PLWHA.19
The purpose of this article is to respond to national calls for greater awareness of the connection between overall health and oral health by examining the impact of access to oral health care on self-reported health status, as measured by the SF-8™ Health Survey6 (SF-8), in a larger sample of PLWHA. This article examines longitudinal data from the Health Resources and Services Administration HIV/AIDS Bureau's Special Projects of National Significance Innovations in Oral Health Care Initiative (hereafter, Oral Health Initiative), a multisite study through which PLWHA who had not received any dental care in the past year were provided comprehensive oral health care. The Oral Health Initiative's evaluation design is grounded in the IOM's conceptual model of access to personal health-care services,20 in which access to care is shaped by structural barriers, such as availability of services; financial barriers, such as insurance coverage; and personal barriers, such as education. Use of services is further conceptualized as being mediated by efficacy of treatment, quality of providers, and patient adherence to health-care treatment. Improved patient outcomes in domains such as health status and quality of life will result from improved access. The overall study design is further informed by the IOM's health disparities conceptual model, which identifies differences in health-care use and health status, system-oriented disparities in care, and discrimination as factors leading to unequal use of health care and inequity of health services.21
METHODS
Study design, eligibility, and recruitment
Data for this analysis were from a convenience sample of 1,499 PLWHA who received care at one of 14 Oral Health Initiative sites. A 15th study site also participated, but complete data were not available from this site; thus, associated study subjects were excluded from this analysis. The programs implemented different models of care and were located in a range of care settings. Sites recruited patients for the study through consumer outreach, collaboration with HIV case managers, and referrals from HIV clinics. Almost all patients were low income, with more than 90% reporting an income of less than $1,700 per month.
Participants were eligible for the study if they were 18 years of age or older, had already tested positive for HIV, and had not received oral health care outside of emergency care to relieve pain and infection for at least 12 months. Sites screened available patients with these eligibility criteria; patients then participated in a baseline interview and received the first oral health-care visit within the next 45 days. Participants were followed for up to 24 months after study enrollment.
Data collection
Data were gathered from two sources. First, structured interviews were conducted in English or Spanish with enrolled patients at baseline and every six months following baseline, from the study inception in May 2007 to the completion of the study's data-gathering phase in August 2010. Baseline face-to-face interviews were conducted on a rolling basis as patients enrolled in the study until the final enrollment date of August 31, 2009. Follow-up interviews were conducted until August 31, 2010, a time frame that allowed for 12 months of study enrollment for all participants. Follow-up interviews were conducted every six months, either in person if the patient was coming in for care or by telephone if a face-to-face interview could not be arranged. Interviewers at each site participated in standardized training provided by a multisite coordinating center.
The survey instrument was developed through a participatory process with representatives of all sites and comprised items from standardized measures including the SF-8 to measure health status. This participatory process led to the decision to use the SF-8 rather than the more comprehensive SF-36.22 Interviewers at the local level preferred to have a more concise measure of health status to promote gathering of complete data. The SF-8 asks the respondent to assess his or her health status within the last four weeks by responding to the following eight questions:6
Overall, how would you rate your health during the past four weeks? (six-point response scale from “excellent” to “very poor”)
During the past four weeks, how much did physical health problems limit your usual physical activities such as walking or climbing stairs?(five-point response scale from “not at all” to “could not do physical activities”)
During the past four weeks, how much difficulty did you have doing your daily work, both at home and away from home, because of your physical health? (five-point response scale from “none at all” to “could not do daily work”)
How much bodily pain have you had during the past four weeks? (six-point response scale from “none” to “very severe”)
During the past four weeks, how much energy did you have? (five-point response scale from “very much” to “none”)
During the past four weeks, how much did your physical health or emotional problems limit your usual social activities with family or friends? (five-point response scale from “not at all” to “could not do social activities”)
During the past four weeks, how much have you been bothered by emotional problems (such as feeling anxious, depressed, or irritable)? (five-point response scale from “not at all” to “extremely”)
During the past four weeks, how much did personal or emotional problems keep you from doing your usual work, school, or other daily activities? (five-point response scale from “not at all” to “could not do daily activities”)
Other data gathered included sociodemographic characteristics, likely HIV transmission route, barriers to accessing oral health care since testing HIV-positive, substance use, dental problems, and oral health-care habits. Feedback from instrument pretesting resulted in slight modifications to selected items to increase clarity. We then gathered longitudinal dental services utilization data, including source of dental coverage, visit type, whether the treatment plan was completed at the visit, and Current Dental Terminology (CDT) codes of services provided at the visit. Dental care providers entered dental services utilization data into a Web-based data-entry system at the point of service or shortly thereafter drawing from dental chart records. All CDT codes were counted. Data quality was affirmed by retrospective chart audits of a randomly selected sample of patient charts.
All sites, including the multisite coordinating center, obtained approval from their Institutional Review Boards to participate in the multisite study; participants signed informed consent forms. Data were entered into a central Web-based data-entry system for storage, cleaning, and file preparation. For the analysis presented in this article, we used complete data for 1,499 study participants who had a baseline and at least one follow-up administration of the study survey. Both the physical and mental health status SF summary scores were used as dependent variables.
Statistical analysis
Study variables were selected with conceptual guidance from the extant literature in which the SF was used to measure health status among PLWHA. We then categorized variables into structural, financial, and personal domains of the IOM's conceptual model. We used linear regression modeling techniques (using generalized estimating equations [GEEs] to account for within-site correlation of the data) to explore whether there was an association between the change in health status and (1) structural barriers (availability and organizational structure of health services), (2) financial barriers (insurance coverage and public support), and (3) personal barriers (age, gender, and education/income).
In addition, analyses included potential confounders such as smoking, alcohol and drug use, CD4 cell count and viral load measures, oral pain, number of dental problems, length of enrollment in the study, and number of oral health-care services provided during the study. Bivariate GEE analyses were used as a data-reduction technique and tested the association between each independent variable and both the physical health summary SF score and the mental health summary SF score. Independent variables that were significantly associated (p≤0.05) with each dependent variable were included in the final GEE multivariate regression model for that dependent variable. Data were analyzed using SPSS®/PASW® version 18.0.23
Dependent variables.
We used changes in SF-8 physical and mental health summary scores as the dependent variables. To compute these variables, we first derived continuous summary SF-8 scores at baseline and follow-up using responses to the questions described previously. We then computed changes in self-reported physical and mental health status between the baseline and last available visit. We calculated and normed the scores according to standardized methods that have been described and validated previously.6
Independent variables.
Independent variables were derived from personal, structural, and financial domains of the IOM model. Personal barriers were conceptualized as age, gender, and education. Age was measured as a continuous variable calculated from the self-reported year of birth. Gender was coded as male (1), female (0), and transgender. Due to the small number of transgender responses (n=20), this category was not included in the analysis. Education was measured with a dichotomous variable of $high school diploma (1) and <high school diploma (0). Health status was measured by the change in SF-8 from baseline to last available visit as well as most recently available CD4 cell count, measured as a dichotomous variable of ≥200 (1) or <200 (0) cells per cubic millimeter (mm3), and viral load, measured as detectable (1) or undetectable (0).
We measured dental problems using a simple count of the frequency with which patients reported that in the last 12 months they experienced each of a list of 11 common dental problems such as a toothache, loose teeth, or bleeding gums. We used this count, gathered with each survey administration, to create a continuous variable that measured the change in the number of dental problems patients reported between baseline and last available visit. Baseline use of tobacco, alcohol, and illicit drugs was measured as a dichotomous variable for each, with 1 representing use of the substance and 0 representing nonuse. A dichotomous variable measuring whether the teeth or gums had caused any pain or distress at the last available visit was also used, with 1 representing pain or distress and 0 representing no pain or distress. Dental services utilization was measured as a continuous count of services provided.
Structural barriers were conceptualized as barriers to availability of care, measured by how long it had been since the patient had received dental care. All study patients had been out of care for at least a year, except for emergency care. The measure used in this analysis categorized patients as having been out of care longer than two years (1) or fewer than two years (0).
Financial barriers were operationalized as reporting dental and health insurance coverage. Dental insurance was coded as 1 for any form of dental insurance (including private insurance, Medicaid, or other) or as 0 for no dental insurance. Health insurance was coded as 1 for Medicaid, Medicare, other public insurance, or private insurance or as 0 for no insurance.
RESULTS
Descriptive statistics
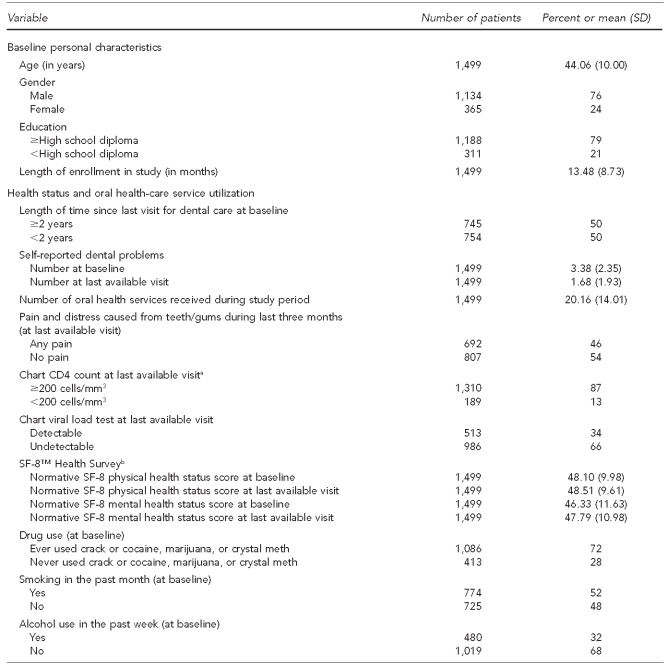
Characteristics of the 1,499 enrollees included in this study are shown in Table 1. Seventy-six percent of study participants were male, the mean age of participants was 44 years, 79% reported having $high school diploma, and the mean study enrollment time was 13 months.
Table 1.
Descriptive characteristics for a sample of HIV-positive adults (n=1,499) enrolled in the SPNS Oral Health Initiative, May 2007–August 2010
aThe range for a healthy CD4 count is 500–1,000 cells/mm3. A CD4 count of <200 cells/mm3 is an indicator of an AIDS diagnosis. Source: Department of Health and Human Services (US). AIDS.gov: understand your test results: CD4 count [cited 2011 Aug 18]. Available from: URL: http://aids.gov/hiv-aids-basics/diagnosed-with-hiv-aids/understand-your-test-results/cd4-count
bSource: Ware JE, Kosinski M, Dewey JE, Gandek B. How to score and interpret single-item health status measures: a manual for users of the SF-8™ Health Survey. Lincoln (RI): Quality Metric Inc.; 2001.
HIV = human immunodeficiency virus
SPNS = Special Projects of National Significance
SD = standard deviation
mm3 = cubic millimeter
SF-8™ = Short Form 8™
meth = methamphetamine
AIDS = acquired immunodeficiency syndrome
At enrollment, 50% of the study participants had not received dental care in two years or longer. At the baseline visit, participants had a mean of 3.38 dental problems, and at the last available visit, the mean number of reported dental problems had declined by about half to 1.68. The mean number of dental clinic services participants received while enrolled was 20.16. At the last available visit, 54% of study participants reported having no pain in their teeth or gums during the past three months. Slightly more than one-third (34%) of the study participants had a detectable viral load and 13% had a CD4 cell count of <200 cells/mm3 at the last available visit.
The mean norm-based SF physical health status summary scores at baseline (48.10) and follow-up (48.51) were comparable. Mental health status summary scores improved from baseline (46.33) to follow-up (47.79). These physical and mental health status scores were below the normed average of 50.00 for the general population.6
At baseline, 72% of participants reported ever having used crack or cocaine, marijuana, or crystal methamphetamine; 52% reported smoking in the past month; and 32% reported using alcohol in the past week. Sixty-five percent of the participants reported having no dental insurance and 28% reported having no health insurance at baseline.
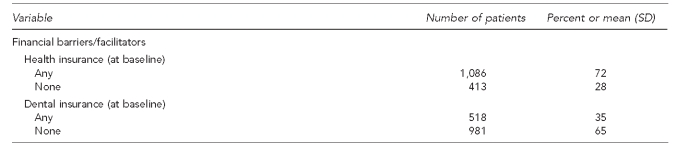
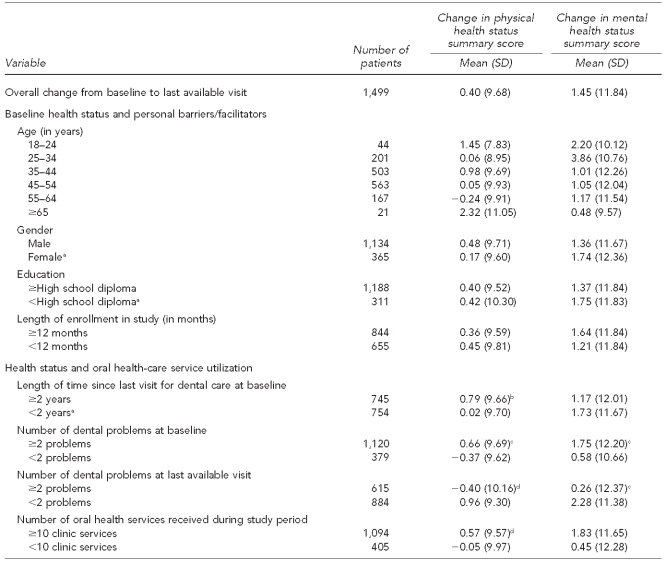
Bivariate analysis
Results of the bivariate analysis are shown in Table 2. Independent variables were analyzed as continuous variables, although results are shown in categories to provide the distribution of the variables. Variables that were significantly associated with a change in physical health status included length of time since last visit for dental care, number of dental problems, number of dental services, and health insurance. Variables that were significantly associated with a change in mental health status included number of dental problems, dental pain, viral load, alcohol use, and health insurance.
Table 2.
Bivariate analysis of characteristics by health status for a sample of HIV-positive adults (n=1,499) enrolled in the SPNS Oral Health Initiative, May 2007–August 2010
aReference group for independent variable
bp≤0.05 (p-values based on GEEs controlling for correlation among observations with each of the 14 sites)
cp≤0.001 (p-values based on GEEs controlling for correlation among observations with each of the 14 sites)
dp≤0.01 (p-values based on GEEs controlling for correlation among observations with each of the 14 sites)
eThe range for a healthy CD4 count is 500–1,000 cells/mm3. A CD4 count of <200 cells/mm3 is an indicator of an AIDS diagnosis. Source: Department of Health and Human Services (US). AIDS.gov: understand your test results: CD4 count [cited 2011 Aug 18]. Available from: URL: http://aids.gov/hiv-aids-basics/diagnosed-with-hiv-aids/understand-your-test-results/cd4-count
HIV = human immunodeficiency virus
SPNS = Special Projects of National Significance
SD = standard deviation
mm3 = cubic millimeter
meth = methamphetamine
GEE = general estimating equation
AIDS = acquired immunodeficiency syndrome
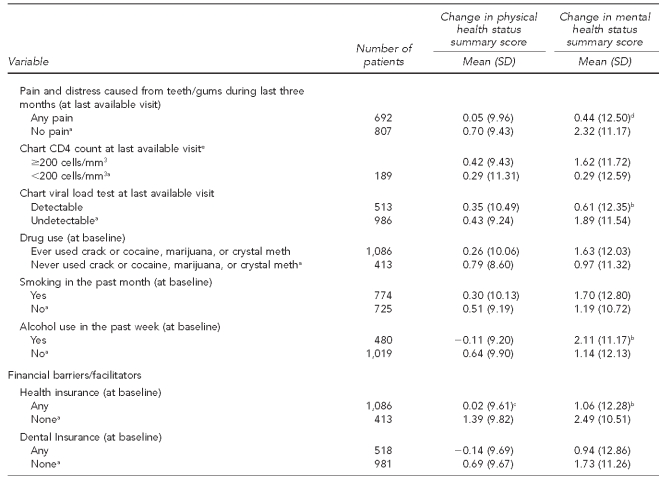
Multivariate analysis
Variables significantly associated with each dependent variable were included in the multivariate linear regression model for that dependent variable: one model used the physical health summary score as the dependent variable, and one model used the mental health summary score as the dependent variable. Length of enrollment was also included in each model to control for this potential confounding. In addition, when the physical health summary score served as the dependent variable, the mental health summary score was included in the model to control for potential confounding. Similarly, when the mental health summary score served as the dependent variable, the physical health summary score was included in the model.
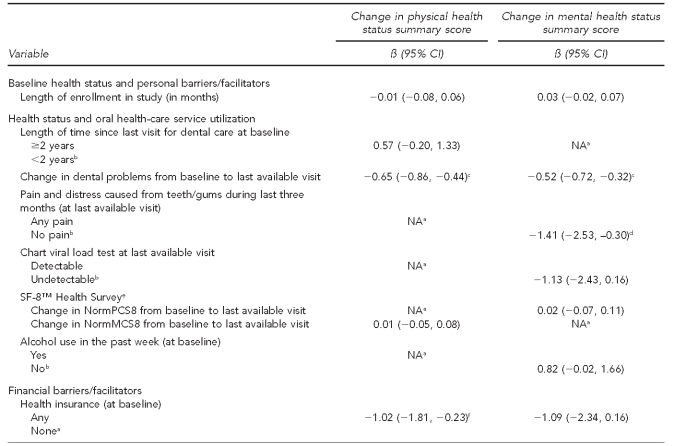
Table 3 shows factors associated with change in self-reported physical and mental health status in an HIV-positive sample following enrollment in a project that promoted access to oral health care. For change in physical health status, a decrease in oral health problems and lack of health insurance were significantly associated with improved physical health status. For change in mental health status, a decrease in oral health problems and no pain at the last available visit were significantly associated with improved mental health status.
Table 3.
Multivariate analysis of characteristics associated with improved health status for a sample of HIV-positive adults (n=1,499) enrolled in the SPNS Oral Health Initiative, May 2007–August 2010
aVariable not included in final model
bReference group for independent variable
cp≤0.001 (p-values based on GEEs controlling for correlation among observations with each of the 14 sites)
dp≤0.05 (p-values based on GEEs controlling for correlation among observations with each of the 14 sites)
eSource: Ware JE, Kosinski M, Dewey JE, Gandek B. How to score and interpret single-item health status measures: a manual for users of the SF-8™ Health Survey. Lincoln (RI): Quality Metric Inc.; 2001.
fp≤0.01 (p-values based on GEEs controlling for correlation among observations with each of the 14 sites)
HIV = human immunodeficiency virus
SPNS = Special Projects of National Significance
CI = confidence interval
NA = not applicable
SF-8™ = Short Form 8™
NormPCS8 = normative physical health status score
NormMCS8 = normative mental health status score
GEE = general estimating equation
DISCUSSION
Among a sample of PLWHA who had not received oral health care for at least a year, results suggest that there was marginal improvement in self-reported physical health status from baseline to follow-up and that better self-reported physical health status was associated with a reduction in dental problems and not having health insurance. Self-reported mental health status showed greater improvement between baseline and follow-up visits. Improved self-reported mental health status was associated with fewer oral health problems and no oral pain at the last available visit.
Although changes in self-reported physical health status and mental health status were not associated with the number of dental services received through the study, overall, results suggest that enrollment in an intervention aimed at increasing access to dental care may increase self-reported well-being for people living with HIV. Improved self-reported mental health status was associated with fewer oral health problems and less oral pain, outcomes that are consistent with the overall goal of the Oral Health Initiative.
The SF scores are widely used as a population-based measure of health status and have been normed to facilitate comparison among different patient groups.23 The clinical meaning and interpretation of the SF scores is still being examined. A systematic review of the literature with respect to randomized trials showed that quality-of-life survey data were gathered in many of the trials, but that health status outcomes were not always reported.24 Results suggest that quality-of-life assessments rarely change the interpretation of the clinical trial results, that quality-of-life data are underutilized, and that quality-of-life assessment may be especially useful in trials for chronic conditions such as HIV. Ware et al. recommend use of normative data for interpretation of the SF results and suggest that differences of less than one point should not be interpreted as meaningful.25 Other authors have suggested that the clinical meaning of changes in SF scores may be assessed by calculating effect sizes.26,27 We calculated effect size for change in self-reported health status and found it to be less than 0.1 for physical health and between 0.1 and 0.2 for mental health status. In terms of clinical relevance, an effect size of 0.2 is considered small.28 Additional research is needed to understand whether significant changes in health status, such as those we observed in this study, are also clinically meaningful. Our results contribute to this body of knowledge by suggesting that access to oral health care can improve health status among PLWHA.
Limitations
The Oral Health Initiative is the largest study of access to oral health care for PLWHA since the HCSUS. Although the results are thus critically important, some study limitations must be considered in interpreting the results. First, the sample included individuals who met three eligibility criteria: participants were at least 18 years of age, were HIV-positive, and had not received dental care, other than to relieve pain and infection, in the last 12 months. Participants were also recruited through convenience sampling methods. Thus, the individuals who participated in the study are not representative of all adults who are HIV-positive.
Second, the data presented in this article were gathered through interviews conducted at each of the study sites. The interviewers were trained by the study's coordinating center, but it was not possible to monitor all interviews as they were completed to assure reliability of the data. The survey data gathered were self-reported, and we did not ascertain the validity of respondent reports. Third, variations among the sites and the states in which they are located may have affected the findings. The programs offered at each site varied such that the types of services available at each location ranged from preventive to oral surgery. These differences may have affected the types of patients who enrolled in the study and the overall sample size at each site.
CONCLUSION
Our results suggest that for low-income PLWHA, access to oral health care increases self-reported well-being as measured by the SF-8. Although there was minimal change in self-reported physical health status, self-reported mental health status improved by nearly two points during study enrollment. Improved self-reported mental health status affirms the association between psychosocial well-being and oral health, as suggested by the Surgeon General's 2000 report.16 Additional research is needed to understand the clinical meaning of the results. For public health practitioners working with PLWHA, however, our findings suggest that promoting access to oral health care is a strategy that may promote overall well-being for this vulnerable population.
Footnotes
This study was supported by grant #H97HA07519 from the U.S. Department of Health and Human Services, Health Resources and Services Administration. This grant is funded through the HIV/AIDS Bureau's Special Projects of National Significance program. The contents of this article are solely the responsibility of the authors and do not necessarily represent the views of the funding agencies or the U.S. government.
This research project was approved by the Institutional Review Board of the Boston University Medical Campus.
REFERENCES
- 1.Delate T, Coons SJ. The discriminative ability of the 12-item Short Form Health Survey (SF-12) in a sample of persons infected with HIV. Clin Ther. 2000;22:1112–20. doi: 10.1016/S0149-2918(00)80088-0. [DOI] [PubMed] [Google Scholar]
- 2.Han C, Pulling CC, Telke SE, Huppler Hullsiek K Terry Beirn Community Programs for Clinical Research on AIDS. Assessing the utility of five domains in SF-12 Health Status Questionnaire in an AIDS clinical trial. AIDS. 2002;16:431–9. doi: 10.1097/00002030-200202150-00015. [DOI] [PubMed] [Google Scholar]
- 3.Riley ED, Bangsberg DR, Perry S, Clark RA, Moss AR, Wu AW. Reliability and validity of the SF-36 in HIV-infected homeless and marginally housed individuals. Qual Life Res. 2003;12:1051–8. doi: 10.1023/a:1026166021386. [DOI] [PubMed] [Google Scholar]
- 4.Riley ED, Wu AW, Perry S, Clark RA, Moss AR, Crane J, et al. Depression and drug use impact health status among marginally housed HIV-infected individuals. AIDS Patient Care STDS. 2003;17:401–6. doi: 10.1089/108729103322277411. [DOI] [PubMed] [Google Scholar]
- 5.Smith MY, Feldman J, Kelly P, Dehovitz JA, Chirgwin K, Minkoff H. Health-related quality of life of HIV-infected women: evidence for the reliability, validity and responsiveness of the Medical Outcomes Study Short-Form 20. Qual Life Res. 1996;5:47–55. doi: 10.1007/BF00435968. [DOI] [PubMed] [Google Scholar]
- 6.Ware JE, Kosinski M, Dewey JE, Gandek B. How to score and interpret single-item health status measures: a manual for users of the SF-8™ Health Survey. Lincoln (RI): Quality Metric Inc; 2001. [Google Scholar]
- 7.Liu C, Johnson L, Ostrow D, Silvestre A, Visscher B, Jacobson LP. Predictors of lower quality of life in the HAART era among HIV-infected men. J Acquir Immune Defic Syndr. 2006;42:470–7. doi: 10.1097/01.qai.0000225730.79610.61. [DOI] [PubMed] [Google Scholar]
- 8.Lightfoot M, Rogers T, Goldstein R, Rotheram-Borus MJ, May S, Kirshenbaum S, et al. Predictors of substance use frequency and reductions in seriousness of use among persons living with HIV. Drug Alcohol Depend. 2005;77:129–38. doi: 10.1016/j.drugalcdep.2004.07.009. [DOI] [PubMed] [Google Scholar]
- 9.Mannheimer SB, Matts J, Telzak E, Chesney M, Child C, Wu AW, et al. Terry Beirn Community Programs for Clinical Research on AIDS. Quality of life in HIV-infected individuals receiving antiretroviral therapy is related to adherence. AIDS Care. 2005;17:10–22. doi: 10.1080/09540120412331305098. [DOI] [PubMed] [Google Scholar]
- 10.Bing EG, Hays RD, Jacobson LP, Chen B, Gange SJ, Kass NE, et al. Health-related quality of life among people with HIV disease: results from the Multicenter AIDS Cohort Study. Qual Life Res. 2000;9:55–63. doi: 10.1023/a:1008919227665. [DOI] [PubMed] [Google Scholar]
- 11.Bakken S, Holzemer WL, Brown MA, Powell-Cope GM, Turner JG, Inouye J, et al. Relationships between perception of engagement with health care provider and demographic characteristics, health status, and adherence to therapeutic regimen in persons with HIV/AIDS. AIDS Patient Care STDS. 2000;14:189–97. doi: 10.1089/108729100317795. [DOI] [PubMed] [Google Scholar]
- 12.Holmes W, Bix B, Shea J. SF-20 and item distributions in a human immunodeficiency virus-seropositive sample. Med Care. 1996;34:562–9. doi: 10.1097/00005650-199606000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Mrus JM, Sherman KE, Leonard AC, Sherman SN, Mandell KL, Tsevat J. Health values of patients coinfected with HIV/hepatitis C: are two viruses worse than one? Med Care. 2006;44:158–66. doi: 10.1097/01.mlr.0000197027.06808.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bennett IM, Chen J, Soroui JS, White S. The contribution of health literacy to disparities in self-rated health status and preventive health behaviors in older adults. Ann Fam Med. 2009;7:204–11. doi: 10.1370/afm.940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Crystal S, Fleishman JA, Hays RD, Shapiro MF, Bozzette SA. Physical and role functioning among persons with HIV: results from a nationally representative survey. Med Care. 2000;38:1210–23. doi: 10.1097/00005650-200012000-00008. [DOI] [PubMed] [Google Scholar]
- 16.Department of Health and Human Services (US), Office of the Surgeon General. Oral health in America: a report of the Surgeon General. 2000. May, [cited 2010 Dec 17]. Available from: URL: http://www.surgeongeneral.gov/library/oralhealth.
- 17.RAND Corporation. Do people with HIV get the dental care they need? Results of the HCSUS study. [cited 2010 Dec 17]. Available from: URL: http://www.rand.org/content/dam/rand/pubs/research_briefs/2005/RAND_RB9067.pdf.
- 18.Institute of Medicine. Advancing oral health in America. Washington: National Academies Press; 2011. [Google Scholar]
- 19.Brown JB, Rosenstein D, Mullooly J, O'Keeffe Rosetti M, Robinson S, Chiodo G. Impact of intensified dental care on outcomes in human immunodeficiency virus infection. AIDS Patient Care STDS. 2002;16:479–86. doi: 10.1089/10872910260351258. [DOI] [PubMed] [Google Scholar]
- 20.Millman M, editor. Institute of Medicine. Access to health care in America. Washington: National Academy Press; 1993. [PubMed] [Google Scholar]
- 21.Smedley BD, Stith AY, Nelson AR, editors. Institute of Medicine. Unequal treatment: confronting racial and ethnic disparities in health care. Washington: National Academies Press; 2002. [PubMed] [Google Scholar]
- 22.Ware JE, Kosinski M, Bjorner J, Turner-Bowker D, Gandek B, Maruish ME. User's manual for the SF-36v2 Health Survey. 2nd ed. Lincoln (RI): Quality Metric Inc.; 2007. [Google Scholar]
- 23.IBM SPSS Inc. SPSS®/PASW®: Version 18.0 for Mac OS. Chicago: IBM SPSS Inc.; 2010. [Google Scholar]
- 24.Contopoulos-Ioannidis DG, Karvouni A, Kouri I, Ioannidis JP. Reporting and interpretation of SF-36 outcomes in randomised trials: systematic review. BMJ. 2009;338:a3006. doi: 10.1136/bmj.a3006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ware JE, Kosinski M. Interpreting SF-36 summary health measures: a response. Qual Life Res. 2001;10:405–13. doi: 10.1023/a:1012588218728. [DOI] [PubMed] [Google Scholar]
- 26.Yost KJ, Haan MN, Levine RA, Gold EB. Comparing SF-36 scores across three groups of women with different health profiles. Qual Life Res. 2005;14:1251–61. doi: 10.1007/s11136-004-6673-8. [DOI] [PubMed] [Google Scholar]
- 27.Iqbal SU, Rogers W, Selim A, Qian S, Lee A, Ren XS, et al. The Veterans RAND 12 Item Health Survey (VR-12): what it is and how it is used. [cited 2011 Jun 25]. Available from: URL: http://www.chqoer.research.va.gov/docs/VR12.pdf.
- 28.Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale (NJ): Lawrence Erlbaum Associates, Inc.; 1988. [Google Scholar]