Abstract
This qualitative study explored the impact on oral health-care knowledge, attitudes, and practices among 39 people living with HIV/AIDS (PLWHA) participating in a national initiative aimed at increasing access to oral health care. Personal values and childhood dental experiences, beliefs about the importance of oral health in relation to HIV health, and concerns for appearance and self-esteem were found to be determinants of oral health knowledge and practice. Program participation resulted in better hygiene practices, improved self-esteem and appearance, relief of pain, and better physical and emotional health. In-depth exploration of the causes for these changes revealed a desire to continue with dental care due to the dental staff and environmental setting, and a desire to maintain overall HIV health, including oral health. Our findings emphasize the importance of addressing both personal values and contextual factors in providing oral health-care services to PLWHA.
For people living with human immunodeficiency virus (HIV) and acquired immunodeficiency syndrome (AIDS) (PLWHA), having appropriate oral hygiene knowledge and practices is essential. Studies have shown that poor oral hygiene increases the risk of oral complications of HIV disease, which may result in poorer physical and mental health status.1,2 PLWHA who receive oral hygiene education and preventive dental care are less likely to require complex procedures and treatment.3,4 Yet, data from the national HIV Cost and Services Utilization Study found that, since learning their HIV-positive status, only 26% of PLWHA reported daily flossing, 34% reported brushing and flossing more often, 23% reported seeing a dentist with less frequency, and 11% reported never doing self-examination.5 Finding strategies to effectively educate PLWHA on these practices is critical for managing oral health, HIV health, and overall quality of life.
Providers need to understand the contextual factors, attitudes, and beliefs toward oral health-care and hygiene practices to effectively educate and improve practices. Studies of the social-behavioral determinants of oral health behaviors and use of dental services in the general adult population found poorer practices among minorities, males, people on social assistance, and those with lower education levels.6–9 Evidence suggests that dental attitudes and patients' perceptions of the importance of oral health care and self-concept may play a role in oral health-care-seeking behavior.10–14 A recent study found that increases in dental knowledge may be associated with better oral health status.15 In addition to cost, factors cited as barriers to care for PLWHA include patient attitudes and beliefs about dental care, low motivation for seeking care given competing needs, and fear/mistrust of dentists.4,5,16 These findings suggest that, despite removing structural and financial barriers to accessing care, use of dental care may still be limited by personal knowledge, values, and cultural perceptions of dental care.
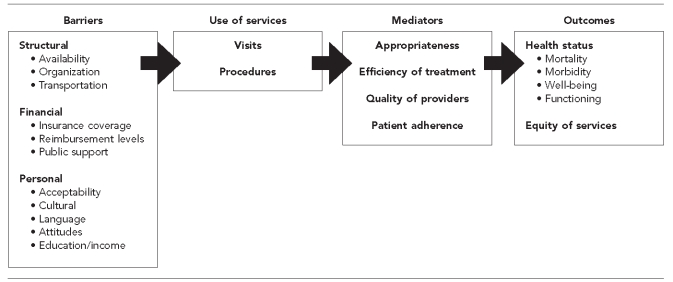
The purpose of this qualitative study was to explore the knowledge, attitudes, and practices of oral health care among PLWHA that may contribute to the access to and use of dental care services. Participants were selected from the Health Resources and Services Administration HIV/AIDS Bureau's Special Projects of National Significance Innovations in Oral Health Care Initiative (hereafter, Oral Health Initiative), aimed at improving access to oral health care. The main research questions were as follows: (1) What are the experiences, knowledge, attitudes, and practices toward dental care pre- and post-HIV diagnosis? (2) How does participation in the Oral Health Initiative impact participants' oral health care and practices? (3) What factors contribute to participants coming back for dental care at this setting? This study was designed to complement a longitudinal survey of the impact of the Oral Health Initiative interventions on increasing access to oral health care in accordance with the Institute of Medicine's model of access to and use of health-care practices (Figure).17 Our aim was to identify the contextual and personal factors that could assist dental providers in developing and communicating a personalized treatment plan that would enhance patient self-care practices and might, in turn, reduce the burden of oral health disease among PLWHA.
Figure.
Framework for access to personal health-care servicesa
aInstitute of Medicine. Millman M, editor. Access to health care in America. Washington: National Academy Press; 1993.
METHODS
An initial subsample of 60 participants was recruited from a national study of HIV-positive patients enrolled in the Oral Health Initiative. Six study sites (two rural and four urban) volunteered to recruit eight to 10 participants each for the study. Participants were selected to reflect each site's patient demographic distribution. All participants had been out of dental care for at least one year and were recently enrolled in dental care at the Oral Health Initiative sites. Each site implemented a program intervention to improve access to and use of dental services for PLWHA. Interventions included using dental care coordinators, improving coordination with HIV medical care, providing transportation assistance, enhancing patient education, and setting up mobile dental units. In-depth descriptions of these intervention models have been published elsewhere.17,18
The study was designed to interview participants at the initial receipt of dental care and approximately 12–15 months later to ascertain participants' perceptions of the program and its effect on their self-care practices, as well as their desire to come back for care. An open-ended interview guide was used to capture participant perceptions and experiences in their own words. The initial interview focused on prior experience with oral health care since childhood and pre- and post-HIV diagnosis. To assess personal values, knowledge, and practices, our questions included the following: (1) How important was oral health care in your childhood and now as an adult? (2) What are some of the ways people take care of their teeth and mouth? (3) What do you currently do to take care of your teeth and mouth? At the follow-up interview, participants were asked: (1) What information did you learn from participating in the Oral Health Initiative program? (2) What changes have you made with respect to taking care of your mouth, teeth, and gums (your oral health habits) since your first dental care visit with our program? (3) What factors have made the biggest difference in your self-care practices? Interviews were conducted in English and Spanish. All interviews were recorded and transcribed for coding and analysis.
We conducted thematic analysis to identify and report patterns within the data.19 Relevant themes emerged based on frequency of discussion and expression of importance by participants. The researchers at the participating sites and multisite research center read each transcript and developed an initial list of codes representing these themes. The coding list was used to assign segments of the narrative data at both initial and follow-up interviews using the qualitative analysis software NVivo version 8.20 To assess knowledge and practices, participant responses were compared with the American Dental Association's (ADA's) recommended care practices for the general consumer.21,22 Two researchers at the multisite center checked and validated the interpretations of the data. Final selection of the narrative data was conducted by the primary researchers at the multisite research center and shared with the researchers at the sites for accuracy in reporting results. Institutional Review Boards from the respective participating institutions approved the study.
RESULTS
A total of 39 participants across five sites completed both interviews. The majority of participants were male (n=30) and were members of racial/ethnic minority groups (African American/black [n=14], Hispanic [n=6], and Asian or Native American [n=3]). Five interviews were conducted in Spanish. The mean age of participants was 46.5 years (range: 29–67 years) and participants had been living with HIV an average of 11 years. Twenty-one participants did not return for a follow-up interview and were either lost to follow-up or moved out of the service area (data not shown). In this section, we describe the knowledge, attitudes, and practices prior to participating in the Oral Health Initiative, during childhood and as an adult, as well as the changes that resulted from having access to dental care via the Oral Health Initiative.
Oral health-care knowledge, attitudes, and practices prior to Oral Health Initiative participation
Limited dental care and education during childhood.
Approximately half of the participants described having limited or no experience with dental care as a child or adolescent. Limited experience was defined as visiting the dentist “once or twice due to an emergency, such as pain or injury.” Participants who had regular/consistent dental care (“I would go at least annually”) emphasized the value placed by parents or caregivers. These participants reported having a family dentist or receiving services via a mobile van or in school. For those without consistent care, the lower priority could be attributed to poverty (“my parents couldn't afford to bring us to the dentist”) or lack of guidance about how to properly care for the teeth. This limited experience as a child was common among both rural and urban participants, and no racial/ethnic differences emerged. One participant from a rural area described his experience and the importance of dental care:
I was not a regular client at the dentist because my parents only took me to the dentist once in my life; so I didn't know the need for follow-up dental [care] or keeping a good hygiene program until I got older and had problems.
Limited knowledge and practice of oral hygiene.
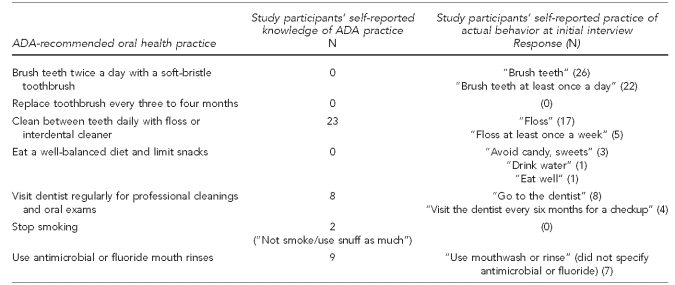
In general, participants had a limited understanding of appropriate oral hygiene practices in comparison with the ADA's recommended practices (Table). While participants correctly cited brushing and flossing as appropriate ways to take care of their teeth and gums, few participants were able to describe the recommended frequency for tooth brushing or flossing. Eight participants were able to describe regularly going to the dentist for checkups as an additional practice, but fewer mentioned having a visit at least once a year. Two participants mentioned additional appropriate oral health-care practices, such as not smoking and dietary/nutritional habits. Another common practice mentioned was “using mouthwash” or “rinsing” to maintain the health of teeth and gums. Only two participants reported staying away from mouthwashes with alcohol and using “fluoride rinses,” which are currently included in the ADA-recommended practices (data not shown).21,22
Table.
Comparison of participants' self-reported oral health-care knowledge and practices with the ADA-recommended practicesa,b (n=39): HIV/AIDS Bureau's SPNS Oral Health Initiative, 2006–2011
aAmerican Dental Association. Cleaning your teeth and gums: patient version [cited 2011 Aug 1]. Available from: URL: http://www.ada.org/3072.aspx
bAmerican Dental Association. Consumer resources [cited 2011 Aug 1]. Available from: URL: http://www.ada.org/2881.aspx
ADA = American Dental Association
HIV/AIDS = human immunodeficiency virus/acquired immunodeficiency syndrome
SPNS = Special Projects of National Significance
Attitudes toward the importance of dental care.
There was a spectrum of attitudes about the value and importance placed on oral health care. Participants with a positive attitude viewed dental care as important due to the presence/absence of oral infections related to HIV disease: “I am really conscious of keeping my mouth clean now because a couple of years ago, my T cells got really low, and I started getting these blisters in my mouth and tongue. It was super painful.” Others valued oral health care but were not able to access care post-diagnosis due to financial reasons or other competing priorities.
Approximately one-third of participants were motivated to seek care because of concerns about their appearance, which affected their self-esteem and social relationships: “My appearance always has been a first priority. It is what makes you. If you are not taking care of yourself, no one will bother with you.”
For others, concerns were linked to employment opportunities: “My teeth are really in horrible shape. They're very embarrassing. I mean, I'm a bartender, and my face counts. It's made it so I don't smile, and it's made me self-conscious to go out and socialize. So it's affected a lot actually; a large impact.”
Still other participants felt oral health care was not important due to either a lack of symptoms or a belief that they had “strong teeth.” This lack of importance was also linked to their limited awareness or their feeling that oral health care was a low priority compared with fulfilling other immediate needs, such as finding a place to live or substance use, even if dental services were available.
Impact of participation in the Oral Health Initiative
At the follow-up interviews, participants were asked about changes made in taking care of their teeth and gums and the biggest difference after participating in the Oral Health Initiative program. Following are the major themes that emerged.
Awareness of the link between HIV health and good oral health.
Participants described gaining knowledge about sound oral health-care practices as part of overall HIV health care. As one participant described, “I realize I have to keep my mouth clean and healthy because people like me [with HIV disease] can get infections in [our] mouth[s].” Others found that taking care of their teeth and mouth helps them “eat more so [they] feel better and healthier with HIV.”
Better hygiene practices.
Participants reported better oral hygiene knowledge and practices following program participation. Several participants described how they brush and floss with improved technique and greater frequency:
“I've learned about the motion for brushing my teeth.… I now brush the back of my teeth.”
“I floss more now, at least once a day, and I learned how to brush my teeth.”
“I carry around my toothbrush and brush after every meal.”
“Teaching about how to keep your teeth… some people might think they know, but I didn't know you were supposed to brush your teeth for at least two minutes.”
More participants described being aware of the detrimental effects of smoking on oral health care even though they did not stop the habit. Others cited changes in their diet, such as reducing soda intake, drinking diet soda, avoiding candy and sweets, and eating healthier foods with less sugar.
Improved self-esteem and appearance.
“Being able to smile again” was cited as a positive outcome of participating in the program. Participants reported feeling less self-conscious and more confident in their social interactions. As one participant described:
I was, for the longest time, real conscious that my teeth were not in good shape and had to be taken out. So I would have to be conscious of the way that I ate because I was fearful [my teeth] were going to fall out. Coming here relieves overall stress about my teeth. This is actually a big thing.… I was very stressed. That was a major part of my stress prior to coming here and dealing with my teeth.
Relief of pain and better physical and emotional health.
Another impact of program participation was relief of pain. Participants reported feeling better physically as well as emotionally.
“Since I came to this program, I got a partial, and now I can eat and chew food. I feel healthier and better about myself.”
“The biggest difference since coming here is the physical.… I feel better now. My teeth don't hurt like they used to. I am able to get out and enjoy myself. I like to smile and talk. I can do more now that there is no pain at all.”
Reasons for returning to dental care
For almost all participants, the Oral Health Initiative made it possible to “have a place to go for care,” something that had been missing in their lives. Creating this access also led to a “desire to keep up with [their] overall health.” When asked about the desire to return to care at the Oral Health Initiative site compared with other dental settings, participants cited the free or limited cost of the dental services. Other cited reasons for returning to dental care included the friendly staff and the dental setting, finding an HIV-knowledgeable dentist, having a care coordinator for support, and being motivated to maintain their oral and general health.
Friendly staff and dental environment.
Treatment by the dental staff was cited as the main difference in oral health care and the desire to continue care. Participants described “feeling comfortable in the environment” and “not worrying about my privacy.” Other critical factors were not having to wait for services and having things done quickly with the utmost professionalism.
[In the past,] even if I would've had the money, I wouldn't have gone because how I felt… I mean, how am I gonna be treated today, wonder what they're gonna do, are they gonna be rude, are they gonna sit there and not wanna even get close to me. You know, they have gloves on [and] a mask, and [they're] not even doing any drilling, just talking to me. They don't wanna get that close. You know, that's not something I wanted to go through. Coming to a place like this… I mean, it didn't matter who was your hygienist, who was around you, they all treated you great, and I would come back.
Finding an HIV-knowledgeable dentist.
Participants valued having a dentist who knew about HIV and its treatment. They valued dentists who could identify problems, take the time to help “save my teeth,” and explain procedures. They described how they finally received quality care and found dental staff who knew how to take care of people with HIV. One participant described his reason for coming back for care:
I definitely want a dentist [who] is aware, as all my medical people must be experienced in HIV care. This didn't happen to me but my partner [who passed] away.… The first thing that they found was a [Kaposi's sarcoma] lesion in his mouth during a dental routine, because he had terrible dental health.… He had a lifetime of bad dental health, so he always went to the dentist; and the dentist actually saw something in his mouth, and his doctor hadn't even seen it. So it was the dentist [who] found it. I don't really think about that. So that is one of the reasons why I want a dentist [who] does understand HIV care. That is absolutely critical.
Having a care coordinator to educate and support dental care.
Four of the sites employed dental care coordinators, staff who worked as either HIV case managers or patient navigators, to tend to the clients' specific dental needs. Participants described care coordinators as contributing to their reasons for returning to care. For example, participants described how care coordinators helped with referrals to specialists, provided reminder phone calls and messages about appointments, and facilitated communication between their medical and dental providers. As one participant described, “She makes it easy to access things I need for my oral care.… If it was someone else less friendly, I would be less likely to call up and get things done.”
Others discussed how seeing a care coordinator helped reduce their fears and anxiety about the dentist and made them feel more comfortable returning for care:
She has helped me very much. First and foremost, she has helped me just with the comfort level of dealing with a place like this. I am kind of intimidated by a dentist. I mean, who is not? But she has been very comforting, and she has been very good at explaining procedures. She is probably pretty much—if it wasn't for what she has done for me as far as helping, scheduling, talking, sitting with me during the dentist, and everything—I may not have followed through. So, it has made a really big difference. It makes me feel like there is somebody committed to my dental care, so my commitment can't be any less than that.
Care coordinators also played a role in patient oral hygiene education. Participants described how the staff member took the time to explain how to take care of the mouth and teeth. The care coordinator could answer the questions and educate and reinforce messages shared by other dental staff.
He started asking me specific questions about how I cared for my teeth—what did I do, what process did I use to do certain things—which reminded me to take those things into mind whenever I started thinking about my mouth. So, just speaking to him encouraged me more to start taking care of my mouth, because he was asking me questions about how my mouth was affecting my general behavior through the entire day and in every situation. I began to see better what he was speaking about, how all the hygiene, the flossing, and everything comes into effect.
Maintaining personal oral health and overall general health.
Another motivating factor for coming back to dental care was maintaining oral health and overall general health. As one participant reported, “I come back because I need [to] keep up with my oral health just the same way I monitor my blood and everything else.” Others reported a desire to “keep their teeth in their mouth” and recognized the importance of the dental program in helping them to achieve this goal by showing them how to care for their teeth and mouth. For others, the desire to maintain their oral health was also linked to their HIV health. As one participant reported, “If your teeth are healthier, that means you are healthier, and that will help with your (CD4) counts.” For one participant, going to the dentist became associated with “doing good for my health” to keep out infections caused by HIV. One participant described the advice he would share with other PLWHA:
If you don't take care of your teeth (or have dentures put in)… It is important, because if your T cells drop below 200, then you are more susceptible to microorganisms, and you can die.… You need to know how to take care of your teeth and be willing to spend the time and energy to do proper daily oral hygiene.
DISCUSSION
The U.S. Surgeon General suggests that a first step to enhancing the overall oral health of the general population is to “change the perceptions regarding oral health and disease so that it becomes an accepted component of general health.”23 In this study among PLWHA, we found that adopting this perception is possible but requires addressing a multitude of personal and environmental factors that contribute to poor oral health-care knowledge and practices. For traditionally underserved populations such as PLWHA, limited experience with dental care since childhood and poor experiences within dental settings have contributed to the low perception in the value of oral health as part of overall HIV health. Studies have described the lack of importance placed on oral health compared with other medical conditions among low-income populations, but this is the first study to explore in-depth attitudes and practices among PLWHA.24
Our findings revealed motivators that could help to change the perceptions and attitudes toward oral health care. One motivator was being able to maintain healthy levels of CD4 and viral load counts. Participants who understood the links between appropriate oral hygiene, fewer oral infections, and the impact on their HIV status tended to place a higher value on oral health care. Another motivator was the concern for personal appearance. Many participants reported that receiving dental services made them want to smile more, reduced their social isolation, and improve their overall self-esteem. These findings support other studies that found self-esteem as a mediating role in supporting changes in dental behavior and oral health-care-seeking behavior.14,25
Our study also highlights the roles played by the dentist, dental staff, and the general environment of the dental setting as critical to participants seeking and returning for dental services. Having a dentist who understood HIV, staff who welcomed and respected the patient, and a care coordinator who reminded them about appointments or could explain and teach proper oral hygiene practices all contributed to improved knowledge and practices and a desire to come back for care. Other studies among vulnerable populations found negative attitudes of dental staff to be obstacles to seeking and continuing with dental care.26 Our findings also suggest the importance of trust of the dental provider, which has been found to be a significant determinant for regular use of dental care among low-income adults.27
Our findings did not differ across participants' race/ethnicity or geographic location, but this homogeneity could be attributed to the small sample and selective recruitment techniques. Other studies on oral health behaviors and beliefs in low-income adult populations have found differences by race/ethnicity, but the impact on oral health-care use has been mixed due to inconsistencies in sample characteristics and measures.6–9 Our findings are also consistent with those of other studies emphasizing an approach that addresses the structural and other underlying contextual factors, and not solely individual behaviors, to reduce disparities to care.28–30
Program implications
The impact of participating in the Oral Health Initiative program suggests promising evidence for promoting strategies that lead to positive changes in oral health knowledge, attitudes, and practices for PLWHA. Our findings support recommendations for more structured interventions and messages about the type and frequency of brushing, flossing, and other preventive behaviors such as regular dental visits, and for addressing patients' cultural perceptions and value for oral health, which contribute to dental behaviors.15,31 For dental providers, part of this strategy could include asking a patient about dental care during childhood, as well as current practices. Another approach is to ask patients to demonstrate their oral hygiene practices, such as flossing, and inquire about dietary habits and frequency of harmful behaviors such as smoking. These simple interventions can help to identify problems and enhance the promotion of preventive practices. Our study found that few participants were aware of the appropriate frequency of oral hygiene practices, and the majority of participants described learning new information about brushing techniques, flossing, and other practices that contribute to better oral health during follow-up interviews. While participants had taken steps toward reducing harmful behaviors, further encouragement was warranted from dental staff. In addition to focusing on individual behavior, dental providers can address the contextual factors, such as treatment by staff, waiting times, and the environment. For PLWHA, who may have a history of fear and mistrust of the dental community, creating a dental setting that places value on privacy, confidentiality, and respect for the patient is essential.
Programs can employ dental care coordinators as part of the dental care team to play this encouraging and supportive role for PLWHA. In the Oral Health Initiative, dental care coordinators were available to answer questions and follow up with dental care and treatment to ensure patients completed necessary treatment plans and adopted appropriate preventive oral health behaviors. They played a key role in finding and making referrals with specialists, providing translation services for non-English-speaking patients, and reminding patients about or rescheduling appointments. These staff had experience and training in the dental and/or HIV fields. Some coordinators were HIV case managers who received training in oral health, and others were dental assistants who were trained in HIV information. At some sites, the dental care coordinator was a new member of the dental health-care team. For dental clinics that may not have additional resources to employ care coordinators, staff such as dental assistants or hygienists could be trained in HIV-related information. Future studies could examine the role and effectiveness of dental care coordinators in improving oral health-care practices.
For HIV and other medical providers, questions about previous dental visits and knowledge of oral health-care behaviors should be asked routinely at regular medical and case-management visits as part of usual intake and reassessment visits. Our population highlighted that having access to dental care increased the awareness of the relationship between good oral health care and overall health in general. HIV social-services and medical providers can foster that link to better dental care and encourage their patients to adopt appropriate oral hygiene and health practices.
Limitations
Our study consisted of a small sample of PLWHA who had access to and the opportunity for continuous dental care and treatment. The results represent the attitudes and perceptions of a small group; nonetheless, we believe they may be widespread among PLWHA. Second, our study was based on interviews and self-reported changes and was not designed to conduct observations of patient practices. There is a possibility that the participants may have provided more positive feedback about participating in the program in an effort to ensure sustainability for dental services; however, asking open-ended questions to describe their knowledge, attitudes, and practices allowed for more in-depth responses that were trustworthy and reliable.
CONCLUSIONS
This qualitative study provides in-depth information about the personal values and practices that can influence oral health-care-seeking behavior among PLWHA. The results highlight a need for strategies that focus on the importance of oral health in the context of HIV health and provide information about and demonstration of appropriate self-care techniques. HIV and dental professionals can also play a critical role by establishing a friendly dental setting that fosters trust, support, and education to encourage the adoption of healthy behaviors.
Acknowledgments
The authors thank Lucy Wright, Gloryanna Valerio-Leonce, Penney Jones-Perry, and Jessica Feltz for assistance with conducting the interviews; Elizabeth Faye and Lauren Ibsen for assistance with data management and analysis; and Sara S. Bachman and Helene Bednarsh for their technical review.
Footnotes
This study was supported by grant #H97HA07519 from the U.S. Department of Health and Human Services, Health Resources and Services Administration. This grant is funded through the HIV/AIDS Bureau's Special Projects of National Significance program. The contents of this article are solely the responsibility of the authors and do not necessarily represent the views of the funding agencies or the U.S. government.
This multisite research project was approved by the Institutional Review Board of the Boston University Medical Campus, 2006–2011.
REFERENCES
- 1.Coulter ID, Heslin KC, Marcus M, Hays RD, Freed J, Der-Martirosian C, et al. Associations of self-reported oral health with physical and mental health in a nationally representative sample of HIV persons receiving medical care. Qual Life Res. 2002;11:57–70. doi: 10.1023/a:1014443418737. [DOI] [PubMed] [Google Scholar]
- 2.Cherry-Peppers G, Daniels CO, Meeks V, Sanders CF, Reznik D. Oral manifestations in the era of HAART. J Natl Med Assoc. 2003;95(2 Suppl 2):21S–32S. [PMC free article] [PubMed] [Google Scholar]
- 3.Hastreiter RJ, Jiang P. Do regular dental visits affect the oral health care provided to people with HIV? J Am Dent Assoc. 2002;133:1343–50. doi: 10.14219/jada.archive.2002.0049. [DOI] [PubMed] [Google Scholar]
- 4.Patton LL, Strauss RP, McKaig RG, Porter DR, Eron JJ., Jr Perceived oral health status, unmet needs, and barriers to dental care among HIV/AIDS patients in a North Carolina cohort: impacts of race. J Public Health Dent. 2003;63:86–91. doi: 10.1111/j.1752-7325.2003.tb03480.x. [DOI] [PubMed] [Google Scholar]
- 5.Freed JR, Marcus M, Freed BA, Der-Martirosian C, Maida CA, Younai FS, et al. Oral health findings for HIV-infected adult medical patients from the HIV Cost and Services Utilization Study. J Am Dent Assoc. 2005;136:1396–405. doi: 10.14219/jada.archive.2005.0053. [DOI] [PubMed] [Google Scholar]
- 6.Davidson PL, Rams TE, Andersen RM. Socio-behavioral determinants of oral hygiene practices among USA ethnic and age groups. Adv Dent Res. 1997;11:245–53. doi: 10.1177/08959374970110020701. [DOI] [PubMed] [Google Scholar]
- 7.Ronis DL, Lang PW, Antonakos CL, Borghakke WS. Preventive oral health behaviors among African-Americans and whites in Detroit. J Public Health Dent. 1998;58:234–40. doi: 10.1111/j.1752-7325.1998.tb02999.x. [DOI] [PubMed] [Google Scholar]
- 8.Bedos C, Levine A, Brodeur JM. How people on social assistance perceive, experience, and improve oral health. J Dent Res. 2009;88:653–7. doi: 10.1177/0022034509339300. [DOI] [PubMed] [Google Scholar]
- 9.Gremobowski D, Spiekerman C, Milgrom P. Racial and ethnic differences in a regular source of dental care and the oral health, behaviors, beliefs and services of low-income mothers. Community Dent Health. 2009;26:69–76. [PMC free article] [PubMed] [Google Scholar]
- 10.Frazer PJ, Jenny J, Bagramian R, Robinson E, Proshek JM. Provider expectations and consumer perceptions of the importance and value of dental care. Am J Public Health. 1977;67:37–43. doi: 10.2105/ajph.67.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Broder HL, Russell SL, Varagiannis E, Reisine ST. Oral health perceptions and adherence with dental treatment referrals among caregivers of children with HIV. AIDS Educ Prev. 1999;11:541–51. [PubMed] [Google Scholar]
- 12.Kiyak HA, Reichmuth M. Barriers to and enablers of older adults' use of dental services. J Dent Educ. 2005;69:975–86. [PubMed] [Google Scholar]
- 13.Riley JL, 3rd, Gilbert GH, Heft MW. Dental attitudes: proximal basis for oral health disparities in adults. Community Dent Oral Epidemiol. 2006;34:289–98. doi: 10.1111/j.1600-0528.2006.00280.x. [DOI] [PubMed] [Google Scholar]
- 14.Macgregor ID, Regis D, Balding J. Self-concept and dental health behaviours in adolescents. J Clin Periodontol. 1997;24:335–9. doi: 10.1111/j.1600-051x.1997.tb00766.x. [DOI] [PubMed] [Google Scholar]
- 15.Brennan D, Spencer J, Roberts-Thomson K. Dental knowledge and oral health among middle-aged adults. Aust N Z J Public Health. 2010;34:472–5. doi: 10.1111/j.1753-6405.2010.00592.x. [DOI] [PubMed] [Google Scholar]
- 16.Shibowski CH, Cohen M, Weber K, Shansky A, Malvin K, Greenblatt RM. Factors associated with use of dental services among HIV-infected and high-risk uninfected women. J Am Dent Assoc. 2005;136:1242–55. doi: 10.14219/jada.archive.2005.0340. [DOI] [PubMed] [Google Scholar]
- 17.Fox JE, Tobias CR, Bachman SS, Reznik DA, Rajabiun S, Verdecias N. Increasing access to oral health care for people living with HIV/AIDS in the U.S.: baseline evaluation results of the Innovations in Oral Health Care Initiative. Public Health Rep. 2012;127(Suppl 2):5–16. doi: 10.1177/00333549121270S203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rajabiun S, Bachman SS, Fox JE, Tobias C, Bednarsh H. A typology of models for expanding access to oral health care for people living with HIV/AIDS. J Public Health Dent. 2011;71:212–9. [PubMed] [Google Scholar]
- 19.Patton MQ. Qualitative research and evaluation methods. 3rd ed. Thousands Oaks (CA): Sage Publications; 2001. [Google Scholar]
- 20.QSR International Pty Ltd. NVivo 8. Melbourne (Australia): QSR International Pty Ltd; 2008. [Google Scholar]
- 21.American Dental Association. Cleaning your teeth and gums: patient version. [cited 2011 Aug 1]. Available from: URL: http://www.ada.org/3072.aspx.
- 22.American Dental Association. Consumer resources. [cited 2011 Aug 1]. Available from: URL: http://www.ada.org/2881.aspx.
- 23.Department of Health and Human Services (US); Office of the Surgeon General. Oral health in America: a report of the Surgeon General. May 2000. [cited 2010 Dec 17]. Available from: URL: http://www.surgeongeneral.gov/library/oralhealth.
- 24.Carr AB, Bebee TJ, Jenkins SM. An assessment of oral health importance: results of a statewide survey. J Am Dent Assoc. 2009;140:580–6. doi: 10.14219/jada.archive.2009.0230. [DOI] [PubMed] [Google Scholar]
- 25.Huff M, Kinion E, Kendra MA, Klecan T. Self-esteem: a hidden concern in oral health. J Community Health Nurs. 2006;23:245–55. doi: 10.1207/s15327655jchn2304_5. [DOI] [PubMed] [Google Scholar]
- 26.Mofidi M, Rozier RG, King RS. Problems with access to dental care for Medicaid-insured children: what caregivers think. Am J Public Health. 2002;92:53–8. doi: 10.2105/ajph.92.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Graham MA, Logan HL, Tomar SL. Is trust a predictor of having a dental home? J Am Dent Assoc. 2004;135:1550–8. doi: 10.14219/jada.archive.2004.0081. [DOI] [PubMed] [Google Scholar]
- 28.Watt RG. From victim blaming to upstream action: tackling the social determinants of oral health inequalities. Community Dent Oral Epidemiol. 2007;35:1–11. doi: 10.1111/j.1600-0528.2007.00348.x. [DOI] [PubMed] [Google Scholar]
- 29.Sanders AE, Spencer AJ, Slade GD. Evaluating the role of dental behaviour in oral health inequalities. Community Dent Oral Epidemiol. 2006;34:71–9. doi: 10.1111/j.1600-0528.2006.00261.x. [DOI] [PubMed] [Google Scholar]
- 30.Sabbah W, Tsakos G, Sheiham A, Watt RG. The role of health-related behaviors in the socioeconomic disparities in oral health. Soc Sci Med. 2009;68:298–303. doi: 10.1016/j.socscimed.2008.10.030. [DOI] [PubMed] [Google Scholar]
- 31.Ganss C, Schlueter N, Preiss S, Klimek J. Tooth brushing habits in uninstructed adults—frequency, technique, duration and force. Clin Oral Investig. 2009;13:203–8. doi: 10.1007/s00784-008-0230-8. [DOI] [PubMed] [Google Scholar]