Abstract
Background
Methadone substitution therapy is an effective harm reduction treatment method for opioid dependent persons. Ability to retain patients in methadone treatment is an accepted predictor of treatment outcomes.
Objectives
The current study evaluates the roles of psychiatric comorbidity, medical comorbidity, and sociodemographic characteristics as predictors of retention in methadone treatment utilizing retrospective analysis of data from a nationwide sample of patients in methadone treatment in the VA.
Methods
Data were gathered using the VA’s national health services use database. A cohort of veterans with a new episode of “opiate substitution” in fiscal year 1999 was identified, and their continuous service use was tracked through fiscal year 2002. The sample included a total of 2,363 patients in 23 VA medical centers. Survival analysis was used to explore factors associated with retention in methadone treatment.
Results
Younger age, having a serious mental illness, being African American, or having race recorded as unknown were associated with lower rates of retention in methadone treatment programs in this population of veterans (controlling for site).
Conclusion
Given that extended methadone treatment is associated with improved outcomes while patients remain in treatment, more longitudinal studies using primary data collection are needed to fully explore factors related to retention. For the VA population specifically, further research is necessary to fully understand the relationship between race/ethnicity and treatment retention.
Scientific Significance
This is the first retention study the authors are aware of that utilizes data from a nationwide, multisite, population of participants in methadone treatment.
Keywords: methadone maintenance, veterans, treatment retention, national sample
INTRODUCTION
Methadone substitution therapy for the treatment of opiate dependence has been available since the 1960s (1). The literature exploring treatment efficacy is difficult to summarize because treatment efficacy has been variably defined. However, methadone substitution therapy is clearly an effective method for decreasing heroin use (2–6), HIV transmission, criminal behaviors, as well as improving overall functioning (7–15).
The ability to retain patients in methadone treatment programs has been a consistent predictor of treatment outcomes, including decreased injectable heroin use and decreased use of other illicit drugs (2, 7, 11, 16–19). Older patients have been shown in several studies to have higher retention rates than younger patients (11, 12, 18, 20–23), and there is some indication that African Americans have lower retention rates than non-African Americans (12, 24–27). At least two studies show retention is related to higher rates of medical comorbidity (28, 29). Previous research indicates that higher dose is the most consistent predictor of treatment retention (22, 26, 30–32).
Findings vary with regard to the impact of comorbid psychiatric disorders on methadone retention. One study demonstrated an association between higher ASI psychiatric severity scores and early attrition (24). Other studies revealed trends toward increased attrition for patients with a personality disorder (33, 34). However, several studies found no impact of psychiatric status on treatment retention (11, 12, 35, 36).
Most prior work examining predictors of retention in methadone programs has used single sites or a handful of sites clustered in a limited region. The few studies using national samples have varied widely in terms of program characteristics (5, 37). The current study is unusual in that it is based on retrospective analysis of data from a nationwide sample of patients in methadone treatment in the Department of Veterans Affairs (VA). The research presented here evaluates the roles of psychiatric comorbidity, medical comorbidity, and sociodemographic characteristics as predictors of retention. We hypothesized that older age, Caucasian race, and higher medical comorbidity would be associated with longer retention in methadone treatment. We also hypothesized that the presence of psychiatric comorbidity would be associated with early attrition from methadone treatment.
METHODS
Data Source
Data were gathered using the VA’s national health services use database. This database maintains diagnostic and demographic information for each inpatient stay and outpatient visit recorded by veterans. Scrambled social security numbers allow for identification of unique patients.
Sample
We identified a cohort of veterans with a new episode of “opiate substitution” in fiscal year (FY) 1999 and tracked their continuous service use through FY 2002. Clinics in the VA offering opiate substitution therapy are coded consistently throughout the system, and eligible patients for this study were identified using the relevant clinic stop code in the database. In FY 1999, buprenorphine was not yet approved for use, and it is, therefore, assumed that most individuals in the “opiate substitution” stop code were receiving methadone or LAAM treatment. The beginning of a new treatment episode was defined as no previous visits in the clinic stop code within the prior 60 days. An episode was defined by searching the VA data for subsequent opiate substitution visits through the end of FY 2002 and defining the end of an episode as no contact in the clinic stop code for 60 days.
Our initial sample consisted of 2,988 treatment participants in 31 VA medical centers who began a new episode in FY 1999. Seven VA medical centers having less than 25 veterans in the clinic stop code during FY 1999 were excluded in an attempt to include only well-established methadone programs and to control for potential errors in the coding of clinic stops for individual veterans. We also excluded one medical center with a mean number of visits of one. Patients with primary diagnoses of opiate, cocaine, or unspecified/mixed dependence/abuse were retained for the analyses. The final sample included a total of 2,363 patients in 23 VA medical centers.
Measures
The dependent variable in the analyses was the number of consecutive days from the first date of a treatment episode (defined above) to the last date of the episode, through September 30, 2002. We devised a 60-day no contact “rule” to be sure we captured the numerous variations in appropriate treatment participation. Subjects were defined as “censored,” i.e., still continuing in methadone treatment, if their last visit dates were in August or September of 2002.
The independent variables used in the analyses were: age, gender, race, marital status, psychiatric comorbidity, and medical severity as measured by the Charlson Comorbidity Index (38). Age was measured continuously. Race was defined as Caucasian, African American, “other” (Hispanic, Asian-Pacific Islander, and Native American), and “unknown race.” The majority of cases in the “other” category were Hispanic. The last category of “unknown race” occurs when veterans do not report their race when asked about it during intake procedures for outpatient or inpatient service contacts. Four years of service use records (FY 1999–2002) in both outpatient and inpatient files were searched to identify race for as many veterans as possible in the sample. Marital status had the categories of married, divorced, unmarried, and unknown marital status.
Medical and psychiatric comorbidity information was obtained by noting ICD-9 diagnoses from each outpatient visit and inpatient stay during FY 1999. For this analysis, psychiatric comorbidity was measured using two dummy variables: “serious mental illness (SMI)” (including ICD-diagnoses for psychotic and bipolar disorder), and “mood/anxiety disorders” (including ICD-9 diagnoses for depressive and anxiety disorders including post-traumatic stress disorders). We followed the same diagnostic query procedure in creating the Charlson Comorbidity Index (38). This index is a single measure of medical severity created by the collection and differential weighting of 22 specific diagnoses (e.g., myocardial infarction, diabetes, renal disease, lymphoma, etc.). Each diagnosis is given a score of either 0, 1, 2, 3, or 6 depending on the risk of mortality within one year, and then totaled for each patient. A higher score indicates greater medical severity.
Data Analysis
We performed survival analysis using the proportional hazard model to explore factors associated with retention in methadone treatment from October 1998 through July 2002. Because we identified an interaction between time and age (thus violating the proportional hazards assumption), we fit a nonproportional hazard model with the inclusion of a time (days in methadone treatment) by age interaction. For this interaction term, time was transformed with a log transformation and centered about its mean, for numeric reasons. Sandwich variance estimates were used to account for the clustering structure of the data with patients within VA medical centers.
RESULTS
Descriptive statistics about the sample are presented in Table 1. The majority of the sample was male (95%) with a mean age of 48 (SD = 9) years old. About half of the sample was African American (45%), and one quarter was Caucasian (25%). The remainder of the sample was Hispanic or “other” (7%) and race unknown (23%). About half of the sample (44%) had at least one psychiatric comorbidity. The arithmetic mean of the Charlson Comorbidity Index was 1.5 (SD = 2.0). Approximately 8% of the patients were in the unknown marital status group, and they were younger, more likely to be female, more likely to be in the unknown-race group, and had less psychiatric and medical comorbidity.
TABLE 1.
Descriptive statistics for patient-level sample (N = 2363).
| Variable | Percent or Mean (SD) |
|---|---|
| Demographics | |
| Age | 48.2(9.1) |
| Gender | |
| Male | 95.2% |
| Female | 4.8% |
| Race | |
| Caucasian | 25.4% |
| African American | 45.0% |
| Other (majority = Hispanic) | 6.9% |
| Unknown | 22.7% |
| Marital status | |
| Married | 20.6% |
| Divorced | 27.3% |
| Unmarried | 44.3% |
| Unknown | 7.8% |
| Comorbidities | |
| Any psychiatric comorbidity | 43.9% |
| Anxiety | 11.8% |
| Bipolar | 7.8% |
| Major depression | 31.3% |
| Psychosis | 11.0% |
| PTSD | 17.8% |
| Charlson medical comorbidity index | 1.5(2.0) |
| Dependent variable | |
| Number of visits | 135.0(250.7) |
| Days in methadone treatment | 242.9(406.0) |
On average, patients attended 135 visits (median = 10 visits, SD = 250.7 visits) and stayed 243 days in methadone treatment (median = 32 days SD = 406 days). Fifty percent (n = 1,172) of the 2,363 veterans stayed for 30 days or less, 484 (20.5%) remained between 30 and 180 days, 222 (9.4%) remained between 180 and 365 days, and 485 (20.5%) were in methadone maintenance for more than a year. Eight percent (n = 207) of patients experienced a continuous episode of methadone treatment from their initial visit in FY 1999 to the end of FY 2002 when data were censored.
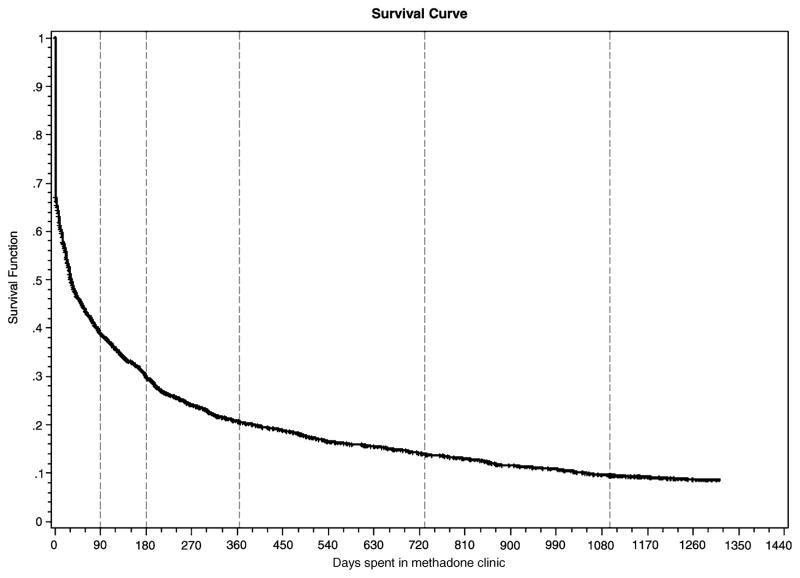
Results from the survival analysis, controlling for clustering within programs, are shown in Table 2 and Fig. 1. Table 2 demonstrates that the significant predictors for attrition from methadone treatment were age, race, and serious mental illness. There was a significant interaction between time and age in the model. During the very early portion of treatment (the first week), for one unit increase in age, the hazard of leaving methadone treatment increased about 1% indicating older people had shorter survival time. However, this trend reversed later in the program. At around one month into treatment, the hazard of leaving methadone treatment decreased about 3% for one unit increase in age, indicating that older people had a longer survival time. This trend continued throughout the remainder of treatment. For example, for one unit increase in age, the hazard of leaving treatment decreased by about 5% and 7%, respectively, at 8 months and at the study’s end (see details in Table 2).
TABLE 2.
Nonproportional hazard model for days in clinic for methadone treatment from October 1998 to July 2002.
| Fixed effect | Coefficient | Standard Error (based on Sandwich Variance) | p-Value | Hazard Ratio | 95% Hazard Ratio Confidence Interval |
|---|---|---|---|---|---|
| Age | −.0237 | .0031 | <.0001* | ||
| At time = 11 | 1.0133 | (1.0004, 1.0265) | |||
| At time = 32 | .9739 | (.9662, .9816) | |||
| At time = 253 | .9510 | (.9403, .9619) | |||
| At time = 1459 | .9321 | (.9157, .9489) | |||
| Age* time | −.0115 | .0011 | <.0001* | ||
| Male | −.0085 | .1056 | .9361 | .992 | (.806, 1.220) |
| Black | .3035 | .0557 | <.0001* | 1.355 | (1.214, 1.511) |
| Other race | .0590 | .0948 | .5336 | 1.061 | (.881, 1.277) |
| Unknown race | .5875 | .0689 | <.0001* | 1.800 | (1.572, 2.060) |
| Divorced | .0718 | .0638 | .2600 | 1.074 | (.948, 1.218) |
| Unmarried | .0411 | .0588 | .4844 | 1.042 | (.929, 1.169) |
| Unknown marital status | .0400 | .1014 | .6930 | 1.041 | (.853, 1.270) |
| Psychiatric comorbidity | |||||
| SMI | .1780 | .0632 | .0048 | 1.195 | (1.056, 1.352) |
| NonSMI | .0400 | .0484 | .4093 | 1.041 | (.947, 1.144) |
| Charlson medical comorbidity index | −.0187 | .0120 | .1189 | .982 | (.959, 1.005) |
p < .05
Time represents days in clinic, and 1, 32, 253, and 1,459 days are its 25%, 50%, 75%, and 100% percentiles, respectively. In models, time was transformed to log(days)-mean(log(days)).
Figure 1.
Survival function for days in methadone clinic. Dashed lines highlight time periods representing days in clinic for 3 months, 6 months, 1 year, two years, and three years.
Compared to Caucasians (the reference group), African Americans and the race-unknown group were more likely to leave methadone treatment early. Specifically, the hazard of departing methadone treatment for African Americans was 1.36 times the hazard for Caucasians, and the hazard for “race unknown” group was 1.80 times that for Caucasians (p < .05 for both). In addition, persons with a serious mental illness (psychosis or bipolar disorder) were more likely to leave treatment earlier than those without. Specifically, the hazard of leaving methadone treatment for the SMI group was 1.20 times that for those without SMI (p < .05). There was no significant effect of other psychiatric comorbidity or medical comorbidity.
DISCUSSION
This is the first retention study, that we are aware of, that utilizes data from a nationwide, multisite, population of participants in methadone treatment. Our findings indicated that younger age, being African American, having a serious mental illness, and having race recorded as unknown were associated with lower rates of retention in methadone treatment programs in this population of veterans. Our study, which adjusted for patient clustering by site, did not show any relation between gender or medical comorbidity and methadone treatment retention. African American status and psychiatric comorbidity (using a dichotomous dummy variable) was associated strongly with site location (data not shown); in an unadjusted model, a dummy variable indicating presence of any psychiatric comorbidity was significantly associated with reduced retention.
The association between older age and methadone treatment retention has been frequently demonstrated in past work (9, 11, 12, 18, 21–23). Our finding that African Americans have a lower rate of retention has also been demonstrated previously, though not in a primarily male VA population (12, 24–27). As noted in the introduction, the literature does not provide consistent findings with regards to the impact of psychiatric comorbidity on treatment retention—in either methadone or other modalities of substance abuse treatment. However, a previous study by coauthors of the current manuscript found serious mental illness (in this case, psychotic disorders alone) did predict early attrition from VA intensive outpatient clinics (39).
An interesting but difficult to explain finding was the fact that having race recorded as unknown was significantly and substantially associated with poor retention in methadone treatment. Over 21% of this sample has no recorded racial/ethnic status in the database. It is unclear why so many veterans chose not to report their racial/ethnic status or how this hesitance to report racial status might be related to treatment retention. Compared to the other groups, persons with no race recorded were more likely to be female, have marital status as unknown, and less likely to have a psychiatric comorbidity. More research is necessary to understand the potential traits or conditions for which “unknown race” is apparently serving as a proxy. The VA center responsible for the oversight of these national data sources, Veterans Information Resource Center (VIReC) (40), is aware of the missing data issue and has been exploring potential remedies.
Several limitations of the study should be noted. Many of the limitations result from our reliance on administrative data. Many important and established predictors of treatment retention in this population were not available for inclusion—e.g., dose of methadone received and prior episodes of treatment. Further, the coding scheme of the dataset blurs important distinctions. For example, we are aware that some methadone programs in the VA at the time were offering both “maintenance” and limited courses of treatment (e.g., 30- or 90-day programs leading to drug-free status), and the database does not make such a distinction in clinic designation. We do know that maintenance is the most popular opiate substitution treatment offered in the VA, but we cannot categorize with accuracy the percentage in this sample who did not attempt a maintenance regimen. This factor could be contributing to the unusually high rate of 30-day attrition that we found (50%). Another possible contributor to this unusual finding is that some VA sites also include patients receiving naltrexone and disulfiram in the “opiate substitution” stop code. That we excluded patients with primary alcohol use disorders should have minimized this potential confounder, but other cases of misclassification in the stop code could have occurred as well, contributing to the unusually high rate of early attrition. Other possible factors contributing to unusually high early attrition rate include the following: 1) some programs might not have been using high enough doses of methadone to maximize retention; 2) the programs could have varied on other quality indicators such as clinic hours, therapeutic alliance, and availability/quality of ancillary services; 3) as many dropped out within the first 5 days, many of these patients might not have started methadone at all as they left during an evaluation phase; and 4) travel distance to the clinics could have played a role as daily dosing is common early in a treatment episode.
Given the limitations of this study, more longitudinal studies using primary data collection, such as found in Villafranca et al. (41), are needed to fully explore factors related to retention. For the VA population specifically, further research is necessary to fully understand the relationship between race/ethnicity and treatment retention. Given that extended methadone treatment is associated with improved outcomes while patients remain in treatment, interventions are important at the clinic and individual patient level to assist veterans with remaining in care.
Acknowledgments
This study was funded by grants from the National Institute on Drug Abuse KO1 DA15102 (Curran) and VA/HSR&D IIR 98–006 (Booth and Curran).
Footnotes
Declaration of Interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
Contributor Information
Michael Mancino, Central Arkansas Veterans Healthcare System, North Little Rock, Arkansas, USA, and University of Arkansas for Medical Sciences Department of Psychiatry, Little Rock, Arkansas, USA
Geoffrey Curran, Central Arkansas Veterans Healthcare System, North Little Rock, Arkansas, USA, and University of Arkansas for Medical Sciences Department of Psychiatry, Little Rock, Arkansas, USA
Xiaotong Han, Central Arkansas Veterans Healthcare System, North Little Rock, Arkansas, USA, and University of Arkansas for Medical Sciences Department of Psychiatry, Little Rock, Arkansas, USA
Elise Allee, Central Arkansas Veterans Healthcare System, North Little Rock, Arkansas, USA, and University of Arkansas for Medical Sciences Department of Psychiatry, Little Rock, Arkansas, USA
Keith Humphreys, Veterans Affairs Palo Alto Health Care System, Palo Alto, California, USA, and Stanford University, Palo Alto, California, USA
Brenda M. Booth, Central Arkansas Veterans Healthcare System, North Little Rock, Arkansas, USA, and University of Arkansas for Medical Sciences Department of Psychiatry, Little Rock, Arkansas, USA
References
- 1.Dole V, Nyswander ME, Warner A. Successful treatment of 750 criminal addicts. JAMA. 1968;206:2708–2711. [PubMed] [Google Scholar]
- 2.Simpson DD, Savage LJ, Lloyd MR. Follow-up evaluation of treatment abuse during 1969 to 1972. Arch Gen Psychiatry. 1979;36:772–780. doi: 10.1001/archpsyc.1979.01780070050005. [DOI] [PubMed] [Google Scholar]
- 3.McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, Pettinati H, Argeriou M. The fifth edition of the Addiction Severity Index. J Subst Abuse Treat. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- 4.Marsch L. The efficacy of methadone maintenance interventions in reducing illicit opiate use, HIV risk behavior and criminality: A meta-analysis. Addiction. 1998;93:515–532. doi: 10.1046/j.1360-0443.1998.9345157.x. [DOI] [PubMed] [Google Scholar]
- 5.Gossop M, Marsden J, Stewart D, Treacy S. Outcomes after methadone maintenance and methadone reduction treatments: Two-year follow-up results from the National Treatment Outcome Research Study. Drug Alcohol Depend. 2001;62:255–264. doi: 10.1016/s0376-8716(00)00211-8. [DOI] [PubMed] [Google Scholar]
- 6.Kwiatkowski CF, Booth RE. Methadone maintenance as HIV risk reduction with street-recruited injecting drug users 2001. J Acquir Immune Defic Syndr. 26:483–489. doi: 10.1097/00126334-200104150-00014. [DOI] [PubMed] [Google Scholar]
- 7.Simpson DD, Joe GW, Bracy SA. Six-year follow-up of opioid addicts after admission to treatment. Arch Gen Psychiatry. 1982;39:1318–1323. doi: 10.1001/archpsyc.1982.04290110070012. [DOI] [PubMed] [Google Scholar]
- 8.Ball JC, Lange WR, Myers CP, Friedman SR. Reducing the risk of AIDS through methadone maintenance. J Health Soc Behav. 1998;29:214–226. [PubMed] [Google Scholar]
- 9.Rhoades HM, Creson D, Elk R, Schmitz J, Grabowski J. Retention, HIV Risk, and illicit drug use during treatment: Methadone dose and visit frequency. Am J Pub Health. 1998;88:34–39. doi: 10.2105/ajph.88.1.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McLellan AT, Luborsky L, O’Brien CP, Woody GE. An improved diagnostic evaluation Instrument for substance abuse patients: The addiction severity index. J Nerv Ment Dis. 1980;168:26–33. doi: 10.1097/00005053-198001000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Magura S, Nwakeze PC, Demsky S. Pre- and in-treatment predictors of retention in methadone treatment using survival analysis. Addiction. 1998;93:51–60. doi: 10.1046/j.1360-0443.1998.931516.x. [DOI] [PubMed] [Google Scholar]
- 12.Saxon AJ, Wells EA, Fleming C, Jackson TR, Calsyn DA. Pre-treatment characteristics, program philosophy and level of ancillary services as predictors of methadone maintenance treatment outcome. Addiction. 1996;91:1197–1209. doi: 10.1046/j.1360-0443.1996.918119711.x. [DOI] [PubMed] [Google Scholar]
- 13.Rothbard A, Alterman A, Rutherford M, Liu F, Zelinski S, McKay J. Revisiting the effectiveness of methadone treatment on crime reductions in the 1990s. J Sub Abuse Treat. 1999;16:329–335. doi: 10.1016/s0740-5472(98)00050-6. [DOI] [PubMed] [Google Scholar]
- 14.Keen J, Rowse G, Mathers N, Campbell M, Seivewright N. Can methadone maintenance for heroin-dependent patients retained in general practice reduce criminal conviction rates and time spent in prison? Br J Gen Pract. 2000;50:48–49. [PMC free article] [PubMed] [Google Scholar]
- 15.Hartel DM, Schoenbaum EE. Methadone treatment protects against HIV infection: two decades of experience in the Bronx, New York City. Public Health Records. 1998;113:107–115. [PMC free article] [PubMed] [Google Scholar]
- 16.Hubbard RL, Craddock SG, Cavanaugh ER, Flynn PM, Anderson J, Etheridge M. Overview of 1-year follow-up outcomes in the Drug Abuse treatment Outcome Study (DATOS) Psychol Addict Behav. 1997;11:261–278. [Google Scholar]
- 17.Simpson DD, Joe GW, Brown SS. Treatment retention and follow-up outcomes in the Drug Abuse Outcome Treatment Study (DATOS) Psychol Addict Behav. 1997;11:294–307. [Google Scholar]
- 18.MacGowan RJ, Swanson NM, Brackbill RM, Rugg DL, Barker T, Molde S. Retention in methadone maintenance treatment programs, Connecti-cut and Massachusetts, 1990–1993. J Psychoactive Drugs. 1996;28:259–265. doi: 10.1080/02791072.1996.10472487. [DOI] [PubMed] [Google Scholar]
- 19.Darke S, Ross J, Teesson M, Ali R, Cooke R, Ritter, Lynskey M. Factors associated with 12 months continuous heroin abstinence: findings from the Australian Treatment Outcome Study (ATOS) J Subst Abuse Treat. 2005;28:255–263. doi: 10.1016/j.jsat.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 20.Schiff M, Levit S, Moreno RC. Retention and illicit drug use among methadone patients in Israel: a gender comparison. Addict Behav. 2007;32(10):2108–2119. doi: 10.1016/j.addbeh.2007.01.010. [DOI] [PubMed] [Google Scholar]
- 21.Deck D, Carlson MJ. Retention in Publicly Funded Methadone Maintenance Treatment in Two Western States. J Behav Health Serv Res. 2005;32:43–60. doi: 10.1007/BF02287327. [DOI] [PubMed] [Google Scholar]
- 22.Anderson JF, Warren LD. Client retention in the British Columbia Methadone Program, 1996–1999. Can J Public Health. 2004;95:104–109. doi: 10.1007/BF03405776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Strike CJ, Gnam W, Urbanoski K, Fischer B, Marsh DC, Millson M. Factors predicting 2-year retention in methadone maintenance treatment for opioid dependence. Addict Behav. 2005;30:1025–1028. doi: 10.1016/j.addbeh.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 24.Mertens JR, Weisner CM. Predictors of substance abuse treatment retention among women and men in an HMO. Alcohol Clin Exp Res. 2000;24:1525–1533. [PubMed] [Google Scholar]
- 25.Sorensen JL, Gibson D, Bernal G, Deitch D. Methadone applicant dropouts: impact of requiring involvement of friends or family treatment. Int J Addictions. 1985;20:1273–1280. doi: 10.3109/10826088509056363. [DOI] [PubMed] [Google Scholar]
- 26.Joe GW, Simpson DD, Hubbard RL. Treatment predictors of tenure in methadone maintenance. J Subst Abuse. 1991;3:73–84. doi: 10.1016/s0899-3289(05)80007-0. [DOI] [PubMed] [Google Scholar]
- 27.Steer RA. Psychosocial correlates of retention in methadone maintenance. Int J Addictions. 1980;15:1003–1009. doi: 10.3109/10826088009040074. [DOI] [PubMed] [Google Scholar]
- 28.Favrat B, Rao S, O’Connor PG, Schottenfeld A staging system to predict prognosis among methadone maintenance patients, based on admission characteristics. J Subst Abuse. 2002;23:233–244. doi: 10.1080/08897070209511496. [DOI] [PubMed] [Google Scholar]
- 29.Gaughwin M, Solomon P, Ali R. Correlates of retention on the South Australian Methadone Program 1981–1991. Aust N Z J Public Health. 1998;22:771–776. doi: 10.1111/j.1467-842x.1998.tb01491.x. [DOI] [PubMed] [Google Scholar]
- 30.Maddux JF, Prihoda TJ, Vogtsberger KN. The relationship of methadone dose and other variables to outcomes of methadone maintenance. Am J Addictions. 1997;6:246–255. [PubMed] [Google Scholar]
- 31.Caplehorn JR, Bell J. Methadone dosage and retention of patients in maintenance treatment. Med J Aust. 1991;154:195–199. [PubMed] [Google Scholar]
- 32.Amato L, Davoli M, Perucci CA, Ferri M, Faggiano F, Mattick RP. An overview of systematic reviews of the effectiveness of opiate maintenance therapies: Available evidence to inform clinical practice and research. J Subst Abuse Treat. 2005;28:321–329. doi: 10.1016/j.jsat.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 33.Cacciola JS, Rutherford MJ, Alterman AI, McKay JR, Snider EC. Personality disorders and treatment outcome in methadone maintenance patients. J Nerv Ment Disease. 1996;184:234–239. doi: 10.1097/00005053-199604000-00006. [DOI] [PubMed] [Google Scholar]
- 34.Cacciola JS, Alterman A, Rutherford MJ, McKay JR, Mulvaney FD. The relationship of psychiatric comorbidity to treatment outcomes in methadone maintained patients. Drug Alcohol Depend. 2001;61:271–280. doi: 10.1016/s0376-8716(00)00148-4. [DOI] [PubMed] [Google Scholar]
- 35.Maremmani I, Zolesi O, Aglietti, Marini G, Tagliamonte A, Shinderman M, Maxwell S. Methadone dose and retention during treatment of heroin addicts with Axis I psychiatric comorbidity. J Addict Dis. 2000;19:29–41. doi: 10.1300/J069v19n02_03. [DOI] [PubMed] [Google Scholar]
- 36.Milby JB, Sims MK, Khuder S, Schumacher JE, Huggins N. Psychiatric comorbidity: Prevalence in methadone maintenance treatment. Am J Drug Alcohol Abuse. 1996;22:95–107. doi: 10.3109/00952999609001647. [DOI] [PubMed] [Google Scholar]
- 37.Hubbard RL, Craddock SG, Anderson J. Overview of 5-year follow-up outcomes in the drug abuse treatment outcome studies (DATOS) J Subst Abuse Treat. 2003;25:125–134. doi: 10.1016/s0740-5472(03)00130-2. [DOI] [PubMed] [Google Scholar]
- 38.Charlson M, Pompie P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 39.Curran GM, Stecker T, Han X, Booth BM. Individual and program predictors of attrition from VA substance use treatment. J Behav Health Serv Res. 2009;36:25–34. doi: 10.1007/s11414-007-9093-z. [DOI] [PubMed] [Google Scholar]
- 40.Veterans Information Resource Center. (VIReC) Available at http://www.virec.research.va.gov/References/DataIssuesBrief/November2009/DIB-0911er.pdf.
- 41.Villafranca SW, McKellar JD, Trafton JA, Humphreys K. Predictors of retention in methadone programs: A signal detection analysis. Drug Alcohol Depend. 2006;83:218–224. doi: 10.1016/j.drugalcdep.2005.11.020. [DOI] [PubMed] [Google Scholar]