Abstract
Purpose
The aim of this study was to investigate the effect of the autologous blood injection (ABI) for chronic recurrent temporomandibular joint (TMJ) dislocation using magnetic resonance imaging (MRI).
Materials and Methods
ABI was applied to 14 patients who had chronic recurrent TMJ dislocation. MRIs of the patients were taken and compared before and one month after the injection.
Results
All of the patients had no dislocations of their TMJs on clinical examination one month after the injection. In the pre-injection, unilateral or bilateral TMJ dislocations were observed on MRIs in all patients. One month after the injection, TMJ dislocations were not observed in MRI evaluation of any patients. A significant structural change that caused by ABI was not observed.
Conclusion
The procedure was easy to perform and it caused no foreign body reaction. However, it was unclear how the procedure prevented the dislocation.
Keywords: Temporomandibular Joint, Dislocations, Magnetic Resonance Imaging
Introduction
Dislocation of the temporomandibular joint (TMJ) occurs when one or both mandibular condyles are displaced in front of the articular eminence. It may be reducible when it returns spontaneously to the glenoid cavity, or irreducible when one or two condyles remain dislocated. In this position, the mouth remains open due to the action of the elevator muscles with or without lateral deviation, depending on whether the dislocation is unilateral or bilateral.1,2 Acute mandibular dislocation is usually managed by manually pressing the mandible downwards and then pulling it back upwards in an attempt to try relocating the condyle in the glenoid fossa. If the condyle continues to dislocate several times, it is described as chronic recurrent TMJ dislocation. Dislocation of TMJ is generally of unknown origin, while several theories put forward to explain its onset. It is commonly associated with poor development of the articular fossa, laxity of the temporomandibular ligament or joint capsule, and excessive activity of the lateral pterygoid and infrahyoid muscles due to drug use or disease. Additionally some disorders of collagen metabolism such as ligamentous hyperlaxity and Ehler-Danlos syndrome might be related.1-3 There were well documented surgical and nonsurgical treatment protocols of chronic recurrent TMJ dislocation in the literatures.1,4 Recently autologous blood injection (ABI) to TMJ has been applied for the treatment of chronic recurrent TMJ dislocation. The procedure is easy to perform and it causes no foreign body reaction. There have been some successful clinical studies in the literatures. On the other hand, there were some concerns about the procedure such as fibrous or bony ankylosis and articular cartilage degeneration. The aim of this study was to evaluate the pathophysiology of the ABI and observe the mechanism of the procedure using magnetic resonance imaging (MRI).
Materials and Methods
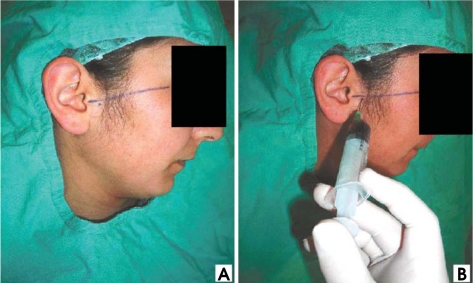
Fourteen patients (5 males) between the ages of 17 and 74 who had chronic recurrent TMJ dislocation visited Fatih University Hospital from the year of 2009 to 2010 (Table 1). They were diagnosed with chronic recurrent TMJ dislocation based on the clinical and radiographic criteria. Six of the fourteen patients had bilateral chronic recurrent TMJ dislocation. The patients' maximal mouth opening (just before dislocation) measured between maxillary and mandibular incisal edges, ranged from 36 to 48 mm, with an average of 41 mm. All of these patients complained of dislocation of their joints at least twice a week. No patients had other TMJ disorders such as disc displacement or osteoarthritis. The patients underwent ABİ (6 bilateral injections). Local anesthesia was given to the auriculatemporal nerve. The articular fossa was assumed as located at a point 10 mm anterior to the tragus of the ear and 2 mm inferior to the tragal-canthal line. Five mL blood was withdrawn from the patients' anticubital fossa. Four mL blood with a 21-gauge needle was injected in the articular cavity and 1mL was injected in the pericapsular tissue (Fig. 1). After the completion of the injection, an elastic bandage was applied and left for 24 hours to constrain the joint movements. All of the patients were scanned before and 1 month after the therapy with a 1.5 T MRI scanner (Achieva; Philips Medical Systems, Best, The Netherlands) using a multichannel head coil. Both of the joints were imaged in each patient. First, the axial scout section was used to localize the mandibular condyle. Based on the axial scout view, oblique sagittal T1-weighted spin echo (SE) sequences were acquired (repetition time [TR]: 450 msec, echo time [TE]: 15 msec, matrix: 180×320, slice thickness: 3 mm, field of view [FOV]: 130 mm, number of excitation [NEX]: 3) in closed mouth position. Eight sagittal images for each joint were obtained. Subsequently, oblique sagittal T1 3-dimensional water only WATS images (TR: 30 msec, TE: 3.9 msec, matrix: 180×256, slice thickness: 1 mm, FOV: 130 mm, NEX: 3, FA: 20°) were acquired in closed mouth position. Twenty-five images were acquired for each TMJ. Also, oblique sagittal T2-weighted fast spin echo (FSE) images (MOVIE) (TR: 131 msec, TE: 14 msec, matrix: 240×192, slice thickness: 3 mm, FOV: 160 mm, NEX: 1, FA: 30°) were acquired in six different mouth opening positions. The patients have been instructed to open their mouth gradually.
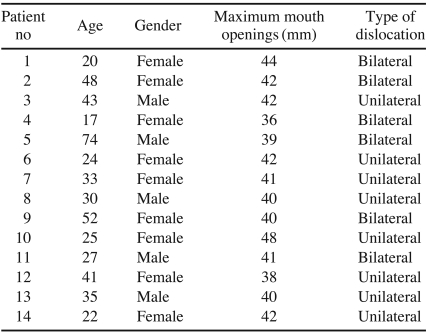
Table 1.
Patients treated with autologous blood injection
Fig. 1.
A. The reference line for locating the articular fossa. B. Autologous blood injection.
Results
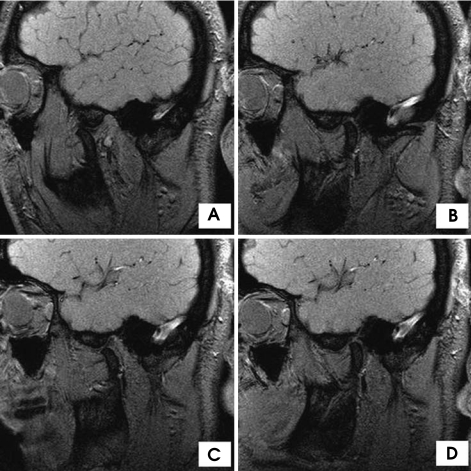
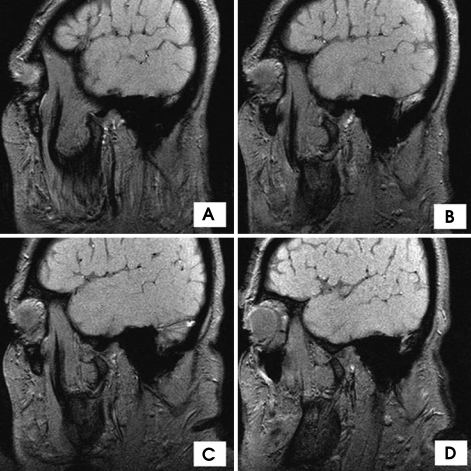
All the patients tolerated the procedure well. There were no infections or any other complications in any of the patients. The post operative pain was tolerable in all the patients and lasted for only few days after the procedure. During four weeks after the operation, all the patients had no dislocations of their TMJs, while one patient showed a recurrent dislocation in the second month after the injection. Two patients with unilateral TMJ dislocation mentioned that the incidence of dislocation had been reduced, but it had not been completely disappeared. After the study, ABI was repeated by the request of the patients who had failed treatment and achieved good results. In pre-injection MRI evaluation, there was no articular cartilage degeneration, disc displacement, or osteoarthritis in any patients. Before administration of the injection, it was identified that the patients had unilateral or bilateral condyles anterior to the eminence with their mouths in the open position. In the first month after the injection, MRIs of all patients taken with the open-mouth position revealed that the condyle was either at the apex of the eminence or posterior to it (Figs. 2 and 3). However, there was no structural variation that described the prevention of the dislocations such as fibrosis in MRI findings. Hematoma was disappeared without any alteration of the joint tissues.
Fig. 2.
Case 1: MRI images of the left TMJ. A. Open-mouth position before injection. B. Close-mouth position before injection. C. Open-mouth position after injection. D. Close-mouth position after injection.
Fig. 3.
Case 2: MRI images of the open-mouth position. A. The left TMJ before injection. B. The right TMJ before injection. C. The left TMJ after injection. D. The right TMJ after injection.
Discussion
Chronic recurrent TMJ dislocation is a painful and alarming illness that patients usually cannot reduce dislocated joints by themselves and need a doctor or an infirmarian for the treatment. Non surgical methods are usually first applied to the patients before decision of surgery. There were some successful nonsurgical treatment models described in the literatures such as injection of a sclerosing solution into the joint cavity (tincture of iodine, alcohol and sodium psylliate). However, many side effects and the possible risk of facial paralysis or traumatic arthritis have hindered its widespread usage.1,5 Another procedure with less side effects is the use of botox.4 The toxin temporarily causes denervation of the muscles that draw the chin down. The muscle of choice for injection is the lateral pterygoid muscle. In this way, the displacement of the condyle is prevented even when the mouth is opened excessively.6,7 Recently ABI has been used for the treatment of chronic recurrent TMJ dislocation. It can be thought that ABI is more advantageous because of the less complication probability regarding to the other nonsurgical methods.
ABI can be readily carried out under local anesthesia in outpatient clinic and the treatment can be performed repeatedly with minimal complications.5 There were some studies that obtained good results regarding this method. However, it has not gained much popularity as the mechanism of action has not been explicitly defined. The pathophysilogy of the procedure has not been introduced with a comment. Additionally there are some concerns with this procedure such as fibrous or bony ankylosis and articular cartilage degeneration.1,5,8 In our knowledge, this was the first study that evaluated the effect of the ABI procedure by MRI.
Machon et al1 mentioned that ABI for chronic TMJ dislocation was first reported in the German literature in 1964 by Brachmann. He had treated 60 patients using this technique and declared good results. Schulz treated 16 patients in 1973 by ABI to the affected TMJ twice a week for 3 weeks followed by immobilization via intermaxillary fixation for 4 weeks. The symptoms were disappeared in 10 patients at 1-year follow-up. In 1981, Jacobbi-Hermanns published the experience with 19 patients who received only 1 ABI and had intermaxillary fixation for 14 days. At 18 months follow-up, 17 patients were symptom free.1 Hasson reported the successfully treated 3 patients with ABI (4 cc superior joint space and 1 cc pericapsular tissues). After the treatment, elastic bandage was applied and left for the first 24 hours.2 Kato et al presented the treatment of chronic recurrent TMJ dislocation by ABI (3 cc superior joint space and 1 cc pericapsular tissues) in an 84-year-old female under local anesthesia. The mandible had been fixed with a bandage and the use of bandage had been continued for 1 month as a precaution.5 Pinto et al successfully treated an 83-year-old female patient by injecting 10 cc of ABI into the superior joint space and the periarticular tissue.9 They used a face lift bandage for one month after the procedure. Machon et al reported that 20 among 25 patients were treated successfully with 1 or 2 injections (2 cc in the superior joint space and 1 cc in the pericapsular tissue). Based on their number of patients, there was no benefit after 2 injections of blood to the TMJ, and surgical intervention should then be pursued.1 In Daif's study, 30 patients having chronic recurrent TMJ dislocation were randomly divided into 2 equal groups (15 patients in each). Group A was treated only by 2 cc autologous blood injection into the superior joint space (SJS), whereas group B received 2 cc ABI to the SJS and 1 cc in the pericapsular tissues (PT). After the completion of the injection procedures, an elastic bandage was applied and left for the first 24 hours. At the end of the follow-up period of 1 year, the results of the current study showed that the ABI to the SJS and PT gave a higher success rate (80%) than its injection only into the SJS (60%). Moreover, the decrease of maximal mouth opening of group B was larger than that of group A. Also, the digital radiographic imaging of the joints in group B only showed the condylar head posterior to the articular eminence in open position, instead of being anterior to it before the injection. In both groups, no destructive changes to the bony components of the joint have been observed.8
The principal aim of the ABI is the limitation of movement of the mandible. It is thought that the mechanism occurs by the formation of a local recess of fibrous tissue in the pericapsular space during the wound healing process. The injection given into the cavity over the joint leads to its formation of adhesions in the cavity. However, this anticipated mechanism has not been studied experimentally or radiologically. The studies mentioned above have just approved the success of the procedure by clinical observations. Some researchers claimed that the contact of cartilage with blood caused the changes in chondrocyte metabolism and thus cartilage destruction.10,11 Other studies showed that these changes were temporary, not permanent. It is thought that ABI procedure could cause articular degeneration and subsequent arthritis.5
The pathophysiology of blood injection resembles that of knee or elbow joint bleeding. Initially, the capsule swells and stretches. In the next few hours or days, an inflammatory reaction starts via mediators released from neighboring platelets, wounded and dead cells. As a result, neighboring tissues swell and the joint has difficulty in motion. Thereafter, organized blood clots and fibrous tissue structures lead to joint stiffness. These tissues cause permanent limitation in joint motion. The contact of cartilage with blood leads to impairment of the cartilage matrix cycle. The injected blood artificially triggers an inflammatory reaction, which in turn leads to fibrosis, adhesions and scars in the neighboring tissues. Immobilization prevents the early tension produced by new fibrous tissue.1 In the experimental studies on the joints concerning injection of blood into TMJs, there were no late period pathologies even in cases of frequent injections. The impairment in the cartilage matrix which could be seen in the early period recovered to complete normal state later.12 Pathologies in late period have only been identified in patients who frequently bore their weight on the extremity joints.13,14 Considering their studies, we performed the MRI investigation to determine the early effect of the procedure after a month. Our previous experimental study using rabbits also showed that there was no pathology in their TMJs on the histopathological evaluation 1 month after ABI.15
The relatively simple procedures of this method, the very low amount of blood involved (the amount is the same as that in open surgery), the restriction of movement after the procedure, and the prevention of weight bearing on the mandible might be the possible reasons for the occurrence of no complication. Some studies applied controlled-exercise programs to patients to potentially limit mandibular movement after the procedure.1
In this study ABİ was applied to 14 patients according to the methods. At the end of the 1 year follow-up period, their symptoms were improved in 13 patients successfully. The results of the treatment were evaluated by physical examination and together with MRI evaluation. These results of treatment were in agreement with the previous studies as mentioned above. However, contrary to the studies mentioned above, a structural change such as fibrosis or other mechanisms were not observed on MRI.
In conclusion, the ABI in the treatment of chronic recurrent TMJ dislocation had advantages such as no requirement of dissection, few or no post operative complications such as facial nerve injury, loss of sensation, swelling, infection and pain, no necessity to stay in hospital, and easiness of administration under local anesthesia. To sum up, ABI for patients with chronic recurrent TMJ dislocation was an effective, safe, and simple technique that could be used before surgery. However, more clinical and experimental studies should be performed to evaluate the efficacy of the treatment modality and to describe the pathophysiology of the treatment.
References
- 1.Machon V, Abramowicz S, Paska J, Dolwick MF. Autologous blood injection for the treatment of chronic recurrent temporomandibular joint dislocation. J Oral Maxillofac Surg. 2009;67:114–119. doi: 10.1016/j.joms.2008.08.044. [DOI] [PubMed] [Google Scholar]
- 2.Hasson O, Nahlieli O. Autologous blood injection for treatment of recurrent temporomandibular joint dislocation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:390–393. doi: 10.1067/moe.2001.116602. [DOI] [PubMed] [Google Scholar]
- 3.Oztan HY, Ulusal BG, Turegun M, Deveci M. Titanium screw implantation to the articular eminence for the treatment of chronic recurrent dislocation of the temporomandibular joint. Int J Oral Maxillofac Surg. 2005;34:921–923. doi: 10.1016/j.ijom.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 4.Ziegler CM, Haag C, Mühling J. Treatment of recurrent temporomandibular joint dislocation with intramuscular botulinum toxin injection. Clin Oral Investig. 2003;7:52–55. doi: 10.1007/s00784-002-0187-y. [DOI] [PubMed] [Google Scholar]
- 5.Kato T, Shimoyama T, Nasu D, Kaneko T, Horie N, Kudo I. Autologous blood injection into the articular cavity for the treatment of recurrent temporomandibular joint dislocation: a case report. J Oral Sci. 2007;49:237–239. doi: 10.2334/josnusd.49.237. [DOI] [PubMed] [Google Scholar]
- 6.Fu KY, Chen HM, Sun ZP, Zhang ZK, Ma XC. Long-term efficacy of botulinum toxin type A for the treatment of habitual dislocation of the temporomandibular joint. Br J Oral Maxillofac Surg. 2010;48:281–284. doi: 10.1016/j.bjoms.2009.07.014. [DOI] [PubMed] [Google Scholar]
- 7.Vázquez Bouso O, Forteza González G, Mommsen J, Grau VG, Rodríguez Fernández J, Mateos Micas M. Neurogenic temporomandibular joint dislocation treated with botulinum toxin: report of 4 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:e33–e37. doi: 10.1016/j.tripleo.2009.10.046. [DOI] [PubMed] [Google Scholar]
- 8.Daif ET. Autologous blood injection as a new treatment modality for chronic recurrent temporomandibular joint dislocation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:31–36. doi: 10.1016/j.tripleo.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 9.Pinto AS, McVeigh KP, Bainton R. The use of autologous blood and adjunctive 'face lift' bandage in the management of recurrent TMJ dislocation. Br J Oral Maxillofac Surg. 2009;47:323–324. doi: 10.1016/j.bjoms.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 10.Lafeber FP, Miossec P, Valentino LA. Physiopathology of haemophilic arthropathy. Haemophilia. 2008;14(Suppl 4):3–9. doi: 10.1111/j.1365-2516.2008.01732.x. [DOI] [PubMed] [Google Scholar]
- 11.Roosendaal G, Lafeber FP. Blood-induced joint damage in hemophilia. Semin Thromb Hemost. 2003;29:37–42. doi: 10.1055/s-2003-37938. [DOI] [PubMed] [Google Scholar]
- 12.Roosendaal G, TeKoppele JM, Vianen ME, van den Berg HM, Lafeber FP, Bijlsma JW. Blood-induced joint damage: a canine in vivo study. Arthritis Rheum. 1999;42:1033–1039. doi: 10.1002/1529-0131(199905)42:5<1033::AID-ANR24>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- 13.Hooiveld MJ, Roosendaal G, Jacobs KM, Vianen ME, van den Berg HM, Bijlsma JW, et al. Initiation of degenerative joint damage by experimental bleeding combined with loading of the joint: a possible mechanism of hemophilic arthropathy. Arthritis Rheum. 2004;50:2024–2031. doi: 10.1002/art.20284. [DOI] [PubMed] [Google Scholar]
- 14.Hooiveld M, Roosendaal G, Vianen M, van den Berg HM, Bijlsma J, Lafeber F. Blood-induced joint damage: longterm effects in vitro and in vivo. J Rheumatol. 2003;30:339–344. [PubMed] [Google Scholar]
- 15.Candrl C, Yüce S, Yldrm S, Sert H. Histopathologic evaluation of autologous blood injection to the temporomandibular joint. J Craniofac Surg. 2011;22:2202–2204. doi: 10.1097/SCS.0b013e3182326f99. [DOI] [PubMed] [Google Scholar]