Abstract
Collagen VI is a major extracellular matrix (ECM) protein with a critical role in maintaining skeletal muscle functional integrity. Mutations in COL6A1, COL6A2 and COL6A3 genes cause Ullrich Congenital Muscular Dystrophy (UCMD), Bethlem Myopathy, and Myosclerosis. Moreover, Col6a1−/− mice and collagen VI deficient zebrafish display a myopathic phenotype. Recently, two additional collagen VI chains were identified in humans, the α5 and α6 chains, however their distribution patterns and functions in human skeletal muscle have not been thoroughly investigated yet. By means of immunofluorescence analysis, the α6 chain was detected in the endomysium and perimysium, while the α5 chain labeling was restricted to the myotendinous junctions. In normal muscle cultures, the α6 chain was present in traces in the ECM, while the α5 chain was not detected. In the absence of ascorbic acid, the α6 chain was mainly accumulated into the cytoplasm of a sub-set of desmin negative cells, likely of interstitial origin, which can be considered myofibroblasts as they expressed α-smooth muscle actin. TGF-β1 treatment, a pro-fibrotic factor which induces trans-differentiation of fibroblasts into myofibroblasts, increased the α6 chain deposition in the extracellular matrix after addition of ascorbic acid. In order to define the involvement of the α6 chain in muscle fibrosis we studied biopsies of patients affected by Duchenne Muscular Dystrophy (DMD). We found that the α6 chain was dramatically up-regulated in fibrotic areas where, in contrast, the α5 chain was undetectable. Our results show a restricted and differential distribution of the novel α6 and α5 chains in skeletal muscle when compared to the widely distributed, homologous α3 chain, suggesting that these new chains may play specific roles in specialized ECM structures. While the α5 chain may have a specialized function in tissue areas subjected to tensile stress, the α6 chain appears implicated in ECM remodeling during muscle fibrosis.
Keywords: Collagen VI, Skeletal muscle, Myotendinous junctions, Fibrosis, Duchenne muscular dystrophy
Highlights
► We study collagen VI alpha 5 and alpha 6 chains expression in human skeletal muscle. ► ► We show that alpha 5 chain is exclusively present at the myotendinous junctions. ► We show that alpha 6 chain is present in the ECM but not at the basement membranes. ► We show that alpha 6 chain increases in Duchenne muscular dystrophy muscle fibrosis. ► We hypothesize the possible formation of alpha1-2-6 or alpha1-2-5 chains trimers.
1. Introduction
Collagen VI is an extracellular matrix protein which forms a distinct microfibrillar network in most connective tissues. It was long considered to consist of three genetically distinct α-chains (α1, α2 and α3), secreted into the extracellular matrix where they form an extended microfilamentous network (Chu et al., 1988; Knupp and Squire, 2001). The collagen VI α1, α2 and α3 chains form heterotrimeric monomers that are assembled intracellularly to dimers and tetramers. After secretion, filaments are formed by end to end interactions of the pre-assembled tetramers, forming characteristic beaded filaments (Bruns, 1984) as visualized by the rotary shadowing electron microscopy technique (von der Mark et al., 1984; Sabatelli et al., 2001).
Collagen VI has a critical role in maintaining skeletal muscle functional integrity; in fact, mutations in the COL6A1, COL6A2, and COL6A3 genes cause a group of inherited muscular dystrophies, namely Ullrich congenital muscular dystrophy (UCMD) (Camacho Vanegas et al., 2001), Bethlem myopathy (BM) (Jöbsis et al., 1996; Lampe and Bushby, 2005; Gualandi et al., 2009), and Myosclerosis myopathy (Merlini et al., 2008). Col6a1−/− mice show a complete absence of collagen VI chains (Bonaldo et al., 1998; Gara et al., 2008) and display a myopathic phenotype associated with an impairment of the autophagy flux that determines the presence of dilated sarcoplasmic reticulum and abnormal mitochondria: these present a latent dysfunction, that causes an increased apoptosis of muscle fibers (Irwin et al., 2003; Grumati et al., 2010). Moreover, zebrafish models of the human collagen VI myopathies develop myopathy and display mitochondrial ultrastructural changes along with an increased rate of spontaneous apoptosis (Telfer et al., 2010).
Collagen VI is also thought to be implicated in tissue remodelling and wound healing, as variations in collagen VI expression have been reported in many pathological conditions, like muscle and liver fibrosis (Freise et al., 2009). Fibrosis is the most conspicuous pathological change in dystrophic muscles; it is characterized by excessive accumulation of collagens and other ECM components, including collagen VI (Zanotti et al., 2007) and is regulated by mechanisms involving cell–cell and cell–matrix interactions, as well as by factors secreted into the ECM. TGF-β1 is one of the most potent regulators of tissue wound healing and fibrosis (Cutroneo, 2007). It is highly expressed in regenerating muscle after injury and in dystrophic muscles, including Duchenne muscular dystrophy patients and mdx mice (Zhou et al., 2006), carrying mutations in the dystrophin gene, and in MDC1A, caused by mutations in LAMA2 gene (Zanotti and Mora, 2006).
Recently, three novel collagen VI chains, α4, α5 and α6 were identified (Fitzgerald et al., 2008; Gara et al., 2008). The new chains structurally resemble the collagen VI α3 chain, each of them consisting of seven VWA domains followed by a collagenous domain, two or three C-terminal VWA domains and chain specific domains. In mouse the novel chains show a differential and restricted expression (Gara et al., 2011). Since Col6a1 null mice do not deposit the new collagen VI chains in the extracellular matrix, it was proposed that their assembly and secretion requires the presence of the α1 chain and that the new chains may substitute for the α3 chain, probably forming (α1 α2 and α4), (α1 α2 and α5) or (α1 α2 and α6) heterotrimers (Gara et al., 2008, 2011). Due to a large scale pericentric inversion, the human COL6A4 gene on chromosome 3 is broken into two pieces and has become a non-processed pseudogene (Wagener et al., 2009). In humans, COL6A5 mRNA expression is restricted to a few tissues, including lung, testis, and colon. In contrast, the COL6A6 mRNA was found in a wide range of fetal and adult tissues, including lung, kidney, liver, spleen, thymus, heart, skeletal muscle, pancreas, testis and uterus (Fitzgerald et al., 2008). Collagen VI α5 chain protein expression in humans was so far studied only in skin, where it was found in a narrow zone just below the dermal epidermal basement membrane and around blood vessels (Sabatelli et al., 2011). It was earlier reported that the α5 chain is present in the epidermis (Söderhäll et al., 2007), but this observation has been challenged (Sabatelli et al., 2011). Collagen VI α6 protein expression in humans was found in kidney, skeletal and cardiac muscle, lung, blood vessels, pancreas, spleen and cartilage (Fitzgerald et al., 2008). However, collagen VI dependent disease is mainly manifested in muscle and the precise localization of the novel chains has not been comprehensively studied in this tissue yet. The discovery of two additional collagen VI chains in humans adds a layer of complexity to collagen VI function in the extracellular matrix (Fitzgerald et al., 2008; Gara et al., 2008).
To provide insight into the expression and function of the α5 and α6 collagen VI chains in human skeletal muscle, we studied these proteins and the corresponding mRNAs in normal muscle tissue and cell cultures, and in Duchenne Muscular Dystrophy (DMD) muscle with marked fibrosis, arisen independently from any mutation in the collagen VI genes.
2. Results
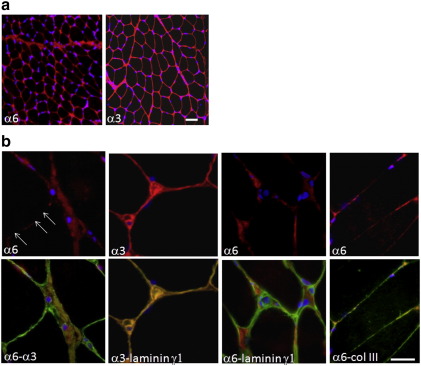
2.1. Immunofluorescence analysis of the collagen VI α6 chain in normal skeletal muscle
To assess the tissue distribution of the α6 chain in human skeletal muscle, frozen sections of tibialis anterior and soleus, obtained from normal subjects were stained with an antibody against the α6 chain. The α6 chain localized both in the perimysium and endomysium, with a less homogeneous pattern in the endomysium as compared to labeling obtained for the homologous α3 chain (Fig. 1a). Double labeling with anti-α3 and α6 chains antibodies revealed a partial co-localization (Fig. 1b), thus to better characterize the differential distribution of α3 and α6 chain, we performed double labeling reactions with an antibody against the laminin γ1 chain, a marker of the basement membrane of myofibers and blood vessels, and with an antibody against collagen III, a component of the fibrillar matrix. The α6 chain appeared mainly interstitial, in fact it was absent from the basement membranes of both muscle and vessels, while it co-localized with collagen III (Fig. 1b). In contrast, the α3 chain was detected at the basement membrane of myofibers and blood vessels, as it co-localized with the laminin γ1 chain (Fig. 1b).
Fig. 1.
Immunofluorescence analysis of collagen VI α6 and α3 chains in transversal muscle sections of tibialis anterior from a normal subject.
a: The α6 chain is expressed both in the perimysium and endomysium, with a discontinuous pattern around the muscle fibers. α3 chain immunolabeling is diffuse and homogeneous both in the perimysium and endomysium. Bar, 100 μm. Nuclei were counterstained with DAPI (blue).
b: α6 chain labeling appears discontinuous in the endomysium (arrows), and a partial co-localization with anti-α3 chain was shown with double labeling. The α3 chain antibody strongly stains basement membranes, as demonstrated by double-labeling for the laminin γ1 chain (yellow fluorescence in merge image); the α6 chain appears expressed in the interstitium between adjacent fibers and absent in basement membrane of both capillary vessels and myofibers. In agreement with an interstitial localization, the α6 chain co-localizes with collagen type III. Bar, 20 μm. Nuclei were counterstained with DAPI (blue).
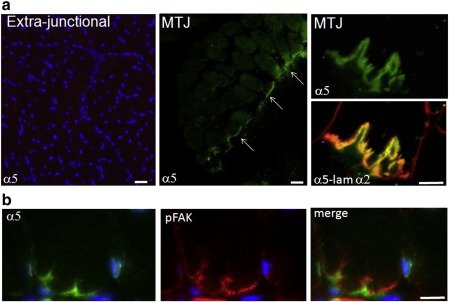
2.2. The collagen VI α5 chain is selectively localized at the basement membrane of myotendinous junctions
By immunofluorescence analysis, the α5 chain was not detected in the endoysium and perimysium of tibialis anterior (Fig. 2), however, when we analyzed a sample derived from the soleus muscle taken at the insertion to the Achille's tendon, we found a selective expression of the α5 chain at the myotendinous junctions (MTJ) where it co-localized with the laminin α2 chain, a marker for the basement membrane of muscle fibers. The labeling pattern obtained with pFAK antibodies, which are selectively expressed at the MTJ, mirrored on the cytoplasmic side the α5 chain signal on the extracellular side at the MTJ level (Fig. 2). The α5 chain was absent in the extra-junctional myofiber basement membrane and within the tendon (Fig. 2). The α6 chain was also detected at the myotendinous junctions, though not as a specific localization but as a continuous labeling of the endomysium. Similarly to the α5 chain, it was absent within the tendon (data not shown).
Fig. 2.
Immunofluorescence analysis of collagen VI α6 in human muscle.
a: Collagen VI α5 chain localization in transversal sections of tibialis anterior (extra-junctional, left panel) and of soleus at the insertion to the Achille's tendon (MTJ, middle and right panels). The α5 chain (green) is absent in the interstitium of tibialis anterior, while it is selectively expressed at the myotendinous junction of soleus (arrows) where it co-localizes with the laminin α2 chain (red), a marker for basement membranes. Bar, 100 μm in left and middle panels, and 20 μm in right upper and lower panels. Nuclei were counterstained with DAPI (blue).
b: Double labeling with anti-α5 chain (green) and anti-pFAK (red) antibodies, of a section of soleus at the insertion to the Achille's tendon, reveals that the α5 chain is expressed at the extracellular side of myotendinous junctions, where pFAK labeling is concentrated. The merged image shows a clear correspondence of the two labeling patterns. Bar, 20 μm. Nuclei were counterstained with DAPI (blue).
2.3. COL6A1 homozygous null mutations affect the deposition of the collagen VI α6 chain in the extracellular matrix of skeletal muscle of an UCMD patient
To assess if COL6A1 mutations affect the deposition of the novel α6 chain in the extracellular matrix of human muscle, in accordance with the reported Col6a1−/− mouse model (Gara et al., 2008), we studied the muscle biopsy of an UCMD patient carrying a homozygous deletion in exon 22 that causes a frameshift, resulting in a premature stop codon at residues 504–505 in the triple helical domain. At the protein level, this mutation causes a complete absence of the α1 chain both in patient's cells and medium of cultured skin fibroblasts (P3 in Giusti et al., 2005) and in muscle biopsy (Demir et al., 2004), similar to the Col6a1−/− mice phenotype (Bonaldo et al., 1998).
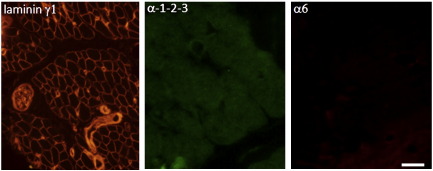
By immunofluorescence analysis we found that both the α3 and the α6 chains were absent in the extracellular matrix (Supplementary Fig. 1); we could not determine the effect of the COL6A1 mutation on the α5 chain deposition since myotendinous junctions were not present in the patient's biopsy, as detected by laminin γ1 chain (Supplementary Fig. 1).
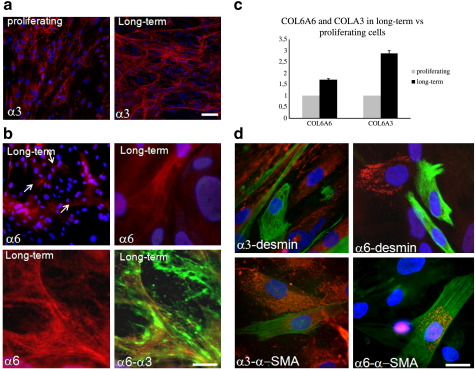
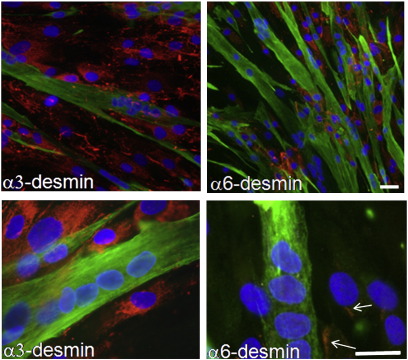
2.4. Collagen VI α5 and α6 chain expression in normal muscle cell cultures
We compared the expression and organization of the α5 and α6 chains with that of their homologue, the α3 chain, in a primary normal muscle cell culture under different culture conditions, i.e. grown for 48 h (proliferating) or 7 days (long term), with and without 0.25 mM L-ascorbic acid, and after induction of myogenic differentiation. The α3 chain was detected in the extracellular matrix of both proliferating and long-term samples, however the microfibrillar network appeared better organized and developed in long-term cultures (Fig. 3a). The α6 and α5 chains were not detectable in proliferating primary muscle cell cultures (not shown). In long-term cultures, slight filamentous, α6-containing deposits were detected in the extracellular matrix (Fig. 3b), while the α5 chain was completely absent (not shown). The α6 antibody co-localized with α3-positive filamentous structures, however, an α3-based independent network could be also detected (Fig. 3b). COL6A5 transcripts were undetectable both in proliferating and in long-term cells. Both COL6A3 and COL6A6 transcript levels were increased in long-term cultures compared to proliferating cells (1.7:1 COL6A6 and 2.9:1 COL6A3) (Fig. 3c). Primary cultures derived from muscle biopsies may contain both interstitial and myogenic cells. To assess which cells produce the α6 chain, long-term muscle cultures were analyzed in the absence of ascorbic acid, to induce intracellular accumulation of under-hydroxylated collagen VI chains (Engvall et al., 1986). In agreement with a previous study which established that interstitial cells, and not myogenic cells, produce collagen VI (Zou et al., 2008), we found that the α3 chain was absent in myogenic (desmin-positive) cells, while it was accumulated in most of desmin-negative cells. The α6 chain was detected intracellularly only in a subset of desmin-negative cells, and, similarly to the α3 chain, it was absent in myogenic cells. Interestingly, most of the α6 chain-producing cells showed a flattened shape and were positive for α-smooth muscle actin (α-SMA), indicating that they could be myofibroblasts, probably of interstitial origin (Fig. 3d).
Fig. 3.
Immunofluorescence analysis of collagen VI α3 and α 6 chains in normal muscle cultures.
a: The collagen VI α3 chain (red fluorescence) is detected in the extracellular matrix of both proliferating and long-term (after ascorbic acid treatment for 7 days post-confluence) samples, however the arrangement of the collagen VI network appears better organized in long term cultures. Bar, 100 μm. Nuclei were counterstained with DAPI (blue).
b: Collagen VI α6 chain (red fluorescence) deposits are detectable in the extracellular matrix of muscle cultures after ascorbic acid treatment for 7 days post-confluence. α6-containing structures (arrows, left upper panel) show a filamentous arrangement, as detected at higher magnification (right upper panel). Lower panels show double labeling with antibodies against the anti-α6 (red fluorescence) and α3 (green fluorescence) chains. Filamentous α6 chain-containing structures (red) co-localize with α3 chain-containing positive microfilaments, as revealed by the merged image (lower, right panel), however, an independent α3 chain-containing network (green fluorescence) can be also detected. Bar, 20 μm. Nuclei were counterstained with DAPI (blue).
c: Real Time-PCR analysis of COL6A3 and COL6A6 transcripts. Reported values are the mean of two different experiments utilizing ACTB and GAPDH as reference transcripts. The relative ratios ofCOL6A3/Actin-GAPDH and COL6A6/Actin-GAPDH mRNAs in proliferating cells were normalized to 1. Both COL6A3 and COL6A6 transcript levels were increased in long-term cells (1.7:1 for COL6A6 and 2.9:1 for COL6A3).
d: Immunofluorescence analysis of collagen VI α3 and α6 chains in long-term normal muscle cell cultures in the absence of ascorbic acid treatment. Samples were double-labeled for desmin (upper panels, green fluorescence) and for α-smooth muscle actin (α-SMA; lower panels, green fluorescence). The collagen VI α3 chain (red fluorescence, left, upper panel) appears to be absent in desmin-positive cells and accumulates in desmin-negative cells, indicating that the fibroblasts are the main source of α3 chain. Similarly, the α6 chain (red, right, upper panel) is absent in desmin-positive, but different from the α3 chain, it is detected intracellularly only in a subset of desmin-negative cells. Cell producing collagen VI α6 chain (red) are positive for α-smooth muscle actin (green, right, lower panel), indicating that they could be myofibroblasts. Bar, 20 μm. Nuclei were counterstained with DAPI (blue).
Under differentiating conditions, the α3 chain was present both in the extracellular matrix surrounding myotubes and inside the cytoplasm of desmin-negative cells. The presence of this protein inside the cytoplasm can be ascribed to the absence of ascorbic acid in differentiating medium (Lattanzi et al., 2000). The α3 chain was not detected inside the cytoplasm of myotubes, confirming that myogenic cells do not produce collagen VI (Zou et al., 2008). The α6 chain was faintly detected in the extracellular matrix as a poorly developed network. Some desmin-negative cells showed cytoplasmic labeling while the protein was absent within myotubes (Supplementary Fig. 2). The alpha5 chain was not detectable both in myotubes and desmin-negative cells, similarly to proliferating and long-term cultures (not shown). These data strongly indicate that regulation of both α5 and α6 chains is not affected by myogenic differentiation.
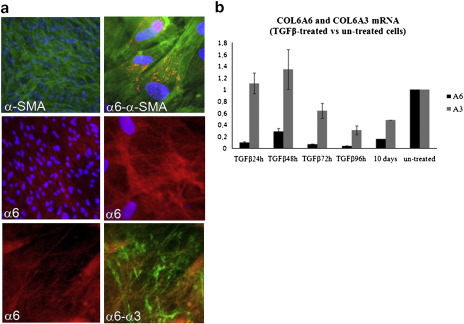
2.5. Trans-differentiation of muscle fibroblasts into myofibroblasts induced by TGFβ1 strongly increases collagen VI α6 chain deposition in the extracellular matrix of normal muscle cultures
TGFβ1 is a strong inducer of muscle fibroblasts activation, when applied to primary muscle cell cultures, and of fibroblast differentiation into myofibroblasts, which acquire an α-SMA-positive phenotype. On the contrary, TGFβ1 inhibits myogenic differentiation. To assess the effect of TGFβ1 on the expression of the novel collagen VI chains, normal primary muscle cells were treated for 10 days. As expected, we detected a strong increase in the number of α-SMA positive cells (Fig. 4a). In contrast, desmin expression was reduced, as well as the number of spontaneously differentiated myotubes (not shown). In these conditions, the amount of α6 chain was increased and the secreted protein deposited in a wide filamentous network in the extracellular matrix (Fig. 4a). The α6 chain mainly co-localized with the α3 chain, however, a distinct α3 chain containing network could also be detected (Fig. 4a). Both COL6A3 and COL6A6 transcript levels were markedly reduced in cells after long-term (10 days) TGFβ1 treatment (0.48:1 COL6A3 and 0.16:1 COL6A6). By analyzing mRNA levels at different time points, we detected constantly low transcriptional levels of COL6A6 mRNA starting from 24 hour of treatment. Differently, an initial up-regulation of COL6A3 mRNA at 24–48 hours was followed by a gradual decrease at prolonged TGFβ1 treatment (Fig. 4b). TGFβ1 treatment did not affect the expression and synthesis of the α5 chain, both at the RNA and protein levels (not shown).
Fig. 4.
Immunofluorescence and Real Time-PCR analysis of α6 chain in normal muscle cultures after TGFβ1 treatment.
a: After 10 days TGFβ1 treatment most of interstitial cells express α-SMA (left upper panel, green fluorescence) indicating trans-differentiation into a myofibroblasts-like phenotype. In the absence of ascorbic acid (right upper panel) most of α-SMA expressing cells accumulated the collagen VI α6 chain (red) intracellularly. After ascorbic acid treatment (left and right middle panels), the α6 chain (red) was abundantly secreted and arranged in a wide filamentous network in the extracellular matrix. Left and right lower panels show double labeling with antibodies against the α6 and α3 chains on samples treated with TGFβ1 for 10 days in presence of ascorbic acid. The α6 chain (red fluorescence) mainly co-localizes with the α3 chain (green) labeling. However, a distinct α3−containing network can also be detected (green fluorescence). Bar, 20 μm . Nuclei were counterstained with DAPI (blue).
b: Real Time-PCR analysis. Reported values are the mean of two different experiments utilizing ACTB and GAPDH as reference transcripts The relative ratios of COL6A3/Actin-GAPDH and COL6A6/Actin-GAPDH mRNAs in untreated cells were normalized to 1. COL6A3 and COL6A6 transcript levels are strongly reduced in cells after long-term (10 days) TGFβ1 treatment (0.48:1 for COL6A3 and 0.16:1 for COL6A6). Analysis of mRNA levels at different time points revealed constantly low transcriptional levels of COL6A6 mRNA starting from 24 hour of treatment. In contrast, an initial slight up-regulation of COL6A3 mRNA at 24–48 hours, was followed by a gradual decrease after prolonged TGFβ1 treatment.
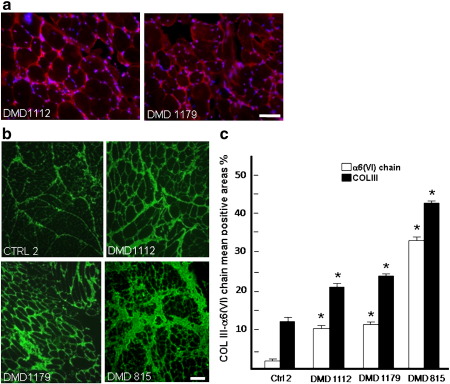
2.6. The collagen VI α6 chain, but not the α5 chain, is up-regulated in dystrophic muscles
As myofibroblasts play a major role upon fibrosis, we studied the expression of the α6 chain in muscle biopsies of five patients affected by Duchenne Muscular Dystrophy (DMD), a muscular dystrophy characterized by a marked fibrosis which is definitely independent from any mutation in collagen VI genes. Because of scarce availability of tissue, only the DMD815 biopsy was studied by means of immunofluorescence, Western blotting and mRNA analysis. The other DMD patients were studied either by immunofluorescence plus mRNA or by immunofluorescence plus Western blotting analysis.
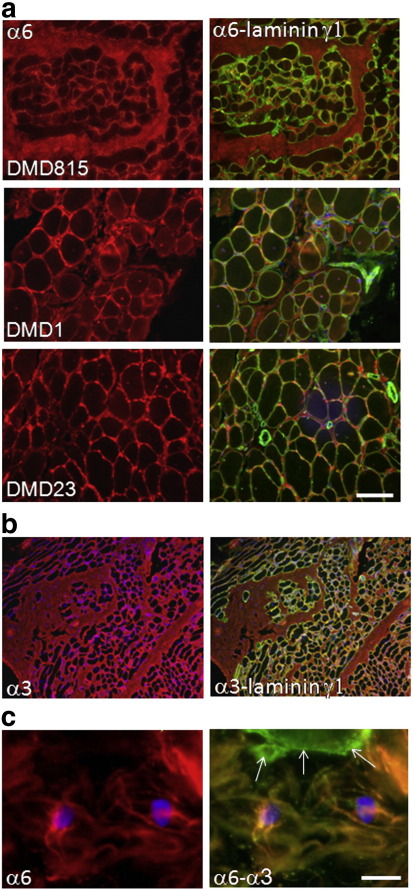
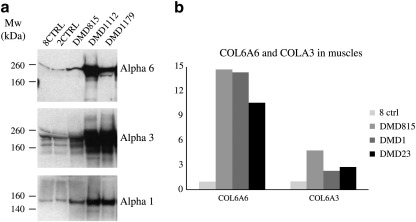
By immunofluorescence analysis, the α6 chain antibody showed an increased amount of protein in the extracellular matrix of all DMD patients (Fig. 5a and Supplementary Fig. 3a). The localization of the α6 chain was interstitial, in fact no labeling was detected at the basement membrane of myofibers and blood vessels, as indicated by double labeling with anti-laminin γ1 antibody (Fig. 5a). By double staining, the α6 chain labeling correlated with collagen III positive areas, used as a marker of fibrosis. Semiquantitative analysis revealed a strong correlation between the increase of α6 chain and collagen III protein amount (supplementary Fig. 3b,c). Also the α3 chain was increased in all DMD patients (Fig. 5b) and matched the degree of fibrosis. Double labeling with antibodies against the α3 and α6 chains showed a partial co-localization, and confirmed the absence of the α6 chain from the basement membranes of vessels and myofibers. At high magnification, undulated/wavy bundles of fibrils of different size containing both the α6 and α3 chains were detected in fibrotic areas (Fig. 5c), suggesting that the α6 and α3 chains may co-assemble and cooperate in remodeling the extracellular matrix upon fibrosis. Western blot analysis confirmed the increase of α3 and α6 chains in the three DMD patients examined (DMD815, DMD1112, DMD1179). The increased protein levels of α3 and α6 chains matched with a general increase of collagen VI as shown by α1 immuno-blotting (Fig. 6a). The protein increase matched a relevant increase of COL6A6 transcript level, with a fold change that ranged from 10 to 14 in the three analyzed DMD muscles (DMD815, DMD1 and DMD23, Fig. 6b). Nevertheless, at the transcriptional level, the increase in COL6A3 mRNA in fibrotic DMD muscles (2–4 fold changes) was significantly lower than the increase in COL6A6 mRNA. In contrast, the α5 chain and the corresponding transcript were not detected (not shown).
Fig. 5.
Immunofluorescence analysis of α6 chain in DMD patients muscle biopsies.
a: Immunofluorescence analysis of the collagen VI α6 chain (red) and the laminin γ1 chain (green) in muscle sections of three patients affected by Duchenne muscular dystrophy (DMD815, DMD1, DMD23). α6 chain labeling appears increased in the endomysium and perimysium, with its increase correlating with the degree of fibrosis. The α6 chain localization is strictly interstitial, as demonstrated by absence of co-localization with the laminin γ1 chain (right panels, green fluorescence),a marker for basal lamina. Bar, 100 μm.
b: Immunofluorescence analysis of the collagen VI α3 chain in DMD815 muscle sections revealed a marked increase in fibrotic ares (red fluorescence, left panel). Double labeling with antibodies against –the laminin γ1 chain (green) reveals the presence of α3 chain at the basal lamina of muscle fibers (yellow fluorescence in merge image, right panel).
c: High magnification of a muscle section from patient DMD815 double labeled with antibodies against collagen VI α6 (red fluorescence) and -α3 (green fluorescence) chains showing the presence of undulated/wavy bundles of fibrils of different size containing both the α6 and α3 chains. In the basement membrane of a muscle fiber, only the α3 chain is found (arrows). Bar, 20 μm. Nuclei were counterstained with DAPI (blue).
Fig. 6.
Western blot and RT-PCR analysis of collagen VI chains in muscle biopsies of DMD patients.
a: Western blot analysis of skeletal muscles extracts from a healthy control (CTRL1,2) and from DMD815, DMD1112 and DMD1179 patients. Proteins were separated by SDS-PAGE under reducing conditions and detected with polyclonal antibodies specific for the collagen VI α6 and α3 and α1 chains; actin was used as loading control.
b: Real Time-PCR analysis of COL6A6 transcripts in DMD skeletal muscle biopsies. Reported values are the mean of two different experiments utilizing ACTB and GAPDH as reference transcripts. The relative ratios of COL6A3/Actin-GAPDH and COL6A6/Actin-GAPDH mRNAs in control muscle were normalized to 1. The increased amount of collagen VI α3 and α6 chains in DMD muscles matched with an increase of the corresponding mRNAs. The COL6A6 transcript level showed a fold change that ranged from 10 to 14 in the three analyzed samples whereas the variation in the COL6A3 mRNA level was lower (2–4 fold change).
3. Discussion
The discovery of two additional collagen VI chains in humans (α5 and α6), which may substitute for the α3 chain, suggests the existence of additional assembly forms of collagen VI (Fitzgerald et al., 2008; Gara et al., 2008, 2011). So far, the localization and the expression pattern of the novel chains in human skeletal muscle, the tissue most affected by collagen VI deficiency, was mostly unknown, with the exception of their reported presence in commercially available samples such as fetal human skeletal muscle extract and non-specified skeletal muscle tissue derived from a normal adult human tissue panel (Fitzgerald et al., 2008).
Our study aims to define more precisely the expression and distribution of collagen VI α5 and α6 chains in mature human skeletal muscle. In fact we show that in human skeletal muscle, the α5 and α6 chains differ from the homologous α3 chain in a number of aspects, e.g. localization pattern, cellular origin and involvement in ECM remodelling upon muscle fibrosis. To distinguish between the different assembly forms (Gara et al., 2008), we used antibodies specific for the individual α3, α5 and α6 chains (Sabatelli et al., 2011).
In normal skeletal muscle sections, the α5 chain was selectively detected at the basement membrane of myotendinous junctions. Our previous studies showed that the α5 chain localizes at junctional sites also in human skin, in particular at the dermal-epidermal junction (Sabatelli et al., 2011). These data indicate that α5 chain-containing collagen VI microfibrils may have a specific function in specialized tissue areas subjected to tensile stress. Myotendinous junctions are crucial elements in the transmission of mechanical force from the muscle via tendons to the skeletal elements. Several molecules have been identified at this site and mutations in their genes lead to pathologic changes of myotendinous junctions: α7β1 integrin, laminin 2, and the dystrophin glycoprotein complex are pivotal at this site (Mayer et al., 1997; Pegoraro et al., 2002; Vainzof and Zatz, 2003). Tenascin, an oligomeric extracellular matrix protein, was one of the first myotendinous junction markers (Chiquet and Fambrough, 1984). Notably, mutations in tenascin XB gene cause Ehlers–Danlos syndrome (Zweers et al., 2003), with muscle weakness and contractures and secondary deficiency of collagen VI, overlapping with the collagen VI myopathies phenotype (Voermans et al., 2007), and pointing to a possible functional interaction between these myotendinous junction components. Therefore α5 gene mutation screening might result appealing in those cases of Ehlers–Danlos disease which are negative for known mutations.
The α6 chain was less abundant than the homologous α3 chain. Its localization was mainly interstitial where it partially co-localized with the α3 chain. The most relevant difference between the α6 and α3 chain localization was the absence of the α6 chain in the basement membrane of both muscle fibers and vessels, where in contrast the α3 chain was specifically detected. Considering that also the α5 chain is absent at the extrajunctional basement membrane, it is possible that the α3-containing microfibrils represent the specific basement membrane collagen VI form. This hypothesis is supported by recent immunoelectron microscopy studies performed with antibodies specific for the collagen VI α1 α2 α3(VI) heterotrimer, which confirmed basement membrane localization of this collagen VI form in skeletal muscle fibers (Gara et al., 2011) and endothelial cells (Groulx et al., 2011). It is interesting to note that absence/reduction of collagen VI at the basement membrane of muscle are features of UCMD/BM muscle biopsies obtained from patients carrying mutations in COL6A1, COL6A2 and COL6A3 genes (Ishikawa et al., 2004; Kawahara et al., 2007; Merlini et al., 2008; Gualandi et al., 2009). Basement membrane abnormalities have also been detected in muscle fibers of Ullrich congenital muscular dystrophy patients (Niiyama et al., 2002; Squarzoni et al., 2006) and in blood vessels of Myosclerosis myopathy patients (Merlini et al., 2008). These data point to a pivotal role of α1 α2 α3 collagen VI form in maintaining basement membrane functional integrity.
As it has been shown for cartilage and skin, the expression of the novel chains in muscle also differs between man and mouse (Fitzgerald et al., 2008; Gara et al., 2011; Sabatelli et al., 2011). Whereas the α5 chain in man is selectively expressed at the myotendinous junction, in mouse the α5 chain is strongly expressed in perimysium and sparsely in epimysium and, in addition, in perineurium of intramuscular peripheral nerves and at the basement membrane of neuromuscular junctions (Gara et al., 2011). The differences in tissue distribution between man and mouse could be the result of α4 chain gene loss in humans, which leads to a functional re-orientation of the remaining chains. In contrast to this, the expression of the α6 chain is similar in human and mouse skeletal muscle. In agreement with reported studies on the Col6a1 null mice model, the α6 collagen VI chain was not expressed in the skeletal muscle of a UCMD patient carrying an α1 null mutation. This result indicates that in humans, similarly to mice, the α6 chain co-assemble with the α1 chain (Gara et al., 2008).
To define the organization of novel collagen VI chains in the extracellular matrix we analyzed normal skeletal muscle cultures. Filamentous α6 chain deposits were detectable in the extracellular matrix only in long term cultures where α6 chain-containing networks were less abundant and organized than those containing the α3 chain. A co-localization was observed, indicating that secreted α3 and α6 chains may co-assemble and form a common network, while the presence of a distinct α3-based network confirmed the immunohistochemical pattern observed in tissue sections.
The α5 chain was absent both at the protein and the mRNA level in proliferating and long term cultures. This is possibly due to the origin of the culture, in fact the muscle fragment we used to establish primary cultures did not include myotendinous junctions. On the other hand, the absence of the α5 chain demonstrates that it is dispensable for cell-substrate adhesion under normal conditions and might underscore a specificity of this chain for junctional structures.
We determined which cells synthesize α6 chain in a primary muscle culture, as this contains both myogenic (desmin-positive) and interstitial (desmin-negative) cells. Collagen VI-producing cells could be identified by omitting ascorbic acid treatment (Prockop et al., 1976; Engvall et al., 1986), as they in this conditions display an intracellular staining with antibodies against collagen VI. The α3 chain was accumulated in desmin-negative cells only, confirming that it is produced by interstitial but not by myogenic cells (Zou et al., 2008). The α6 chain was also absent in desmin-positive cells, but, in contrast to the α3 chain, the α6 chain was detected intracellularly only in a subset of desmin-negative cells which resulted to be α-SMA positive, likely myofibroblasts of interstitial origin.
As TGFβ1 treatment induces transdifferentiation of interstitial muscle fibroblasts to a myofibroblast phenotype (Zanotti et al., 2010), we evaluated its effect on α5 and α6 chain expression and deposition in extracellular matrix. A striking increase in the number of α-SMA-positive cells was observed after 10 days treatment, indicating that the treatment induced transdifferentiation. In addition, TGFβ1 treatment induced a marked increase of the α6 chain-containing filamentous network in the ECM, which only partially overlapped with labeling for α3 chains. In contrast, α5 chain expression remained undetectable, even after TGFβ1 treatment. As expected, and in contrast with the α6 chain increase, desmin expression was reduced, as well as the number of spontaneously differentiated myotubes.
Time course Real Time-PCR experiments showed down-regulation of COL6A6 mRNA levels, starting from 24 h of TGFβ1 treatment, indicating that in the cell culture model, despite a very early induction occurred, the increased protein amounts cannot be ascribed to a direct effect of TGFβ1 on COL6A6 transcription.
Previous studies reported that in vitro treatment with TGF-β1 induces the expression of several collagen VI interacting proteins, as collagens I and IV (Evans et al., 2003), biglycan (Todorova et al., 2011), as well as fibronectin and integrins (Reinboth et al., 2006; Honda et al., 2010). It is possible that TGF-β1 treatment improves the efficiency of the extracellular binding/assembly of the α6 chain by induction of collagen VI related-proteins, resulting in an increased deposition in the extracellular matrix.
Our results indicate that myofibroblasts are the main α6 chain producing cells and that TGF-β1 treatment enhances α6 chain secretion, pointing to a possible involvement of the α6 chain in fibrosis (Wipff and Hinz, 2008). Fibrosis is a conspicuous pathological change in dystrophic muscles. It is characterized by excessive accumulation of collagens and other ECM components including collagen VI. For this reason we evaluated the expression of α5 and α6 chains in muscle biopsies of three DMD patients with different degrees of fibrosis. We found that collagen VI was generally increased in fibrotic muscle and, in particular, the α6 chain was strongly up-regulated in DMD muscle at protein level, as shown by Western blot, real time PCR and immuno-histochemical analysis. The increase of the α6 chain was particularly evident in fibrotic areas and maintained an interstitial localization at the endomysium, since no colocalization with basement membrane markers was detected.
On the basis of their high homology with the α3 chain, the collagen VI α5 and α6 chains are likely to interact with α1 and α2 chains, in agreement with previous studies on Col6a1 knockout mice (Gara et al., 2008, 2011) and on human skin (Sabatelli et al., 2011). This may give rise to homologous heterotrimers, which appear to function differently, most probably with regard to tissue adhesion. Specifically, in human skeletal muscle we hypothesize that the α3-containing collagen VI is involved in basement membranes adhesion to the interstitial extracellular matrix; the α5-containing collagen VI is involved in junctional adhesion at myotendinous junctions and dermal-epidermal junctions, and the α6-containing collagen VI has a role in adhesion to endomysium and in the development of fibrosis, in association with fibrillar collagen. Future studies will concern the role of the novel collagen VI chains in human disease. Moreover, since our data suggest specific roles in specialized ECM structures for α5 and α6 chains, being the α5 related to tensile stress and the α6 implicated in ECM fibrotic remodelling, they might respectively represent new biomarkers for monitoring these stressing events.
4. Experimental procedures
4.1. Preparation of antibodies against the new collagen VI chains
The purified recombinant collagen VI fragments were used to immunize rabbits and guinea pigs. The antisera obtained were purified by affinity chromatography on a column with antigen coupled to CNBr-activated Sepharose (GE Healthcare). The specific antibodies were eluted with 0.1 M glycine, pH 2.5, and the eluate was neutralized with 1 M Tris–HCl, pH 8.8 (Sabatelli et al., 2011).
4.2. Patients
All subjects studied granted informed consent. Skeletal muscle biopsies of one soleus at the insertion with Achille's tendon and two tibialis anterior from healthy subjects, tibialis anterior from five DMD patients and gastrocnemius from one UCMD patient were frozen in isopentane pre-chilled in liquid nitrogen and stored in liquid nitrogen. All patients (Table 1) were previously diagnosed by genetic and immunohistochemical analysis.
Table 1.
Table of muscle biopsies.
| Patient | Age of biopsy (years_months) | Sex | Disease status | Muscle type | Mutation |
|---|---|---|---|---|---|
| DMD1 | 4.7 | Male | Slow in running | Tibialis | del 51 |
| DMD815 | 10.2 | Male | Unable to climb stairs | Tibialis | splicing in 25c_3641-1G>A |
| DMD23 | 9.1 | Male | Difficulty with stairs | Tibialis | del45-52 |
| DMD1112 | 0.9 | Male | Delayed motor milestones | Tibialis | c_5551C>T |
| DMD1179 | 11 | Male | Unable to climb stairs | Tibialis | del 1M-2 |
| UCMD | 1.5 | Male | Sitter, diffuse muscle wasting and weakness | Gastrocnemius | COL6A1 IG del 1456nt (Giusti et al., 2005) |
| CTRL2 | 10 | Male | Healthy donor | Tibialis | |
| CTRL1120 | 9 | Female | Healthy donor | Tibialis | |
| CTRL8 | 35 | Male | Healthy donor | Tibialis |
4.3. Immunofluorescence analysis
Frozen sections (7 μm-thick) from muscles of healthy donors and of five DMD (DMD1, DMD815, DMD23, DMD1112 and DMD1179) and one UCMD patients (see Table 1) were incubated with the affinity purified rabbit polyclonal antibody against the collagen VI α5 chain (diluted in PBS 1/40). For the immunofluorescence analysis of the collagen α6 chain, frozen sections from healthy donors and patients were fixed with 2% paraformaldehyde in phosphate buffered saline (PBS), washed in PBS and permeabilized with 0.15% Triton X100, saturated with 5% normal goat serum (Sigma) and incubated with the rabbit or guinea pig antibody against the α6 chain diluted 1/40. All sections were developed with anti-rabbit or anti-guinea pig TRITC or FITC-conjugated IgG (DAKO) and double labeled with mouse monoclonal antibodies against the laminin γ1, laminin α2 chain, collagen type III (Chemicon), or with anti-pp125 FAK antibody (Santa Cruz) and revealed with anti-mouse or anti-rabbit FITC or TRITC-conjugated secondary antibodies (DAKO). An antibody against the collagen VI α1α2α3 chains (Fitzgerald) was used on sections of the UCMD patient to assess the expression of collagen VI. Samples were mounted with an anti-fading reagent (Molecular Probes) and observed with a Nikon epifluorescence microscope. Nuclei were counterstained with DAPI.
The proliferation of connective tissue in DMD muscle biopsies was evaluated by immunofluorescence analysis of collagen type III (Hantaï et al., 1985) and compared with the normal muscle biopsy. Double labeling with anti-α6 chain antibody was performed in order to evaluate whether collagen III-positive areas correlated with the alpha6 chain labeling. Five different fields for each biopsy were taken with a fixed exposure time by the NIS-Elements AR (Nikon) imaging program using the multi-channel acquisition function. All images, which included both signals for the collagen VI α6 chain and for collagen III, were captured using an high-resolution CCD camera (Nikon). Semi-quantitative analysis was performed by a software developed in cooperation with Nikon Italy (NIS-Elements 3.0 AR imaging program, Nikon). The fluorescent areas were evaluated by the area fraction function, and the mean values were calculated. For graphic representation, area fraction mean values were expressed as percentage. Data were analyzed using the Mann–Whitney test and the significance was calculated versus normal muscle.
4.4. Muscle cultures
Primary muscle cells derived from tibialis anterior of a normal subject were established as described (Cenni et al., 2005) and maintained in D-MEM plus 20% fetal calf serum (Rando and Blau, 1994). For immunofluorescence analysis of the collagen VI α5 and α6 chains muscle cells were grown onto coverslips for 48 hrs or 7 days, with and without 0.25 mM l-ascorbic acid. When needed, cells were treated with 10 ng/ml TGF-β1 (Sigma). Differentiation to myotubes was induced by incubating subconfluent cells for 7 days with D − MEM plus 10% fetal calf serum (Lattanzi et al., 2000). Samples were fixed with cold methanol, washed with PBS and incubated with rabbit or guinea pig antibodies against the α5, α6 or α3 chains. Double labeling was performed with mouse monoclonal anti-desmin (Novocastra) or anti-alpha-SMA (SIGMA) antibodies. Nuclei were counterstained with DAPI
4.5. Quantification of COL6A5 and COL6A6 transcripts by real-time PCR
Total RNA was isolated from muscle sections of normal tibialis or tibialis from patients DMD815, DMD1 and DMD23 or from cell cultures by using RNeasy Kit (QIAGEN, Chatsworth, CA) and reverse transcribed by using High Capacity cDNA Reverse Transcription Kit (Applied Biosystems). In order to quantify the steady state level of COL6A5 and COL6A6 transcripts, commercially available TaqMan expression assays (Applied Biosystems) were used for target genes (COL6A3: Hs00915102_m1 Ex 23–24; COL6A5 (COL29A1): Hs00542046_m1 exons 35–36; COL6A6: Hs01029204_m1 exons 12–13) and for β actin and GAPDH as housekeeping reference genes (ACTB Endogenous Control- GAPDH endogenous control). Real-time PCR was performed in triplicate on the Applied Biosystems Prism 7900HT system, using 10 ng of cDNA and default parameters. Evaluation of COL6A3 and COL6A6 transcripts levels was performed by the comparative CT method (ΔΔCT Method; Applied Biosystems User Bullettin #2). cDNAs from control muscle sections or untreated cells were utilized as calibrators.
4.6. Western blot analysis
Frozen sections (20 μm) were prepared from skeletal muscles biopsies of two healthy donors and patients DMD815, DMD1112 and DMD1179. The sections were extracted by incubation for 10 min at 70 °C in a lysis solution containing 50 mM Tris–HCl, pH 7.5, 150 mM NaCl, 10 mM MgCl2, 2% SDS, 1% Triton X-100, 0.5 mM dithiothreitol, 1 mM ethylenediaminetetraacetic acid, 10% glycerol and protease inhibitors. For each sample, the total protein content was determinate using “BCA Protein Assay Kit” (Pierce). Samples were reduced with 5% β-mercaptoethanol and separated by SDS-PAGE on 3-8% (w/v) gradient polyacrylamide gels. Collagen VI α3 and α6 chains were detected using the affinity-purified antibodies developed in rabbit (Sabatelli et al., 2011). Collagen VI α1 chain was detected using a specific collagen VI α1 antibody (H-200, Santa Cruz Biotechnologies). As a loading control, actin was used (Sigma). Secondary antibodies conjugated with horseradish peroxidase were employed (GE Healthcare) and bands detected by chemiluminescence (SuperSignal West Pico, Pierce).
The following are the supplementary materials related to this article.
Supplemental Fig. 1.
Immunofluorescence analysis of the laminin γ1 chain (left panel), collagen VI α1α2α3 chains (middle panel) and the collagen VI α6 chain (right panel) on muscle sections of tibialis anterior of an UCMD patient with a mutation in COL6A1 gene, showing complete absence of collagen VI chains in muscle and in capillary vessels, which in contrast display a normal laminin γ1 labeling. Bar, 20 μm.
Supplemental Fig. 2.
Immunofluorescence analysis of collagen VI α3 (left panels, red) and α6 chains (right panels, red) in normal muscle cultures after 7 days of myogenic differentiation. Double labeling with a desmin antibody (green) shows efficient myogenic differentiation, as indicated by the presence of multinucleated myotubes. The α3 chain (red, left upper and lower panels) is present both in the extracellular matrix surrounding myotubes and inside the cytoplasm of desmin-negative cells. No red labeling can be detected inside differentiated myotubes (left lower panel). The α6 chain is faintly detectable in the extracellular matrix. Some desmin-negative cells showed cytoplasmic labeling (arrows, right lower panel) while the protein was absent within myotubes. Bar, 20 μm. Nuclei were counterstained with DAPI (blue).
Supplemental Fig. 3.
a: Immunofluorescence analysis of muscle sections from DMD1179 and DMD1112 patients with antibody against the collagen VI α6 chain (upper, left panel) shows a marked α6 chain deposition in the endomysium of both dystrophic biopsies. Bar 20 μm. Nuclei were counterstained with DAPI (blue). b: Immunofluorescence analysis of collagen type III in muscle sections from a normal control CTRL2, and the DMD1112, DMD1179 and DMD815 patients. Collagen III, which is indicative of connective tissue proliferation, appears increased in the endomysium and perimysium of all DMD patients with respect to the control CTRL2. Bar 20 μm. c: Graphic representation of semiquantitative analysis of collagen VI α6 chain and collagen III positive areas, showing a strong correlation between the increase of the collagen III and the α6 chain protein amount in DMD patients. *P < 0.05.
Supplementary materials related to this article can be found online at doi:10.1016/j.matbio.2011.12.003.
Acknowledgments
This work has been funded by the BIO-NMD Grant (EC, 7th FP, proposal #241665; “http://www.bio-nmd.eu” to AF as coordinator) and Italian Research Ministry “Prin 2008” grant no. 2008PB5S89 to PB, PS, SS, AF, by Fondazione CaRisBo and by the Deutsche Forschungsgemeinschaft (WA1338/2-6 and SFB 829) to RW and MP. SKG is a member of the International Graduate School in Genetics and Functional Genomics at the University of Cologne. The authors wish to thank Dr Rosa Curci for assistance in human muscle cultures establishment.
Contributor Information
Patrizia Sabatelli, Email: sabatelli@area.bo.cnr.it.
Stefano Squarzoni, Email: squarzoni@area.bo.cnr.it.
References
- Bonaldo P., Braghetta P., Zanetti M., Piccolo S., Volpin D., Bressan G.M. Collagen VI deficiency induces early onset myopathy in the mouse: an animal model for Bethlem myopathy. Hum. Mol. Genet. 1998;7:2135–2140. doi: 10.1093/hmg/7.13.2135. [DOI] [PubMed] [Google Scholar]
- Bruns R.R. Beaded filaments and long-spacing fibrils: relation to type VI collagen. J. Ultrastruct. Res. 1984;89:136–145. doi: 10.1016/s0022-5320(84)80010-6. [DOI] [PubMed] [Google Scholar]
- Camacho Vanegas O., Bertini E., Zhang R.Z., Petrini S., Minosse C., Sabatelli P., Giusti B., Chu M.L., Pepe G. Ullrich scleroatonic muscular dystrophy is caused by recessive mutations in collagen type VI. Proc. Natl. Acad. Sci. U. S. A. 2001;98:7516–7521. doi: 10.1073/pnas.121027598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cenni V., Sabatelli P., Mattioli E., Marmiroli S., Capanni C., Ognibene A., Squarzoni S., Maraldi N.M., Bonne G., Columbaro M., Merlini L., Lattanzi G. Lamin A N-terminal phosphorylation is associated with myoblast activation: impairment in Emery–Dreifuss muscular dystrophy. J. Med. Genet. 2005;42:214–220. doi: 10.1136/jmg.2004.026112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiquet M., Fambrough D.M. Chick myotendinous antigen. I. A monoclonal antibody as a marker for tendon and muscle morphogenesis. J. Cell Biol. 1984;98:1926–1936. doi: 10.1083/jcb.98.6.1926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu M.L., Conway D., Pan T.C., Baldwin C., Mann K., Deutzmann R., Timpl R. Amino acid sequence of the triple-helical domain of human collagen type VI. J. Biol. Chem. 1988;263:18601–18606. [PubMed] [Google Scholar]
- Cutroneo K.R. TGF-beta-induced fibrosis and SMAD signaling: oligo decoys as natural therapeutics for inhibition of tissue fibrosis and scarring. Wound Repair Regen. 2007;15:S54–S60. doi: 10.1111/j.1524-475X.2007.00226.x. [DOI] [PubMed] [Google Scholar]
- Demir E., Ferreiro A., Sabatelli P., Allamand V., Makri S., Echenne B., Maraldi N.M., Merlini L., Topaloglu H., Guicheney P. Collagen VI status and clinical severity in Ullrich congenital muscular dystrophy: phenotype analysis of 11 families linked to the COL6 loci. Neuropediatrics. 2004;35:103–112. doi: 10.1055/s-2004-815832. [DOI] [PubMed] [Google Scholar]
- Engvall E., Hessle H., Klier G. Molecular assembly, secretion, and matrix deposition of type VI collagen. J. Cell Biol. 1986;102:703–710. doi: 10.1083/jcb.102.3.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans R.A., Tian Y.C., Steadman R., Phillips A.O. TGF-beta1-mediated fibroblast-myofibroblast terminal differentiation-the role of Smad proteins. Exp. Cell. Res. 2003;282:90–100. doi: 10.1016/s0014-4827(02)00015-0. [DOI] [PubMed] [Google Scholar]
- Fitzgerald J., Rich C., Zhou F.H., Hansen U. Three novel collagen VI chains, alpha 4 VI, alpha 5 VI and alpha 6 VI. J. Biol. Chem. 2008;283:20170–20180. doi: 10.1074/jbc.M710139200. [DOI] [PubMed] [Google Scholar]
- Freise C., Erben U., Muche M., Farndale R., Zeitz M., Somasundaram R., Ruehl M. The alpha 2 chain of collagen type VI sequesters latent proforms of matrix-metalloproteinases and modulates their activation and activity. Matrix Biol. 2009;28:480–489. doi: 10.1016/j.matbio.2009.08.001. [DOI] [PubMed] [Google Scholar]
- Gara S.K., Grumati P., Urciuolo A., Bonaldo P., Kobbe B., Koch M., Paulsson M., Wagener R. Three novel collagen VI chains with high homology to the {alpha}3 chain. J. Biol. Chem. 2008;283:10658–10670. doi: 10.1074/jbc.M709540200. [DOI] [PubMed] [Google Scholar]
- Gara S.K., Grumati P., Squarzoni S., Sabatelli P., Urciuolo A., Bonaldo P., Paulsson M., Wagener R. Differential and restricted expression of novel collagen VI chains in mouse. Matrix Biol. 2011;30:248–257. doi: 10.1016/j.matbio.2011.03.006. [DOI] [PubMed] [Google Scholar]
- Giusti B., Lucarini L., Pietroni V., Lucioli S., Bandinelli B., Sabatelli P., Squarzoni S., Petrini S., Gartioux C., Talim B., Roelens F., Merlini L., Topaloglu H., Bertini E., Guicheney P., Pepe G. Dominant and recessive COL6A1 mutations in Ullrich scleroatonic muscular dystrophy. Ann. Neurol. 2005;58:400–410. doi: 10.1002/ana.20586. [DOI] [PubMed] [Google Scholar]
- Groulx J.F., Gagné D., Benoit Y.D., Martel D., Basora N., Beaulieu J.F. Collagen VI is a basement membrane component that regulates epithelial cell-fibronectin interactions. Matrix Biol. 2011;30:195–206. doi: 10.1016/j.matbio.2011.03.002. [DOI] [PubMed] [Google Scholar]
- Grumati P., Coletto L., Sandri M., Bonaldo P. Autophagy is defective in collagen VI muscular dystrophies, and its reactivation rescues myofiber degeneration. Nat. Med. 2010;16:1313–1320. doi: 10.1038/nm.2247. [DOI] [PubMed] [Google Scholar]
- Gualandi F., Urciuolo A., Martoni E., Sabatelli P., Squarzoni S., Bovolenta M., Messina S., Mercuri E., Franchella A., Ferlini A., Bonaldo P., Merlini L. Autosomal recessive Bethlem myopathy. Neurology. 2009;73:1883–1891. doi: 10.1212/WNL.0b013e3181c3fd2a. [DOI] [PubMed] [Google Scholar]
- Hantaï D., Labat-Robert J., Grimaud J.A., Fardeau M. Fibronectin, laminin, type I, III and IV collagens in Duchenne's muscular dystrophy, congenital muscular dystrophies and congenital myopathies: an immunocytochemical study. Connect. Tissue Res. 1985;13:273–281. doi: 10.3109/03008208509152408. [DOI] [PubMed] [Google Scholar]
- Honda E., Yoshida K., Munakata H. Transforming growth factor-beta upregulates the expression of integrin and related proteins in MRC-5 human myofibroblasts. Tohoku J. Exp. Med. 2010;220:319–327. doi: 10.1620/tjem.220.319. [DOI] [PubMed] [Google Scholar]
- Irwin W., Bergamin N., Sabatelli P., Reggiani C., Megighian A., Merlini L., Braghetta P., Columbaro M., Volpin D., Bressan G.M., Bernardi P., Bonaldo P. Mitochondrial dysfunction and apoptosis in myopathic mice with collagen VI deficiency. Nat. Genet. 2003;35:367–371. doi: 10.1038/ng1270. [DOI] [PubMed] [Google Scholar]
- Ishikawa H., Sugie K., Murayama K., Awaya A., Suzuki Y., Noguchi S., Hayashi Y.K., Nonaka I., Nishino I. Ullrich disease due to deficiency of collagen VI in the sarcolemma. Neurology. 2004;62:620–623. doi: 10.1212/01.wnl.0000113023.84421.00. [DOI] [PubMed] [Google Scholar]
- Jöbsis G.J., Keizers H., Vreijling J.P., de Visser M., Speer M.C., Wolterman R.A., Baas F., Bolhuis P.A. Type VI collagen mutations in Bethlem myopathy, an autosomal dominant myopathy with contractures. Nat. Genet. 1996;14:113–115. doi: 10.1038/ng0996-113. [DOI] [PubMed] [Google Scholar]
- Kawahara G., Okada M., Morone N., Ibarra C.A., Nonaka I., Noguchi S., Hayashi Y.K., Nishino I. Reduced cell anchorage may cause sarcolemma-specific collagen VI deficiency in Ullrich disease. Neurology. 2007;69:1043–1049. doi: 10.1212/01.wnl.0000271386.89878.22. [DOI] [PubMed] [Google Scholar]
- Knupp C., Squire J.M. A new twist in the collagen story—the type VI segmented supercoil. EMBO J. 2001;20:372–376. doi: 10.1093/emboj/20.3.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lampe A.K., Bushby K.M. Collagen VI related muscle disorders. J. Med. Genet. 2005;42:673–685. doi: 10.1136/jmg.2002.002311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lattanzi G., Muntoni F., Sabatelli P., Squarzoni S., Maraldi N.M., Cenni V., Villanova M., Columbaro M., Merlini L., Marmiroli S. Unusual laminin alpha2 processing in myoblasts from a patient with a novel variant of congenital muscular dystrophy. Biochem. Biophys. Res. Commun. 2000;277:639–642. doi: 10.1006/bbrc.2000.3735. [DOI] [PubMed] [Google Scholar]
- Mayer U., Saher G., Fässler R., Bornemann A., Echtermeyer F., von der Mark H., Miosge N., Pöschl E., von der Mark K. Absence of integrin alpha 7 causes a novel form of muscular dystrophy. Nat. Genet. 1997;17:318–323. doi: 10.1038/ng1197-318. [DOI] [PubMed] [Google Scholar]
- Merlini L., Martoni E., Sabatelli P., Squarzoni S., Bovolenta M., Messina S., Mercuri E., Franchella A., Ferlini A., Bonaldo P. Autosomal recessive myosclerosis myopathy is a collagen VI disorder. Neurology. 2008;71:1245–1253. doi: 10.1212/01.wnl.0000327611.01687.5e. [DOI] [PubMed] [Google Scholar]
- Niiyama T., Higuchi I., Suehara M., Hashiguchi T., Shiraishi T., Nakagawa M., Arimura K., Maruyama I., Osame M. Electron microscopic abnormalities of skeletal muscle in patients with collagen VI deficiency in Ullrich's disease. Acta Neuropathol. 2002;104:67–71. doi: 10.1007/s00401-002-0522-z. [DOI] [PubMed] [Google Scholar]
- Pegoraro E., Cepollaro F., Prandini P., Marin A., Fanin M., Trevisan C.P., El-Messlemani A.H., Tarone G., Engvall E., Hoffman E.P., Angelini C. Integrin alpha 7 beta 1 in muscular dystrophy/myopathy of unknown etiology. Am. J. Pathol. 2002;160:2135–2143. doi: 10.1016/s0002-9440(10)61162-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prockop D.J., Berg R.A., Kivirikko K.I., Uitto J. In: Biochemistry of Collagen. Ramachandran G.N., Reddi A.H., editors. Plenum Press; New York: 1976. pp. 163–273. [Google Scholar]
- Rando T.A., Blau H.M. Primary mouse myoblast purification, characterization, and transplantation for cell-mediated gene therapy. J. Cell Biol. 1994;125:1275–1287. doi: 10.1083/jcb.125.6.1275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinboth B., Thomas J., Hanssen E., Gibson M.A. Beta ig-h3 interacts directly with biglycan and decorin, promotes collagen VI aggregation, and participates in ternary complexing with these macromolecules. J. Biol. Chem. 2006;281:7816–7824. doi: 10.1074/jbc.M511316200. [DOI] [PubMed] [Google Scholar]
- Sabatelli P., Bonaldo P., Lattanzi G., Braghetta P., Bergamin N., Capanni C., Mattioli E., Columbaro M., Ognibene A., Pepe G., Bertini E., Merlini L., Maraldi N.M., Squarzoni S. Collagen VI deficiency affects the organization of fibronectin in the extracellular matrix of cultured fibroblasts. Matrix Biol. 2001;20:475–486. doi: 10.1016/s0945-053x(01)00160-3. [DOI] [PubMed] [Google Scholar]
- Sabatelli P., Gara S.K., Grumati P., Urciuolo A., Gualandi F., Curci R., Squarzoni S., Zamparelli A., Martoni E., Merlini L., Paulsson M., Bonaldo P., Wagener R. Expression of the collagen VI α5 and α6 chains in normal human skin and in skin of patients with collagen VI-related myopathies. J. Invest. Dermatol. 2011;131:99–107. doi: 10.1038/jid.2010.284. [DOI] [PubMed] [Google Scholar]
- Söderhäll C., Marenholz I., Kerscher T., Rüschendorf F., Esparza-Gordillo J., Worm M., Gruber C., Mayr G., Albrecht M., Rohde K., Schulz H., Wahn U., Hubner N., Lee Y.A. Variants in a novel epidermal collagen gene COL29A1 are associated with atopic dermatitis. PLoS Biol. 2007;5:e242. doi: 10.1371/journal.pbio.0050242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Squarzoni S., Sabatelli P., Bergamin N., Guicheney P., Demir E., Merlini L., Lattanzi G., Ognibene A., Capanni C., Mattioli E., Columbaro M., Bonaldo P., Maraldi N.M. Ultrastructural defects of collagen VI filaments in an Ullrich syndrome patient with loss of the alpha3 VI N10-N7 domains. J. Cell. Physiol. 2006;206:160–166. doi: 10.1002/jcp.20443. [DOI] [PubMed] [Google Scholar]
- Telfer W.R., Busta A.S., Bonnemann C.G., Feldman E.L., Dowling J.J. Zebrafish models of collagen VI-related myopathies. Hum. Mol. Genet. 2010;19:2433–2444. doi: 10.1093/hmg/ddq126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Todorova L., Bjermer L., Westergren-Thorsson G., Miller-Larsson A. TGFβ-induced matrix production by bronchial fibroblasts in asthma: Budesonide and formoterol effects. Respir. Med. 2011;105:1296–1307. doi: 10.1016/j.rmed.2011.03.020. [DOI] [PubMed] [Google Scholar]
- Vainzof M., Zatz M. Protein defects in neuromuscular diseases. Braz. J. Med. Biol. Res. 2003;36:543–555. doi: 10.1590/s0100-879x2003000500001. [DOI] [PubMed] [Google Scholar]
- Voermans N.C., Jenniskens G.J., Hamel B.C., Schalkwijk J., Guicheney P., van Engelen B.G. Ehlers–Danlos syndrome due to tenascin-X deficiency: muscle weakness and contractures support overlap with collagen VI myopathies. Am. J. Med. Genet. A. 2007;143A:2215–2219. doi: 10.1002/ajmg.a.31899. [DOI] [PubMed] [Google Scholar]
- von der Mark H., Aumailley M., Wick G., Fleischmajer R., Timpl R. Immunochemistry, genuine size and tissue localization of collagen VI. Eur. J. Biochem. 1984;142:493–502. doi: 10.1111/j.1432-1033.1984.tb08313.x. [DOI] [PubMed] [Google Scholar]
- Wagener R., Gara S.K., Kobbe B., Paulsson M., Zaucke F. The knee osteoarthritis susceptibility locus DVWA on chromosome 3p24.3 is the 5′ part of the split COL6A4 gene. Matrix Biol. 2009;28:307–310. doi: 10.1016/j.matbio.2009.05.003. [DOI] [PubMed] [Google Scholar]
- Wipff P.J., Hinz B. Integrins and the activation of latent transforming growth factor beta1 — an intimate relationship. Eur. J. Cell Biol. 2008;87:601–615. doi: 10.1016/j.ejcb.2008.01.012. [DOI] [PubMed] [Google Scholar]
- Zanotti S., Mora M. Proteoglycans are differentially altered in muscular dystrophies. Sci. World J. 2006;6:446–448. doi: 10.1100/tsw.2006.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanotti S., Saredi S., Ruggieri A., Fabbri M., Blasevich F., Romaggi S., Morandi L., Mora M. Altered extracellular matrix transcript expression and protein modulation in primary Duchenne muscular dystrophy myotubes. Matrix Biol. 2007;26:615–624. doi: 10.1016/j.matbio.2007.06.004. [DOI] [PubMed] [Google Scholar]
- Zanotti S., Gibertini S., Mora M. Altered production of extra-cellular matrix components by muscle-derived Duchenne muscular dystrophy fibroblasts before and after TGF-beta1 treatment. Cell Tissue Res. 2010;339:397–410. doi: 10.1007/s00441-009-0889-4. [DOI] [PubMed] [Google Scholar]
- Zhou L., Porter J.D., Cheng G., Gong B., Hatala D.A., Merriam A.P., Zhou X., Rafael J.A., Kaminski H.J. Temporal and spatial mRNA expression patterns of TGF-beta1, 2, 3 and TbetaRI, II, III in skeletal muscles of mdx mice. Neuromuscul. Disord. 2006;16:32–38. doi: 10.1016/j.nmd.2005.09.009. [DOI] [PubMed] [Google Scholar]
- Zou Y., Zhang R.Z., Sabatelli P., Chu M.L., Bönnemann C.G. Muscle interstitial fibroblasts are the main source of collagen VI synthesis in skeletal muscle: implications for congenital muscular dystrophy types Ullrich and Bethlem. J. Neuropathol. Exp. Neurol. 2008;67:144–154. doi: 10.1097/nen.0b013e3181634ef7. [DOI] [PubMed] [Google Scholar]
- Zweers M.C., Bristow J., Steijlen P.M., Dean W.B., Hamel B.C., Otero M., Kucharekova M., Boezeman J.B., Schalkwijk J. Haploinsufficiency of TNXB is associated with hypermobility type of Ehlers-Danlos syndrome. Am. J. Hum. Genet. 2003;73:214–217. doi: 10.1086/376564. [DOI] [PMC free article] [PubMed] [Google Scholar]