Abstract
Pre-eclampsia is increasingly recognized as more than an isolated disease of pregnancy. Women who have had a pregnancy complicated by pre-eclampsia have a 4-fold increased risk of later cardiovascular disease. Intriguingly, the offspring of affected pregnancies also have an increased risk of higher blood pressure and almost double the risk of stroke in later life. Experimental approaches to identify the key features of pre-eclampsia responsible for this programming of offspring cardiovascular health, or the key biological pathways modified in the offspring, have the potential to highlight novel targets for early primary prevention strategies. As pre-eclampsia occurs in 2–5% of all pregnancies, the findings are relevant to the current healthcare of up to 3 million people in the U.K. and 15 million people in the U.S.A. In the present paper, we review the current literature that concerns potential mechanisms for adverse cardiovascular programming in offspring exposed to pre-eclampsia, considering two major areas of investigation: first, experimental models that mimic features of the in utero environment characteristic of pre-eclampsia, and secondly, how, in humans, offspring cardiovascular phenotype is altered after exposure to pre-eclampsia. We compare and contrast the findings from these two bodies of work to develop insights into the likely key pathways of relevance. The present review and analysis highlights the pivotal role of long-term changes in vascular function and identifies areas of growing interest, specifically, response to hypoxia, immune modification, epigenetics and the anti-angiogenic in utero milieu.
Keywords: blood pressure, cardiovascular disease, in utero, offspring, pre-eclampsia, pregnancy, vascular function
Abbreviations: BP, blood pressure; BMI, body mass index; CYP, cytochrome P450; eNOS, endothelial NO synthase; HUVEC, human umbilical vein endothelial cell; IMT, intima-media thickness; I/R, ischaemia/reperfusion; IUGR, intra-uterine growth restriction; L-NAME, NG-nitro-L-arginine methyl ester; LV, left ventricular; LVH, LV hypertrophy; MMP, matrix metalloproteinase; PlGF, placental growth factor; PKCϵ, protein kinase Cϵ; ROS, reactive oxygen species; RUPP, reduced uterine artery perfusion; SBP, systolic BP; sEng, soluble endoglin; sFlt-1, soluble fms-like tyrosine kinase-1; TGF, transforming growth factor; TIMP, tissue inhibitor of metalloproteinases; VEGF, vascular endothelial growth factor
CLINICAL IMPORTANCE
Traditionally pre-eclampsia was viewed as a self-limiting maternal condition that resolved completely with delivery of the placenta [1,2]. However, it is now recognized that a woman who has a pregnancy complicated by pre-eclampsia [3,4] has a 4-fold increased risk of hypertension, and a 2-fold increased risk of ischaemic heart disease and stroke [3] in the 10–15 years after the pregnancy. Intriguingly, the offspring of that pregnancy will also have increased BP (blood pressure) during childhood and nearly double the risk of stroke in later life [5–16]. As pre-eclampsia affects 2–5% of pregnancies, 1.2–3 million people in the U.K. and 6–15 million in the U.S.A. [1,2] are offspring of pregnancies complicated by pre-eclampsia. Experimental approaches to identify the key biological variation that infer the increased risks in this large cohort therefore have the potential to pivotally alter our understanding of the early development of cardiovascular disease and hypertension in the population. The fact that exposed children and adults can be easily identified based on precise clinical criteria, namely a diagnosis of pre-eclampsia in their mother, also raises the possibility for novel, very early, targeted, primary prevention strategies for cardiovascular risk reduction in a high risk group within the community [17].
EPIDEMIOLOGICAL CLUES TO THE MECHANISM
The epidemiological data used to uncover the relationships between maternal pre-eclampsia and offspring cardiovascular health provide clues to the broad nature of the biological variation that underlies the risk [15]. Meta-analysis of available BP data indicates that children exposed to pre-eclampsia in utero have approximately 2–3 mmHg higher SBP (systolic BP) during childhood and young adult life [18]. This difference, if maintained into adulthood, would be associated with a 12% increased risk from stroke [19,20]. In reality, long-term follow-up studies demonstrate a doubling of risk [6]. The key biological pathways relevant to offspring cardiovascular health are therefore likely to have additional effects, on other features of stroke risk, beyond clinic BP measures alone.
Pre-eclampsia is a condition with a heritability of approximately 55% [21], which is contributed to by both maternal and fetal genes. It is plausible that some of the alterations in risk seen in the offspring of pre-eclamptic pregnancies relate to shared genetic factors between the mother and child. The modification to these pathways also appears to be induced specifically by in utero exposure to pre-eclampsia. Siblings of offspring born to pregnancies complicated by pre-eclampsia, who themselves were born to uncomplicated pregnancies, do not demonstrate the vascular abnormalities seen in the offspring [11]. This observation has clear parallels with the ‘developmental programming’ hypothesis [22], which holds that an insult or deprivation during a critical period of growth and development can lead to long-term alterations in the risk of chronic disease [23]. This hypothesis was developed in response to epidemiological data that associated a low birthweight, a pregnancy-related outcome with multi-factorial determinants, to a variety of cardiovascular and non-cardiovascular outcomes, including mortality from coronary artery disease [24,25], BP [24], the metabolic syndrome [26] and non-insulin-dependent diabetes (Type 2 diabetes) [27].
Offspring of pre-eclamptic pregnancies, particularly those with early-onset pre-eclampsia, can also have a low birthweight due to IUGR (intra-uterine growth restriction) or pre-term birth [23]. Prematurity and IUGR have themselves been associated with alterations in cardiovascular risk factors [28,29]. Furthermore, early- and late-onset pre-eclampsia are increasingly being recognized as different subclasses of disease, which may have different implications for cardiovascular risk in the offspring [30]. This complicated combination of in utero insults means that in many currently available human studies it is challenging to separate the effects of exposure to pre-eclampsia from other in utero insults. However, if a baby is born at term without IUGR, but their mother had pre-eclampsia, they still have an increased risk of stroke [6] and vascular abnormalities [31] that persist after adjustment for birthweight. It therefore seems plausible that there is a unique insult within the in utero environment during pre-eclampsia which is incremental to, or acts in synergy with, any risks inferred by IUGR. This hypothesis is supported further by the observation that pre-term birth largely protects offspring from the adverse associations between birthweight and later cardiovascular disease [24,32]. Pre-eclampsia is one of the leading causes of pre-term birth, and the largest differences in later BP are seen in those offspring of pre-eclamptic pregnancies born pre-term [12]; findings that focus attention on key insults that may operate early in pregnancy.
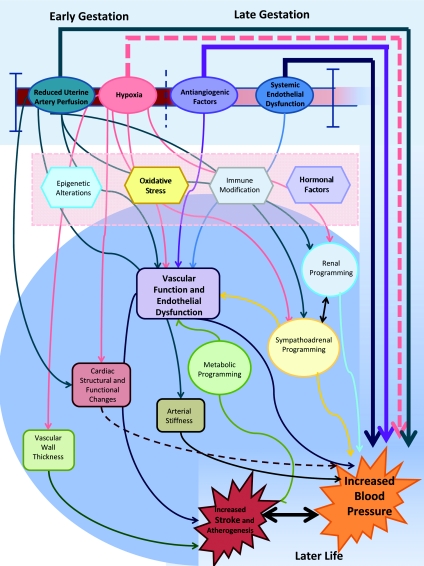
On the basis of these observations, we have now gone on to review the current experimental literature to gain insight into potential mechanisms for in utero cardiovascular programming in relation to pre-eclampsia. We have focused on experiments that use models designed to replicate features of pre-eclampsia, in particular the early detrimental exposures that characterize the fetal experience in this condition. We have compared the findings with those from human studies of offspring, or tissues, from pre-eclamptic pregnancies. The cumulative body of work supports associations between pre-eclampsia exposure and offspring cardiovascular health, as well as a potential pivotal role for long-term programmed changes in vascular biology (Table 1 and Figure 1).
Table 1. Evidence of cardiovascular programming following pre-eclampsia.
An overview of some of the evidence for cardiovascular programming in offspring of animal models and humans born to pre-eclamptic mothers. Positive findings are underlined in roman and negative findings are indicated in italic.
| Human offspring | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Animal model offspring | Perinatal | Later life | |||||||||
| Parameter | RUPP | Hypoxia | sFLT1 | eNOS | Placenta | Cord blood | HUVECs | Neonate | Childhood | Adolescence | Young adult |
| BP | |||||||||||
| ↑BP | [63–65][54–58,60–62,159,160,162,180] | [72,100] | [78,181] | [82,182] | – | – | – | [183] | [114,184][10,15,177,178,185] | [11][7,8,13,14] | [12] |
| Altered BP under stress | – | – | [72] | [82] | – | – | – | – | – | – | – |
| Vascular structural changes | |||||||||||
| ↑IMT/vascular wall thickness | [63,64,86] | [87–89] | – | – | – | – | – | [92] | – | – | [12] |
| ↑Arterial stiffness | [55,63] | [69] | – | [186][113] | – | – | – | – | [15] | – | [12] |
| Vascular functional changes | |||||||||||
| Endothelial dysfunction | [63,141][54,110] | [69–71] | – | [112,113,182,186] | – | [116] | [187] | [31] | [15] | [11] | [12] |
| Non-endothelial function | [110,141] | [71] | [188] | [113,182] | – | – | – | – | – | [11] | [12] |
| Cardiac structural and functional changes | |||||||||||
| Altered cardiac structure | [65][57,86] | [72,95–98] | [181] | – | – | – | – | – | [105] | – | – |
| LV dysfunction | – | [95] | – | – | – | – | – | [189] | [105] | – | – |
| ↑IR injury | – | [94,99–101,190] | – | – | – | – | – | – | – | – | – |
| Renal structural and functional changes | |||||||||||
| Altered structure and function | [59,62,65][57,58,61,64,65,86,159–161] | – | [191] | – | – | – | – | – | – | – | – |
| Metabolic changes | |||||||||||
| ↑BMI | [54,56–59,62,65,86, 110,180,192,193][194,195] | [71,72,88,94,95, 100,131,196] | [77,181,188] | [82,113] | – | – | – | [92] | [178,184][7,8,10,15] | [11,14][16] | [12][13] |
| ↑Serum lipids | [56,63,195] | [196] | [181] | – | – | [92,126–130] | – | – | [15] | [14] | [12] |
| [131] | [114] | ||||||||||
| Altered glucose metabolism | [63][56,194,195,197] | [196] | [181] | – | – | – | – | – | – | [14] | [12] |
| Altered sympatho-adrenal function | |||||||||||
| Adrenal hormones | [62,161,195] | [72,155,157] | – | – | – | [198,199] | – | – | – | [154] | – |
| [14] | |||||||||||
| Sympathetic changes | [200] | [72,158] | – | – | – | – | – | – | – | – | – |
| Genetic/epigenetic changes | |||||||||||
| Gene expression | [57,61,65,160,161][62,63,159] | [96,97,100,131,190,196] | – | [191] | [67,103,164,201–206] | – | – | – | – | – | – |
| Epigenetics | – | [101] | – | – | [135–137] | – | – | – | – | – | – |
| Other | |||||||||||
| ↓Antioxidants | – | – | – | – | [207] | [127,147] | – | – | – | – | – |
| ↑Oxidative stress | [56] | – | – | – | [148] | [127,147,148] | – | – | – | – | – |
| ↑Anti-angiogenic factors | – | – | – | – | – | [120,121] | – | – | [114] | – | – |
| ↑PlGF/VEGF | – | – | – | – | – | [120] | – | – | [114] | – | – |
| Altered inflammation | [63] | [131] | [181] | – | – | – | [173–176] | [208] | [15,114] | – | – |
Figure 1. Potential mechanism of cardiovascular programming in the offspring following a pre-eclamptic pregnancy.
Summary of the potential and demonstrated mechanisms by which in utero exposure to pre-eclampsia may lead to altered cardiovascular physiology and risk in the offspring in later life.
THE IN UTERO INSULT
Disturbed placentation in early pregnancy is considered the key pathological event that leads to subsequent development of pre-eclampsia [2,33]. Normal placental development is characterized by invasion of maternal spiral arteries by fetal cytotrophoblasts and their transformation into high-calibre capacitance vessels, which provides low-resistance placental perfusion to sustain fetal growth [34]. In pre-eclampsia, the spiral arteries inadequately remodel so that uterine flow is reduced by 50% and there is chronic placental ischaemia or, at best, intermittent flow that induces an ischaemia/reperfusion phenomenon [35]. ROS (reactive oxygen species) and cytokines released from the ischaemic placenta trigger a systemic oxidative [36] and inflammatory [35,37] state. The placenta also overexpresses anti-angiogenic factors that inhibit the normal function of pregnancy-related pro-angiogenic factors, including VEGF (vascular endothelial growth factor) and PlGF (placental growth factor) [38]. The combination of these factors is believed to underlie the systemic endothelial dysfunction that is consistently found during symptomatic pre-eclampsia in the mother.
Offspring of pre-eclamptic pregnancies therefore develop from the first trimester onwards within an environment of placental insufficiency and restricted oxygen supply. By the start of the second trimester there is, in addition, exposure to elevated circulating anti-angiogenic factors, which predates the later emergence of the clinical pre-eclamptic syndrome and the diffuse maternal inflammatory, oxidative and dysfunctional endothelial state. Experimental studies have an important role to help us understand how, and whether, these specific insults have an impact on the developing cardiovascular system of the offspring. Their findings have the potential to unravel the developmental programming that underlies the observed long-term cardiovascular disease risk in the offspring.
However, the ideal animal model of pre-eclampsia does not exist, in part because the spontaneous development of pre-eclampsia during pregnancy is a condition largely unique to humans [39,40]. To mimic the human syndrome a model would need to be characterized by the development of pregnancy-specific hypertension, proteinuria and associated alterations in vascular function and biomarkers. To replicate the condition perfectly, these changes must be secondary to impaired trophoblastic invasion [40]. Although a variety of models based on different aspects of the pathophysiology of pre-eclampsia exist [39,40], no model has been able to successfully mimic all of the pathophysiological features of pre-eclampsia or to accurately replicate the first trimester origin of the human condition. For example, the currently available animal models are limited in their capacity to produce the metabolic alterations which are evident in human pre-eclamptic pregnancies [41,42]. Another limitation is that the models have been primarily developed to investigate pre-eclampsia in the mother not the offspring. However, fortuitously, the adequacy of animal models developed to study pre-eclampsia has, in part, been defined by their ability to induce IUGR. As a result, these ‘pre-eclampsia’ models have been adopted to study how IUGR has an impact on the offspring [43]. The findings from these offspring studies, in particular those that maintain experimental set ups that would be expected to induce pre-eclampsia-like syndromes in the dams, thereby provide insights into the role of pre-eclampsia-related insults. We have used data available from animal models to dissect out whether there is evidence that key features of the pre-eclamptic in utero environment induce long-term changes characteristic of the cardiovascular risk phenotype seen in offspring of pre-eclamptic pregnancies, namely elevated resting BP.
Uterine perfusion
Mechanical reduction in maternal uterine artery blood flow [RUPP (reduced uterine artery perfusion)], by unilateral or bilateral uterine artery ligation, in animal models induces a pregnancy-specific increase in maternal BP [44]. The model is well established and has been applied in a range of species from initial work in dogs to rats [40], rabbits [45], sheep [46], guinea-pigs [47] and non-human primates [48]. In dogs, other cardinal features of pre-eclampsia are evident such as renal glomerular endotheliosis and, in some instances, proteinuria [49]. In rats, RUPP pressure between days 14 and 19 of pregnancy induces a full pre-eclampsia pregnancy phenotype, including markedly elevated BP and changes in renal artery flow and glomerular filtration rate [50]. Furthermore, other distinct biological changes occur in the mother, specifically dysfunction of endothelium-dependent vascular relaxation [51,52] and increased circulating levels of sFlt-1 (soluble fms-like tyrosine kinase-1) with a resultant reduction in VEGF and PlGF [53].
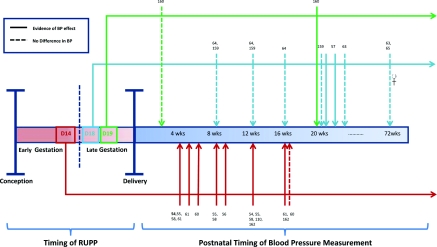
Variations of the RUPP model have been used to study the influence of reduced uterine perfusion on offspring BP and, interestingly, BP does not differ from controls in a large number of the studies [54–62]. Variation in the species investigated or techniques for BP measurement have been postulated to account for this disparity from the observations in humans. However, when all of the studies are considered together (Figure 2), the time when uterine perfusion is reduced appears to be critical. If at 14 days into gestation, changes in resting BP are consistently evident in the offspring throughout life. When uterine perfusion is only introduced late in gestation, despite inducing growth restriction, the studies show either no increase in BP or modest changes in later life that may require stimuli to elicit variability [63–65]. These findings argue for early exposure to uterine perfusion abnormalities to be critical to the BP programming in the offspring. However, early ligation has been associated with the full range of pre-eclampsia-like features in the dams, including deranged anti-angiogenic factors and vascular dysfunction. Therefore an evaluation of the specific relevance of the individual insults is not possible from this model.
Figure 2. Timing of the reduction in uterine artery perfusion and offspring BP.
Summary of the results of studies (reference number given) considering the effect of RUPP at different points of gestation on offspring BP. Continuous lines indicate that studies have demonstrated an increase in BP in RUPP animals compared with controls at this time point, whereas broken lines indicate no difference in BP compared with controls. The colour of the lines indicates the timing of the in utero insult; the red line showing the result of studies in which uterine artery perfusion was reduced at day (D) 14, the blue line at day 18 and the green line at day 19 of gestation. This suggest that the timing of the insult may be critical in determining the effect on offspring BP. Studies of mid-gestation (14 days of gestation) reduction in uterine artery flow have demonstrated relatively consistent increases in BP from early life (4 weeks of age). Interventions later in gestation (days 18 and 19 of gestation) have not indicated consistent increases in early life, although some studies have indicated later development of hypertension which may be linked to dietary factors.
Hypoxia
Placental insufficiency is likely to lead to offspring of pre-eclamptic pregnancies developing in an environment of significant hypoxia from early in pregnancy. In all pregnancies, early placental development takes place under low oxygen conditions as this predates the formation of an effective maternal–fetal circulation [66,67]. Even in later stages of normal pregnancy, fetuses whose mothers have normal placental perfusion and breathe 21% inspired O2 are still exposed to intervillous oxygen levels equivalent to only 8–11% O2. The abnormal placentation in pre-eclampsia is therefore likely to result in significantly lower oxygen delivery to the fetus for the majority of gestation. Interestingly, even in pregnant mice with normal placental development, exposure to an inappropriate level of hypoxia from early in pregnancy (9.5% O2 from day 7.5 to day 17 of gestation) induces a range of pre-eclampsia-like symptoms in the mother, including hypertension, proteinuria, IUGR, renal pathology and elevations in maternal sEng (soluble endoglin) [68]. The underlying reason for this is not clear, although it could be because the degree of hypoxia induced at the level of the placenta is sufficient to trigger the ‘pre-eclampsia cascade’ of events, similar to that present in a mother with abnormal placental development. Consistent with this hypothesis, less severe hypoxia (11% O2) or hypoxia later in gestation (9.5% O2 from day 10 or 15 to day 17 of gestation) does not induce these changes [68].
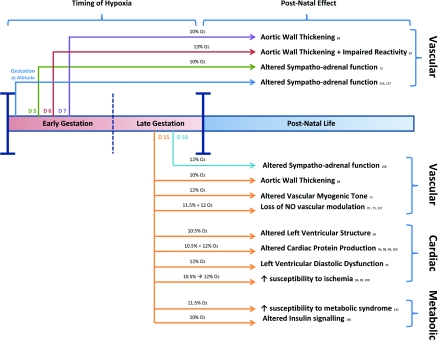
When the data from models of pregnancy hypoxia are collated (Figure 3), despite a range of changes in other cardiovascular measures, there is a striking lack of any consistent reports of elevated BP in the offspring. This may be because the majority of studies are based on the use of oxygen concentrations higher than 9.5% and/or exposed animals later in pregnancy [69–71]. Even in models in which oxygen availability is reduced early in development (days 5–20 of pregnancy), the level of maternal hypoxia (10% O2) has been relatively higher than that normally associated with induction of a pre-eclampsia-like syndrome in the mother. BP variation in the offspring has been demonstrated in response to stress [72], but this BP phenotype is distinct from that observed in human offspring of pre-eclamptic pregnancies, who have increased resting BP in early life [18]. These findings may suggest that hypoxia alone is insufficient to induce the long-term effects of pre-eclampsia seen in the offspring, or that the levels of hypoxia currently used are not representative of the levels offspring are exposed to during development.
Figure 3. Cardiovascular changes associated with in utero exposure to hypoxia.
The major findings from studies (reference number given) considering the effects of pre-natal chronic hypoxia at different points of gestation on offspring cardiovascular physiology are outlined. The colour of the lines indicates the timing of commencement of in utero hypoxia; The dark blue line indicates hypoxia for the entire period of gestation, the green line from day 5, the red line from day 6, the purple line from day 7, the orange line from day 15, and the pale blue line from day 18 of gestation. The percentage of oxygen used in each study is indicated above the lines. Studies have been divided into those where hypoxia was commenced in early pregnancy (before day 10 in rat models or from conception in other animals) and those where hypoxia was commenced later in pregnancy. Studies later in pregnancy have demonstrated vascular, cardiac and metabolic alterations in the offspring. Fewer studies have considered the effects of early-onset hypoxia, but these have demonstrated similar findings in terms of the vascular phenotype.
Anti-angiogenic factors
Multiple studies have now demonstrated a key step in the progression of pre-eclampsia from placental underperfusion and hypoxia to a clinical syndrome is an increase in levels of circulating anti-angiogenic factors. These include sFlt-1, the alternatively spliced truncated form of VEGF receptor 1 [73], and sEng [74–76]. sFlt-1 inhibits the normal function of pregnancy-related angiogenic factors, including VEGF and PlGF [38], and a Sprague–Dawley model of pre-eclampsia based on adenovirus vector administration of sFlt-1 early in the second trimester (days 8–9 of pregnancy), when the levels are seen to increase in human pregnancy, has been developed [74]. This model overexpresses sFlt-1 and the transfected rats develop hypertension, heavy proteinuria and glomerular endotheliosis. These signs also occur in non-pregnant rats treated with sFlt-1 [74], indicative of the broader relevance of deranged anti-angiogenic factors to vascular homoeostasis. The same intervention in mice induces a slightly different phenotype with maternal hypertension, fetal growth restriction and impairment of maternal platelet count [77]. Lu et al. [78] have investigated the effect of administration of an adenovirus carrying sFlt-1 to pregnant mice on offspring BP over the first 6 months of life. They found a sustained increase in BP in male offspring evident from the first day of life, which persisted during the period of measurement. As with other models of pre-eclampsia, a range of clinical features of the condition are induced [79] and specific culpability for sFlt-1 in programming of offspring cardiovasculature cannot be confirmed. Nevertheless, the results suggest that, even with normal placentation and uterine blood flow in early pregnancy, exposure to an excess of anti-angiogenic factors, specifically raised sFlt-1 and its biological sequelae, is sufficient to induce long-term changes in BP in the offspring.
Systemic endothelial dysfunction
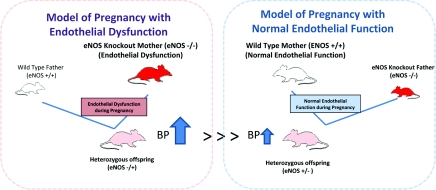
The specific role of systemic maternal endothelial dysfunction is relatively simpler to explore. This is because targeted animal models are available that allow in utero development in a mother with endothelial dysfunction to be studied. These models are based either on systemic inhibition of eNOS (endothelial NO synthase) by administration of L-NAME (NG-nitro-L-arginine methyl ester) or by eNOS knockout [39]. A limitation is that these are not good models of pre-eclampsia itself as the hypertension in eNOS-knockout mice [80] is not pregnancy-specific and, indeed, one study has reported that eNOS-knockout mothers have no difference in BP during pregnancy [81]. Nevertheless, the mice consistently exhibit abnormal endothelial function and, through selective breeding of an eNOS-knockout mother with a wild-type male, an experimental scenario can be generated to study the impact of maternal endothelial dysfunction on the in utero development of an eNOS-heterozygous offspring (Figure 4). These offspring have higher BP during adulthood than the genetically similar offspring bred from a wild-type mother and an eNOS-knockout father, who differ only in that their in utero development was in a wild-type mother with normal endothelial responses [82]. Such findings highlight the potential pivotal importance of maternal endothelial dysfunction during pregnancy, even in the absence of other pre-eclamptic features, on long-term offspring outcome.
Figure 4. Effect of maternal systemic endothelial dysfunction during pregnancy on offspring BP.
Experiments in eNOS-knockout mice have demonstrated the importance of the development in an environment of maternal systemic endothelial dysfunction. eNOS-knockout heterozygotes born to knockout mothers have shown some evidence of increased BP and BP variability compared with heterozygotes gestated in an environment with normal endothelial function. Second-generation offspring also show alterations in BP. Maternal systemic endothelial dysfunction during pregnancy is characteristic of the human syndrome of pre-eclampsia and these models highlight the potential importance of this in utero insult on later offspring vascular function [82].
MECHANISM OF LONG-TERM PROGRAMING? THE CARDIOVASCULAR SYSTEM
The data from available animal models implicate reduced uterine perfusion, if present from early in pregnancy, as well as exposure to anti-angiogenic factors and systemic endothelial dysfunction, from at least the second trimester, as capable of inducing long-term changes in BP in offspring. The evidence for a specific effect of hypoxia is weaker in current animal models, although some changes in BP response if hypoxia occurs from early in pregnancy is observed. To understand how these insults during pregnancy might lead to long-term alterations in BP, a more in-depth study of the cardiovascular phenotype that might be relevant to BP in these experimental models is required.
Vascular structure
A key determinant of BP in humans is arterial stiffness, with increased arterial stiffness being associated with elevation of central BPs [83,84]. Therefore one possibility is that exposure to the abnormal intra-uterine milieu of pre-eclampsia leads to vascular structural remodelling that persists into post-natal life [85]. One RUPP model study has evaluated the stress–stain relationship of offspring arteries and found evidence of increased aortic stiffness, as well as greater elastic fibre content in the vessel wall [63]. Apparently in support of the hypothesis that pre-eclamptic insults induce structural changes in blood vessels are findings from a guinea-pig model of RUPP-exposed offspring, which showed increased thickness of the aortic media [86]. Offspring of dams, hypoxic from early in gestation, were also found to have a thicker aortic media with increased smooth muscle cell density in fetal life [87,88]. However, changes in arterial stiffness are not found in studies of human offspring in adolescence (14 years of age) [11] or young adulthood (20–30 years of age) [12] and, in animal models, by adult life, 16-month-old offspring of hypoxic dams start to exhibit quite distinct vascular structural changes with oedematous and necrotic aortic endothelium and disarranged proliferative smooth muscle cells [89]. These findings are more characteristic of atherogenic vascular remodelling rather than the vascular structural matrix changes associated with abnormal arterial stiffness [84]. Other studies of rat RUPP offspring have also identified an increased propensity to develop arterial internal elastic lamina lesions, an early atherosclerotic process, when studied at 8 and 16 weeks of age [64].
These observations highlight development of an early atherogenic phenotype, independent of BP, as an additional potential link between pre-eclampsia exposure and later cardiovascular disease. Atherosclerosis in humans is characterized by thickening of the arterial intima media, which can be evaluated non-invasively by ultrasound [90], and carotid artery IMT (intima-media thickness) associates with the extent of coronary artery disease [90,91]. Consistent with the observations in animal studies, offspring of pre-eclamptic pregnancies also show an increased IMT in their 20s [12] with aortic arterial thickening already evident at birth [92]. Therefore the features of vascular remodelling that have been observed are predominantly not those associated with the arterial stiffening that underlies BP variation. However, there appear to be significant early atherosclerosis-related changes in the vascular wall, the importance of which require further exploration.
Cardiac structure
An alternative possibility to explain the variation in BP is that the in utero insult alters cardiac development. The structural and functional changes, such as increased cardiac output or LVH [LV (left ventricular) hypertrophy], then predispose to development of hypertension [93]. Hypoxic exposure in pregnancy does lead to abnormalities in cardiac appearances, although these seem to be predominantly of a cardiomyopathic phenotype more commonly linked with the development of heart failure. Rat offspring exposed to hypoxia during late gestation have increased cardiac size relative to body weight [89,94–96], with reduced LV wall thickness, reduced cardiomyocte proliferation and epicardial detachment [96,97]. It has been hypothesized that this detachment of the epicardium in fetal life [97] may be mechanistically related to the changes in the myocardium, as the epicardium is a major source of growth factors during cardiac development [96,97]. Higher levels of apoptotic proteins and induction of HIF (hypoxia-inducible factor)-1α are also evident and may drive some of this process [98,99].
Additionally, offspring cardiac collagen content can be altered by maternal hypoxia, with rats exposed to hypoxia during late gestation having increased cardiac levels of collagen I and III [96,100]. These animals express a complex array of alterations in extracellular matrix regulation so that, by day 21, rat fetuses exposed to hypoxia have decreased MMP (matrix metaloproteinase)-1 and increased MMP-13 and TIMP (tissue inhibitor of metalloproteinases)-3 and TIMP-4. In neonatal life, both MMP-1 and MMP-13 levels are still raised and at 4 months of age MMP-2 levels are reduced [96,100]. Another potential link between in utero hypoxia and later cardiovascular disease is through alterations in cardiac ischaemia/reperfusion mechanisms. Specifically, rats exposed to hypoxia in late gestation have been found to have alterations in cardiac proton production and increased myocardial production of acetyl-CoA during reperfusion [94,99]. In fetal life, such animals also have a significant reduction in cardiac PKCϵ (protein kinase Cϵ), possibly secondary to increased methylation at the PKCϵ promoter site [101]. As PKCϵ plays a critical role in cardioprotection during ischaemia [102], this may underlie the observed differences.
However, these findings need to be interpreted with caution in relation to pre-eclampsia. None of the studies have investigated low levels of hypoxia early in pregnancy and the data for long-term changes in cardiac function are variable. Offspring of Sprague–Dawley rats exposed to hypoxia (12% O2) from days 15 to 21 of pregnancy showed no differences from controls in cardiac function at 4 months of age, as assessed by echocardiography, but, by 12 months, male offspring only demonstrated signs of LVH. In a second study, both male and female offspring had structurally similar hearts, but those exposed to hypoxia had impaired diastolic function and evidence of pulmonary hypertension in later life [95].
In humans, placental tissue from pre-eclamptic pregnancy has differential expression of genes associated with cardiovascular development [103]. However, an 18-year follow-up of children born to hypertensive pregnancies did not show differences in LV mass, as assessed by echocardiography [104]. More recently, one study in children aged 5–8 years exposed to pre-eclampsia in utero found they had smaller hearts, increased heart rate and increased late diastolic velocity at the mitral valve attachments [105]. Overall, a pragmatic conclusion is that more detailed work is needed to understand whether pre-eclampsia leads to cardiac changes in humans. If so, the geometric cardiac changes observed so far are likely to be a distinct pathway to disease, or secondary to BP variation, rather than the primary underlying mechanism for the hypertensive phenotype of the offspring of pre-eclamptic pregnancies.
Vascular function
One possibility is that the variation in BP is driven by underlying induced abnormalities in vascular function, rather than structural cardiovascular changes. In particular, systemic endothelial function is associated with traditional cardiovascular risk factors, including hypertension [106]. Endothelial dysfunction is also an early biological factor in the development of atherosclerotic vascular disease [107,108] and predisposes to the development of LVH [109]. Consistent with vascular function being a central factor in the association between pre-eclampsia and long-term cardiovascular health, abnormalities in vascular responses are found in nearly all offspring models that mimic pre-eclampsia, as well as the majority of human studies of offspring of pre-eclamptic pregnancies. RUPP offspring have enhanced vascular contraction in response to phenylephrine and a reduction in endothelium-dependent relaxation during early life [54,63,110]. Lower flow-mediated vasodilation is also evident up to 12 months of age in rats born to mothers housed under hypoxic conditions, even if only during late gestation (days 15–21 of pregnancy) with relatively high oxygen levels (11.5–12% O2) [69,70]. In more specific ‘pre-eclampsia’ models, long-term effects on endothelial responses are the major adverse change reported in cardiovascular phenotype of male offspring of sFlt-1-induced ‘pre-eclamptic’ mothers. They exhibit the same pattern of higher responses to phenylephrine and reduced vasorelaxation in response to acetylcholine [111] observed in the RUPP offspring model. Mice heterozygous for eNOS, whose mothers were eNOS-knockout and therefore who developed in an in utero environment of endothelial dysfunction, similarly have enhanced phenylephrine-induced contraction and reduced acetylcholine-mediated relaxation compared with heterozygous mice with wild-type mothers [112,113].
This finding is also evident in humans, with young adults (20–30 years of age) born pre-term to hypertensive pregnancies having a distinct vascular phenotype when compared with those born pre-term to normotensive pregnancies, despite both groups demonstrating a similar magnitude of increase in BP when compared with term-born controls [12]. Only those born to hypertensive pregnancies had evidence of impaired flow-mediated endothelial responses. Offspring of pre-eclamptic women also have impaired endothelial function in childhood (5–8 years of age) [114] and adolescence (14 years of age) [11]. Only one study, in children between 9 and 10 years of age, has not been able to demonstrate this difference in endothelial response [15]. Recently, it has been reported that there are endothelium-dependent differences evident within the microvasculature in offspring of pre-eclamptic pregnancies during neonatal life [115], and evidence has been found of endothelial activation at birth based on cord blood analysis [116].
Experimental studies provide some insight into the potential underlying vascular abnormality. In arterial segments from RUPP model offspring, both basal and acetylcholine-induced NO production is reduced and arterial segments from RUPP animals do not demonstrate the normal impairment of acetylcholine-induced vasodilation after L-NAME pre-treatment [54]. This latter observation suggests there may also be a compensatory up-regulation of NO-independent pathways to maintain the vasodilation response. This loss of NO-mediated vasomodulation due to reduced NO production also underlies the vascular dysfunction demonstrated in several studies of rats exposed to hypoxia in utero [69–71,117] and has been observed in studies of HUVECs (human umbilical vein endothelial cells) grown from umbilical cords from pre-eclamptic pregnancies [118].
What might underlie the reduced NO synthesis? A characteristic feature of pre-eclampsia is a derangement of circulating anti-angiogenic factors. Elevated sEng in the pre-eclamptic mother, with resultant alterations in TGF (transforming growth factor)-β signalling, has been directly implicated in reduced NO bioavailability in the mother. Persistent abnormalities in anti-angiogenic factors in the offspring could therefore lead to persistent endothelial dysfunction in later life. Studies during neonatal life demonstrate that the fetus is exposed to elevated anti-angiogenic factors in utero, as amniotic fluid levels of sFlt-1 are higher in pre-eclamptic pregnancies [119] and neonates born to pre-eclamptic pregnancies have significantly higher circulating sFlt-1 and sEng, as well as lower VEGF and PlGF levels [120,121]. However, to date, the only study of anti-angiogenic factors in children of 5–8 years of age has demonstrated no long-term differences [114].
One possibility is that in utero exposure to anti-angiogenic factors leads to altered in utero endothelial development and physiology. Consistent with this hypothesis, sFlt-1 administered in vitro inhibits endothelial cell proliferation and tubule formation [122]. HUVECs from pre-eclamptic donors also appear to differ from normal in their response to oxygen levels. Under normoxic conditions, they develop a higher numbers of connections and shorter tubule lengths, creating networks similar to those seen when control cells were grown under hypoxic conditions [118]. These findings suggest that endothelial cells from pre-eclamptic pregnancies may be fixed in a ‘hypoxic’ phenotype. This ‘hypoxic’ programming may not be endothelium-specific, as gene expression in pre-eclamptic placentae is also similar to that seen in control placental explants grown at 3% O2 [67], and metabolomic studies have demonstrated that pre-eclamptic placental tissue grown under normoxic conditions behaves similarly to control tissue grown under hypoxia [123].
Another possibility is that the endothelial dysfunction represents a biomarker of other underlying metabolic abnormalities related to cardiovascular disease. However, there is limited evidence that pre-eclampsia leads to the metabolic syndrome in the offspring [18,124], with no convincing evidence for changes in serum lipids or glucose tolerance beyond acute transient changes in cord blood samples [12,14,15,114,125–130]. Animal studies of maternal hypoxia suggest that it is possible to induce metabolic changes in animals exposed to a high-fat diet, leading to increased serum leptin, triacylglycerols (triglycerides), non-esterified (‘free’) fatty acids and impaired glucose tolerance [131]. However, the need for a secondary inducer would suggest that lipid and glucose abnormalities are not fundamental features of the underlying hypertensive cardiovascular phenotype.
Alternatively, the vascular changes could be inherited between mother and child. Polymorphisms in certain genes, such as those encoding eNOS, ACE (angiotensin-converting enzyme) and angiotensin, have been proposed as potential links [132] underlying the development of the condition, although no consistent associations have been found [133]. Adverse exposures during fetal life could also lead to heritable characteristics through programming of the epigenome, as the greatest level of active programming of the epigenome occurs during fetal life [134]. This is clearly possible in humans, as placental DNA is hypomethylated following early-, but not late-, onset pre-eclampsia [135,136] and imprinting of non-coding RNA in placental tissue also differs in studies of pre-eclamptic tissues [137]. As epigenetic changes are potentially dynamic [138,139], this mechanism is of interest as a target for intervention [140]. Transgenerational, potentially epigenetic, effects are seen in ‘pre-eclampsia’ models. Elevated BP is evident in the first 12 weeks of life in both male and female second-generation offspring born to RUPP offspring [141]. Such transgenerational effects are also evident in eNOS-knockout models as second-generation offspring born to the eNOS-heterozygous mothers, who developed in an in utero environment of endothelial dysfunction, have increased BP compared with those born to genetically similar mothers who had a normal in utero development.
A potential stimulus for epigenetic programming is hypoxia, which has been shown to induce a global decrease in transcriptional activity in the vascular endothelium [142]. Alternatively, the systemic maternal oxidative stress evident during pre-eclampsia could alter the delicate balance between the production of ROS and cellular defences in the neonate. Oxidative stress has been suggested to influence histone acetylation and phosphorylation [143], telomere length [144] and vascular gene expression. Some oxidative stress is required for normal fetal development [145], but the ischaemic pre-eclamptic placenta has significantly decreased total antioxidant capacity compared with the normal placenta, and there is a correlation between levels of oxidative stress in maternal peripheral blood and cord blood in normotensive and pre-eclamptic pregnancies [146,147], with levels significantly higher in pre-eclampsia [127,147]. The levels of oxidative stress induced by pre-eclampsia itself are sufficient to cause damage to the fetus, as placental tissue samples have higher levels of oxidative DNA damage in pre-eclamptic pregnancies, whether or not there has been fetal growth restriction [148]. This independent effect of pre-eclampsia is not surprising, as fetal antioxidant capacity generally only increases in the last trimester after the increase in oxidative stress observed in early-onset pre-eclampsia [127,149]. Mitochondrial oxidative species may be particularly relevant to this fetal programming mechanism as, following pre-eclampsia, fetal-derived HUVECs have impaired mitochondrial function [150] associated with increased endothelial mitochondrial oxidative species generation.
OTHER POTENTIAL MECHANISMS FOR LONG-TERM PROGRAMING
Altered sympatho-adrenal function
It is also possible that the increased BP following in utero exposure to pre-eclampsia is explained, in part, by non-vascular alterations. The sympathetic nervous system has a key role in regulating BP in humans and overactivity may be associated with development of hypertension [151]. Heart rate variability, a marker of autonomic nervous system function, has been associated with and precedes the development of several cardiovascular risk factors, as well as being a predictor of mortality in high- and low-risk populations [152]. Furthermore, alterations in adrenal function have been associated with features of the metabolic syndrome in adults [153]. Tenhola et al. [14,154] have suggested that, in childhood, children born to a pre-eclamptic mother have increased serum adrenaline, but were not able to demonstrate differences in other adrenal hormones. Despite this lack of human data, there is some supportive evidence from animal models. In particular, hypoxia studies have considered sympatho-adrenal function in both fetal and post-natal life. A chick embryo that has developed at high altitude, and therefore has been exposed to significant hypoxia throughout gestation, has elevated plasma corticotrophin, decreased plasma corticosterone and elevated adrenal adrenaline and noradrenaline compared with those incubated at sea level [155]. Fetuses of pregnant ewes who undergo gestation at high altitude similarly had reduced adrenal mRNA for CYP (cytochrome P450) 17, CYP11A1 and ACTH (corticotropin) [156], and higher eNOS expression in the inner adrenal cortex [157]. There is some evidence that these alterations in sympatho-adrenal programming also persist through post-natal life, as the offspring of Sprague–Dawley rats exposed to hypoxia from pre-natal days 5–20 demonstrate persistent alterations in the levels and utilization of catecholamines in the heart and stellate ganglion at 12 weeks of age [72]. Even shorter exposures later in pregnancy may effect adrenal function, as exposure of rat fetuses to 12% O2 in the last 3 days of gestation led to altered aldosterone levels at 7 days of age [158]. Further studies will be required to elucidate whether this mechanism is significant in humans.
Renal dysfunction
Another possibility is that changes in renal function are central to the programming of hypertension in offspring of pre-eclamptic pregnancies. Offspring of the rat RUPP model have inhibition of the RAS (renin–angiotensin system), and bilateral renal denervation normalizes their BP without influencing BP in control animals [61,62]. RUPP offspring also have reductions in glomerular number [57,65,159], increased glomerular collagen deposition [86], increased glomerular volume [57,159,160], altered renal VEGF expression [161] and alterations in intrarenal renin and angiotensin expression [61], although no difference in plasma renin activity has been demonstrated [59,60,162]. At 18 months of age, female RUPP offspring have increased plasma creatinine and renal expression of TGF-β, MMP-9 and type VI collagen [65]. Additionally, RUPP offspring have reduced renal expression of the glucocorticoid receptor at day 21 after birth and increased mineralocorticoid receptor expression at birth compared with control animals [160]. Similar findings have never been demonstrated in humans, but conceivably these changes would be relevant to BP control and a further understanding of the potential role of pre-eclampsia-induced renal changes in humans subjects requires investigation [163].
Altered immune function and inflammation
Finally, evidence for a further non-vascular non-hypertension pathway of relevance to cardiovascular disease development in the offspring of pre-eclamptic pregnancy has recently emerged. Integration of data from genome-wide gene expression studies of pre-eclamptic decidua basalis tissue with tissue from subjects with a history of familial heart disease has identified commonality between disease processes and several differentially expressed genes relevant to immune function and inflammatory responses [164]. These include NOD1 [NOD (nucleotide-binding and oligomerization domain)-like receptor 1], which plays a key role in intracellular innate immunity [165], and SPPL2 (signal peptide peptidase-like 2), which has been shown to play a role in the release of pro-inflammatory cytokines [166]. Pre-eclampsia involves a range of key immune responses at different stages of the syndrome [34], with the final symptomatic phase characterized by an intense maternal systemic inflammatory response [34]. Women who suffer from autoimmune conditions are at an increased risk of developing pre-eclampsia [167], and in animal models the transfer of activated Th1 cells or infusion of inflammatory cytokines induces pre-eclampsia-like symptoms [168–170]. Inflammation has a key role in cardiovascular disease, with inflammatory cell infiltration of the vessel wall an early pathophysiological stage in the development of atherosclerotic cardiovascular disease [171,172]. Interestingly, neonates born following pre-eclamptic pregnancies have elevated IL (interleukin)-8 and greater percentages of natural killer cells, reduced number of T-cells and altered expression of the Fas/Fas ligand in their umbilical cord blood [173–176]. However, without longer term follow-up it is difficult to determine whether these changes reflect acute changes associated with the pregnancy or long-term changes relevant to disease. A single study of 5–8-year-old children born to women who experienced pre-eclampsia showed no difference in general systemic inflammation, assessed by high-sensitivity CRP (C-reactive protein) [114], but more sophisticated immunological or inflammatory markers were not considered. Nevertheless, given the growing understanding of the importance of inflammation and immune function in the pathophysiology of pre-eclampsia and cardiovascular disease, further investigation of these factors may prove useful in understanding the links between pre-eclampsia and offspring cardiovascular health.
Gender differences and the effect of hormonal status
In addition to other potential programming mechanisms, some studies have suggested the association between exposure to pre-eclampsia and alteration of offspring phenotype may be sex-specific. Animal work suggests that hormonal status may play some role in phenotypic modulation. Lu et al. [78] have demonstrated that the male offspring of sFlt-1-induced ‘pre-eclamptic’ mothers demonstrated a sustained increase in BP from the first day of life, which was not shown in female offspring [78]. The hormonal status of RUPP offspring may play a significant role, as castration of male RUPP offspring has been demonstrated to normalize BP [162], whereas ovarianectomy induced hypertension in otherwise normotensive female RUPP offspring [60]. Such findings suggest that gender-specific hormone expression may mediate or alter the phenotype associated with exposure to adverse intra-uterine conditions. Some human studies of BP in children born to pre-eclamptic mothers have also demonstrated gender differences; however, these differed with some showing elevation in males and some in females [177–179]. A recent meta-analysis of data considering BP in children born to pre-eclamptic pregnancies has suggested that the phenotype is similar in both males and females [18]. Despite this, the findings from animal models arguably suggest that gender-related changes in biology may require closer investigation in relation to other aspects of the phenotype in human populations.
CONCLUSIONS
Pre-eclampsia has a long-term impact on the cardiovascular health of both mother and offspring. The pre-eclamptic in utero environment is characterized by reduced uterine perfusion, hypoxia, raised anti-angiogenic factors and systemic oxidative stress, leading to maternal endothelial dysfunction. Animal studies support the potential relevance of these insults to programming of offspring BP and, in combination with human experimental studies, have demonstrated a range of potential mechanisms for the hypertensive phenotype. In particular, endothelial dysfunction is consistently observed in offspring of both animal and human studies well into adult life. The underlying programming of vascular function may relate to ‘structural’, ‘hypoxic’ or ‘epigenetic’ programming of endothelial development and physiology. In addition, complementary pathways to disease development, including changes in cardiac function, accelerated atherogenesis or alterations in renal and immune function, may emerge as relevant to later disease in offspring of pre-eclamptic pregnancies. Greater understanding of all of these mechanisms will provide the basis for future novel strategies to prevent cardiovascular disease in this high-risk group.
FUNDING
This review is part of a programme of work supported by the British Heart Foundation (BHF) [grant numbers FS/06/024 and FS/11/65/28865], the NIHR Oxford Biomedical Research Centre and the Oxford BHF Centre for Research Excellence (to P.L.). E.F.D. is supported by a Clarendon Scholarship and A.J.L. by a Commonwealth Commission Scholarship.
References
- 1.Wen S. W., Chen X.-K., Rodger M., Rennicks White R., Yang Q., Smith G. N., Sigal R. J., Perkins S. L., Walker M. C. Folic acid supplementation in early second trimester and the risk of preeclampsia. Am. J. Obstet. Gynecol. 2008;198:45.e41–45.e47. doi: 10.1016/j.ajog.2007.06.067. [DOI] [PubMed] [Google Scholar]
- 2.Steegers E.A.P., von Dadelszen P., Duvekot J. J., Pijnenborg R. Pre-eclampsia. Lancet. 2010;376:631–644. doi: 10.1016/S0140-6736(10)60279-6. [DOI] [PubMed] [Google Scholar]
- 3.Bellamy L., Casas J.-P., Hingorani A. D., Williams D. J. Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ. 2007;335:974. doi: 10.1136/bmj.39335.385301.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McDonald S. D., Malinowski A., Zhou Q., Yusuf S., Devereaux P. J. Cardiovascular sequelae of preeclampsia/eclampsia: a systematic review and meta-analyses. Am. Heart J. 2008;156:918–930. doi: 10.1016/j.ahj.2008.06.042. [DOI] [PubMed] [Google Scholar]
- 5.Ferreira I., Peeters L. L., Stehouwer C. D. Preeclampsia and increased blood pressure in the offspring: meta-analysis and critical review of the evidence. J. Hypertens. 2009;27:1955–1959. doi: 10.1097/HJH.0b013e328331b8c6. [DOI] [PubMed] [Google Scholar]
- 6.Kajantie E., Eriksson J. G., Osmond C., Thornburg K., Barker D.J. P. Pre-eclampsia is associated with increased risk of stroke in the adult offspring: the Helsinki Birth Cohort Study. Stroke. 2009;40:1176–1180. doi: 10.1161/STROKEAHA.108.538025. [DOI] [PubMed] [Google Scholar]
- 7.Vatten L. J., Romundstad P. R., Holmen T. L., Hsieh C.-c., Trichopoulos D., Stuver S. O. Intrauterine exposure to preeclampsia and adolescent blood pressure, body size, and age at menarche in female offspring. Obstet. Gynecol. 2003;101:529–533. doi: 10.1016/s0029-7844(02)02718-7. [DOI] [PubMed] [Google Scholar]
- 8.Ogland B., Vatten L. J., Romundstad P. R., Nilsen S. T., Forman M. R. Pubertal anthropometry in sons and daughters of women with preeclamptic or normotensive pregnancies. Arch. Dis. Child. 2009;94:855–859. doi: 10.1136/adc.2008.150870. [DOI] [PubMed] [Google Scholar]
- 9.Kvehaugen A. S., Andersen L. F., Staff A. C. Dietary intake and physical activity in women and offspring after pregnancies complicated by preeclampsia or diabetes mellitus. Acta Obstet. Gynecol. Scand. 2010;89:1486–1490. doi: 10.3109/00016349.2010.519378. [DOI] [PubMed] [Google Scholar]
- 10.Geelhoed J. J. M., Fraser A., Tilling K., Benfield L., Davey Smith G., Sattar N., Nelson S. M., Lawlor D. A. Preeclampsia and gestational hypertension are associated with childhood blood pressure independently of family adiposity measures: the Avon Longitudinal Study of Parents and Children. Circulation. 2010;122:1192–1199. doi: 10.1161/CIRCULATIONAHA.110.936674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jayet P.-Y., Rimoldi S. F., Stuber T., Salmon C. S., Hutter D., Rexhaj E., Thalmann S., Schwab M., Turini P., Sartori-Cucchia C., et al. Pulmonary and systemic vascular dysfunction in young offspring of mothers with preeclampsia. Circulation. 2010;122:488–494. doi: 10.1161/CIRCULATIONAHA.110.941203. [DOI] [PubMed] [Google Scholar]
- 12.Lazdam M., de la Horra A., Pitcher A., Mannie Z., Diesch J., Trevitt C., Kylintireas I., Contractor H., Singhal A., Lucas A., et al. Elevated blood pressure in offspring born premature to hypertensive pregnancy: is endothelial dysfunction the underlying vascular mechanism? Hypertension. 2010;56:159–165. doi: 10.1161/HYPERTENSIONAHA.110.150235. [DOI] [PubMed] [Google Scholar]
- 13.Seidman D. S., Laor A., Gale R., Stevenson D. K., Mashiach S., Danon Y. L. Pre-eclampsia and offspring's blood pressure, cognitive ability and physical development at 17-years-of-age. Br. J. Obstet. Gynaecol. 1991;98:1009–1014. doi: 10.1111/j.1471-0528.1991.tb15339.x. [DOI] [PubMed] [Google Scholar]
- 14.Tenhola S., Rahiala E., Martikainen A., Halonen P., Voutilainen R. Blood pressure, serum lipids, fasting insulin, and adrenal hormones in 12-year-old children born with maternal preeclampsia. J. Clin. Endocrinol. Metab. 2003;88:1217–1222. doi: 10.1210/jc.2002-020903. [DOI] [PubMed] [Google Scholar]
- 15.Lawlor D. A., Macdonald-Wallis C., Fraser A., Nelson S. M., Hingorani A., Davey Smith G., Sattar N., Deanfield J. Cardiovascular biomarkers and vascular function during childhood in the offspring of mothers with hypertensive disorders of pregnancy: findings from the Avon Longitudinal Study of Parents and Children. Eur. Heart J. 2012;33:335–345. doi: 10.1093/eurheartj/ehr300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Øglænd B., Forman M. R., Romundstad P. R., Nilsen S. T., Vatten L. J. Blood pressure in early adolescence in the offspring of preeclamptic and normotensive pregnancies. J. Hypertens. 2009;27:2051–2054. doi: 10.1097/HJH.0b013e328330052a. [DOI] [PubMed] [Google Scholar]
- 17.Leeson P. Pediatric prevention of atherosclerosis: targeting early variation in vascular biology. Pediatrics. 2007;119:1204–1206. doi: 10.1542/peds.2007-0833. [DOI] [PubMed] [Google Scholar]
- 18.Davis E. F., Lazdam M., Lewandowski A. J., Worton S. A., Kelly B. A., Kenworthy Y., Adwani S., Wilkinson A. R., McCormick K., Sargent I., et al. Cardiovascular risk factors in children and young adults born to preeclamptic pregnancies: a systematic review. Pediatrics. 2012 doi: 10.1542/peds.2011-3093. doi:10.1542/peds.2011-3093. [DOI] [PubMed] [Google Scholar]
- 19.Chen X., Wang Y. Tracking of blood pressure from childhood to adulthood: a systematic review and meta-regression analysis. Circulation. 2008;117:3171–3180. doi: 10.1161/CIRCULATIONAHA.107.730366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.NICE. Hypertension (Update) London: National Institute for Health and Clinical Excellence; 2011. [Google Scholar]
- 21.Williams P. J., Broughton Pipkin F. The genetics of pre-eclampsia and other hypertensive disorders of pregnancy. Best Pract. Res. Clin. Obstet. Gynaecol. 2011;25:405–417. doi: 10.1016/j.bpobgyn.2011.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Warner M. J., Ozanne S. E. Mechanisms involved in the developmental programming of adulthood disease. Biochem. J. 2010;427:333–347. doi: 10.1042/BJ20091861. [DOI] [PubMed] [Google Scholar]
- 23.Lucas A. Programming by early nutrition in man. Ciba Found. Symp. 1991;156:38–50. [PubMed] [Google Scholar]
- 24.Bonamy A.-K. E., Norman M., Kaijser M. Being born too small, too early, or both: does it matter for risk of hypertension in the elderly? Am. J. Hypertens. 2008;21:1107–1110. doi: 10.1038/ajh.2008.241. [DOI] [PubMed] [Google Scholar]
- 25.Barker D. J. P. Fetal origins of coronary heart disease. Br. Med. J. 1995;311:171–174. doi: 10.1136/bmj.311.6998.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Barker D. J., Bull A. R., Osmond C., Simmonds S. J. Fetal and placental size and risk of hypertension in adult life. Br. Med. J. 1990;301:259–262. doi: 10.1136/bmj.301.6746.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Barker D. J., Hales C. N., Fall C. H., Osmond C., Phipps K., Clark P. M. Type 2 (non-insulin-dependent) diabetes mellitus, hypertension and hyperlipidaemia (syndrome X): relation to reduced fetal growth. Diabetologia. 1993;36:62–67. doi: 10.1007/BF00399095. [DOI] [PubMed] [Google Scholar]
- 28.Norman M. Preterm birth: an emerging risk factor for adult hypertension? Semin. Perinatol. 2010;34:183–187. doi: 10.1053/j.semperi.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 29.Huxley R. R., Shiell A. W., Law C. M. The role of size at birth and postnatal catch-up growth in determining systolic blood pressure: a systematic review of the literature. J. Hypertens. 2000;18:815–831. doi: 10.1097/00004872-200018070-00002. [DOI] [PubMed] [Google Scholar]
- 30.van der Merwe J. L., Hall D. R., Wright C., Schubert P., Grové D. Are early and late preeclampsia distinct subclasses of the disease-what does the placenta reveal? Hypertens. Pregnancy. 2010;29:457–467. doi: 10.3109/10641950903572282. [DOI] [PubMed] [Google Scholar]
- 31.Touwslager R. N., Houben A. J., Gielen M., Zeegers M. P., Stehouwer C. D., Zimmermann L. J., Kessels A. G., Gerver W. J., Blanco C. E., Mulder A. L. Endothelial vasodilatation in newborns is related to body size and maternal hypertension. J. Hypertens. 2011;31:124–131. doi: 10.1097/HJH.0b013e32834d75c6. [DOI] [PubMed] [Google Scholar]
- 32.Singhal A., Kattenhorn M., Cole T. J., Deanfield J., Lucas A. Preterm birth, vascular function, and risk factors for atherosclerosis. Lancet. 2001;358:1159–1160. doi: 10.1016/S0140-6736(01)06276-6. [DOI] [PubMed] [Google Scholar]
- 33.Kanasaki K., Kalluri R. The biology of preeclampsia. Kidney Int. 2009;76:831–837. doi: 10.1038/ki.2009.284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Redman C. W. G., Sargent I. L. Immunology of pre-eclampsia. Am. J. Reprod. Immunol. 2010;63:534–543. doi: 10.1111/j.1600-0897.2010.00831.x. [DOI] [PubMed] [Google Scholar]
- 35.Redman C. W. G., Sargent I. L. Placental stress and pre-eclampsia: a revised view. Placenta. 2009;30:38–42. doi: 10.1016/j.placenta.2008.11.021. [DOI] [PubMed] [Google Scholar]
- 36.Rodie V. A., Freeman D. J., Sattar N., Greer I. A. Pre-eclampsia and cardiovascular disease: metabolic syndrome of pregnancy? Atherosclerosis. 2004;175:189–202. doi: 10.1016/j.atherosclerosis.2004.01.038. [DOI] [PubMed] [Google Scholar]
- 37.Poston L. Endothelial dysfunction in pre-eclampsia. Pharmacol. Rep. 2006;58(Suppl.):69–74. [PubMed] [Google Scholar]
- 38.Furuya M., Kurasawa K., Nagahama K., Kawachi K., Nozawa A., Takahashi T., Aoki I. Disrupted balance of angiogenic and antiangiogenic signalings in preeclampsia. J. Pregnancy. 2011;2011:123717. doi: 10.1155/2011/123717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sunderland N., Hennessy A., Makris A. Animal models of pre-eclampsia. Am. J. Reprod. Immunol. 2011;65:533–541. doi: 10.1111/j.1600-0897.2010.00929.x. [DOI] [PubMed] [Google Scholar]
- 40.McCarthy F. P., Kingdom J. C., Kenny L. C., Walsh S. K. Animal models of preeclampsia; uses and limitations. Placenta. 2011;32:413–419. doi: 10.1016/j.placenta.2011.03.010. [DOI] [PubMed] [Google Scholar]
- 41.Kaaja R., Laivuori H., Laakso M., Tikkanen M. J., Ylikorkala O. Evidence of a state of increased insulin resistance in preeclampsia. Metab. Clin. Exp. 1999;48:892–896. doi: 10.1016/s0026-0495(99)90225-1. [DOI] [PubMed] [Google Scholar]
- 42.Scioscia M., Gumaa K., Rademacher T. W. The link between insulin resistance and preeclampsia: new perspectives. J. Reprod. Immunol. 2009;82:100–105. doi: 10.1016/j.jri.2009.04.009. [DOI] [PubMed] [Google Scholar]
- 43.Vuguin P. M. Animal models for small for gestational age and fetal programming of adult disease. Horm. Res. 2007;68:113–123. doi: 10.1159/000100545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ogden E., Hildebrand G. J., Page E. W. Rise of blood pressure during ischemia of the gravid uterus. Proc. Soc. Exp. Biol. Med. 1940;43:49–51. [Google Scholar]
- 45.Abitbol M. M., Gallo G. R., Pirani C. L., Ober W. B. Production of experimental toxemia in the pregnant rabbit. Am. J. Obstet. Gynecol. 1976;124:460–470. doi: 10.1016/0002-9378(76)90169-1. [DOI] [PubMed] [Google Scholar]
- 46.Clark K. E., Durnwald M., Austin J. E. A model for studying chronic reduction in uterine blood flow in pregnant sheep. Am. J. Physiol. 1982;242:H297–H301. doi: 10.1152/ajpheart.1982.242.2.H297. [DOI] [PubMed] [Google Scholar]
- 47.Golden J. G., Hughes H. C., Lang C. M. Experimental toxemia in the pregnant guinea pig (Cavia porcellus) Lab. Anim. Sci. 1980;30:174–179. [PubMed] [Google Scholar]
- 48.Cavanagh D., Rao P. S., Tsai C. C., O'Connor T. C. Experimental toxemia in the pregnant primate. Am. J. Obstet. Gynecol. 1977;128:75–85. doi: 10.1016/0002-9378(77)90296-4. [DOI] [PubMed] [Google Scholar]
- 49.Abitbol M. M., Pirani C. L., Ober W. B., Driscoll S. G., Cohen M. W. Production of experimental toxemia in the pregnant dog. Obstet. Gynecol. 1976;48:537–548. [PubMed] [Google Scholar]
- 50.Alexander B. T., Kassab S. E., Miller M. T., Abram S. R., Reckelhoff J. F., Bennett W. A., Granger J. P. Reduced uterine perfusion pressure during pregnancy in the rat is associated with increases in arterial pressure and changes in renal nitric oxide. Hypertension. 2001;37:1191–1195. doi: 10.1161/01.hyp.37.4.1191. [DOI] [PubMed] [Google Scholar]
- 51.Walsh S. K., English F. A., Johns E. J., Kenny L. C. Plasma-mediated vascular dysfunction in the reduced uterine perfusion pressure model of preeclampsia. Hypertension. 2009;54:345–351. doi: 10.1161/HYPERTENSIONAHA.109.132191. [DOI] [PubMed] [Google Scholar]
- 52.Crews J. K., Herrington J. N., Granger J. P., Khalil R. A. Decreased endothelium-dependent vascular relaxation during reduction of uterine perfusion pressure in pregnant rat. Hypertension. 2000;35:367–372. doi: 10.1161/01.hyp.35.1.367. [DOI] [PubMed] [Google Scholar]
- 53.Gilbert J. S., Babcock S. A., Granger J. P. Hypertension produced by reduced uterine perfusion in pregnant rats is associated with increased soluble Fms-like tyrosine kinase-1 expression. Hypertension. 2007;50:1142–1147. doi: 10.1161/HYPERTENSIONAHA.107.096594. [DOI] [PubMed] [Google Scholar]
- 54.Payne J. A., Alexander B. T., Khalil R. A. Reduced endothelial vascular relaxation in growth-restricted offspring of pregnant rats with reduced uterine perfusion. Hypertension. 2003;42:768–774. doi: 10.1161/01.HYP.0000084990.88147.0C. [DOI] [PubMed] [Google Scholar]
- 55.Anderson C. M., Lopez F., Sandeen A., Johnson L. Placental insufficiency: programming of leptin secretion, blood pressure, and postnatal growth in two generations of Sprague-Dawley rats. Biol. Res. Nurs. 2009;10:284–291. doi: 10.1177/1099800408324127. [DOI] [PubMed] [Google Scholar]
- 56.Heltemes A., Gingery A., Soldner E.L. B., Bozadjieva N., Jahr K. N., Johnson B. K., Gilbert J. S. Chronic placental ischemia alters amniotic fluid milieu and results in impaired glucose tolerance, insulin resistance and hyperleptinemia in young rats. Exp. Biol. Med. 2010;235:892–899. doi: 10.1258/ebm.2010.009357. [DOI] [PubMed] [Google Scholar]
- 57.Wlodek M. E., Westcott K., Siebel A. L., Owens J. A., Moritz K. M. Growth restriction before or after birth reduces nephron number and increases blood pressure in male rats. Kidney Int. 2008;74:187–195. doi: 10.1038/ki.2008.153. [DOI] [PubMed] [Google Scholar]
- 58.Alexander B. T. Placental insufficiency leads to development of hypertension in growth-restricted offspring. Hypertension. 2003;41:457–462. doi: 10.1161/01.HYP.0000053448.95913.3D. [DOI] [PubMed] [Google Scholar]
- 59.Ojeda N. B., Johnson W. R., Dwyer T. M., Alexander B. T. Early renal denervation prevents development of hypertension in growth-restricted offspring. Clin. Exp. Pharmacol. Physiol. 2007;34:1212–1216. doi: 10.1111/j.1440-1681.2007.04754.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ojeda N. B., Grigore D., Robertson E. B., Alexander B. T. Estrogen protects against increased blood pressure in postpubertal female growth restricted offspring. Hypertension. 2007;50:679–685. doi: 10.1161/HYPERTENSIONAHA.107.091785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Grigore D., Ojeda N. B., Robertson E. B., Dawson A. S., Huffman C. A., Bourassa E. A., Speth R. C., Brosnihan K. B., Alexander B. T. Placental insufficiency results in temporal alterations in the renin angiotensin system in male hypertensive growth restricted offspring. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2007;293:R804–R811. doi: 10.1152/ajpregu.00725.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Alexander B. T., Hendon A. E., Ferril G., Dwyer T. M. Renal denervation abolishes hypertension in low-birth-weight offspring from pregnant rats with reduced uterine perfusion. Hypertension. 2005;45:754–758. doi: 10.1161/01.HYP.0000153319.20340.2a. [DOI] [PubMed] [Google Scholar]
- 63.Mazzuca M. Q., Wlodek M. E., Dragomir N. M., Parkington H. C., Tare M. Uteroplacental insufficiency programs regional vascular dysfunction and alters arterial stiffness in female offspring. J. Physiol. 2010;588:1997–2010. doi: 10.1113/jphysiol.2010.187849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pascoe K. C., Wlodek M. E., Jones G. T. Increased elastic tissue defect formation in the growth restricted brown Norway rat: a potential link between in utero condition and cardiovascular disease. Pediatr. Res. 2008;64:125–130. doi: 10.1203/PDR.0b013e3181761859. [DOI] [PubMed] [Google Scholar]
- 65.Moritz K. M., Mazzuca M. Q., Siebel A. L., Mibus A., Arena D., Tare M., Owens J. A., Wlodek M. E. Uteroplacental insufficiency causes a nephron deficit, modest renal insufficiency but no hypertension with ageing in female rats. J. Physiol. 2009;587:2635–2646. doi: 10.1113/jphysiol.2009.170407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zamudio S. The placenta at high altitude. High Alt. Med. Biol. 2003;4:171–191. doi: 10.1089/152702903322022785. [DOI] [PubMed] [Google Scholar]
- 67.Soleymanlou N., Jurisica I., Nevo O., Ietta F., Zhang X., Zamudio S., Post M., Caniggia I. Molecular evidence of placental hypoxia in preeclampsia. J. Clin. Endocrinol. Metab. 2005;90:4299–4308. doi: 10.1210/jc.2005-0078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lai Z., Kalkunte S., Sharma S. A critical role of interleukin-10 in modulating hypoxia-induced preeclampsia-like disease in mice. Hypertension. 2011;57:505–514. doi: 10.1161/HYPERTENSIONAHA.110.163329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Morton J. S., Rueda-Clausen C. F., Davidge S. T. Flow-mediated vasodilation is impaired in adult rat offspring exposed to prenatal hypoxia. J. Appl. Physiol. 2011;110:1073–1082. doi: 10.1152/japplphysiol.01174.2010. [DOI] [PubMed] [Google Scholar]
- 70.Williams S. J., Hemmings D. G., Mitchell J. M., McMillen I. C., Davidge S. T. Effects of maternal hypoxia or nutrient restriction during pregnancy on endothelial function in adult male rat offspring. J. Physiol. 2005;565:125–135. doi: 10.1113/jphysiol.2005.084889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hemmings D. G., Williams S. J., Davidge S. T. Increased myogenic tone in 7-month-old adult male but not female offspring from rat dams exposed to hypoxia during pregnancy. Am. J. Physiol. Heart Circ. Physiol. 2005;289:H674–H682. doi: 10.1152/ajpheart.00191.2005. [DOI] [PubMed] [Google Scholar]
- 72.Peyronnet J., Dalmaz Y., Ehrström M., Mamet J., Roux J.-C., Pequignot J.-M., Thorén P., Lagercrantz H. Long-lasting adverse effects of prenatal hypoxia on developing autonomic nervous system and cardiovascular parameters in rats. Pflügers Arch. 2002;443:858–865. doi: 10.1007/s00424-001-0766-9. [DOI] [PubMed] [Google Scholar]
- 73.Mutter W. P., Karumanchi S. A. Molecular mechanisms of preeclampsia. Microvasc. Res. 2008;75:1–8. doi: 10.1016/j.mvr.2007.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Maynard S. E., Min J.-Y., Merchan J., Lim K.-H., Li J., Mondal S., Libermann T. A., Morgan J. P., Sellke F. W., Stillman I. E., et al. Excess placental soluble fms-like tyrosine kinase 1 (sFlt1) may contribute to endothelial dysfunction, hypertension, and proteinuria in preeclampsia. J. Clin. Invest. 2003;111:649–658. doi: 10.1172/JCI17189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ahmad S., Ahmed A. Elevated placental soluble vascular endothelial growth factor receptor-1 inhibits angiogenesis in preeclampsia. Circ. Res. 2004;95:884–891. doi: 10.1161/01.RES.0000147365.86159.f5. [DOI] [PubMed] [Google Scholar]
- 76.Levine R. J., Maynard S. E., Qian C., Lim K.-H., England L. J., Yu K. F., Schisterman E. F., Thadhani R., Sachs B. P., Epstein F. H., et al. Circulating angiogenic factors and the risk of preeclampsia. N. Engl. J. Med. 2004;350:672–683. doi: 10.1056/NEJMoa031884. [DOI] [PubMed] [Google Scholar]
- 77.Lu F., Longo M., Tamayo E., Maner W., Al-Hendy A., Anderson G. D., Hankins G.D. V., Saade G. R. The effect of over-expression of sFlt-1 on blood pressure and the occurrence of other manifestations of preeclampsia in unrestrained conscious pregnant mice. Am. J. Obstet. Gynecol. 2007;196:396.e1–396.e7. doi: 10.1016/j.ajog.2006.12.024. [DOI] [PubMed] [Google Scholar]
- 78.Lu F., Bytautiene E., Tamayo E., Gamble P., Anderson G. D., Hankins G. D., Longo M., Saade G. R. Gender-specific effect of overexpression of sFlt-1 in pregnant mice on fetal programming of blood pressure in the offspring later in life. Am. J. Obstet. Gynecol. 2007;197:418.e1–418.e5. doi: 10.1016/j.ajog.2007.06.064. [DOI] [PubMed] [Google Scholar]
- 79.Maynard S., Epstein F. H., Karumanchi S. A. Preeclampsia and angiogenic imbalance. Annu. Rev. Med. 2008;59:61–78. doi: 10.1146/annurev.med.59.110106.214058. [DOI] [PubMed] [Google Scholar]
- 80.Huang P. L., Huang Z., Mashimo H., Bloch K. D., Moskowitz M. A., Bevan J. A., Fishman M. C. Hypertension in mice lacking the gene for endothelial nitric oxide synthase. Nature. 1995;377:239–242. doi: 10.1038/377239a0. [DOI] [PubMed] [Google Scholar]
- 81.Shesely E. G., Gilbert C., Granderson G., Carretero C. D., Carretero O. A., Beierwaltes W. H. Nitric oxide synthase gene knockout mice do not become hypertensive during pregnancy. Am. J. Obstet. Gynecol. 2001;185:1198–1203. doi: 10.1067/mob.2001.118142. [DOI] [PubMed] [Google Scholar]
- 82.Van Vliet B. N., Chafe L. L. Maternal endothelial nitric oxide synthase genotype influences offspring blood pressure and activity in mice. Hypertension. 2007;49:556–562. doi: 10.1161/01.HYP.0000257876.87284.3c. [DOI] [PubMed] [Google Scholar]
- 83.Mitchell G. F., Conlin P. R., Dunlap M. E., Lacourcière Y., Arnold J. M. O., Ogilvie R. I., Neutel J., Izzo J. L., Pfeffer M. A. Aortic diameter, wall stiffness, and wave reflection in systolic hypertension. Hypertension. 2008;51:105–111. doi: 10.1161/HYPERTENSIONAHA.107.099721. [DOI] [PubMed] [Google Scholar]
- 84.Shirwany N. A., Zou M.-h. Arterial stiffness: a brief review. Acta Pharmacol. Sin. 2010;31:1267–1276. doi: 10.1038/aps.2010.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lewandowski A. J., Lazdam M., Davis E., Kylintireas I., Diesch J., Francis J., Neubauer S., Singhal A., Lucas A., Kelly B., Leeson P. Short-term exposure to exogenous lipids in premature infants and long-term changes in aortic and cardiac function. Arterioscler. Thromb. Vasc. Biol. 2011;31:2125–2135. doi: 10.1161/ATVBAHA.111.227298. [DOI] [PubMed] [Google Scholar]
- 86.Briscoe T. A., Rehn A. E., Dieni S., Duncan J. R., Wlodek M. E., Owens J. A., Rees S. M. Cardiovascular and renal disease in the adolescent guinea pig after chronic placental insufficiency. Am. J. Obstet. Gynecol. 2004;191:847–855. doi: 10.1016/j.ajog.2004.01.050. [DOI] [PubMed] [Google Scholar]
- 87.Herrera E. A., Camm E. J., Cross C. M., Mullender J. L., Wooding F. B., Giussani D. A. Morphological and functional alterations in the aorta of the chronically hypoxic fetal rat. J. Vasc. Res. 2011;49:50–58. doi: 10.1159/000330666. [DOI] [PubMed] [Google Scholar]
- 88.Camm E. J., Hansell J. A., Kane A. D., Herrera E. A., Lewis C., Wong S., Morrell N. W., Giussani D. A. Partial contributions of developmental hypoxia and undernutrition to prenatal alterations in somatic growth and cardiovascular structure and function. Am. J. Obstet. Gynecol. 2010;203:495.e24–495.e34. doi: 10.1016/j.ajog.2010.06.046. [DOI] [PubMed] [Google Scholar]
- 89.Wang Z., Huang Z., Lu G., Lin L., Ferrari M. Hypoxia during pregnancy in rats leads to early morphological changes of atherosclerosis in adult offspring. Am. J. Physiol. Heart Circ. Physiol. 2009;296:H1321–H1328. doi: 10.1152/ajpheart.00440.2008. [DOI] [PubMed] [Google Scholar]
- 90.Urbina E. M., Williams R. V., Alpert B. S., Collins R. T., Daniels S. R., Hayman L., Jacobson M., Mahoney L., Mietus-Snyder M., Rocchini A., et al. Noninvasive assessment of subclinical atherosclerosis in children and adolescents: recommendations for standard assessment for clinical research: a scientific statement from the American Heart Association. Hypertension. 2009;54:919–950. doi: 10.1161/HYPERTENSIONAHA.109.192639. [DOI] [PubMed] [Google Scholar]
- 91.Lorenz M. W., Markus H. S., Bots M. L., Rosvall M., Sitzer M. Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and meta-analysis. Circulation. 2007;115:459–467. doi: 10.1161/CIRCULATIONAHA.106.628875. [DOI] [PubMed] [Google Scholar]
- 92.Akcakus M., Altunay L., Yikilmaz A., Yazici C., Koklu E. The relationship between abdominal aortic intima-media thickness and lipid profile in neonates born to mothers with preeclampsia. J. Pediatr. Endocrinol. Metab. 2010;23:1143–1149. doi: 10.1515/jpem.2010.179. [DOI] [PubMed] [Google Scholar]
- 93.Aeschbacher B. C., Hutter D., Fuhrer J., Weidmann P., Delacretaz E., Allemann Y. Diastolic dysfunction precedes myocardial hypertrophy in the development of hypertension. Am. J. Hypertens. 2001;14:106–113. doi: 10.1016/s0895-7061(00)01245-0. [DOI] [PubMed] [Google Scholar]
- 94.Rueda-Clausen C. F., Morton J. S., Lopaschuk G. D., Davidge S. T. Long-term effects of intrauterine growth restriction on cardiac metabolism and susceptibility to ischaemia/reperfusion. Cardiovasc. Res. 2011;90:285–294. doi: 10.1093/cvr/cvq363. [DOI] [PubMed] [Google Scholar]
- 95.Rueda-Clausen C. F., Morton J. S., Davidge S. T. Effects of hypoxia-induced intrauterine growth restriction on cardiopulmonary structure and function during adulthood. Cardiovasc. Res. 2009;81:713–722. doi: 10.1093/cvr/cvn341. [DOI] [PubMed] [Google Scholar]
- 96.Tong W., Xue Q., Li Y., Zhang L. Maternal hypoxia alters matrix metalloproteinase expression patterns and causes cardiac remodeling in fetal and neonatal rats. Am. J. Physiol. Heart Circ. Physiol. 2011;301:H2113–H2122. doi: 10.1152/ajpheart.00356.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ream M., Ray A. M., Chandra R., Chikaraishi D. M. Early fetal hypoxia leads to growth restriction and myocardial thinning. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2008;295:R583–R595. doi: 10.1152/ajpregu.00771.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Bae S., Xiao Y., Li G., Casiano C. A., Zhang L. Effect of maternal chronic hypoxic exposure during gestation on apoptosis in fetal rat heart. Am. J. Physiol. Heart Circ. Physiol. 2003;285:H983–H990. doi: 10.1152/ajpheart.00005.2003. [DOI] [PubMed] [Google Scholar]
- 99.Li G., Xiao Y., Estrella J. L., Ducsay C. A., Gilbert R. D., Zhang L. Effect of fetal hypoxia on heart susceptibility to ischemia and reperfusion injury in the adult rat. J. Soc. Gynecol. Investig. 2003;10:265–274. doi: 10.1016/s1071-5576(03)00074-1. [DOI] [PubMed] [Google Scholar]
- 100.Xu Y., Williams S. J., O'Brien D., Davidge S. T. Hypoxia or nutrient restriction during pregnancy in rats leads to progressive cardiac remodeling and impairs postischemic recovery in adult male offspring. FASEB J. 2006;20:1251–1253. doi: 10.1096/fj.05-4917fje. [DOI] [PubMed] [Google Scholar]
- 101.Patterson A. J., Chen M., Xue Q., Xiao D., Zhang L. Chronic prenatal hypoxia induces epigenetic programming of PKCϵ gene repression in rat hearts: novelty and significance. Circ. Res. 2010;107:365–373. doi: 10.1161/CIRCRESAHA.110.221259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Budas G. R., Mochly-Rosen D. Mitochondrial protein kinase Cϵ (PKCϵ): emerging role in cardiac protection from ischaemic damage. Biochem. Soc. Trans. 2007;35:1052–1054. doi: 10.1042/BST0351052. [DOI] [PubMed] [Google Scholar]
- 103.Enquobahrie D. A., Abetew D. F., Sorensen T. K., Willoughby D., Chidambaram K., Williams M. A. Placental microRNA expression in pregnancies complicated by preeclampsia. Am. J. Obstet. Gynecol. 2011;204:178.e12–178.e21. doi: 10.1016/j.ajog.2010.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Himmelmann A., Svensson A., Hansson L. Five-year follow-up of blood pressure and left ventricular mass in children with different maternal histories of hypertension: the Hypertension in Pregnancy Offspring Study. J. Hypertens. 1994;12:89–95. [PubMed] [Google Scholar]
- 105.Fugelseth D., Ramstad H. B., Kvehaugen A. S., Nestaas E., Støylen A., Staff A. C. Myocardial function in offspring 5–8 years after pregnancy complicated by preeclampsia. Early Hum. Dev. 2011;87:531–535. doi: 10.1016/j.earlhumdev.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 106.Hadi H. A., Carr C. S., Al Suwaidi J. Endothelial dysfunction: cardiovascular risk factors, therapy, and outcome. Vasc. Health Risk Manag. 2005;1:183–198. [PMC free article] [PubMed] [Google Scholar]
- 107.Halcox J.P. J., Donald A. E., Ellins E., Witte D. R., Shipley M. J., Brunner E. J., Marmot M. G., Deanfield J. E. Endothelial function predicts progression of carotid intima-media thickness. Circulation. 2009;119:1005–1012. doi: 10.1161/CIRCULATIONAHA.108.765701. [DOI] [PubMed] [Google Scholar]
- 108.Luscher T. F. The endothelium and cardiovascular disease: a complex relation. N. Engl. J. Med. 1994;330:1081–1083. doi: 10.1056/NEJM199404143301511. [DOI] [PubMed] [Google Scholar]
- 109.Lazdam M., Lewandowski A. J., Kylintireas I., Cunnington C., Diesch J., Francis J., Trevitt C., Neubauer S., Singhal A., Leeson P. Impaired endothelial responses in apparently healthy young people associated with subclinical variation in blood pressure and cardiovascular phenotype. Am. J. Hypertens. 2012;25:46–53. doi: 10.1038/ajh.2011.176. [DOI] [PubMed] [Google Scholar]
- 110.Payne J. A., Alexander B. T., Khalil R. A. Decreased endothelium-dependent NO-cGMP vascular relaxation and hypertension in growth-restricted rats on a high-salt diet. Hypertension. 2004;43:420–427. doi: 10.1161/01.HYP.0000111832.47667.13. [DOI] [PubMed] [Google Scholar]
- 111.Lu F., Goharkhay N., Bytautiene E., Tamayo E., Orise P., Anderson G. D., Longo M., Saade G. R. Fetal programming of adult vascular function in a preeclampsia-like animal model is gender-specific. Am. J. Obstet. Gynecol. 2007;197:S141–S141. [Google Scholar]
- 112.Chiossi G., Costantine M. M., Tamayo E. H., Orise P., Hankins G. D. V., Saade G. R., Longo M. Effect of age and gender on the progression of adult vascular dysfunction in a mouse model of fetal programming lacking endothelial nitric oxide synthase. Am. J. Physiol. Heart Circ. Physiol. 2011;301:H297–H305. doi: 10.1152/ajpheart.01284.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Longo M., Jain V., Vedernikov Y. P., Bukowski R., Garfield R. E., Hankins G. D., Anderson G. D., Saade G. R. Fetal origins of adult vascular dysfunction in mice lacking endothelial nitric oxide synthase. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2005;288:R1114–R1121. doi: 10.1152/ajpregu.00367.2004. [DOI] [PubMed] [Google Scholar]
- 114.Kvehaugen A. S., Dechend R., Ramstad H. B., Troisi R., Fugelseth D., Staff A. C. Endothelial function and circulating biomarkers are disturbed in women and children after preeclampsia. Hypertension. 2011;58:63–69. doi: 10.1161/HYPERTENSIONAHA.111.172387. [DOI] [PubMed] [Google Scholar]
- 115.Touwslager R. N., Houben A. J., Gielen M., Zeegers M. P., Stehouwer C. D., Zimmermann L. J., Kessels A. G., Gerver W. J., Blanco C. E., Mulder A. L. Endothelial vasodilatation in newborns is related to body size and maternal hypertension. J. Hypertens. 2012;30:124–131. doi: 10.1097/HJH.0b013e32834d75c6. [DOI] [PubMed] [Google Scholar]
- 116.Davidge S. T., Signorella A. P., Lykins D. L., Gilmour C. H., Roberts J. M. Evidence of endothelial activation and endothelial activators in cord blood of infants of preeclamptic women. Am. J. Obstet. Gynecol. 1996;175:1301–1306. doi: 10.1016/s0002-9378(96)70045-5. [DOI] [PubMed] [Google Scholar]
- 117.Morton J. S., Rueda-Clausen C. F., Davidge S. T. Mechanisms of endothelium-dependent vasodilation in male and female, young and aged offspring born growth restricted. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2010;298:R930–R938. doi: 10.1152/ajpregu.00641.2009. [DOI] [PubMed] [Google Scholar]
- 118.Moyes A. J., Maldonado-Perez D., Gray G. A., Denison F. C. Enhanced angiogenic capacity of human umbilical vein endothelial cells from women with preeclampsia. Reprod. Sci. 2011;18:374–382. doi: 10.1177/1933719110385131. [DOI] [PubMed] [Google Scholar]
- 119.Staff A. C., Braekke K., Harsem N. K., Lyberg T., Holthe M. R. Circulating concentrations of sFlt1 (soluble fms-like tyrosine kinase 1) in fetal and maternal serum during pre-eclampsia. Eur. J. Obstet. Gynecol. Reprod. Biol. 2005;122:33–39. doi: 10.1016/j.ejogrb.2004.11.015. [DOI] [PubMed] [Google Scholar]
- 120.Tsao P.-N., Wei S.-C., Su Y.-N., Chou H.-C., Chen C.-Y., Hsieh W.-S. Excess soluble fms-like tyrosine kinase 1 and low platelet counts in premature neonates of preeclamptic mothers. Pediatrics. 2005;116:468–472. doi: 10.1542/peds.2004-2240. [DOI] [PubMed] [Google Scholar]
- 121.Orbak Z., Zor N., Energin V. M., Selimoğlu M. A., ALP H., Akçay F. Endothelin-1 levels in mothers with eclampsia-pre-eclampsia and their newborns. J. Trop. Pediatr. 1998;44:47–49. doi: 10.1093/tropej/44.1.47. [DOI] [PubMed] [Google Scholar]
- 122.Wang Y., Zhou Y., He L., Hong K., Su H., Wu Y., Wu Q., Han M., Cheng X. Gene delivery of soluble vascular endothelial growth factor receptor-1 (sFlt-1) inhibits intra-plaque angiogenesis and suppresses development of atherosclerotic plaque. Clin. Exp. Med. 2011;11:113–121. doi: 10.1007/s10238-010-0112-7. [DOI] [PubMed] [Google Scholar]
- 123.Heazell A. E., Brown M., Worton S. A., Dunn W. B. The effects of oxygen on normal and pre-eclamptic placental tissue–insights from metabolomics. Placenta. 2011;32(Suppl. 2):S119–S124. doi: 10.1016/j.placenta.2010.12.001. [DOI] [PubMed] [Google Scholar]
- 124.Libby G., Murphy D., McEwan N., Greene S., Forsyth J., Chien P., Morris A. Pre-eclampsia and the later development of type 2 diabetes in mothers and their children: an intergenerational study from the Walker cohort. Diabetologia. 2007;50:523–530. doi: 10.1007/s00125-006-0558-z. [DOI] [PubMed] [Google Scholar]
- 125.Akcakus M., Koklu E., Baykan A., Yikilmaz A., Coskun A., Gunes T., Kurtoglu S., Narin N. Macrosomic newborns of diabetic mothers are associated with increased aortic intima-media thickness and lipid concentrations. Horm. Res. 2007;67:277–283. doi: 10.1159/000098157. [DOI] [PubMed] [Google Scholar]
- 126.Catarino C., Rebelo I., Belo L., Rocha-Pereira P., Rocha S., Bayer Castro E., Patrício B., Quintanilha A., Santos-Silva A. Fetal lipoprotein changes in pre-eclampsia. Acta Obstetr. Gynecol. Scand. 2008;87:628–634. doi: 10.1080/00016340802085318. [DOI] [PubMed] [Google Scholar]
- 127.Howlader M. Z., Parveen S., Tamanna S., Khan T. A., Begum F. Oxidative stress and antioxidant status in neonates born to pre-eclamptic mother. J. Trop. Pediatr. 2009;55:363–367. doi: 10.1093/tropej/fmp025. [DOI] [PubMed] [Google Scholar]
- 128.Ophir E., Dourleshter G., Hirsh Y., Fait V., German L., Bornstein J. Newborns of pre-eclamptic women: a biochemical difference present in utero. Acta Obstet. Gynecol. Scand. 2006;85:1172–1178. doi: 10.1080/00016340600697272. [DOI] [PubMed] [Google Scholar]
- 129.Rodie V. A., Caslake M. J., Stewart F., Sattar N., Ramsay J. E., Greer I. A., Freeman D. J. Fetal cord plasma lipoprotein status in uncomplicated human pregnancies and in pregnancies complicated by pre-eclampsia and intrauterine growth restriction. Atherosclerosis. 2004;176:181–187. doi: 10.1016/j.atherosclerosis.2004.04.026. [DOI] [PubMed] [Google Scholar]
- 130.Yavuz T., Yavuz O., Ozdemir I., Afsar Y. Cord blood lipoprotein profile after magnesium sulphate treatment in pre-eclamptic patients. Acta Paediatr. 2006;95:1224–1227. doi: 10.1080/08035250600589017. [DOI] [PubMed] [Google Scholar]
- 131.Rueda-Clausen C. F., Dolinsky V. W., Morton J. S., Proctor S. D., Dyck J. R. B., Davidge S. T. Hypoxia-induced intrauterine growth restriction increases the susceptibility of rats to high-fat diet-induced metabolic syndrome. Diabetes. 2011;60:507–516. doi: 10.2337/db10-1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Medica I., Kastrin A., Peterlin B. Genetic polymorphisms in vasoactive genes and preeclampsia: a meta-analysis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2007;131:115–126. doi: 10.1016/j.ejogrb.2006.10.005. [DOI] [PubMed] [Google Scholar]
- 133.Yu C. K., Casas J. P., Savvidou M. D., Sahemey M. K., Nicolaides K. H., Hingorani A. D. Endothelial nitric oxide synthase gene polymorphism (Glu298Asp) and development of pre-eclampsia: a case-control study and a meta-analysis. BMC Pregnancy Childbirth. 2006;6:7. doi: 10.1186/1471-2393-6-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Odom L. N., Taylor H. S. Environmental induction of the fetal epigenome. Expert Rev. Obstet. Gynecol. 2010;5:657–664. doi: 10.1586/EOG.10.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Yuen R. K. C., Penaherrera M. S., von Dadelszen P., McFadden D. E., Robinson W. P. DNA methylation profiling of human placentas reveals promoter hypomethylation of multiple genes in early-onset preeclampsia. Eur. J. Hum. Genet. 2010;18:1006–1012. doi: 10.1038/ejhg.2010.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Gao W.-l., Li D., Xiao Z.-x., Liao Q.-p., Yang H.-x., Li Y.-x., Ji L., Wang Y.-l. Detection of global DNA methylation and paternally imprinted H19 gene methylation in preeclamptic placentas. Hypertens. Res. 2011;34:655–661. doi: 10.1038/hr.2011.9. [DOI] [PubMed] [Google Scholar]
- 137.Yu L., Chen M., Zhao D., Yi P., Lu L., Han J., Zheng X., Zhou Y., Li L. The H19 gene imprinting in normal pregnancy and pre-eclampsia. Placenta. 2009;30:443–447. doi: 10.1016/j.placenta.2009.02.011. [DOI] [PubMed] [Google Scholar]
- 138.Bannister A. J., Kouzarides T. Reversing histone methylation. Nature. 2005;436:1103–1106. doi: 10.1038/nature04048. [DOI] [PubMed] [Google Scholar]
- 139.Weaver I. C. G., Champagne F. A., Brown S. E., Dymov S., Sharma S., Meaney M. J., Szyf M. Reversal of maternal programming of stress responses in adult offspring through methyl supplementation: altering epigenetic marking later in life. J. Neurosci. 2005;25:11045–11054. doi: 10.1523/JNEUROSCI.3652-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Lewandowski A. J., Davis E. F., Lazdam M., Leeson P. From gene to epigene-based therapies targeting the vascular endothelium. Curr. Vasc. Pharmacol. 2011;21:21. doi: 10.2174/157016112798829814. [DOI] [PubMed] [Google Scholar]
- 141.Anderson C. M., Lopez F., Zimmer A., Benoit J. N. Placental insufficiency leads to developmental hypertension and mesenteric artery dysfunction in two generations of Sprague-Dawley rat offspring. Biol. Reprod. 2006;74:538–544. doi: 10.1095/biolreprod.105.045807. [DOI] [PubMed] [Google Scholar]
- 142.Shirodkar A. V., Marsden P. A. Epigenetics in cardiovascular disease. Curr. Opin. Cardiol. 2011;26:209–215. doi: 10.1097/HCO.0b013e328345986e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Rahman I., Marwick J., Kirkham P. Redox modulation of chromatin remodeling: impact on histone acetylation and deacetylation, NF-κB and pro-inflammatory gene expression. Biochem. Pharmacol. 2004;68:1255–1267. doi: 10.1016/j.bcp.2004.05.042. [DOI] [PubMed] [Google Scholar]
- 144.von Zglinicki T. Oxidative stress shortens telomeres. Trends Biochem. Sci. 2002;27:339–344. doi: 10.1016/s0968-0004(02)02110-2. [DOI] [PubMed] [Google Scholar]
- 145.Dennery P. A. Oxidative stress in development: Nature or nurture? Free Radical Biol. Med. 2010;49:1147–1151. doi: 10.1016/j.freeradbiomed.2010.07.011. [DOI] [PubMed] [Google Scholar]
- 146.Arikan S., Konukoglu D., Arikan C., Akcay T., Davas I. Lipid peroxidation and antioxidant status in maternal and cord blood. Gynecol. Obstet. Invest. 2001;51:145–149. doi: 10.1159/000052913. [DOI] [PubMed] [Google Scholar]
- 147.Erdem M., Harma M., Harma I., Arikan I., Barut A. Comparative study of oxidative stress in maternal blood with that of cord blood and maternal milk. Arch. Gynecol. Obstet. 2012;285:1–5. doi: 10.1007/s00404-011-1993-8. [DOI] [PubMed] [Google Scholar]
- 148.Fujimaki A., Watanabe K., Mori T., Kimura C., Shinohara K., Wakatsuki A. Placental oxidative DNA damage and its repair in preeclamptic women with fetal growth restriction. Placenta. 2011;32:367–372. doi: 10.1016/j.placenta.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 149.Davis J. M., Auten R. L. Maturation of the antioxidant system and the effects on preterm birth. Semin. Fetal Neonatal Med. 2010;15:191–195. doi: 10.1016/j.siny.2010.04.001. [DOI] [PubMed] [Google Scholar]
- 150.Illsinger S., Janzen N., Sander S., Schmidt K. H., Bednarczyk J., Mallunat L., Bode J., Hagebolling F., Hoy L., Lucke T., et al. Preeclampsia and HELLP syndrome: impaired mitochondrial function in umbilical endothelial cells. Reprod. Sci. 2010;17:219–226. doi: 10.1177/1933719109351597. [DOI] [PubMed] [Google Scholar]
- 151.Hart E., Charkoudian N. Sympathetic neural mechanisms in human blood pressure regulation. Curr. Hypertens. Rep. 2011;13:237–243. doi: 10.1007/s11906-011-0191-1. [DOI] [PubMed] [Google Scholar]
- 152.Thayer J. F., Yamamoto S. S., Brosschot J. F. The relationship of autonomic imbalance, heart rate variability and cardiovascular disease risk factors. Int. J. Cardiol. 2010;141:122–131. doi: 10.1016/j.ijcard.2009.09.543. [DOI] [PubMed] [Google Scholar]
- 153.Phillips D. I. W., Jones A., Goulden P. A. Birth weight, stress, and the metabolic syndrome in adult life. Ann. N.Y. Acad. Sci. 2006;1083:28–36. doi: 10.1196/annals.1367.027. [DOI] [PubMed] [Google Scholar]
- 154.Tenhola S., Rahiala E., Halonen P., Vanninen E., Voutilainen R. Maternal preeclampsia predicts elevated blood pressure in 12-year-old children: evaluation by ambulatory blood pressure monitoring. Pediatr. Res. 2006;59:320–324. doi: 10.1203/01.pdr.0000196734.54473.e3. [DOI] [PubMed] [Google Scholar]
- 155.Salinas C. E., Villena M., Blanco C. E., Giussani D. A. Adrenocortical suppression in highland chick embryos is restored during incubation at sea level. High Alt. Med. Biol. 2011;12:79–87. doi: 10.1089/ham.2010.1040. [DOI] [PubMed] [Google Scholar]
- 156.Myers D. A., Hyatt K., Mlynarczyk M., Bird I. M., Ducsay C. A. Long-term hypoxia represses the expression of key genes regulating cortisol biosynthesis in the near-term ovine fetus. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2005;289:R1707–R1714. doi: 10.1152/ajpregu.00343.2005. [DOI] [PubMed] [Google Scholar]
- 157.Monau T. R., Vargas V. E., King N., Yellon S. M., Myers D. A., Ducsay C. A. Long-term hypoxia increases endothelial nitric oxide synthase expression in the ovine fetal adrenal. Reprod. Sci. 2009;16:865–874. doi: 10.1177/1933719109336678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Raff H., Bruder E., Jankowski B., Engeland W. The effect of fetal hypoxia on adrenocortical function in the 7-day-old rat. Endocrine. 2000;13:111–116. doi: 10.1385/ENDO:13:1:111. [DOI] [PubMed] [Google Scholar]
- 159.Wlodek M. E., Mibus A., Tan A., Siebel A. L., Owens J. A., Moritz K. M. Normal lactational environment restores nephron endowment and prevents hypertension after placental restriction in the rat. J. Am. Soc. Nephrol. 2007;18:1688–1696. doi: 10.1681/ASN.2007010015. [DOI] [PubMed] [Google Scholar]
- 160.Baserga M., Hale M. A., Wang Z. M., Yu X., Callaway C. W., McKnight R. A., Lane R. H. Uteroplacental insufficiency alters nephrogenesis and downregulates cyclooxygenase-2 expression in a model of IUGR with adult-onset hypertension. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2007;292:R1943–R1955. doi: 10.1152/ajpregu.00558.2006. [DOI] [PubMed] [Google Scholar]
- 161.Baserga M., Bares A. L., Hale M. A., Callaway C. W., McKnight R. A., Lane P. H., Lane R. H. Uteroplacental insufficiency affects kidney VEGF expression in a model of IUGR with compensatory glomerular hypertrophy and hypertension. Early Hum. Dev. 2009;85:361–367. doi: 10.1016/j.earlhumdev.2008.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Ojeda N. B., Grigore D., Yanes L. L., Iliescu R., Robertson E. B., Zhang H., Alexander B. T. Testosterone contributes to marked elevations in mean arterial pressure in adult male intrauterine growth restricted offspring. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2007;292:R758–R763. doi: 10.1152/ajpregu.00311.2006. [DOI] [PubMed] [Google Scholar]
- 163.Weir M. R. Hypertension and the kidney: perspectives on the relationship of kidney disease and cardiovascular disease. Clin. J. Am. Soc. Nephrol. 2009;4:2045–2050. doi: 10.2215/CJN.03050509. [DOI] [PubMed] [Google Scholar]
- 164.Johansson A., Curran J. E., Johnson M. P., Freed K. A., Fenstad M. H., Bjorge L., Eide I. P., Carless M. A., Rainwater D. L., Goring H. H. H., et al. Identification of ACOX2 as a shared genetic risk factor for preeclampsia and cardiovascular disease. Eur. J. Hum. Genet. 2011;19:796–800. doi: 10.1038/ejhg.2011.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Geddes K., Magalhaes J. G., Girardin S. E. Unleashing the therapeutic potential of NOD-like receptors. Nat. Rev. Drug Discovery. 2009;8:465–479. doi: 10.1038/nrd2783. [DOI] [PubMed] [Google Scholar]
- 166.Friedmann E., Hauben E., Maylandt K., Schleeger S., Vreugde S., Lichtenthaler S. F., Kuhn P.-H., Stauffer D., Rovelli G., Martoglio B. SPPL2a and SPPL2b promote intramembrane proteolysis of TNFα in activated dendritic cells to trigger IL-12 production. Nat. Cell Biol. 2006;8:843–848. doi: 10.1038/ncb1440. [DOI] [PubMed] [Google Scholar]
- 167.Duckitt K., Harrington D. Risk factors for pre-eclampsia at antenatal booking: systematic review of controlled studies. BMJ. 2005;330:565. doi: 10.1136/bmj.38380.674340.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Zenclussen A. C., Fest S., Joachim R., Klapp B. F., Arck P. C. Introducing a mouse model for pre-eclampsia: adoptive transfer of activated Th1 cells leads to pre-eclampsia-like symptoms exclusively in pregnant mice. Eur. J. Immunol. 2004;34:377–387. doi: 10.1002/eji.200324469. [DOI] [PubMed] [Google Scholar]
- 169.LaMarca B. B. D., Bennett W. A., Alexander B. T., Cockrell K., Granger J. P. Hypertension produced by reductions in uterine perfusion in the pregnant rat. Hypertension. 2005;46:1022–1025. doi: 10.1161/01.HYP.0000175476.26719.36. [DOI] [PubMed] [Google Scholar]
- 170.LaMarca B. B. D., Cockrell K., Sullivan E., Bennett W., Granger J. P. Role of endothelin in mediating tumor necrosis factor-induced hypertension in pregnant rats. Hypertension. 2005;46:82–86. doi: 10.1161/01.HYP.0000169152.59854.36. [DOI] [PubMed] [Google Scholar]
- 171.Hansson G. K., Hermansson A. The immune system in atherosclerosis. Nat. Immunol. 2011;12:204–212. doi: 10.1038/ni.2001. [DOI] [PubMed] [Google Scholar]
- 172.Roifman I., Beck P. L., Anderson T. J., Eisenberg M. J., Genest J. Chronic inflammatory diseases and cardiovascular risk: a systematic review. Can. J. Cardiol. 2011;27:174–182. doi: 10.1016/j.cjca.2010.12.040. [DOI] [PubMed] [Google Scholar]
- 173.Laskowska M., Laskowska K., Leszczyńska-Gorzelak B., Oleszczuk J. Comparative analysis of the maternal and umbilical interleukin-8 levels in normal pregnancies and in pregnancies complicated by preeclampsia with intrauterine normal growth and intrauterine growth retardation. J. Matern.-Fetal Neonat. Med. 2007;20:527–532. doi: 10.1080/14767050701412719. [DOI] [PubMed] [Google Scholar]
- 174.Bujold E., Chaiworapongsa T., Romero R., Gervasi M. T., Espinoza J., Goncalves L. F., Berman S., Yoon B. H., Kim Y. M. Neonates born to pre-eclamptic mothers have a higher percentage of natural killer cells (CD3−/CD56+16+) in umbilical cord blood than those without pre-eclampsia. J. Matern.-Fetal Neonat. Med. 2003;14:305–312. doi: 10.1080/jmf.14.5.305.312. [DOI] [PubMed] [Google Scholar]
- 175.Kuntz T. B., Christensen R. D., Stegner J., Duff A., Patrick A., Koenig J. M. Fas and Fas ligand expression in maternal blood and in umbilical cord blood in preeclampsia. Pediatr. Res. 2001;50:743–749. doi: 10.1203/00006450-200112000-00019. [DOI] [PubMed] [Google Scholar]
- 176.Baker D. A., Hameed C., Tejani N., Thomas J., Dattwyler R. Lymphocyte subsets in the neonates of preeclamptic mothers. Am. J. Reprod. Immunol. Microbiol. 1987;14:107–109. doi: 10.1111/j.1600-0897.1987.tb00129.x. [DOI] [PubMed] [Google Scholar]
- 177.Langford H., Watson R. Prepregnant blood pressure, hypertension during pregnancy, and later blood pressure of mothers and offspring. Hypertension. 1980;2:130–133. [PubMed] [Google Scholar]
- 178.Palti H., Rothschild E. Blood pressure and growth at 6 years of age among offsprings of mothers with hypertension of pregnancy. Early Hum. Dev. 1989;19:263–269. doi: 10.1016/0378-3782(89)90061-3. [DOI] [PubMed] [Google Scholar]
- 179.Higgins M., Keller J., Moore F., Ostrander L., Metzner H., Stock L. Studies of blood pressure in Tecumseh, Michigan. I. Blood pressure in young people and its relationship to personal and familial characteristics and complications of pregnancy in mothers. Am. J. Epidemiol. 1980;111:142–155. doi: 10.1093/oxfordjournals.aje.a112882. [DOI] [PubMed] [Google Scholar]
- 180.Schreuder M. F., van Wijk J. A., Delemarre-van de Waal H. A. Intrauterine growth restriction increases blood pressure and central pulse pressure measured with telemetry in aging rats. J. Hypertens. 2006;24:1337–1343. doi: 10.1097/01.hjh.0000234114.33025.fd. [DOI] [PubMed] [Google Scholar]
- 181.Bytautiene E., Tamayo E., Kechichian T., Drever N., Gamble P., Hankins G. D. V., Saade G. R. Prepregnancy obesity and sFlt1-induced preeclampsia in mice: developmental programming model of metabolic syndrome. Am. J. Obstet. Gynecol. 2011;204:398.e1–398.e8. doi: 10.1016/j.ajog.2011.02.031. [DOI] [PubMed] [Google Scholar]
- 182.Costantine M. M., Ghulmiyyah L. M., Tamayo E., Hankins G. D. V., Saade G. R., Longo M. Transgenerational effect of fetal programming on vascular phenotype and reactivity in endothelial nitric oxide synthase knockout mouse model. Am. J. Obstet. Gynecol. 2008;199:250.e1–250.e7. doi: 10.1016/j.ajog.2008.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Miller F. C., Read J. A., Cabal L., Siassi B. Heart rate and blood pressure in infants of pre-eclamptic mothers during the first hour of life. Crit. Care Med. 1983;11:532–535. doi: 10.1097/00003246-198307000-00010. [DOI] [PubMed] [Google Scholar]
- 184.Kvehaugen A. S., Andersen L. F., Staff A. C. Anthropometry and cardiovascular risk factors in women and offspring after pregnancies complicated by preeclampsia or diabetes mellitus. Acta Obstet. Gynecol. Scand. 2010;89:1478–1485. doi: 10.3109/00016349.2010.500368. [DOI] [PubMed] [Google Scholar]
- 185.Hiller J. E., Crowther C. A., Moore V. A., Willson K., Robinson J. S. Calcium supplementation in pregnancy and its impact on blood pressure in children and women: follow up of a randomised controlled trial. Aust. N.Z. J. Obstet. Gynaecol. 2007;47:115–121. doi: 10.1111/j.1479-828X.2007.00696.x. [DOI] [PubMed] [Google Scholar]
- 186.Longo M., Jain V., Langenveld J., Vedernikov Y. P., Garfield R. E., Hankins G. D. V., Anderson G. D., Saade G. R. Enhanced growth and improved vascular function in offspring from successive pregnancies in endothelial nitric oxide synthase knockout mice. Am. J. Obstet. Gynecol. 2004;191:1470–1476. doi: 10.1016/j.ajog.2004.05.043. [DOI] [PubMed] [Google Scholar]
- 187.Veas C. J., Aguilera V. C., Munoz I. J., Gallardo V. I., Miguel P. L., Gonzalez M. A., Lamperti L. I., Escudero C. A., Aguayo C. R. Fetal endothelium dysfunction is associated with circulating maternal levels of sE-selectin, sVCAM1, and sFlt-1 during pre-eclampsia. J. Matern.-Fetal Neonatal. Med. 2011;24:1371–1377. doi: 10.3109/14767058.2011.556204. [DOI] [PubMed] [Google Scholar]
- 188.Byers B. D., Betancourt A., Lu F., Hankins G. D. V., Longo M., Saade G. R., Bytautiene E. The effect of prepregnancy obesity and sFlt-1-induced preeclampsia-like syndrome on fetal programming of adult vascular function in a mouse model. Am. J. Obstet. Gynecol. 2009;200:432.e1–432.e7. doi: 10.1016/j.ajog.2009.01.044. [DOI] [PubMed] [Google Scholar]
- 189.Cetinkaya M., Bostan O., Koksal N., Semizel E., Ozkan H., Cakir S. Early left ventricular diastolic dysfunction in premature infants born to preeclamptic mothers. J. Perinat. Med. 2011;39:89–95. doi: 10.1515/jpm.2010.126. [DOI] [PubMed] [Google Scholar]
- 190.Xue Q., Dasgupta C., Chen M., Zhang L. Foetal hypoxia increases cardiac AT2R expression and subsequent vulnerability to adult ischaemic injury. Cardiovasc. Res. 2011;89:300–308. doi: 10.1093/cvr/cvq303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Ghulmiyyah L. M., Costantine M. M., Yin H., Tamayo E., Clark S. M., Hankins G. D. V., Saade G. R., Longo M. The role of oxidative stress in the developmental origin of adult hypertension. Am. J. Obstet. Gynecol. 2011;205:155.e7–155.e11. doi: 10.1016/j.ajog.2011.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Engelbregt M. J., van Weissenbruch M. M., Popp-Snijders C., Lips P., Delemarre-van de Waal H. A. Body mass index, body composition, and leptin at onset of puberty in male and female rats after intrauterine growth retardation and after early postnatal food restriction. Pediatr. Res. 2001;50:474–478. doi: 10.1203/00006450-200110000-00009. [DOI] [PubMed] [Google Scholar]
- 193.Ojeda N. B., Royals T. P., Black J. T., Dasinger J. H., Johnson J. M., Alexander B. T. Enhanced sensitivity to acute angiotensin II is testosterone dependent in adult male growth-restricted offspring. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2010;298:R1421–R1427. doi: 10.1152/ajpregu.00096.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Simmons R. A., Templeton L. J., Gertz S. J. Intrauterine growth retardation leads to the development of Type 2 diabetes in the rat. Diabetes. 2001;50:2279–2286. doi: 10.2337/diabetes.50.10.2279. [DOI] [PubMed] [Google Scholar]
- 195.Nüsken K.-D., Dötsch J., Rauh M., Rascher W., Schneider H. Uteroplacental insufficiency after bilateral uterine artery ligation in the rat: impact on postnatal glucose and lipid metabolism and evidence for metabolic programming of the offspring by sham operation. Endocrinology. 2008;149:1056–1063. doi: 10.1210/en.2007-0891. [DOI] [PubMed] [Google Scholar]
- 196.Camm E. J., Martin-Gronert M. S., Wright N. L., Hansell J. A., Ozanne S. E., Giussani D. A. Prenatal hypoxia independent of undernutrition promotes molecular markers of insulin resistance in adult offspring. FASEB J. 2011;25:420–427. doi: 10.1096/fj.10-158188. [DOI] [PubMed] [Google Scholar]
- 197.Styrud J., Eriksson U. J., Grill V., Swenne I. Experimental intrauterine growth retardation in the rat causes a reduction of pancreatic β-cell mass, which persists into adulthood. Biol. Neonate. 2005;88:122–128. doi: 10.1159/000086136. [DOI] [PubMed] [Google Scholar]
- 198.Goland R. S., Tropper P. J., Warren W. B., Stark R. I., Jozak S. M., Conwell I. M. Concentrations of corticotrophin-releasing hormone in the umbilical-cord blood of pregnancies complicated by pre-eclampsia. Reprod. Fertil. Dev. 1995;7:1227–1230. doi: 10.1071/rd9951227. [DOI] [PubMed] [Google Scholar]
- 199.Laatikainen T., Virtanen T., Kaaja R., Salminen-Lappalainen K. Corticotropin-releasing hormone in maternal and cord plasma in pre-eclampsia. Eur. J. Obstet. Gynecol. Reprod. Biol. 1991;39:19–24. doi: 10.1016/0028-2243(91)90136-9. [DOI] [PubMed] [Google Scholar]
- 200.Jansson T., Lambert G. W. Effect of intrauterine growth restriction on blood pressure, glucose tolerance and sympathetic nervous system activity in the rat at 3–4 months of age. J. Hypertens. 1999;17:1239–1248. doi: 10.1097/00004872-199917090-00002. [DOI] [PubMed] [Google Scholar]
- 201.Sitras V., Paulssen R. H., Grønaas H., Leirvik J., Hanssen T. A., Vårtun Å., Acharya G. Differential placental gene expression in severe preeclampsia. Placenta. 2009;30:424–433. doi: 10.1016/j.placenta.2009.01.012. [DOI] [PubMed] [Google Scholar]
- 202.Zhu X.-m., Han T., Sargent I. L., Yin G.-w., Yao Y.-q. Differential expression profile of microRNAs in human placentas from preeclamptic pregnancies vs normal pregnancies. Am. J. Obstet. Gynecol. 2009;200:661.e1–661.e7. doi: 10.1016/j.ajog.2008.12.045. [DOI] [PubMed] [Google Scholar]
- 203.Hoegh A. M., Borup R., Nielsen F. C., Sorensen S., Hviid T. V. Gene expression profiling of placentas affected by pre-eclampsia. J. Biomed. Biotechnol. 2010;2010:787545. doi: 10.1155/2010/787545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Centlow M., Wingren C., Borrebaeck C., Brownstein M. J., Hansson S. R. Differential gene expression analysis of placentas with increased vascular resistance and pre-eclampsia using whole-genome microarrays. J. Pregnancy. 2011;2011:472354. doi: 10.1155/2011/472354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Loset M., Mundal S. B., Johnson M. P., Fenstad M. H., Freed K. A., Lian I. A., Eide I. P., Bjorge L., Blangero J., Moses E. K., Austgulen R. A transcriptional profile of the decidua in preeclampsia. Am. J. Obstet. Gynecol. 2011;204:84.e1–84.e27. doi: 10.1016/j.ajog.2010.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Várkonyi T., Nagy B., Füle T., Tarca A. L., Karászi K., Schönléber J., Hupuczi P., Mihalik N., Kovalszky I., Rigó J., Jr, et al. Microarray profiling reveals that placental transcriptomes of early-onset HELLP syndrome and preeclampsia are similar. Placenta. 2011;32(Suppl. 1):S21–S29. doi: 10.1016/j.placenta.2010.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Ozturk E., Balat O., Acılmıs Y. G., Ozcan C., Pence S., Erel Ö. Measurement of the placental total antioxidant status in preeclamptic women using a novel automated method. J. Obstet. Gynaecol. Res. 2011;37:337–342. doi: 10.1111/j.1447-0756.2010.01346.x. [DOI] [PubMed] [Google Scholar]
- 208.McElrath T. F., Fichorova R. N., Allred E. N., Hecht J. L., Ismail M. A., Yuan H., Leviton A. Blood protein profiles of infants born before 28 weeks differ by pregnancy complication. Am. J. Obstet. Gynecol. 2011;204:418.e1–e418.e12. doi: 10.1016/j.ajog.2010.12.010. [DOI] [PubMed] [Google Scholar]