Abstract
Background
Genes that, when mutated, cause Fanconi anemia or greatly increase breast cancer risk encode for proteins that converge on a homology-directed DNA damage repair process. Mutations in the SLX4 gene, which encodes for a scaffold protein involved in the repair of interstrand cross-links, have recently been identified in unclassified Fanconi anemia patients. A mutation analysis of SLX4 in German or Byelorussian familial cases of breast cancer without detected mutations in BRCA1 or BRCA2 has been completed, with globally negative results.
Methods
The genomic region of SLX4, comprising all exons and exon-intron boundaries, was sequenced in 94 Spanish familial breast cancer cases that match a criterion indicating the potential presence of a highly-penetrant germline mutation, following exclusion of BRCA1 or BRCA2 mutations.
Results
This mutational analysis revealed extensive genetic variation of SLX4, with 21 novel single nucleotide variants; however, none could be linked to a clear alteration of the protein function. Nonetheless, genotyping 10 variants (nine novel, all missense amino acid changes) in a set of controls (138 women and 146 men) did not detect seven of them.
Conclusions
Overall, while the results of this study do not identify clearly pathogenic mutations of SLX4 contributing to breast cancer risk, further genetic analysis, combined with functional assays of the identified rare variants, may be warranted to conclusively assess the potential link with the disease.
Background
A functionally coherent network of gene and/or protein interactions, altered in Fanconi anemia (FA) and breast cancer (BrCa), has emerged in recent years [1]. Fifteen genes that, when mutated, cause FA (FANC genes) and several genes that may harbor mutations of high, moderate or low penetrance for BrCa risk encode for proteins that converge on a homology-directed DNA damage repair process [2]. As further evidence of a fundamental common causal basis between these diseases, germline bi- and mono-allelic loss-of-function mutations in four of these genes cause FA and BrCa, respectively: FANCD1/BRCA2 [3,4], FANCJ/BRIP1 [5-8], FANCN/PALB2 [9-11] and FANCO/RAD51C [12,13] (more recent data suggests that mutations in RAD51C may be primarily linked to ovarian cancer risk [14]). This evidence marks any novel gene involved in the aforementioned network or process as a candidate to harbor mutations in unclassified FA and/or BrCa patients.
Interstrand DNA cross-link agents, such as mitomycin-C used in diagnostic tests for FA, block replication forks and may therefore cause genome instability. Homologs of SLX4 in model organisms were initially identified as necessary for replication fork restart following exposure to DNA-damaging agents [15]. Subsequently, SLX4 homologs have been shown to play a key role as docking molecules for the repair of interstrand cross-links [16,17]. These observations pointed to the human SLX4 gene as a FANC candidate for unclassified patients and, as a result, two groups have recently described mutations (renamed FANCP gene or FA-P subtype) [18,19]. The potential link to BrCa risk has been examined, to date, in 52 German or Byelorussian patients with familial breast cancer [20]: the study has not revealed truncating or clearly pathogenic mutations, but has identified four unclassified missense variants. Here, we conducted a more detailed study of the SLX4 gene in 94 index BrCa cases from Spanish families negative for BRCA1 and BRCA2 mutations. As recently reported [20], our results do not show truncating or clearly pathogenic mutations, although they do describe seven missense variants of unknown biological significance that are not found in controls.
Methods
Study samples
Since its creation in 1999, the Hereditary Cancer Program at the ICO has identified a set of high-risk families with suspected hereditary breast and/or ovarian cancer syndrome. Following the Catalan Consensus Onco Guidelines on genetic testing for this condition, patients are analysed for mutations in the BRCA1 or BRCA2 genes after receiving appropriate genetic counselling and providing written informed consent. This genetic analysis consists of screening for point mutations and large rearrangements affecting those genes. For the present study, a total of 94 affected individuals belonging to 94 unrelated families negative for BRCA1 or BRCA2 mutations were selected. In addition to negativity for mutations in BRCA1 or BRCA2, the inclusion criteria were: at least three first-degree relatives affected by breast or ovarian cancer; or at least two first-degree female relatives affected by breast cancer (at least one of them diagnosed before the age of 50); or at least one case of female breast cancer plus at least one case of either ovarian, female bilateral breast, or male breast cancer. Among the selected cases, 10 families were represented with an elevated prior risk of harboring a high-penetrance mutation, as calculated with the BRCAPRO [21] algorithm (briefly, 94 families mean = 0.40, standard deviation = 0.26, 95% confidence interval 0.11-0.99). Control samples, consisting of 138 women and 146 men, were taken from a hospital-based cancer association study (a detailed description of the study population, composition and interviews has been given elsewhere [22]). Specifically, these individuals were randomly enrolled from non-cancer patients admitted to the same general hospital as the BrCa cases. To avoid selection bias, the inclusion criterion for controls was that the current admission to the hospital should be for a new disease (not previously diagnosed). The studies were approved by the IDIBELL ethics committee and participants gave written informed consent for their participation, and for the genetic analysis of their biological samples, according to the Declaration of Helsinki.
Mutation analysis
The SLX4 exons and exon-intron boundaries were sequenced from polymerase chain reactions using previously defined primers and conditions [18]; for exon 7, AmpliTaq Gold DNA Polymerase (Applied Biosystems) and 10% of dimethyl sulfoxide were used. The reaction products were purified from remaining primers using ExoSAP-IT (GE Healthcare) and sequencing reactions performed following a standard Sanger method with the BigDye Terminator v3.1 Cycle Sequencing Kit (Applied Biosystems). Samples harboring DNA variants were re-sequenced at least once using an independent DNA aliquot from the first-pass analysis. The guidelines of the Human Genome Variation Society and the reference sequences NM_032444.2 and NP_115820.2 of the National Center for Biotechnology Information were used for nomenclature.
Genotyping
Assays based on the KASPar technology were performed following the manufacturer's instructions (KBioscience). Reactions were carried out in a 384-well format with 2% of duplicates, and negative and positive (i.e. BrCa patient carrier) sample controls present in each plate.
Results and discussion
The genomic region of SLX4, comprising all exons and exon-intron boundaries, was sequenced in 94 BrCa familial cases that match a criterion indicating the potential presence of a highly-penetrant germline mutation, following exclusion of BRCA1 or BRCA2 mutations (see Methods). This mutational analysis revealed 49 variants: 21 novel and 28 which are currently annotated in the single nucleotide polymorphism database (dbSNP [23]) (Table 1). Of the 49 variants, 21 were found only once, which include three changes identified by the 1,000 Genomes Project [24] (Table 1): rs72778139-T has no known frequency data; rs76488917-A has an allele frequency of 0.02 in Caucasians; and rs115694169-A has an allele frequency of 0.03 in the Yoruba people of Ibadan (there is no data for Caucasians). Excluding these from the set of 21 with low frequency revealed eight missense and five silent changes at the protein level, and five intronic changes (Table 1). A neural network splicing prediction [25] model did not strongly support alteration by any of the identified intronic variants (data not shown). Together, these results suggest extensive genetic variation at the SLX4 locus among individuals in our population, but provide no obvious link to BrCa risk.
Table 1.
SLX4 variants found in non-BRCA1/2-mutated familial BrCa cases
| Exon | Nucleotide change | Change type |
Amino acid change | Number of carriers* | dbSNP† | ||
|---|---|---|---|---|---|---|---|
| Het (%) | Hom (%) | Total | |||||
| 2 | c.248G > C | Missense | p.Gly83Ala | 1 (1.1) | 0 | 94 | NA |
| 2 | c.339T > C | Silent | p. = | 1 (1.1) | 0 | 94 | NA |
| 2 | c.421G > T | Missense | p.Gly141Trp | 1 (1.1) | 0 | 94 | NA |
| 3 | c.555C > T | Silent | p. = | 9 (9.5) | 0 | 94 | rs74640850 |
| 3 | c.610C > T | Missense | p.Arg204Cys | 10 (10.6) | 0 | 94 | rs79842542 |
| 3 | c.678C > T | Silent | p. = | 3 (3.2) | 0 | 94 | rs28516461 |
| 3 | c.590T > C | Missense | p.Val197Ala | 1 (1.1) | 0 | 94 | NA |
| 3 | c.710G > A | Missense | p.Arg237Gln | 2 (2.1) | 0 | 94 | NA |
| 3 | c.753G > A | Silent | p. = | 24 (25.5) | 2 (2.1) | 94 | rs8061528 |
| 4 | c.761-32T > G | Intronic | p. = | 2 (2.1) | 0 | 94 | NA |
| 5 | c.1152A > G | Silent | p. = | 11 (11.7) | 0 | 94 | rs112511042 |
| 5 | c.1153C > A | Missense | p.Pro385Thr | 1 (1.1) | 0 | 94 | rs115694169 |
| 5 | c.1156A > G | Missense | p.Met386Val | 11 (11.7) | 0 | 94 | rs113490934 |
| 5 | c.1163 + 10C > T | Intronic | p. = | 11 (11.7) | 0 | 94 | rs80116508 |
| 6 | c.1164-16T > C | Intronic | p. = | 1 (1.1) | 0 | 94 | NA |
| 6 | c.1164-40C > A | Intronic | p. = | 1 (1.1) | 0 | 94 | NA |
| 6 | c.1164-66T > A | Intronic | p. = | 2 (2.1) | 0 | 94 | NA |
| 6 | c.1164-75C > G | Intronic | p. = | 11 (11.7) | 0 | 94 | rs59622164 |
| 6 | c.1366 + 11T > C | Intronic | p. = | 12 (12.8) | 0 | 94 | rs76350200 |
| 7 | c.1371T > G | Missense | p.Asn457Lys | 10 (10.6) | 0 | 94 | rs74319927 |
| 7 | c.1419C > T | Silent | p. = | 1 (1.1) | 0 | 94 | NA |
| 8 | c.1846G > A | Missense | p.Val616Met | 1 (1.1) | 0 | 94 | NA |
| 9 | c.2012T > C | Missense | p.Leu671Ser | 11 (11.8) | 0 | 93 | rs77985244 |
| 9 | c.2013 + 23G > A | Intronic | p. = | 11 (11.7) | 0 | 94 | rs112226642 |
| 9 | c.2013 + 137G > C | Intronic | p. = | 11 (11.7) | 0 | 94 | rs80186343 |
| 10 | c.2160 + 50C > T | Intronic | p. = | 10 (10.6) | 0 | 94 | rs75762935 |
| 12 | c.2346C > T | Silent | p. = | 1 (1.1) | 0 | 94 | NA |
| 12 | c.2469G > C | Missense | p.Trp823Cys | 1 (1.1) | 0 | 94 | NA |
| 12 | c.2854G > A | Missense | p.Ala952Thr | 8 (8.5) | 0 | 94 | rs59939128 |
| 12 | c.2855C > T | Missense | p.Ala952Val | 8 (8.5) | 0 | 94 | rs78637028 |
| 12 | c.3162G > A | Silent | p. = | 1 (1.1) | 0 | 94 | rs76488917 |
| 12 | c.3365C > T | Missense | p.Pro1122Leu | 12 (12.8) | 1 (1.1) | 94 | rs714181 |
| 12 | c.3662C > T | Missense | p.Ala1221Val | 10 (10.6) | 0 | 94 | rs3827530 |
| 12 | c.3812C > T | Missense | p.Ser1271Phe | 4 (4.2) | 0 | 94 | rs3810813 |
| 12 | c.3872C > T | Missense | p.Thr1291Met | 1 (1.1) | 0 | 94 | NA |
| 12 | c.4261A > T | Missense | p.Ile1421Phe | 1 (1.1) | 0 | 94 | NA |
| 12 | c.4409C > T | Missense | p.Pro1470Leu | 1 (1.1) | 0 | 94 | rs72778139 |
| 12 | c.4500T > C | Silent | p. = | 42 (44.7) | 21 (22.3) | 94 | rs3810812 |
| 12 | c.4530G > T | Silent | p. = | 1 (1.1) | 0 | 94 | NA |
| 13 | c.4637-125C > T | Intronic | p. = | 1 (1.1) | 0 | 94 | NA |
| 13 | c.4637-227C > T | Intronic | p. = | 9 (9.6) | 0 | 94 | rs75693937 |
| 13 | c.4739 + 10C > T | Intronic | p. = | 1 (1.1) | 0 | 94 | NA |
| 13 | c.4739 + 24G > T | Intronic | p. = | 20 (21.3) | 2 (2.1) | 94 | rs12933120 |
| 14 | c.5072A > G | Missense | p.Asn1691Ser | 1 (1.1) | 0 | 94 | NA |
| 15 | c.5389C > T | Silent | p. = | 1 (1.1) | 0 | 93 | NA |
| 15 | c.5501A > G | Missense | p.Asn1834Ser | 2 (2.2) | 0 | 93 | rs111738042 |
| 15 | c.*8A > G | Intronic | p. = | 9 (9.7) | 0 | 93 | rs3751839 |
| 15 | c.*102G > A | Intronic | p. = | 1 (1.1) | 0 | 93 | NA |
| 15 | c.*113C > T | Intronic | p. = | 8 (8.6) | 0 | 93 | rs76661336 |
*Het, heterozygous; Hom, homozygous
†Build 133; NA, not applicable
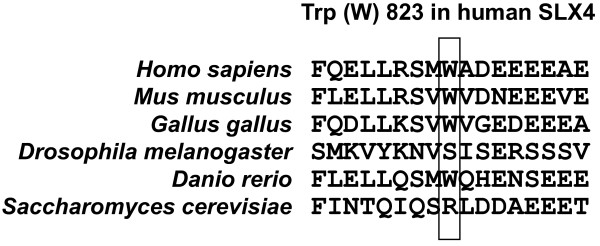
Having identified rare variants in BrCa familial cases, we next assessed the presence of 10 of these variants in a cohort of controls collected at the same hospital as the cases (see Methods). The selection of these variants was based on the observed low frequency in the 94 BrCa cases and on their identification as missense variations. In addition, a causative prediction was obtained using two algorithms (PolyPhen-2 [26] and SIFT [27]), plus a weighted average of scores (Condel [28]). Seven of these variants were not found in controls and, intriguingly, five of them were predicted to be "deleterious" (Table 2). Among this group, only one amino acid position (Trp823) showed some evolutionary conservation (Figure 1), and the substitution may be disfavored (Trp to Cys) [29]; tumor samples were not available for any case that would have allowed assessment of the existence of loss of heterozygosity at the SLX4 locus. Nonetheless, predictions of a deleterious effect should be taken with caution as neutral polymorphisms can frequently be misclassified (from ~15-50% depending on the method [28]). On the other hand, extensive genetic variation in SLX4 might reflect an unknown evolutionary pressure or could be related to a similar observation made for other DNA repair-related genes [30].
Table 2.
Pathological prediction and frequency in controls of selected SLX4 missense variants
| Exon | Nucleotide change |
Amino acid change |
dbSNP† | Pathological prediction | Controls tested (n) |
Number of control carriers (%) |
|||
|---|---|---|---|---|---|---|---|---|---|
| SIFT (score < 0.05, deleterious) |
PolyPhen-2 (false positive rate) |
Condel (weighted average of scores) |
Condel prediction |
||||||
| 2 | c.248G > C | p.Gly83Ala | NA | 0.14 | 0.15 | 0.15 | Neutral | 283 | 0 |
| 2 | c.421G > T | p.Gly141Trp | NA | 0.00 | 0.86 | 0.86 | Deleterious | 284 | 2 (0.7) |
| 3 | c.590T > C | p.Val197Ala | NA | 0.48 | 0.01 | 0.00 | Neutral | 284 | 1 (0.4) |
| 3 | c.710G > A | p.Arg237Gln | NA | 0.49 | 0.00 | 0.38 | Neutral | 284 | 4 (1.4) |
| 8 | c.1846G > A | p.Val616Met | NA | 0.17 | 0.62 | 0.80 | Deleterious | 281 | 0 |
| 12 | c.2469G > C | p.Trp823Cys | NA | 0.01 | 1.00 | 0.97 | Deleterious | 282 | 0 |
| 12 | c.3872C > T | p.Thr1291Met | NA | 0.05 | 0.98 | 0.99 | Deleterious | 283 | 0 |
| 12 | c.4261A > T | p.Ille1421Phe | NA | 0.08 | 0.77 | 0.77 | Deleterious | 285 | 0 |
| 12 | c.4409C > T | p.Pro1470Leu | rs72778139 | 0.02 | 0.99 | 0.96 | Deleterious | 283 | 0 |
| 14 | c.5072A > G | p.Asn1691Ser | NA | 0.56 | 0.00 | 0.01 | Neutral | 285 | 0 |
†Build 133; NA, not applicable
Figure 1.
CLUSTALW-based multi-alignment of human SLX4 and eukaryotic homologs. The region surrounding human Trp823 is shown.
While SLX4 serves as a scaffold for multiple proteins involved in the DNA damage response [16,17], the functional involvement of the Trp823 position, and of the other rare variants not found in controls in this study, is unknown. None of the identified variants changes a critical amino acid residue and there is no data that could suggest an alteration of protein interactions or complexes; however, the Pro1470Leu variant might disrupt a mitotic phosphorylation site at Ser1469 [31,32]. In this context, a SLX4 pathological variant linked to BrCa should consist of a hypomorphic mutation that would cause genome instability. Accordingly, SLX4 is a key regulator of the function of structure-specific endonucleases involved in the repair of DNA damage; in particular, proper function of SLX4 is fundamental for repair during replication and for resolving Holliday junctions formed during homologous recombination [16,17,33,34]. Overall, the results of this study do not support the existence of loss-of-function mutations of SLX4 associated with BrCa risk; nonetheless, further genetic analysis in patients and controls, combined with functional assays of specific rare variants, may be warranted.
Conclusions
The mutational analysis of SLX4 in 94 familial BrCa index cases without mutations in BRCA1 or BRCA2 has revealed extensive genetic variation. Twenty-nine novel single nucleotide variants have been detected, 21 of them showing relatively low allele frequencies: however, none can be linked to a clear alteration of the protein function. Nonetheless, analysis of 10 of these variants failed to detect seven of them in a set of controls. While the results of this study do not support the common existence of SLX4 mutations contributing to BrCa risk, additional studies may be warranted.
Abbreviations
BrCa: Breast cancer; BRCA1/2: Breast cancer 1/2: early onset genes; BRCAPRO: BRCA carrier prediction model; Condel: Consensus deleteriousness score; dbSNP: Single nucleotide polymorphism database; DNA: Deoxyribonucleic acid; FA: Fanconi anemia; Het: Heterozygous; Hom: Homozygous; PolyPhen: Polymorphism phenotyping; SIFT: Sorting intolerant from tolerant; SLX4: Structure-specific endonuclease subunit homolog (S. cerevisiae) gene.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
The project was conceived by DS, CL and MAP. The experiments and data analyses were coordinated by JF-R, CL and MAP. The mutational analysis was performed by JF-R and FQ. The clinical and BRCA1/2 annotations were performed by IB, AT, LF, JV, MS, AI, ED, GC, JB and CL. The selection of index cases was performed by IB. The manuscript was written by MAP. All authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Contributor Information
Juana Fernández-Rodríguez, Email: jfrodriguez@iconcologia.net.
Francisco Quiles, Email: fquiles@iconcologia.net.
Ignacio Blanco, Email: iblanco@iconcologia.net.
Alex Teulé, Email: ateule@iconcologia.net.
Lídia Feliubadaló, Email: lfeliubadalo@iconcologia.net.
Jesús del Valle, Email: jdelvalle@iconcologia.net.
Mónica Salinas, Email: msalinas@iconcologia.net.
Àngel Izquierdo, Email: aizquierdo@iconcologia.net.
Esther Darder, Email: edarder@iconcologia.net.
Detlev Schindler, Email: schindler@biozentrum.uni-wuerzburg.de.
Gabriel Capellá, Email: gcapella@iconcologia.net.
Joan Brunet, Email: jbrunet@iconcologia.net.
Conxi Lázaro, Email: clazaro@iconcologia.net.
Miguel Angel Pujana, Email: mapujana@iconcologia.net.
Acknowledgements
We wish to thank all study participants, clinicians, centers and members of the case-control study at the Catalan Institute of Oncology for their valuable contributions. The authors recognize the following grants provided to support this study: Generalitat de Catalunya 2009SGR290 to IB and CL, and 2009-SGR283 to MAP; Spanish Association Against Cancer (AECC groups) to GC; Spanish Ministry of Health "Instituto de Salud Carlos III" 10/31488, 10/01422, and 09/02483 to IB, CL, and MAP, respectively; 2009 Spanish Society of Medical Oncology to JB; and CIBERESP group 55 and Ramón Areces Foundation XV to MAP. JF-R was supported by a research support contract (CA08/00248) from the "Instituto de Salud Carlos III".
References
- Wang W. Emergence of a DNA-damage response network consisting of Fanconi anaemia and BRCA proteins. Nat Rev Genet. 2007;8:735–748. doi: 10.1038/nrg2159. [DOI] [PubMed] [Google Scholar]
- D'Andrea AD. Susceptibility pathways in Fanconi's anemia and breast cancer. N Engl J Med. 2010;362:1909–1919. doi: 10.1056/NEJMra0809889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howlett NG, Taniguchi T, Olson S, Cox B, Waisfisz Q, De Die-Smulders C, Persky N, Grompe M, Joenje H, Pals G. et al. Biallelic inactivation of BRCA2 in Fanconi anemia. Science. 2002;297:606–609. doi: 10.1126/science.1073834. [DOI] [PubMed] [Google Scholar]
- Wooster R, Bignell G, Lancaster J, Swift S, Seal S, Mangion J, Collins N, Gregory S, Gumbs C, Micklem G. Identification of the breast cancer susceptibility gene BRCA2. Nature. 1995;378:789–792. doi: 10.1038/378789a0. [DOI] [PubMed] [Google Scholar]
- Seal S, Thompson D, Renwick A, Elliott A, Kelly P, Barfoot R, Chagtai T, Jayatilake H, Ahmed M, Spanova K. et al. Truncating mutations in the Fanconi anemia J gene BRIP1 are low-penetrance breast cancer susceptibility alleles. Nat Genet. 2006;38:1239–1241. doi: 10.1038/ng1902. [DOI] [PubMed] [Google Scholar]
- Levran O, Attwooll C, Henry RT, Milton KL, Neveling K, Rio P, Batish SD, Kalb R, Velleuer E, Barral S. et al. The BRCA1-interacting helicase BRIP1 is deficient in Fanconi anemia. Nat Genet. 2005;37:931–933. doi: 10.1038/ng1624. [DOI] [PubMed] [Google Scholar]
- Levitus M, Waisfisz Q, Godthelp BC, de Vries Y, Hussain S, Wiegant WW, Elghalbzouri-Maghrani E, Steltenpool J, Rooimans MA, Pals G. et al. The DNA helicase BRIP1 is defective in Fanconi anemia complementation group J. Nat Genet. 2005;37:934–935. doi: 10.1038/ng1625. [DOI] [PubMed] [Google Scholar]
- Litman R, Peng M, Jin Z, Zhang F, Zhang J, Powell S, Andreassen PR, Cantor SB. BACH1 is critical for homologous recombination and appears to be the Fanconi anemia gene product FANCJ. Cancer Cell. 2005;8:255–265. doi: 10.1016/j.ccr.2005.08.004. [DOI] [PubMed] [Google Scholar]
- Erkko H, Xia B, Nikkila J, Schleutker J, Syrjakoski K, Mannermaa A, Kallioniemi A, Pylkas K, Karppinen SM, Rapakko K. et al. A recurrent mutation in PALB2 in Finnish cancer families. Nature. 2007;446:316–319. doi: 10.1038/nature05609. [DOI] [PubMed] [Google Scholar]
- Reid S, Schindler D, Hanenberg H, Barker K, Hanks S, Kalb R, Neveling K, Kelly P, Seal S, Freund M. et al. Biallelic mutations in PALB2 cause Fanconi anemia subtype FA-N and predispose to childhood cancer. Nat Genet. 2007;39:162–164. doi: 10.1038/ng1947. [DOI] [PubMed] [Google Scholar]
- Rahman N, Seal S, Thompson D, Kelly P, Renwick A, Elliott A, Reid S, Spanova K, Barfoot R, Chagtai T. et al. PALB2, which encodes a BRCA2-interacting protein, is a breast cancer susceptibility gene. Nat Genet. 2007;39:165–167. doi: 10.1038/ng1959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meindl A, Hellebrand H, Wiek C, Erven V, Wappenschmidt B, Niederacher D, Freund M, Lichtner P, Hartmann L, Schaal H. et al. Germline mutations in breast and ovarian cancer pedigrees establish RAD51C as a human cancer susceptibility gene. Nat Genet. 2010;42:410–414. doi: 10.1038/ng.569. [DOI] [PubMed] [Google Scholar]
- Vaz F, Hanenberg H, Schuster B, Barker K, Wiek C, Erven V, Neveling K, Endt D, Kesterton I, Autore F. et al. Mutation of the RAD51C gene in a Fanconi anemia-like disorder. Nat Genet. 2010;42:406–409. doi: 10.1038/ng.570. [DOI] [PubMed] [Google Scholar]
- Pelttari LM, Heikkinen T, Thompson D, Kallioniemi A, Schleutker J, Holli K, Blomqvist C, Aittomaki K, Butzow R, Nevanlinna H. RAD51C is a susceptibility gene for ovarian cancer. Hum Mol Genet. 2011;20:3278–3288. doi: 10.1093/hmg/ddr229. [DOI] [PubMed] [Google Scholar]
- Roberts TM, Kobor MS, Bastin-Shanower SA, Ii M, Horte SA, Gin JW, Emili A, Rine J, Brill SJ, Brown GW. Slx4 regulates DNA damage checkpoint-dependent phosphorylation of the BRCT domain protein Rtt107/Esc4. Mol Biol Cell. 2006;17:539–548. doi: 10.1091/mbc.E05-08-0785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Svendsen JM, Smogorzewska A, Sowa ME, O'Connell BC, Gygi SP, Elledge SJ, Harper JW. Mammalian BTBD12/SLX4 assembles a Holliday junction resolvase and is required for DNA repair. Cell. 2009;138:63–77. doi: 10.1016/j.cell.2009.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fekairi S, Scaglione S, Chahwan C, Taylor ER, Tissier A, Coulon S, Dong MQ, Ruse C, Yates JR, Russell P. et al. Human SLX4 is a Holliday junction resolvase subunit that binds multiple DNA repair/recombination endonucleases. Cell. 2009;138:78–89. doi: 10.1016/j.cell.2009.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoepker C, Hain K, Schuster B, Hilhorst-Hofstee Y, Rooimans MA, Steltenpool J, Oostra AB, Eirich K, Korthof ET, Nieuwint AW. et al. SLX4, a coordinator of structure-specific endonucleases, is mutated in a new Fanconi anemia subtype. Nat Genet. 2011;43:138–141. doi: 10.1038/ng.751. [DOI] [PubMed] [Google Scholar]
- Kim Y, Lach FP, Desetty R, Hanenberg H, Auerbach AD, Smogorzewska A. Mutations of the SLX4 gene in Fanconi anemia. Nat Genet. 2011;43:142–146. doi: 10.1038/ng.750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landwehr R, Bogdanova NV, Antonenkova N, Meyer A, Bremer M, Park-Simon TW, Hillemanns P, Karstens JH, Schindler D, Dork T. Mutation analysis of the SLX4/FANCP gene in hereditary breast cancer. Breast Cancer Res Treat. 2011;130:1021–1028. doi: 10.1007/s10549-011-1681-1. [DOI] [PubMed] [Google Scholar]
- Euhus DM, Smith KC, Robinson L, Stucky A, Olopade OI, Cummings S, Garber JE, Chittenden A, Mills GB, Rieger P. et al. Pretest prediction of BRCA1 or BRCA2 mutation by risk counselors and the computer model BRCAPRO. J Natl Cancer Inst. 2002;94:844–851. doi: 10.1093/jnci/94.11.844. [DOI] [PubMed] [Google Scholar]
- Landi S, Moreno V, Gioia-Patricola L, Guino E, Navarro M, de Oca J, Capella G, Canzian F. Association of common polymorphisms in inflammatory genes interleukin (IL) 6, IL8, tumor necrosis factor alpha, NFKB1, and peroxisome proliferator-activated receptor gamma with colorectal cancer. Cancer Res. 2003;63:3560–3566. [PubMed] [Google Scholar]
- Sherry ST, Ward MH, Kholodov M, Baker J, Phan L, Smigielski EM, Sirotkin K. dbSNP: the NCBI database of genetic variation. Nucleic Acids Res. 2001;29:308–311. doi: 10.1093/nar/29.1.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Consortium GP. A map of human genome variation from population-scale sequencing. Nature. 2010;467:1061–1073. doi: 10.1038/nature09534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reese MG, Eeckman FH, Kulp D, Haussler D. Improved splice site detection in Genie. J Comput Biol. 1997;4:311–323. doi: 10.1089/cmb.1997.4.311. [DOI] [PubMed] [Google Scholar]
- Adzhubei IA, Schmidt S, Peshkin L, Ramensky VE, Gerasimova A, Bork P, Kondrashov AS, Sunyaev SR. A method and server for predicting damaging missense mutations. Nat Methods. 2010;7:248–249. doi: 10.1038/nmeth0410-248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar P, Henikoff S, Ng PC. Predicting the effects of coding non-synonymous variants on protein function using the SIFT algorithm. Nat Protoc. 2009;4:1073–1081. doi: 10.1038/nprot.2009.86. [DOI] [PubMed] [Google Scholar]
- González-Pérez A, Lopez-Bigas N. Improving the assessment of the outcome of nonsynonymous SNVs with a consensus deleteriousness score, Condel. Am J Hum Genet. 2011;88:440–449. doi: 10.1016/j.ajhg.2011.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betts MJ, Russell RB. In: Bioinformatics for Geneticists. Barnes MR, Gray IC, editor. Chichester: John Wiley and Sons; 2003. Amino acid properties and consequences of subsitutions; pp. 289–316. [Google Scholar]
- Mohrenweiser HW, Wilson DM, Jones IM. Challenges and complexities in estimating both the functional impact and the disease risk associated with the extensive genetic variation in human DNA repair genes. Mutat Res. 2003;526:93–125. doi: 10.1016/S0027-5107(03)00049-6. [DOI] [PubMed] [Google Scholar]
- Cantin GT, Yi W, Lu B, Park SK, Xu T, Lee JD, Yates JR. Combining protein-based IMAC, peptide-based IMAC, and MudPIT for efficient phosphoproteomic analysis. J Proteome Res. 2008;7:1346–1351. doi: 10.1021/pr0705441. [DOI] [PubMed] [Google Scholar]
- Dephoure N, Zhou C, Villen J, Beausoleil SA, Bakalarski CE, Elledge SJ, Gygi SP. A quantitative atlas of mitotic phosphorylation. Proc Natl Acad Sci USA. 2008;105:10762–10767. doi: 10.1073/pnas.0805139105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crossan GP, van der Weyden L, Rosado IV, Langevin F, Gaillard PH, McIntyre RE, Gallagher F, Kettunen MI, Lewis DY, Brindle K. et al. Disruption of mouse Slx4, a regulator of structure-specific nucleases, phenocopies Fanconi anemia. Nat Genet. 2011;43:147–152. doi: 10.1038/ng.752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler T, Newman S, West SC. Aberrant chromosome morphology in human cells defective for Holliday junction resolution. Nature. 2011;471:642–646. doi: 10.1038/nature09790. [DOI] [PMC free article] [PubMed] [Google Scholar]