Abstract
Extensive work has documented an association between sustaining intimate partner violence (IPV) and alcohol/drug abuse among women, yet little research has documented the same association in men, even though men comprise 25%–50% of all IPV victims in a given year. The present study investigates the associations among sustaining IPV and alcohol/drug abuse among both a clinical and community sample of men. The clinical sample is comprised of 302 men who sustained intimate terrorism -- a form of IPV that is characterized by much violence and controlling behavior -- from their female partners and sought help. The community sample is comprised of 520 men, 16% of whom sustained common couple violence, a lower level of more minor, reciprocal IPV. Analyses showed that among both groups of men who sustained IPV, the prevalence and frequency of alcohol/drug abuse was significantly higher than in men who did not sustain IPV. However, a dose-response relationship between sustaining IPV and alcohol/drug abuse was found only among men in the community sample. Path modeling showed that for the community sample, the best fitting models were ones that showed that the alcohol/drug abuse predicted IPV victimization, an association that was fully mediated by their use of IPV.
Keywords: domestic violence, male victims, intimate terrorism, alcohol abuse, drug abuse
A significant association between alcohol/drug abuse and women sustaining intimate partner violence (IPV) has been well-documented (Amaro, Fried, Cabral, & Zuckerman, 1990; Kantor & Asdigian, 1997; Salomon, Bassuk, & Huntington, 2002; Stark & Flitcraft, 1988; Stith, Smith, Penn, Ward, & Tritt, 2004), yet little research has documented whether there is an association between alcohol/drug abuse and men sustaining IPV. To our knowledge, only a handful studies have investigated this association, with no focus on men who report sustaining more severe types of IPV. For example, Halford and Osgarby (1993) investigated, among other issues, the association between female partners’ violence and men’s alcohol abuse among 56 men seeking marital therapy in Australia. Although they found no association, their sample size was small, had limited generalizability, and did not investigate the abuse of other substances. Among male college students, Simons, Gwin, Brown, and Gross (2008) found that IPV victimization was associated with higher rates of both alcohol and drug use, but this study also has limited generalizability and does not test possible mediators of this association. More research among men who sustain IPV is warranted, especially given that between 25% and 50% of people who sustain IPV in a given year are men (Archer, 2000; Catalano, 2007; Murray A. Straus, 1995; Tjaden, 2000) and men are more likely than women to abuse alcohol or other substances in response to a stressful event (Cooper, Russell, Skinner, Frone, & Mudar, 1992). We propose to address these limitations in this paper.
Theoretical Models Explaining Associations Among IPV and Alcohol/Drug Abuse
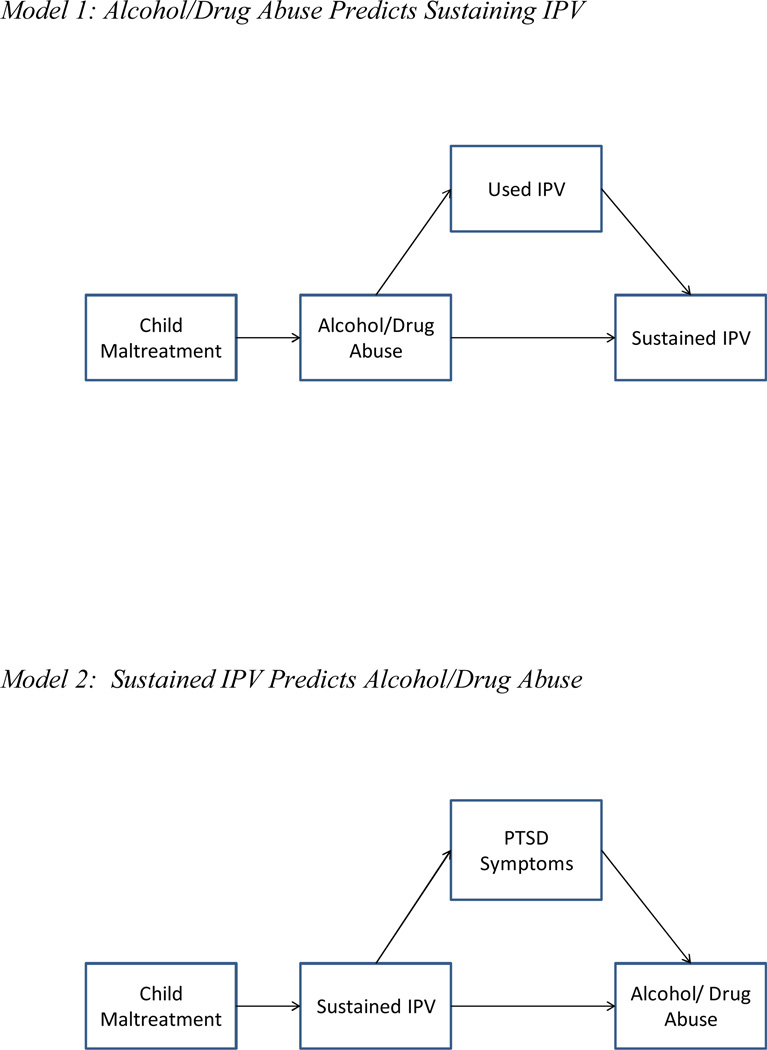
In the current study, we investigated whether there was an association between alcohol/substance abuse and sustaining IPV among two samples of men: a community sample and those who sustained IPV from their female partner and sought help. We then investigated possible reasons for any association. Specifically, if alcohol/substance abuse is related to sustaining IPV in men, previous research on female IPV victims suggests at least two possibilities for explaining that relationship (Kilpatrick, Acierno, Resnick, Saunders, & Best, 1997):
Alcohol/drug abuse is a risk factor for sustaining IPV (Kilpatrick, et al., 1997). This possibility is thought to be related to one’s lifestyle, such that alcohol/drug abuse leads one into certain situations or relationships in which sustaining IPV is more likely. Another explanation is that alcohol/drug abuse can lead to certain behaviors that increase the likelihood of sustaining IPV, and one such behavior could be IPV perpetration. It has been well-documented that both alcohol and drug abuse are risk factors for men using IPV against their female partners (Fals-Stewart, 2003; Fals-Stewart, Leonard, & Birchler, 2005; Leonard, 1993; Murphy, O'Farrell, Fals-Stewart, & Feehan, 2001; O'Farrell, Fals-Stewart, Murphy, & Murphy, 2003), and the strongest risk for sustaining IPV is perpetrating IPV (Kessler, Molnar, Feurer, & Appelbaum, 2001; Stets & Straus, 1990). Thus, IPV perpetration can be a mediator for the relationship between alcohol/drug abuse and sustaining IPV.
Sustaining IPV is a risk factor for alcohol/drug abuse (Kilpatrick, et al., 1997). This association is typically thought to be related to the overwhelmingly negative emotions or post-traumatic stress symptoms that someone who experiences a traumatic event, like IPV, would experience. In an effort to cope with and reduce these emotions, the person might use alcohol or other drugs (Jacobsen, Southwick, & Kosten, 2001; J. S. Simons, Gaher, Jacobs, Meyer, & Johnson-Jimenez, 2005; Stewart, 1996). In fact, post-traumatic stress disorder (PTSD) and alcohol/drug abuse are highly comorbid disorders that are functionally related (Chilcoat & Breslau, 1998; Jacobsen, et al., 2001; Stewart, 1996; Stewart, Pihl, Conrod, & Dongier, 1998), and the model with the most support to explain this association is the self-medication model (Chilcoat & Breslau, 1998; Jacobsen, et al., 2001; Stewart, 1996; Stewart, et al., 1998). In this model, alcohol and other drugs seem to provide acute symptom relief of PTSD: In particular, they seem to lessen the hyperarousal components and facilitate the forgetting of traumatic memories through their effects on the central nervous system (Chilcoat & Breslau, 1998; Jacobsen, et al., 2001; Stewart, 1996; Stewart, Conrod, Pihl, & Dongier, 1999; Stewart, et al., 1998). In other words, alcohol and other drugs seem to be used in an effort to self-medicate for the distressing symptoms of PTSD (Chilcoat & Breslau, 1998). Thus, PTSD symptoms may serve as a mediator for any association between sustaining IPV and alcohol/drug abuse.
In addition, it is well-documented that sustaining physical abuse or witnessing interparental violence during childhood can put one at risk for abusing alcohol or other drugs (e.g., Liebschutz et al., 2002) and for sustaining IPV (e.g., Stith et al., 2000). Thus, any model investigating the associations among IPV and alcohol/drug abuse should consider any potential trauma of previous childhood abuse.
Previous longitudinal research among female victims of IPV and assault in general provide some support for the hypothesized models (Kilpatrick, et al., 1997; Martino, Collins, & Ellickson, 2005; Salomon, et al., 2002; Testa, Livingston, & Leonard, 2003), yet there are some caveats. For example, in a longitudinal, population-based sample of women, drug abuse, but not alcohol abuse, may put one at risk for sustaining any kind of assault; and sustaining an assault puts one at risk for both alcohol and drug abuse, a relationship that is particularly strong for alcohol abuse (Kilpatrick, et al., 1997). In a multi-year panel study of women living with a male partner, drug use did not predict subsequent IPV nor did IPV predict subsequent drug use, but IPV did predict later heavy drinking (Martino, et al., 2005). In a longitudinal, random-digit dial phone survey of Buffalo-area women, drug abuse predicted subsequent IPV victimization, and although alcohol abuse did not predict subsequent victimization, IPV victimization did predict alcohol abuse (Testa, et al., 2003). Among poor women in a longitudinal study, sustaining IPV put one at risk for abusing drugs, but not alcohol; sustaining child abuse also contributed to drug abuse, PTSD was only a weak mediator of the association between sustaining IPV and drug abuse; and there was no support for a model positing that alcohol/drug abuse put one at risk for sustaining IPV (Salomon, et al., 2002).
Overall, there is support for IPV victimization predicting subsequent alcohol abuse, some support for IPV victimization predicting drug abuse, some support for drug abuse predicting subsequent IPV victimization, and no support for alcohol abuse predicting IPV victimization. In addition, there is support for child abuse as a contributor to drug abuse and PTSD as a possible mediator. Given these caveats, it is important to test models separately for alcohol abuse and drug abuse.
Although there is little research on the association between alcohol/drug abuse and IPV victimization among men, studies mentioned previously suggest that such as association exists (L. Simons, et al., 2008). Moreover, there are studies investigating whether alcohol/drug abuse is linked with violent victimization in general among males. For example, in adolescent males, problem alcohol use is a risk factor for subsequent violent victimization as assessed with longitudinal data (Thompson, Sims, Kingree, & Windle, 2008), and cross-sectional studies show that experiencing a physical or sexual assault either within the home or in general is associated with subsequent drug abuse and that PTSD increases the risk of drug abuse (Kilpatrick et al., 2000). In addition, among male college students, sustaining a sexual assault is associated with a subsequent increased risk of using alcohol or drugs (Amos et al., 2008). Given these findings, it is important to further investigate these associations among men who sustain IPV.
Intimate Terrorism versus Common Couple Violence
In addition to studying these associations among men who sustain IPV, it is also important to investigate whether these associations may differ among men who represent two different types of IPV: intimate terrorism (IT) and common couple violence (CCV). According to Johnson (Johnson, 1995, 2006; Johnson & Ferraro, 2000), IT is a type of IPV that is characterized by frequent and severe physical IPV and controlling behaviors, and has traditionally be used to describe and is consistent with samples of battered women seeking shelter. He labeled the IPV found in community and population-based samples CCV, which is characterized by low-level (e.g., slapping, pushing), low-frequency violence in a couple where both members are about equally violent; this IPV is not part of an overall pattern of control of one partner over the other, but is the result of a conflict “getting out of hand.”
The current study utilizes both “helpseeking” and “community” samples of men with regard to IPV. The helpseeking sample is comprised of men who sustained IPV from their female partners and sought help of some sort; the community sample is comprised of a convenience sample of men recruited from the community to participate in a study on how men and women get along. In a previous analysis that focused on describing the IPV in these two samples (Hines & Douglas, 2010), we found that the helpseeking sample conformed to Johnson’s (1995, 2006; Johnson & Ferraro, 2000) definition of IT; the frequency of physical IPV the men sustained was comparable to the frequency with which shelter samples of battered women sustained physical IPV (Giles-Sims, 1983; Johnson, 2006; McDonald, Jouriles, Tart, & Minze, 2009; Okun, 1986; M. A. Straus, 1990); the physical assaults were accompanied by high levels of controlling behaviors, severe psychological aggression, and physical injuries. Moreover, the overwhelming majority of the physical arguments were reportedly initiated by the female partner (Hines & Douglas, 2010).
On the other hand, the 16% of the men in our community sample who sustained physical IPV conformed to Johnson’s (1995, 2006; Johnson & Ferraro, 2000) conceptualization of common couple violence (CCV). These men reported that they and their female partners used low-level, low-frequency IPV at approximately the same rates, with an equal likelihood that either the man or his female partner hit first, and the aggression did not involve frequent and severe physical IPV or controlling behaviors (Hines & Douglas, 2010).
Johnson (1995) argues that such helpseeking and community samples are functionally different and should therefore have different patterns of predictors and consequences of IPV. For example, he would argue that the conceptual models outlined above would be different between the community and helpseeking samples of men. Therefore, although we will test the above models on both samples, we hypothesize that they will operate differently between them. Moreover, Johnson would argue that any potential consequences of IPV, such as alcohol/drug abuse, would be more severe among men in helpseeking samples versus men in community samples, because their experiences of IPV are much more severe and thus, more traumatic. Therefore, in the current study, we hypothesized that in comparison to men in the community sample who sustained either CCV or no violence, alcohol/drug abuse would be more severe among the men who sustained IT (i.e., the helpseeking sample). Previous analyses of these datasets did not focus on the associations between alcohol/drug abuse and the IPV these men experienced.
Method
Participants and Procedure
Two separate samples of male participants were recruited for this study: a helpseeking sample and a community sample. For both samples, the men had to speak English, live in the U.S., and be between the ages of 18 and 59 to be eligible; they also had to have been involved in an intimate relationship with a woman lasting at least one month in the previous year. In addition, to be eligible for the helpseeking sample, the men had to have sustained a physical assault from their female partner within the previous year, and they had to have sought help/assistance for their partner’s violence. Help/assistance was broadly defined and included seeking help from formal sources such as hotlines, domestic violence agencies, the police, mental health and medical health professionals, lawyers, and ministers, to more informal helpseeking efforts, such as talking with friends and family members and searching the Internet for information on IPV or support groups for IPV victims in general or male IPV victims specifically.
The helpseeking sample of men (n = 302) was recruited from a variety of sources, including the Domestic Abuse Helpline for Men and Women (DAHMW; a U.S. national hotline specializing in male victims of domestic violence), and online websites, newsletters, blogs, and listservs that specialized in treatment of IPV, male victims of IPV, fathers’ rights issues, divorced men’s issues, men’s health issues, and men’s rights issues. Men who called the DAHMW seeking assistance and who met the eligibility criteria were invited to participate in this study either by calling a survey research center to complete the interview over the phone or by visiting the study website to complete an anonymous, secure version of the study questionnaire online. Men who saw an advertisement for the study online were directed to the study website to complete the online version of the study. Screener questions regarding the study criteria were on the first page of the survey, and men who were eligible, given the stated criteria for the helpseeking sample, were allowed to continue the survey. Men who did not meet the eligibility requirements were thanked for their time and were redirected to an “exit page” of the survey. Sixteen men completed the interview over the phone; the remaining 286 completed it online. Demographics of the helpseeking sample can be found in Table 1.
Table 1.
Demographics, Intimate Partner Violence Sustained, PTSD, and Childhood Aggression Experiences
| Helpseeking Sample (n = 302) |
Community Sample (n = 520) |
||
|---|---|---|---|
| % or M (SD) | % or M (SD) | χ2 or t | |
| Demographics | |||
| Age (in years) | 40.49 (8.97) | 43.68 (10.88) | 4.52*** |
| Education‡ | 4.40 (1.56) (n = 300) |
4.04 (1.72) (n = 514) |
3.13** |
| Income (in thousands) | $50.44K (25.69) (n = 296) |
$48.98K (26.13) (n = 508) |
0.77 |
| % White | 86.8 | 84.8 | 0.59 |
| % currently in a relationship | 56.3% | 95.8% | 193.70*** |
| % with minor children | 73.2% | 45.3% | 64.60*** |
| Length of relationship (in months) | 97.90 (82.06) | 164.90 (131.01) | 8.93*** |
| % Sustaining IPV | |||
| % Sustaining Controlling Behaviors | 93.4 | 20.0 | 412.20*** |
| % Sustaining Severe Psychological Aggression | 96.0 | 13.7 | 526.31*** |
| % Sustaining Physical Aggression | 100.0 | 16.3 | 536.60*** |
| % Sustaining Injury in previous year | 78.5 | 4.0 | 491.56*** |
| Mean # of Acts of IPV Sustained Among Those Sustaining IPV | |||
| # of Controlling Acts in previous year | 42.62 (36.25) (n = 282) |
11.36 (16.31) (n = 104) |
11.64*** |
| # of Severe Psychological Aggression Acts in previous year | 28.90 (26.20) (n = 290) |
9.13 (13.26) (n = 71) |
8.98*** |
| # of Physically Aggressive Acts in previous year | 46.72 (53.48) (n = 302) |
12.22 (33.29) (n = 85) |
7.27*** |
| # of Injuries sustained in previous year | 11.68 (15.61) (n = 237) |
5.52 (11.42) (n = 21) |
2.29* |
| % Using IPV | |||
| % Using Controlling Behaviors | 45.7 | 11.5 | 121.90*** |
| % Using Severe Psychological Aggression | 40.1 | 10.4 | 100.44*** |
| % Using Physical Aggression | 55.0 | 13.8 | 159.19*** |
| % Using Injury in previous year | 26.2 | 4.6 | 80.90*** |
| Mean # of Acts of IPV Used Among Those Using IPV | |||
| # of Controlling Acts in previous year | 7.20 (8.99) (n = 138) |
12.29 (16.99) (n = 60) |
2.19* |
| # of Severe Psychological Aggression Acts in previous year | 5.74 (8.59) (n = 121) |
6.07 (14.49) (n = 54) |
0.19 |
| # of Physically Aggressive Acts in previous year | 7.71 (14.25) (n = 166) |
8.68 (24.21) (n = 72) |
0.40 |
| # of Injuries partner sustained in previous year | 5.19 (6.40) (n = 79) |
6.96 (12.01) (n = 24) |
0.69 |
| Levels of PTSD Symptoms and Childhood Aggression Experienced | |||
| PCL Score | 46.56 (14.22) | 20.43 (8.28) | 29.19*** |
| % sustaining child physical aggression | 46.8 | 35.3 | 10.65*** |
| % witnessing IPV between parents | 21.5 | 14.3 | 7.03** |
Educational Status: 1 = Less than high school, 2 = High school graduate or GED, 3 = Some college/trade school, 4 = Two-year college graduate, 5 = Four-year college graduate, 6 = Some graduate school, 7 = Graduate degree.
p < .01,
p < .001.
Participants also included 520 men from the community. Approximately half of the community sample (n = 255) was recruited to participate in a phone version of the survey by a survey research center, using a random digit dialing technique and CATI administration. The interviewers attempted to reach each phone number on 15 different days, at different times of the day, and made call-back appointments whenever possible. They also made refusal conversion efforts when appropriate. Because of low response rates (8%) during the first two months, advanced letters were sent to potential participants informing them that they were randomly selected to participate in a study sponsored by the National Institutes of Health that was focusing on how men and women get along and that they would be contacted within a week by a survey research center interviewer. The response rate for the participants who received an advanced letter was 15.5%. The overall response rate was 9.8%. The other half of the community sample (n = 265) was recruited through a panel of survey participants maintained by Survey Sampling, Inc. (SSI), to complete an online version of the same survey. Email invitations were sent to 16,000 male SSI panel members inviting them to participate in a study on how men and women get along. They were directed to an anonymous, secure, online version of the survey. The first page of the survey included screener questions testing for eligibility (i.e., between 18 and 59 years of age; in an intimate relationship with a woman lasting at least one month in the previous year). Eligible men were able to continue to the survey, whereas non-eligible men were thanked for their time. The survey was closed after we met our target sample size of 265 men. Because data collection was ceased when the target goal for the number of completed surveys was reached and we did not wait for all men who received invitations to complete the survey, response rates for the Internet sample cannot be reliably calculated. Demographic information on the full community sample (n = 520) can be found in Table 1. Multivariate analyses indicated that the only differences between the phone and online community samples were that men in the phone sample had more social support, were less likely to score above a clinical cut-off for PTSD symptoms, and were more likely to have ever used drugs. There were no differences in IPV victimization or perpetration. Further information on the phone and online community samples that is beyond the scope of the current analysis can be found in Hines, Douglas, and Mahmood (2010).
The methods for this study were approved by the boards of ethics at the participating institutions. All of the men participated anonymously, were apprised of their rights as study participants, and gave their consent to participate before beginning the survey. Steps were taken to ensure their safety: At the completion of the survey, the participants were given information about obtaining help for IPV victimization and how to delete the history on their Internet web browser.
Measures
Both the helpseeking and community samples were given the same core questionnaires regarding demographics, aggressive behaviors that they and their female partners may have used in the previous year, more detailed information regarding their last physical argument (if applicable), their mental health, and various risk factors. The helpseeking sample was given additional questions pertaining to their specific helpseeking experiences in an aggressive relationship and what prevents them from leaving the relationship. Only the questionnaires used in the current analyses will be described below.
Demographic information
Men were asked basic demographic information about both themselves and their partners, including age, race/ethnicity, personal income, education, and occupation. Men were also asked about the current status of their relationship, the length of their relationship with their partners, how long ago the relationship ended (if applicable), and how many minor children were involved in that relationship, if any.
Revised Conflict Tactics Scales (CTS2)
The CTS2 (Murray A. Straus, Hamby, Boney-McCoy, & Sugarman, 1996) was used to measure the extent to which the men in the study sustained psychological, physical, and sexual aggression, and injuries in their relationships. The items used for this study included 5 items assessing minor physical aggression (e.g., grabbing, shoving, slapping) and 7 items assessing severe physical aggression (e.g., beating up, using knife/gun) that were combined into a total physical aggression scale; and 6 items assessing injuries (e.g., having a small cut or bruise, broken bone, passing out). The eight CTS2 items regarding psychological aggression were supplemented with seven items from the Psychological Maltreatment of Women Inventory (Tolman, 1995). To investigate the factor structure of this combined psychological aggression scale, a factor analysis that combined the two samples was conducted using the victimization items (see Hines & Douglas, 2010, for further details on this analysis). The factor analysis revealed that there were three subscales: Minor Psychological Aggression (e.g., insulting/swearing, shouting/yelling, doing something to spite partner), Controlling Behaviors (e.g., not allowing to leave the house, monitoring time and whereabouts), and Severe Psychological Aggression (e.g., threatening to harm partner, intentionally destroying something belonging to partner). For the current study, only the controlling behaviors and severe psychological aggression scales were used because they theoretically differentiate IT from CCV (Johnson, 1995).
Participants responded to items depicting each of the conflict tactics by indicating the number of times these tactics were used by the participant and his partner in the previous year. Participants indicated on a scale from 0 to 6 how many times they experienced each of the acts in the previous year, 0 = 0 times; 1 = 1 time; 2 = 2 times; 3 = 3–5 times; 4 = 6–10 times; 5 = 11–20 times; 6 = more than 20 times. These data were then transformed in order to obtain an approximate count of the number of times each act occurred in the previous year, using the following scale: 0 = 0 acts in previous year; 1 = 1 act in the previous year; 2 = 2 acts in the previous year; 3 = 4 acts in the previous year; 4 = 8 acts in the previous year; 5 = 16 acts in the previous year; 6 = 25 acts in the previous year.
The CTS2 has been shown to have good construct and discriminant validity and good reliability, with internal consistency coefficients ranging from .79 to .95 (Murray A. Straus, et al., 1996). Reliability statistics for the current samples were .82 for both the Controlling Behaviors and Severe Psychological Aggression scales, .92 for the Physical Aggression scale, and .68 for the Injury scale.
Abusive Childhood Experiences of the Participant
Childhood abusive experiences were assessed using 2 questions that condensed the 8 items from the Violence Socialization (VS) scale of the Personal and Relationships Profile (Murray A. Straus, Hamby, Boney-McCoy, & Sugarman, 1999). Participants indicated the extent to which they agreed or disagreed (1=strongly disagree, 4=strongly agree) with each statement: “When I was less than 12 years old, I was spanked or hit a lot by my mother or father” (sustaining child physical aggression), and “When I was a kid, I saw my mother or father kick, punch, or beat up their partner” (witnessed interparental IPV). Reports of the psychometric properties of the full VS scale indicates adequate validity and an overall alpha of .73 (Murray A. Straus & Mouradian, 1999).
Posttraumatic Stress Symptoms
The PTSD Checklist (PCL) (Weathers, Litz, Herman, Huska, & Keane, 1993) is a 17-item self-report measure of the severity of PTSD symptomology. Items reflect three symptom clusters: re-experiencing, numbing/avoidance, and hyperarousal. Consistent with the concept of PTSD and per the instructions of the PCL, questions were anchored to one potentially traumatic event: Participants were asked to think about their worst argument with their female partner, and then indicate the extent to which they were bothered by each symptom in the preceding month using a 5-point scale (1 = not at all, 5 = extremely). The items were then summed to create a continuous measure of PTSD symptoms. One item, “Feeling as if your future will somehow be cut short”, was not included in the survey because participants reported that they did not understand the item during pilot testing of the instrument. The PCL has been validated for use in both combat and civilian populations, and the civilian version was used for this study. The PCL has been shown to have excellent reliability (Weathers, et al., 1993) and strong convergent and divergent validity (Blanchard, Jones-Alexander, Buckley, & Forneris, 1996; Ruggiero, DelBen, Scotti, & Rabalais, 2003). For the current samples, the alpha was .97.
Alcohol and Drug Abuse
Alcohol and drug abuse were measured using a scale developed for the National Women’s Study to assess the association between IPV victimization and alcohol/drug abuse among female victims (Kilpatrick, et al., 1997). The scale included up to 19 items asking respondents about their use and abuse of alcohol and illicit drugs (i.e., marijuana, cocaine, methamphetamines, crack, LSD, heroin, or other such drug) in their lifetimes and in the past year, and included items regarding negative experiences resulting from alcohol abuse. Consistent with Kilpatrick et al.’s (1997) guidelines for scoring this scale, we measured alcohol abuse within the past year by two indicators that approximated the diagnostic criteria for the Diagnostic and Statistical Manual of Mental Disorders IV (American Psychiatric Association, 1994): (1) Participants who answered affirmatively to any of the six questions on negative experiences (e.g., getting in trouble with the police or a boss) within the past year because of alcohol were classified as meeting the criteria for alcohol abuse in the past year, and (2) Frequency of intoxication within the past year: Participants were asked to indicate how frequently they were intoxicated in the past year on a scale from 0 = never to 7 = every day/almost every day.
Similarly, according to the guidelines established by Kilpatrick et al. (1997), drug abuse was measured by two indicators that approximate the frequency of usage considered significant by the Diagnostic Interview Schedule substance abuse screen (Robins, Helzer, Cottler, & Goldring, 1988): (1) If participants indicated they used any illegal drugs more than 4 times in the past year, they were considered nonexperimental users/drug abusers, and (2) Actual frequency of drug use within the past year from 0 = never to 3 = more than 10 occasions. This scale has demonstrated excellent construct validity (Kilpatrick, et al., 1997).
Results
Table 1 presents the demographics of the helpseeking and community samples, and descriptive information for all predictor, mediator, and outcome variables. A full discussion of these samples can be found in previous analyses of this dataset (e.g. Hines & Douglas, 2010).
Hypothesis 1: Differences in Proposed Conceptual Models
Bivariate Correlations Among IPV and Alcohol/Drug Abuse
To test Hypothesis 1, we first performed a series of correlational analyses on the alcohol/drug abuse and IPV variables (Table 2). For each sample separately, we correlated the frequency with which the participants sustained all four forms of IPV with the four alcohol/drug abuse variables: alcohol abuse in past year, frequency of intoxication in past year, drug abuse in past year, and frequency of drug use in past year. As shown, there was only one significant association for the helpseeking sample, and it was in the opposite direction hypothesized. For the community sample, all but two of the associations were significant. The results indicate that there is a dose-response relationship between alcohol/drug abuse and sustaining IPV for the community sample, but not the helpseeking sample.
Table 2.
Bivariate Correlations Among Sustained IPV and Alcohol/Drug Abuse for Both Samples
| Helpseeking Sample (n = 302) | Community Sample (n = 520) | |||||||
|---|---|---|---|---|---|---|---|---|
| Controlling Behaviors |
Severe Psychological Aggression |
Physical Aggression |
Injuries | Controlling Behaviors |
Severe Psychological Aggression |
Physical Aggression |
Injuries | |
| Alcohol Use/Abuse | ||||||||
| Abused Alcohol in Past Year | .08 | −.03 | −.05 | −.04 | .18*** | .14*** | .16*** | .12** |
| Freq of Intoxication in Past Year | .00 | −.08 | .02 | .04 | .11* | .12** | .24*** | .18*** |
| Drug Use/Abuse | ||||||||
| Abused Drugs in Past Year | .01 | −.11 | −.06 | −.02 | .21*** | .13** | .13** | .01 |
| Freq of Drug Use in Past Year | .00 | −.12* | −.05 | −.05 | .25*** | .17*** | .18*** | .07 |
p < .05,
p < .01,
p < .001.
Path Models
Because only the community sample showed associations among alcohol/drug abuse and sustaining IPV, we then investigated the hypothesized path models for the community sample only (Figure 1).i In the interest of parsimony, we combined the scores on the two childhood physical aggression measures (sustaining child physical aggression and witnessing interparental IPV) into a variable called Child Maltreatment. For sustaining IPV, we only used the frequency with which they sustained physical aggression because CCV, the type of IPV that occurs among a minority of couples in a community sample, is not theoretically tied to controlling behaviors and severe psychological aggression (1995, 2006; Johnson & Ferraro, 2000). Finally, for the alcohol and drug abuse variables, we used the frequency of intoxication and frequency of drug use in the past year variables, respectively, to have continuous outcome measures for our path modeling.
Figure 1.
Hypothesized Path Models for the Associations Between Alcohol/Drug Abuse and Sustaining IPV Among Community Sample Only
As indicated, in the first model, we hypothesized that child maltreatment would predict alcohol/drug abuse, which would then predict sustaining IPV in adulthood; this latter association would be partially mediated by the use of IPV. In the second model, we predicted that child maltreatment would predict sustaining IPV, which would then predict alcohol/substance abuse, and this latter association would be partially mediated by levels of PTSD symptoms. These full models were tested for alcohol and drug abuse separately, and each model was evaluated using four fit measures – chi-square, RMSEA, NFI, and GFI – as recommended by Tabachnick and Fidell (2006). This method ensures a model fit is tested from several different perspectives (Meyers, Gamst, & Guarino, 2006). Non-significant paths were pruned one at a time until an excellent-fitting model was achieved. This end model was compared with the original model on their AIC and ECVI; smaller AIC values represent better-fitting models, and smaller ECVI values represent the greatest potential for replication (Byrne, 2010).
Within the community sample, five cases (0.1%) were removed because of incomplete data on the child maltreatment measures. For the frequency of drug usage variable, two cases (0.4%) were missing and replaced with the mean on that variable. For the frequency of intoxication variable, seven cases (1.4%) were missing and replaced with the mean on that variable. For physical aggression used, there was one extreme outlier that was replaced with a value that was one act higher than the next closest value, as per Tabachnick and Fidell (2006). Similarly, for physical aggression sustained, there were two extreme outliers that were replaced with values that were one and two acts higher than the next closest value. Models were tested both with and without the outliers replaced, and there were some slight differences in the path estimates (but no differences in model fits or significance of path estimates); therefore, the results for the models with the outliers replaced are presented.
Initially, the full model for each analysis was evaluated for its adherence to the assumption of multivariate normality. Mardia’s (1970, 1974) normalized estimate of multivariate kurtosis equaled 258.39 for the model where alcohol abuse predicted IPV victimization, 98.89 for the model where IPV victimization predicted alcohol abuse, 271.65 for the model where drug abuse predicted IPV victimization, and 109.18 for the model where IPV victimization predicted drug abuse. All of these values are well above the standard cut-off of 5 and indicated nonnormal distributions (Bentler, 2005). Therefore, we employed the bootstrapping procedure for estimating standard errors and reducing bias in our estimates of parameters and their significance. Although not without its limitations, bootstrapping is a procedure that is routinely used when estimating path models with nonnormal data (Byrne, 2010).
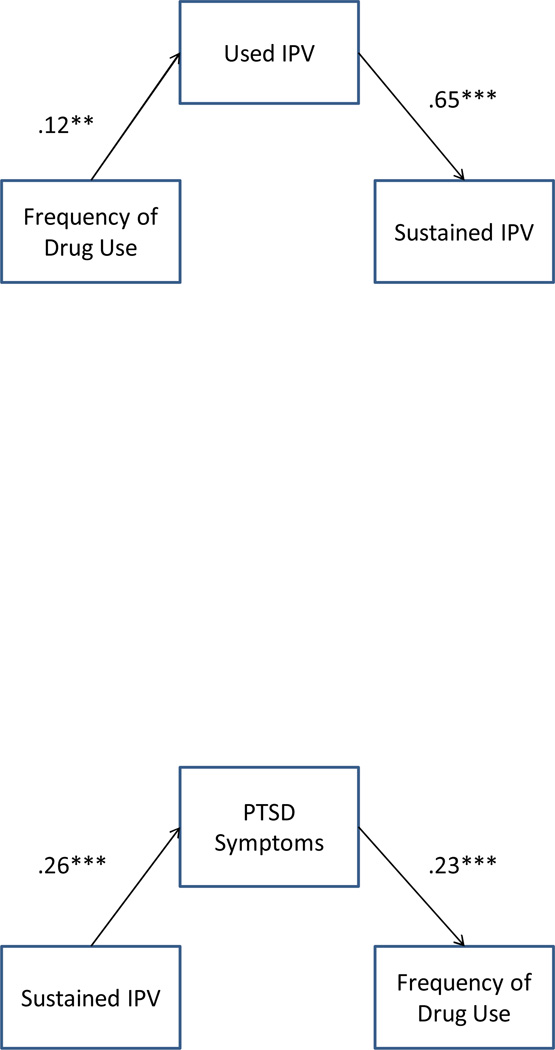
For alcohol abuse predicting IPV sustained, the full hypothesized model achieved a moderate-to-good fit to the data, χ2 (2) = 12.27, p = .002; NFI = .96; GFI = .99; RMSEA = .10, AIC = 28.27, ECVI = .06. The final, parsimonious model achieved an excellent fit: χ2 (1) = 0.05, p = .82; NFI = 1.00; GFI = 1.00; RMSEA = .00, AIC = 12.00, ECVI = .02. This final model represents a significant improvement in the chi-square fit of the model, Δχ2 (1) = 12.23, p = .0005, and the parameter estimates for this model are shown in Figure 3. Child maltreatment dropped out of the model, and the influence of alcohol intoxication on sustaining IPV was fully mediated by the use of IPV. Overall, this model explained 42.5% of the variance in sustaining physical IPV.
Figure 3.
Final Models Explaining Associations Among Drug Abuse and Sustaining IPV Among Community Sample Only, **p < .01, *** p < .001.
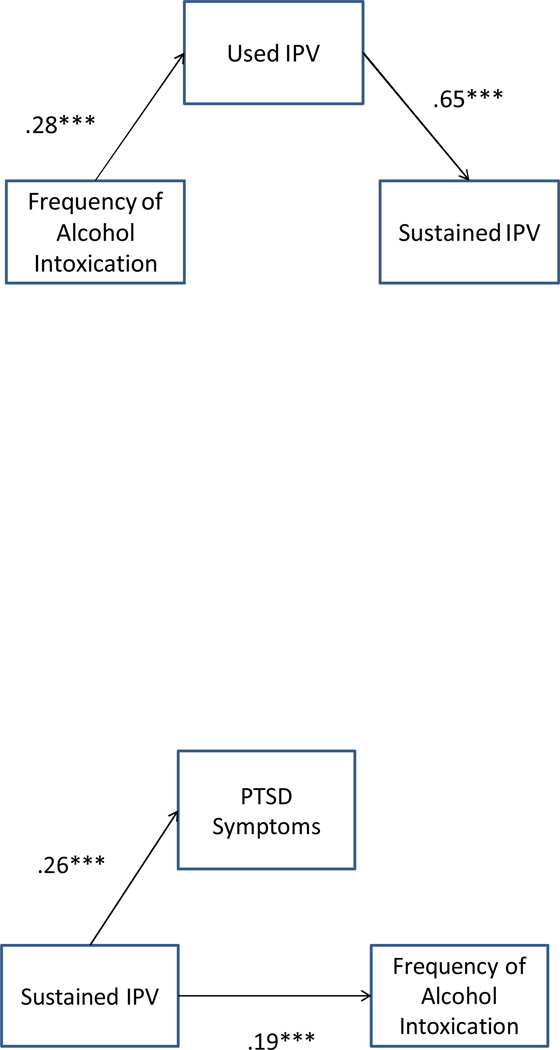
The full model for sustaining IPV predicting alcohol abuse also achieved a moderate-to-good fit, χ2 (2) = 7.36, p = .03; NFI = .90; GFI = .99; RMSEA = .07, AIC = 23.36, ECVI = .05. After non-significant paths were removed one-by-one, the final model, shown in the bottom half of Figure 2, achieved an excellent fit, χ2 (1) = 0.10, p = .76; NFI = .99; GFI = 1.00; RMSEA = .00, AIC = 10.10, ECVI = .02. This reduced model was a significant improvement over the full model, Δχ2 (1) = 7.26, p = .007, but explained only 4% of the variance in alcohol abuse. Overall, the model shows that sustaining IPV has direct influences on both frequency of alcohol intoxication and the level of PTSD symptoms, but that the level of PTSD symptoms does not serve as a mediator between sustaining IPV and alcohol intoxication.
Figure 2.
Final Models for the Association Among Alcohol Abuse and Sustaining IPV Among Community Sample Only, *** p < .001.
To determine whether the final model predicting sustaining IPV from alcohol abuse was a better fit than the final model predicting alcohol abuse from sustaining IPV, we compared the two models’ AICs and ECVIs. There were no differences in the ECVIs. The final model where alcohol intoxication predicted sustaining IPV had a slightly lower AIC than the final model where sustaining IPV predicted alcohol abuse; therefore, it was concluded that the best-fitting model was one where alcohol intoxication predicts sustaining IPV. In addition, the differences in the percent of variance explained (41% v. 4%) provide further evidence that the model where alcohol intoxication predicts sustaining IPV is a better model.
The full model investigating drug abuse as a predictor of sustaining IPV achieved a moderate-to-good fit of the data, χ2 (2) = 11.63, p = .003; NFI = .96; GFI = .99; RMSEA = .10, AIC = 27.63, ECVI = .05. After removing nonsignificant paths one at a time, the final model achieved a good-to-excellent fit, χ2 (1) = 2.94, p = .09; NFI = .99; GFI = .99; RMSEA = .06, AIC = 12.94, ECVI = .02. This reduced model was a significant improvement over the full model, Δχ2 (1) = 8.69, p = .003, and showed that using IPV served as a full mediator of the relationship between frequency of drug use and sustaining IPV (Figure 3). This model explained 42% of the variance in physical IPV sustained.
The full model predicting drug abuse from sustaining IPV was a moderate fit to the data, χ2 (2) = 7.52, p = .02; NFI = .91; GFI = .99; RMSEA = .07, AIC = 23.52, EDVI = .05. The final model, also displayed in Figure 3, was a good-to-excellent fit, χ2 (1) = 3.11, p = .08; NFI = 1.00; GFI = .99; RMSEA = .06, AIC = 13.11, ECVI = .023, and was a significant improvement over the full model, Δχ2 (1) = 4.41, p = .04. This model explained 5% of the variance in drug abuse, and showed that the level of PTSD symptoms was a full mediator between sustaining IPV and frequency of drug use.
To determine whether the final model predicting sustaining IPV from drug abuse was a better fit than the final model predicting drug abuse from sustaining IPV, we compared the two models’ AICs and ECVIs. There were no differences in the ECVIs. The final model where drug abuse predicted sustaining IPV had a lower AIC than the final model where sustaining IPV predicted drug abuse; therefore, it was concluded that the best-fitting model was one where drug abuse predicts sustaining IPV. In addition, the difference in the percent of variance explained (42% v. 5%) provides further evidence that the model where drug abuse predicts sustaining IPV is a better model.
Hypothesis 2: Differences Among IT, CCV, and No Violence Groups in Alcohol and Drug Abuse
To test our first hypothesis, we divided the community sample into those who sustained IPV (CCV group) and those who sustained no IPV; the helpseeking sample was as an indicator of IT. These divisions were in line with our previous analyses that established the no violence, IT, and CCV groups (Hines & Douglas, 2010).ii We then performed chi-square and ANCOVA analyses to investigate whether there were significant differences among the three groups in the variables assessing alcohol and drug abuse the percentage of men meeting the criteria for alcohol abuse and drug abuse.
As shown in Table 3, the no IPV group was the group least likely to have abused alcohol in the past year. The IT group was significantly more likely to have abused alcohol than the no IPV group, but the CCV group had the highest rates of alcohol abuse in the past year. Similarly, the CCV group reported intoxication in the past year significantly more frequently than either the no IPV or IT groups, who were not different from each other in reported intoxication frequency within the past year. For drug abuse, the no IPV group had the lowest rates and frequency within the past year. Both the IT and CCV groups had significantly higher rates and frequencies of drug abuse in comparison to the no IPV group, but they were not different from each other on either measure of drug abuse.
Table 3.
AN(C)OVA and chi-square results on the differences among IPV groups in alcohol/drug abuse
| No Violence %or M(SD) |
CCV† % or M(SD) |
IT† % or M(SD) |
F or χ2 (df) |
η2 | |
|---|---|---|---|---|---|
| Abused Alcohol in Past Year | 11.5a | 30.6a | 17.9a | 21.00*** (2) |
|
| Freq of Intoxication in Past Year | 0.76 (1.35)a | 1.80 (2.16)a,b | 1.00 (1.46)b | 11.33*** (2, 794) |
.03 |
| Abused Drugs in Past Year | 5.3a,b | 15.3a | 11.6b | 14.29*** (2) |
|
| Freq of Drug Use in Past Year | 0.20 (0.65)a,b | 0.51 (1.06)a | 0.43 (0.90)b | 8.24*** (2, 783) |
.02 |
Note: Means in the same row sharing superscripts are significantly different from each other. For frequency of intoxication, means in the same row sharing superscripts are significantly different from each other after controlling for age and presence of children. For frequency of drug use, means in the same row sharing superscripts are significantly different from each other after controlling for age, presence of children, and educational level. For ANCOVA results, unadjusted means are presented, and Tamhane post-hoc tests (because they correct for heterogeneity of variance) were used to identify the locus of any significant differences.
CCV = common couple violence, IT = intimate terrorism
p < .001.
Discussion
The purpose of this study was to investigate the associations and possible mediators between alcohol/drug abuse and sustaining IPV among two samples of men: a helpseeking sample that sustained IT and a community sample, 16% of which sustained CCV. Our study showed support for the hypothesis that the predictors and mediators of any associations among sustaining IPV and alcohol/drug abuse would differ among the two samples; however, only the community sample conformed to any of the proposed models. Moreover, our study showed mixed support for the hypothesis that sustaining more severe types of IPV would be associated with higher levels of alcohol/drug abuse because the experience would be more traumatic.
Alcohol Abuse
Overall, and consistent with Simons et al. (2008), there was support for the hypothesis that sustaining IPV would be associated with higher levels of alcohol abuse. However, contrary to our prediction, the men who experienced CCV had the highest levels of alcohol abuse and frequency of intoxication within the past year. In addition, although in comparison to men who sustained no IPV, men who experienced IT had higher levels of alcohol abuse within the past year, they did not report a greater frequency of intoxication.
Men who experience CCV would be in relationships in which the incidence and frequency of all types of IPV would be about equal between them and their female partners (Johnson, 1995, 2006; Johnson & Ferraro, 2000), as was the case with the men in the community sample (Hines & Douglas, 2010). Therefore, the reason that the CCV group had the highest levels of alcohol abuse and intoxication could lie in the fact that perhaps in men, alcohol abuse is more predictive of the use of IPV, rather than sustaining IPV. This is supported by the fact that in the helpseeking sample, there were no associations between sustaining IPV and either alcohol abuse or intoxication. In addition, our best-fitting path model for the men in the community sample showed that the association between alcohol intoxication and sustaining IPV was fully mediated by the men’s use of IPV. This finding supports Kilpatrick et al.’s (1997) theory that perhaps alcohol abuse is a risk factor for sustaining IPV because alcohol abuse leads one into certain situations or relationships, or leads one to behave in a certain way, in which sustaining IPV is more likely. Thus, it seems that for the community men, alcohol intoxication led them to use IPV, which then led to them sustaining IPV from their partners, perhaps in retaliation or self-defense.
We tested an alternative explanation to this hypothesis (results not shown), in which we hypothesized that the association between alcohol intoxication and using IPV would be mediated by sustaining IPV. In this situation, alcohol intoxication would lead to the man sustaining IPV, which would then lead to him using IPV, perhaps in retaliation or self-defense. This model proved to be a poor fit to the data, χ2 (1) = 23.45, p < .001, NFI = .93, GFI = .97, RMSEA = .21. Thus, it seems that alcohol intoxication has little to do with directly predicting men’s victimization from IPV, but only indirectly predicts men’s victimization from IPV through his perpetration of IPV. These results support studies on women who sustain IPV or violence (Kilpatrick, et al., 1997; Martino, et al., 2005; Testa, et al., 2003), which show no evidence that alcohol intoxication leads to sustaining IPV or violence.
It is also important to note that among the community men, there was support for Kilpatrick’s (1997) hypothesis that sustaining IPV is a risk factor for alcohol abuse. Although this model was an excellent fit to the data, it was not as good of a fit as the model in which alcohol abuse predicted sustaining IPV, and it only predicted a small percentage of the variance in alcohol abuse. In addition, there was no support for the hypothesis that this association would be mediated by the level of PTSD symptoms. In fact, sustaining IPV directly predicted both levels of PTSD symptoms and alcohol intoxication, which were not significantly related to each other. We can only speculate as to why levels of PTSD symptoms did not serve as a mediator between sustaining IPV and alcohol intoxication, given the current literature that states that PTSD and alcohol/substance abuse are highly comorbid disorders that are functionally related (Chilcoat & Breslau, 1998; Jacobsen, et al., 2001; Stewart, 1996; Stewart, et al., 1998) because alcohol and other drugs seem to provide acute symptom relief of PTSD (Chilcoat & Breslau, 1998; Jacobsen, et al., 2001; Stewart, 1996; Stewart, et al., 1998).
Perhaps the differences in our findings are due to the fact that we were not able to make a definitive diagnosis of PTSD; we were assessing levels of PTSD symptoms on a continuous scale in our path models. Thus, we recommend additional research that explores the associations among alcohol intoxication and both levels of PTSD symptoms and actual diagnosis of PTSD among studies of IPV using men in community samples. In addition, because there was support for, and minimal differences between, both models -- that alcohol intoxication predicted sustaining IPV through using IPV, and that sustaining IPV predicted alcohol intoxication and levels of PTSD symptoms -- we need to further investigate the associations among sustained IPV and alcohol intoxication among men, preferably with longitudinal data.
It is also worth speculating as to why there was no dose-response relationship between alcohol abuse and violence victimization (or perpetration) among the helpseeking sample of men. Past research suggests that men are more likely than women to abuse alcohol or other substances in response to a stressful event (Cooper, et al., 1992), and being victimized by IT would certainly be considered a stressful event. However, the men in the helpseeking sample were no more likely to abuse alcohol than the men in the community sample who experienced less frequent and severe IPV, nor were they drinking more in response to increasing levels of IT victimization.
The answer to this contradiction may lie in the nature of the helpseeking sample. Men are less likely than women to seek help for a wide range of psychological, social, and physical health issues; moreover, men are even less likely to seek help for an issue that is non-normative for men (i.e., victimization from domestic violence is considered a women’s issue), that others may perceive they should be able to handle themselves, and that may cast him as being “deviant” (Addis & Mahalik, 2003). Thus, the men in our sample had to overcome many social and psychological barriers to seeking help, in addition to any external barriers that they may have had to encounter after deciding to seek help (e.g., being told that a domestic violence agency only helps women) (Douglas & Hines, 2010). Men who are able to overcome such barriers may have better coping mechanisms and be less likely to abuse alcohol in response to IT victimization. The fact that our helpseeking sample seems to be significantly better educated and have a slightly higher income, despite their younger age, than men in the community sample, lends support to the notion that these men are in some way different than a sample of average men – maybe their higher educational status allows them to psychologically break from traditional masculine norms and seek help for a non-normative issue. Therefore, male victims of IT who do not seek help may indeed show a dose-response relationship between IPV victimization and alcohol/drug abuse, and may even evidence the highest levels of alcohol abuse among all male victims of IPV, since they do not seek help and may use other coping mechanisms, such as alcohol or other drugs. We recommend research that strives to study the associations between alcohol/drug abuse and IPV victimization among such a population.
Drug Abuse
Consistent with previous research (Kilpatrick, et al., 1997; Kilpatrick, et al., 2000; Salomon, et al., 2002; Testa, et al., 2003), we also found that men sustaining either CCV or IT had higher levels of drug abuse in the past year and higher frequencies of drug use, in comparison to men who did not sustain IPV. However, contrary to our expectation that men who sustained IT would have higher levels of drug abuse than men who sustained CCV because their experiences would be more traumatic, we found no differences between men sustaining CCV and IT in either the percentage of men abusing drug in the past year or their frequency of drug use in the past year. Thus, for men, it seems that sustaining IPV is associated with elevated levels of drug abuse, but it does not matter which type of IPV is sustained – they both have equally elevated levels of drug abuse. This is inconsistent with Johnson’s (1995, 2006; Johnson & Ferraro, 2000) assertion that CCV and IT would necessarily have different predictors and consequences. However, as previously mentioned, this inconsistency could be due to the unique nature of our helpseeking sample, and Johnson’s hypothesis may be borne out among a sample of male IT victims who do not seek help.
What is consistent with Johnson’s (1995, 2006; Johnson & Ferraro, 2000) assertion is that the associations among sustaining IPV and drug abuse were different for the two samples. For men in the helpseeking sample, there was no dose-response relationship between sustaining any type of IPV and drug abuse or frequency of drug use. For the community sample, there was. Thus, perhaps once one reaches a certain level of IPV victimization, sustaining further acts of IPV would no longer increase one’s risk for drug abuse. We performed three regression analyses with both samples combined (results not shown) to test this hypothesis -- linear, cubic, and quadratic -- and the only significant regression model was a cubic model that showed that initially, frequency of drug use increased as IPV victimization increased and then leveled off between 50 and 225 acts sustained in the past year; at about 225 acts sustained, there was again an increase in the frequency of drug use in the past year. Alternatively, the lack of a dose-response relationship for the helpseeking sample could be due to the uniqueness of such a sample, as discussed previously.
For the community sample, there was support for the hypothesis that drug abuse would predict sustaining IPV, which is consistent with both Kilpatrick et al.’s (1997) and Testa et al.’s (2003) findings among women. In addition, our findings expand upon these results by pointing towards a mediator that, to our knowledge, has never been tested among women: Specifically, among the community men, perpetrating IPV was a full mediator of the association between drug abuse and sustaining IPV. Thus, similar to our results with alcohol intoxication, among men, frequency of drug use predicts the use of IPV, which then predicts sustaining IPV, perhaps in retaliation or self-defense.
The opposite model, that sustaining IPV would predict drug abuse, was also a good fit to the data, which is consistent with previous research among women who sustain IPV and violence (Kilpatrick, et al., 1997; Salomon, et al., 2002) and among adolescent male victims of violence in general (Kilpatrick, et al., 2000). In addition, this association was fully mediated by levels of PTSD symptoms, which is consistent with the self-medication model that posits that in an effort to cope with and reduce the overwhelming negative emotions that accompany a trauma like IPV, the person might abuse substances (Jacobsen, et al., 2001; J. S. Simons, et al., 2005; Stewart, 1996).
Thus, among the community sample, there was support for sustaining IPV predicting drug abuse and for drug abuse predicting sustaining IPV. The model showing that sustaining substance abuse predicts IPV was a better fitting model and also explained a much higher percentage of the variance in the outcome variable, but both were good-to-excellent fits to the data. These results are consistent with Kilpatrick et al.’s (1997) study of women who sustain violence. In addition to finding support for both models, using longitudinal analyses, they found evidence for a vicious cycle between drug abuse and violence, in which drug abuse increased the risk for violent victimization, which in turn, led to increased risk for further drug abuse. Such a model could also be occurring among men as well, but because our data are cross-sectional, we are unable to test this hypothesis. Thus, future studies should aim to investigate the temporal associations among drug abuse and sustaining IPV in men using longitudinal designs.
Limitations and Future Research
The limitations of this study need to be addressed so that future research can replicate and expand on the findings reported here. First, as mentioned previously, this is a cross-sectional study, and therefore, inferences about causality cannot be firmly established. In fact, for both alcohol and drug abuse, although we were able to distinguish which models fit the data the best, the models that predicted opposite effects were both excellent fits. Therefore, future research should aim to test these models in a longitudinal design. Second, it is possible that some of the men who were classified as IT victims were really victims of CCV and vice versa. Johnson (Johnson, 1995, 2006; Johnson & Ferraro, 2000) does not provide “cut-off” criteria to establish which individuals sustain IT versus CCV; he only provides modest guidelines to establish whether a sample would be characteristic of IT or CCV. We agree with Johnson’s efforts to distinguish types of violence and find this differentiation useful; however, without existing cut-off measures, it is currently not possible to definitively categorize individuals into IT or CCV groups. It is important to note that if there are CCV victims in our IT group and/or IT victims in our CCV group, that would serve as error and would weaken all associations reported in this paper.
Third, the study relies solely on the men’s reports of their partners’ aggressive behaviors and their own psychosocial characteristics. This limitation is important to consider for three primary reasons: (1) Correlations between aggressive behaviors and psychosocial characteristics may be inflated because certain traits of the participant may influence how he answers both sets of questions (Cooper, 2002); (2) It is possible that the men overestimated their female partners’ use of IPV; however, studies of couples reporting on IPV show no difference between male and female partners in their estimates of women’s use of IPV (Archer, 1999); (3) By using only the men’s reports, we have no external validation of the authenticity of their reports. We were concerned, particularly for our helpseeking sample, about the confidentiality and safety of the participants if we asked their partners to participate in this study as well. Therefore, we opted not to obtain these data directly from the female partner, but note that such methodology has been used in most of the studies on IPV and on samples measuring IT that we cited in this article. Thus, we recommend that future studies, whenever possible, should strive to obtain information from multiple informants.
Conclusion
In closing, this study provides valuable information regarding our understanding of male IPV victimization. We can conclude that men who sustain IPV from their female partners engage in more alcohol and drug abuse than men who do not sustain IPV. However, among men who seek help for IT victimization, increased levels of victimization do not predict increased levels of alcohol or drug abuse, possibly because they have active coping mechanisms. Given that our helpseeking sample of men is a unique sample, it would be valuable to investigate whether such associations would be found among men who sustain IT and do not seek help. Among men who sustain CCV, increased levels of IPV victimization are associated with increased levels of alcohol and drug abuse, as expected, and the best potential explanation for this association seems to be that alcohol/drug abuse leads to IPV perpetration, which then leads to IPV victimization.
The results of this study can be useful to alcohol and drug abuse providers and other service providers in the field of family violence. We encourage the screening of alcohol and drug abuse among male IPV victims and the screening of IPV among men who seek treatment for alcohol and drug use. Even though this paper documents that alcohol and drug abuse among IT victims is not an overarching issue, we encourage family violence providers to have a method of providing alcohol and drug abuse treatment for men, even if this means making referrals to providers outside of domestic violence agencies. At the same time, men do not usually seek help for CCV, and thus we encourage the screening of IPV among men who seek help for alcohol and drug abuse, because in for these men, it may be a red flag for other problematic behaviors that may otherwise go unnoticed.
Acknowledgments
The project described was supported by Grant Number 5R21MH074590 from the National Institute of Mental Health. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIMH. Special thanks to Dr. Murray Straus for his continued guidance, support, and consultation on this project.
Footnotes
To be certain, we did run the same models with the helpseeking sample as we did with the community sample. As expected, none of the models were good fits to the data, even when nonsignificant parameters were pruned. In fact, for the models where we were using alcohol/drug abuse to predict IPV victimization, the only significant paths were from IPV perpetration to IPV victimization, and for the models where we predicted alcohol/drug abuse from IPV victimization, the only significant paths were from IPV victimization to levels of PTSD symptoms and from levels of PTSD symptoms to drug abuse.
A full description of how we determined that the helpseeking sample was a sample of IT victims can be found in Hines and Douglas (2010). Briefly, we did a series of comparisons between the helpseeking and community samples in the rates and frequencies of physical IPV, controlling behaviors, severe psychological IPV, and injuries reported by the male participants, to test Johnson’s conceptualization of IT that it is physical IPV in the context of controlling behaviors and severe psychological IPV, whereas CCV is characterized by low-level mutual physical IPV without the same level of controlling behaviors as in IT. In comparison to the male helpseekers, the female partners of men in the helpseeking sample had significantly higher rates of all types of IPV, and just among those men and women who engaged in physical and psychological IPV, the female partners used 5–6 times the frequency of physical IPV, severe psychological IPV, and controlling behaviors. The helpseeking men also had significantly higher rates of injuries than their female partners, and among those men and women who sustained injuries, the men were injured at approximately twice the frequency. Finally, the frequency with which men sustained violence in the previous year (46.72 acts) is comparable to the frequency of violence sustained in samples of battered women (between 15 and 68 acts per year). Patterns of IT were also found when we compared the helpseeking with the community sample. In comparison to the female partners of community men, the female partners of helpseeking men engaged in significantly higher rates and frequency of all types of IPV: they were 54 (controlling behaviors) to 407 (minor physical IPV) times more likely to use IPV. Among just those women who used IPV, the female partners in the helpseeking sample had significantly higher frequencies of IPV, ranging from about 1.5 times (severe physical IPV) to over 3.75 times (controlling behaviors, total physical IPV) the frequency of IPV than female partners in the community sample. Moreover, the men in the helpseeking sample were injured at higher rates and frequencies – they were close to 90 times more likely to have sustained an injury in the past year, and when comparing just those men who were injured, men in the helpseeking sample had about twice the frequency of injuries. Finally, the female partners in the helpseeking sample were significantly more likely to have used physical IPV first, in both the last physical argument (97% v. 56.9%) and ever (91.7% v. 53.0%).
Contributor Information
Denise A. Hines, Clark University
Emily M. Douglas, Bridgewater State University
References
- Addis ME, Mahalik JR. Men masculinity, and the contexts of help seeking. American Psychologist. 2003;58:5–14. doi: 10.1037/0003-066x.58.1.5. [DOI] [PubMed] [Google Scholar]
- Amaro H, Fried LE, Cabral H, Zuckerman MD. Violence during pregnancy and substance use. American Journal of Public Health. 1990;80:575–579. doi: 10.2105/ajph.80.5.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- Amos C, Peters RJ, Williams L, Johnson RJ, Martin Q, Yacoubian GS. The link between recent sexual abuse and drug use among African American male college students: It's not just a female problem in and around campus. Journal of Psychoactive Drugs. 2008;40(2):161–166. doi: 10.1080/02791072.2008.10400626. [DOI] [PubMed] [Google Scholar]
- Archer J. Assessment of the reliability of the Conflict Tactics Scales: A meta-analytic review. Journal of Interpersonal Violence. 1999;14:1263–1289. [Google Scholar]
- Archer J. Sex differences in aggression between heterosexual couples: A meta-analytic review. Psychological Bulletin. 2000;126:651–680. doi: 10.1037/0033-2909.126.5.651. [DOI] [PubMed] [Google Scholar]
- Bentler PM. EQS 6 Structural equations program manual. Encino, CA: Multivariate Software; 2005. [Google Scholar]
- Blanchard EB, Jones-Alexander JB, Buckley TC, Forneris CA. Psychometric properties of the PTSD checklist (PCL) Behavior Research and Therapy. 1996;34:669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Byrne BM. Structural equation modeling with AMOS: Basic concepts, applications, and programming. 2nd ed. New York: Routledge; 2010. [Google Scholar]
- Catalano S. Intimate partner violence in the United States. 2007 Retrieved from http://bjs.ojp.usdoj.gov/index.cfm?ty=pbdetail&iid=1000.
- Chilcoat HD, Breslau N. Investigations of causal pathways between PTSD and drug use disorders. Addictive Behaviors. 1998;23(6):827–840. doi: 10.1016/s0306-4603(98)00069-0. [DOI] [PubMed] [Google Scholar]
- Cooper ML. Personality and close relationships: Embedding people in important social contexts. Journal of Personality. 2002;70:757–782. doi: 10.1111/1467-6494.05023. [DOI] [PubMed] [Google Scholar]
- Cooper ML, Russell M, Skinner JB, Frone MR, Mudar P. Stress and alcohol use: Moderating effects of gender, coping, and alcohol expectancies. Journal of Abnormal Psychology. 1992;101(1):139–152. doi: 10.1037//0021-843x.101.1.139. [DOI] [PubMed] [Google Scholar]
- Douglas EM, Hines DA. The helpseeking experiences of men who sustain intimate partner violence: An overlooked population and implications for practice. Journal of Family Violence, provisionally accepted for publication. 2010 doi: 10.1007/s10896-011-9382-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fals-Stewart W. The occurrence of partner physical aggression on days of alcohol consumption: A longitudinal diary study. Journal of Consulting and Clinical Psychology. 2003;71:41–52. doi: 10.1037//0022-006x.71.1.41. [DOI] [PubMed] [Google Scholar]
- Fals-Stewart W, Leonard KE, Birchler GR. The occurrence of male-to-female intimate partner violence on days of men’s drinking: The moderating effects of antisocial personality disorder. Journal of Consulting and Clinical Psychology. 2005;73(2):239–248. doi: 10.1037/0022-006X.73.2.239. [DOI] [PubMed] [Google Scholar]
- Giles-Sims J. Wife battering: A systems theory approach. New York: Guilford Press; 1983. [Google Scholar]
- Halford WK, Osgarby SM. Alcohol abuse in clients presenting with marital problems. Journal of Family Psychology. 1993;6(3):245–254. [Google Scholar]
- Hines DA, Douglas EM. Intimate terrorism by women towards men: Does it exist? Journal of Aggression, Conflict, and Peace Research. 2010;2(3):36–56. doi: 10.5042/jacpr.2010.0335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hines DA, Douglas EM, Mahmood S. The Effects of Survey Administration on Disclosure Rates to Sensitive Items Among Men: A Comparison of an Internet Panel Sample with a RDD Telephone Sample. Computers in Human Behavior. 2010;26:1327–1335. doi: 10.1016/j.chb.2010.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobsen LK, Southwick SM, Kosten TR. Substance use disorders in patients with posttraumatic stress disorder: A review of the literature. American Journal of Psychiatry. 2001;158(8):1184–1190. doi: 10.1176/appi.ajp.158.8.1184. [DOI] [PubMed] [Google Scholar]
- Johnson MP. Patriarchal terrorism and common couple violence: Two forms of violence against women. Journal of Marriage and the Family. 1995;57:283–294. [Google Scholar]
- Johnson MP. Conflict and control: Gender symmetry and asymmetry in domestic violence. Violence Against Women. 2006;12(11):1003–1018. doi: 10.1177/1077801206293328. [DOI] [PubMed] [Google Scholar]
- Johnson MP, Ferraro KJ. Research on domestic violence in the 1990s: Making distinctions. Journal of Marriage and the Family. 2000;62:948–963. [Google Scholar]
- Kantor GK, Asdigian N. When women are under the influence: Does drinking or drug use by women provoke beatings by men? In: Galenter M, editor. Recent developments in alcoholism, Vol. 13: Alcohol and violence. New York: Plenum; 1997. pp. 315–336. [PubMed] [Google Scholar]
- Kessler RC, Molnar BE, Feurer ID, Appelbaum M. Patterns and mental health predictors of domestic violence in the United States: Results from the National Comorbidity Survey. International Journal of Law and Psychiatry. 2001;24:487–508. doi: 10.1016/s0160-2527(01)00080-2. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Acierno R, Resnick HS, Saunders BE, Best CL. A 2-year longitudinal analysis of the relationship between violent assault and substance use in women. Journal of Consulting and Clinical Psychology. 1997;65:834–847. doi: 10.1037//0022-006x.65.5.834. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Acierno R, Saunders BE, Resnick HS, Best CL, Schnurr PP. Risk factors for adolescent substance abuse and dependence: Data from a national sample. Journal of Consulting and Clinical Psychology. 2000;68(1):19–30. doi: 10.1037//0022-006x.68.1.19. [DOI] [PubMed] [Google Scholar]
- Leonard KE. U.S. Department of Health and Human Services. Research Monograph 24: Alcohol and interpersonal violence: Fostering multidisciplinary perspectives. Rockville, MD: National Institutes of Health; 1993. Drinking patterns and intoxication n marital violence: Review, critique, and future directions for research; pp. 253–280. [Google Scholar]
- Liebschutz J, Savetsky JB, Saitz R, Horton NJ, Lloyd-Travaglini C, Samet JH. The relationship between sexual and physical abuse and substance abuse consequences. Journal of Substance Abuse Treatment. 2002;22(3):121–128. doi: 10.1016/s0740-5472(02)00220-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mardia KV. Measures of multivariate skewness and kurtosis with applications. Biometrika. 1970;57:519–530. [Google Scholar]
- Mardia KV. Applications of some measures of multivariate skewness and kurtosis in testing normality and robustness studies. Sankhya. 1974;B36:115–128. [Google Scholar]
- Martino SC, Collins RL, Ellickson PL. Cross-lagged relationships between substance use and intimate partner violence among a sample of young adult women. Journal of Studies on Alcohol. 2005;66(1):139–148. doi: 10.15288/jsa.2005.66.139. [DOI] [PubMed] [Google Scholar]
- McDonald R, Jouriles EN, Tart CD, Minze LC. Children's adjustment problems in families characterized by men's severe violence toward women: Does other family violence matter? Child Abuse and Neglect. 2009;33:94–101. doi: 10.1016/j.chiabu.2008.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyers LS, Gamst G, Guarino AJ. Applied multivariate research: Design and interpretation. Thousand Oaks, CA: Sage; 2006. [Google Scholar]
- Murphy CM, O'Farrell TJ, Fals-Stewart W, Feehan M. Correlates of intimate partner violence among male alcoholic patients. Journal of Consulting and Clinical Psychology. 2001;69:528–540. doi: 10.1037/0022-006X.69.3.528. [DOI] [PubMed] [Google Scholar]
- O'Farrell TJ, Fals-Stewart W, Murphy M, Murphy CM. Partner violence before and after individually based alcoholism treatment for male alcoholic patients. Journal of Consulting and Clinical Psychology. 2003;71:92–102. doi: 10.1037//0022-006x.71.1.92. [DOI] [PubMed] [Google Scholar]
- Okun L. Woman abuse: Facts replacing myths. Albany, NY: State University of New York Press; 1986. [Google Scholar]
- Robins L, Helzer J, Cottler L, Goldring E. NIMH Diagnostic Interview Schedule. Vol. 3. St. Louis, MO: Washington University Press; 1988. [Google Scholar]
- Ruggiero KJ, DelBen K, Scotti JR, Rabalais AE. Psychometric properties of the PTSD Checklist--Civilian Version. Journal of Traumatic Stress. 2003;16:495–502. doi: 10.1023/A:1025714729117. [DOI] [PubMed] [Google Scholar]
- Salomon A, Bassuk SS, Huntington N. The relationship between intimate partner violence and the use of addictive substances in poor and homeless single mothers. Violence Against Women. 2002;8(7):785–815. [Google Scholar]
- Simons JS, Gaher RM, Jacobs GA, Meyer D, Johnson-Jimenez E. Associations between alcohol use and PTSD symptoms among American Red Cross disaster relief workers responding to the 9/11/2001 attacks. American Journal of Drug and Alcohol Abuse. 2005;31:385–304. [PubMed] [Google Scholar]
- Simons L, Gwin D, Brown M, Gross J. Alcohol and other drug use among college students: Intimate partner violence and health-comprimising behaviors. Alcoholism Treatment Quarterly. 2008;26(3):347–364. [Google Scholar]
- Stark E, Flitcraft A. Violence among intimates: An epidemiological review. In: Van Hesselt V, Morrison R, Bellack A, Hersen M, editors. Handbook of family violence. New York: Plenum; 1988. pp. 293–297. [Google Scholar]
- Stets JE, Straus MA. Gender differences in reporting marital violence and its medical and psychological consequences. In: Straus MA, Gelles RJ, editors. Physical violence in American families: Risk factors and adaptation to violence in 8,145 families. New Brunswick, NJ: Transaction; 1990. pp. 151–166. [Google Scholar]
- Stewart SH. Alcohol abuse in individuals exposed to trauma: A critical review. Psychological Bulletin. 1996;120(1):83–112. doi: 10.1037/0033-2909.120.1.83. [DOI] [PubMed] [Google Scholar]
- Stewart SH, Conrod PJ, Pihl RO, Dongier M. Relations between posttraumatic stress syndrome dimensions and substance dependence in a community-recruited sample of substance-abusing women. Psychology of Addictive Behaviors. 1999;13:78–88. [Google Scholar]
- Stewart SH, Pihl RO, Conrod PJ, Dongier M. Functional associations among trauma, PTSD, and substance-related disorders. Addictive Behaviors. 1998;23(6):797–812. doi: 10.1016/s0306-4603(98)00070-7. [DOI] [PubMed] [Google Scholar]
- Stith SM, Rosen KH, Middleton KL, Busch AL, Lundeberg K, Carlton RP. The intergenerational transmission of spouse abuse: A meta-analysis. Journal of Marriage and the Family. 2000;62:640–654. [Google Scholar]
- Stith SM, Smith DB, Penn CE, Ward DB, Tritt D. Intimate partner physical abuse perpetration and victimization risk factors: A meta-analysis review. Aggression and Violent Behavior. 2004;10(1):65–98. [Google Scholar]
- Straus MA. Injury and frequency of assault and the ‘representative sample fallcy’ in measuring wife beating and child abuse. In: Straus MA, Gelles RJ, editors. Physical violence in American families: Risk factors and adaptations in 8,145 families. New Brunswick, NJ: Transaction; 1990. pp. 75–89. [Google Scholar]
- Straus MA. Trends in cultural norms and rates of partner violence: An update to 1992. In: Stith S, Straus MA, editors. Understanding partner violence: Prevalence, causes, consequences, and solutions. Minneapolis, MN: National Council on Family Relations; 1995. pp. 30–33. [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, Sugarman D. The Revised Conflict Tactics Scales (CTS-2): Development and preliminary psychometric data. Journal of Family Issues. 1996;17:283–316. [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, Sugarman D. The Personal and Relationships Profile (PRP) 1999 Available from http://pubpages.unh.edu/~mas2/
- Straus MA, Mouradian VE. Preliminary psychometric data from the Personal and Relationships Profile (PRP): A multi-scale tool for clinical screening and research on partner violence. 1999 from http://pubpages.unh.edu/~mas2/
- Tabachnik BG, Fidell LS. Using Multivariate Statistics. 5th ed. New York: Allyn & Bacon; 2006. [Google Scholar]
- Testa M, Livingston JA, Leonard KE. Women's substance use and experiences of intimate partner violence: A longitudinal investigation among a community sample. Addictive Behaviors. 2003;28(9):1649–1664. doi: 10.1016/j.addbeh.2003.08.040. [DOI] [PubMed] [Google Scholar]
- Thompson MP, Sims L, Kingree JB, Windle M. Longitudinal associations between problem alcohol use and violent victimization in a national sample of adolescents. Journal of Adolescent Health. 2008;42(1):21–27. doi: 10.1016/j.jadohealth.2007.07.003. [DOI] [PubMed] [Google Scholar]
- Tjaden P, Thoennes N. Extent, nature, and consequences of intimate partner violence: Findings from the National Violence Against Women Survey. (No. NCJ 181867) Washington, DC: National Institute of Justice and Centers for Disease Control and Prevention; 2000. [Google Scholar]
- Tolman RM. Psychological Maltreatment of Women Inventory. [Retrieved October 15, 2007];1995 from http://www-personal.umich.edu/~rtolman/pmwif.htm.
- Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. Paper presented at the International Society for Traumatic Stress Studies.1993. [Google Scholar]