Abstract
In the former Soviet republics of central Asia, ethnic Russians have exhibited higher adult mortality than native ethnic groups (e.g., Kazakh, Kyrgyz, Uzbek) in spite of the higher socioeconomic status of ethnic Russians. The mortality disadvantage of ethnic Russians at adult ages appears to have even increased since the breakup of the Soviet Union. The most common explanation for this “Russian mortality paradox,” is that deaths are better reported among ethnic Russians. In this study, we use detailed mortality data from Kyrgyzstan between 1959 and 1999 to evaluate various explanations for the Russian mortality paradox: data artifacts, migration effects, and cultural effects. We find that the most plausible explanation is the cultural hypothesis because the personal behaviors that appear to generate a large part of the observed mortality differences (alcohol consumption, in particular) seem to be closely tied to cultural practices. We examine the implications of this finding for understanding the health crisis in post-Soviet states.
Keywords: Adult mortality, Central Asia, Kyrgyzstan, Alcohol, Former Soviet Union
Introduction
Calculations based on official data show that ethnic Russians living in the former Soviet republics of central Asia have experienced higher adult mortality than the indigenous ethnic groups of these republics, such as the Kazakh, Kyrgyz, or Uzbek (Darsky and Andreev 1991; Dobrovolskaya 1990). The mortality disadvantage of ethnic Russians at adult ages appears to have even increased since the breakup of the Soviet Union (Guillot 2007). This reported difference is surprising because it is commonly believed that ethnic Russians living in central Asia have enjoyed higher socioeconomic status than the indigenous population of these republics. The most common explanation for this paradox, which we term the “Russian mortality paradox,” is that deaths are better reported among ethnic Russians (Dobrovolskaya 1990; Sinelnikov 1988).
In this study, we use detailed data from one central Asian republic, Kyrgyzstan, between 1959 and 1999 to evaluate various explanations for this mortality paradox. We first review and update the existing literature on the nature and extent of this mortality difference. We also review and update the proposition that ethnic Russians living in central Asia have enjoyed a more favorable socioeconomic position than the indigenous population. We then evaluate three relevant hypotheses for the mortality paradox: data artifacts, migration effects, and cultural effects. Finally, we discuss the implications of this mortality paradox for understanding the health crisis in post-Soviet states.
Background
Central Asian Republics and Their Ethnic Groups
The populations of the five former Soviet republics of central Asia—Kazakhstan, Kyrgyzstan, Tajikistan, Turkmenistan, and Uzbekistan—are composed of many ethnic groups. The five most important indigenous groups are the Kazakhs, the Kyrgyz, the Tajiks, the Turkmens, and the Uzbeks. These ethnic groups are called “titular” because they are the groups after which the republics are named. The predominant religion among them is Sunni Islam.
Alongside these five central Asian groups live sizable population groups of Slavic origin. These include primarily Russians and, to a lesser extent, Ukrainians and Belorussians. The presence of Russians in central Asia can be traced to the colonial conquest of central Asia by the tsarist armies in the eighteenth and nineteenth centuries. The bulk of the Russian presence in central Asia, however, is the result of large migration flows that occurred during the 1950s and 1960s, under the impulse of the Soviet government. Net migration flows of Russians changed direction in the 1970s, when the number of Russians leaving central Asia started to exceed the number of arrivals. This trend dramatically accelerated after 1991, as the region experienced massive flows of Russians out of central Asian republics following the breakup of the Soviet Union and the republics’ access to independence.
In Kyrgyzstan, the ethnic Kyrgyz represented only 64.9% of the population at the 1999 census. This is explained in part by the fact that the territory of Kyrgyzstan includes areas in the South that have been predominantly populated by ethnic Uzbeks. In 1999, Uzbeks represented 13.8% of the total population. Kyrgyzstan has also had a relatively large Russian population in comparison with other central Asian republics. In the 1999 census, ethnic Russians represented 12.5% of the total population (13.6% if also including Ukrainians and Belorussians).
There are many other ethnic groups in central Asian republics in addition to the five titular central Asian groups and the Slavs. These groups represent small percentages of the total population. In Kyrgyzstan in 1999, for example, only 6.0% of the population was neither central Asian nor Slavic.
Evidence about the Excess Mortality of Ethnic Russians in Central Asia
Systematic evidence about the excess mortality of ethnic Russians in central Asia appeared in Soviet and Russian publications in the early 1990s. Dobrovolskaya (1990) compared, for each Soviet republic in 1969–1970 and 1978–1979, the mortality of the republic’s titular ethnic group to that of ethnic Russians living in that republic. She found that in almost all republics, the life expectancy at age 5 (e5) was lower for ethnic Russians than for the titular ethnic group and that this mortality disadvantage was particularly important for males and for Central Asian republics (with differences ranging from 2.8 years in Kazakhstan to 9.8 years in Tajikistan). Darsky and Andreev (1991) made similar calculations for the period 1988–1989 and found similar patterns for mortality in the age range 15–59. Andreev et al. (1992) also examined mortality differences at infant and child ages. At these ages, however, they found a Russian advantage. The excess mortality of ethnic Russians in central Asia thus appears to be primarily an adult phenomenon.
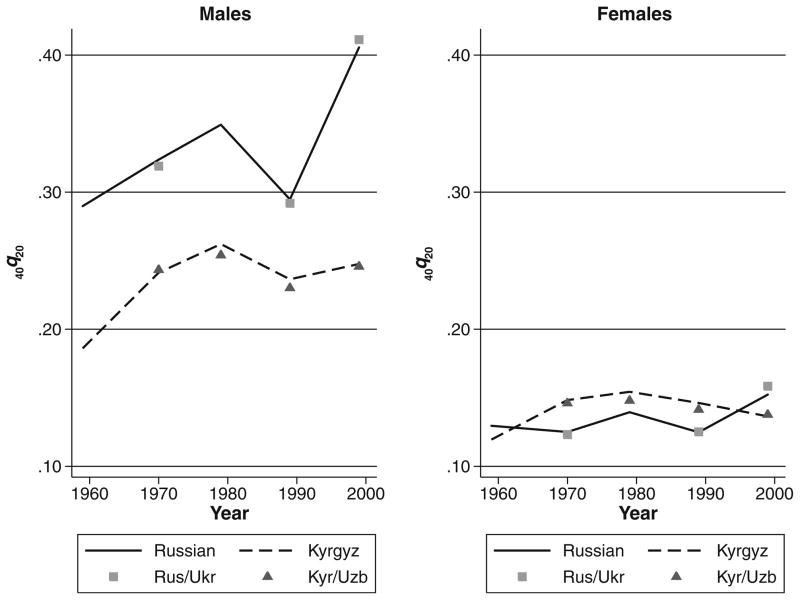
Our access to unpublished census and death tabulations from the National Statistical Committee (NSC) of the Kyrgyz Republic allows us to confirm and update the existence of this ethnic mortality difference for Kyrgyzstan. We focus here, and in the remainder of this study, on mortality in the age range 20–59 rather than on some more ambiguous measure of adult mortality, such as e5. This age range has emerged as a critical age range for understanding mortality fluctuations in Soviet and post-Soviet states (Anderson and Silver 1986, 1990, 1994; Vallin and Meslé 2001). We summarize mortality in this age range using 40q20, which is the probability that a person who survived to age 20 would die before age 60. It is not possible to estimate 40q20 by ethnicity on an annual basis because age distributions of population and deaths by ethnicity were tabulated only at the time of the census. Nonetheless, the available data allow us to calculate life tables by ethnicity that pertain to two-year periods, centered on each census date (1959, 1970, 1979, 1989, and 1999). We show estimates for the ethnic Kyrgyz and ethnic Russians for each census year since 1959. These are the only two ethnic groups that we can consistently follow throughout the period. Whenever possible, we present estimates for Russians and Ukrainians combined (the two most important Slavic groups in Kyrgyzstan), and for Kyrgyz and Uzbeks combined (the two most important central Asian ethnic groups). These estimates are shown in Fig. 1.
Fig. 1.
Probability of dying between ages 20 and 60 (40q20) by sex and ethnicity, Kyrgyzstan, 1959–1999. Rus/Ukr = Russians and Ukrainians combined; Kyr/Uzb = Kyrgyz and Uzbeks combined. Data are from authors’ calculations based on national census and vital registration data
Figure 1 shows that for males, the excess adult mortality of ethnic Russians is large and ubiquitous. The difference is established as early as 1959, the first year for which we have data. Strikingly, we find that although both Russian and Kyrgyz males experienced a mortality increase between 1989 and 1999, the increase was much larger among Russians. As a result, the mortality disadvantage of Russian males, which was already large in 1989, became even larger by 1999. For females, the levels of adult mortality were much lower than for males. Russian females exhibited a slight advantage in 1970–1989. Nonetheless, they lost this advantage by 1999, after experiencing some increase in mortality. The Russian mortality paradox, which prevails only among males during the Soviet period, is found among both males and females in 1999. Similar results are described by Guillot (2004, 2007).
The Relative Socioeconomic Status of Ethnic Russians in Central Asia
These mortality patterns are surprising because it is commonly believed that at least during the Soviet period, ethnic Russians living in central Asia have had higher socioeconomic status than titular ethnic groups. Indeed, Russians arrived in central Asia with the purpose of developing, modernizing, and industrializing the region and settled mostly in urban areas, while the indigenous populations retained their mostly rural and agricultural character. This pattern is moderated by the emergence, during the course of the twentieth century, of a highly educated, indigenous elite that was well represented in local political, social, economic, and cultural structures. However, on balance, it is believed that indigenous populations lagged behind in many respects during the Soviet period. Kahn, for example, showed that Russians (and, more generally, Slavs) are overrepresented in managerial positions (Kahn 1993). Poujol made a similar conclusion and even talked about a “European” versus “Indigenous” dichotomy, not unlike that observed in French Algeria or British India (Poujol 1995). Indeed, it would be surprising to discover that during the colonial period, the French in Algeria or the British in India were experiencing higher mortality than the native Algerians or Indians. As noted earlier, the difference is in the other direction for infant and child mortality, with Russians exhibiting lower mortality at these ages (Andreev et al. 1992). This difference is more in accordance with expectations, given patterns of social stratification in the area.
Survey data collected after the breakup of the Soviet Union confirm this mostly qualitative assessment of the relative socioeconomic status of Russians in the region. Indeed, poverty estimates by ethnicity based on the World Bank’s Multipurpose Poverty Surveys for Kyrgyzstan (KMPS), which are presented in Table 1, show a large and systematic advantage for the Russians. For all three dates at which poverty rates by ethnicity are calculated (1993, 1997, and 2005), the prevalence of poverty among ethnic Russians is substantially lower than among either ethnic Kyrgyz or ethnic Uzbeks. Moreover, the Russians’ relative advantage appears to grow over time. In 2005, the prevalence of poverty among the Kyrgyz was 4.7 times higher than among Russians.
Table 1.
Percentage of individuals below the poverty line, by ethnicity of the household head, Kyrgyzstan: World Bank poverty surveys, 1993–2005
| Ethnicity | Year
|
||
|---|---|---|---|
| 1993 | 1997 | 2005 | |
| Russian (%) | 28.6 | 16.8 | 10.0 |
| Kyrgyz (%) | 52.7 | 60.0 | 46.9 |
| Uzbek (%) | 39.4 | 53.3 | 55.5 |
| Total (%) | 45.0 | 51.0 | 43.1 |
Notes: The poverty line is calculated using an absolute poverty approach, based on a minimum subsistence basket. Households are assigned to poverty categories on the basis of their expenditures. For more details, see Ackland and Falkingham (1997:85).
Sources: For 1993, Ackland and Falkingham (1997:90, Table 5.3). For 1997, World Bank (1999:10, Table 7). For 2005, World Bank (2007:15, Table 1.8).
We complement this description of ethnic differences in standards of living by presenting estimates of median per capita expenditures by ethnicity for the age group 20–59, our age range of interest; and for 1998, the survey year that is closest to the most recent mortality estimate in Fig. 1. These median values, shown in Table 2, are much higher among Russians, illustrating here also their higher standards of living. The difference holds when we consider urban and rural areas separately. This implies that differences in standards of living between Russians and Kyrgyz or Uzbeks are not an artifact of their greater propensity to live in urban areas.
Table 2.
Median per capita yearly expenditures of individuals aged 20–59, by ethnicity and urban/rural residence, Kyrgyzstan, both sexes combined, 1998 (in Soms)
| Ethnicity | Residence
|
||
|---|---|---|---|
| Urban | Rural | Total | |
| (1) Russian | 38,563 | 25,298 | 32,061 |
| (2) Kyrgyz or Uzbek | 23,810 | 8,667 | 9,852 |
| Ratio (1) / (2) | 1.62 | 2.92 | 3.25 |
Note: All expenditures are in Soms, the national currency of the Kyrgyz Republic.
Source: Authors’ calculations based on the 1998 Kyrgyzstan Poverty Monitoring Survey.
In light of these data, the advantageous material situation of ethnic Russians in Kyrgyzstan compared with the native ethnic groups is unambiguous. Their higher recorded mortality thus appears paradoxical. Indeed, in populations around the world, subgroups with higher socioeconomic status tend to experience lower mortality. We term this situation the “Russian mortality paradox” (Guillot 2007). (In the United States, the term “Hispanic mortality paradox” is used to refer to the lower mortality of Hispanics compared with non-Hispanics whites, in spite of the lower socioeconomic status of Hispanics; Palloni and Arias 2004.)
Three Explanations for the Russian Mortality Paradox
In this study, we evaluate three relevant explanations for the Russian mortality paradox: (1) data artifacts, (2) migration effects, and (3) cultural effects.
Data Artifacts
Age-specific mortality rates by ethnicity, which are the basic quantities producing the ethnic differences in 40q20 shown in Fig. 1, are subject to a number of possible data errors. These possible errors include incompleteness of the death information, incompleteness of the population information, age-reporting errors, and inconsistent reporting of ethnicity in the population and death information. To the extent that these errors are large and vary substantially by ethnicity, the size and direction of the reported ethnic difference in mortality may be affected. Among possible errors, differential completeness of the death information between Russians and central Asians is perhaps the most commonly cited. If indeed completeness of deaths was lower among central Asian ethnic groups, their mortality could appear spuriously lower than that of Russians. Dobrovolskaya (1990) raised the possibility that death undercount among titular nationalities in central Asia explains their lower e5 values in 1978–1979. Sinelnikov (1988) believed that death registration at older ages is likely to be inadequate among central Asians because of the Islamic tradition that the deceased should be buried on the day of the death, before sunset, which makes it difficult to obtain a death certificate on time. After the deceased is buried, the incentive to obtain a death certificate may be lessened (Sinelnikov 1988:130). Although not referring specifically to the Russian mortality paradox, Anderson and Silver (1997) also believed that there is large undercount of deaths in central Asian republics during the Soviet period. While they stressed the problems at infant and older ages, they also argued that the reported mortality rates in the age range 20–59 are too low, especially among males and in rural areas where the indigenous ethnic groups predominantly live. Although the data quality explanation is commonly raised and plausible, no conclusive evidence has been presented showing that it is the main explanation for the observed patterns.
Migration Effects
It is well known that migrants tend to be a healthier subset of their origin population. This can produce mortality levels among migrants that are relatively lower than among nonmigrants in the place of origin as well as in the place of destination, a phenomenon that has been termed the “healthy migrant effect.” This explanation is of little help for explaining the direction of the ethnic difference in Kyrgyzstan because in this case, it is the migrants—that is, the Russians—who have been experiencing excess mortality. However, the healthy migrant effect could be invoked for explaining the large increase in mortality among ethnic Russians between 1989 and 1999, contrasting with the small changes among ethnic Kyrgyz. Indeed, during that period, one-third of Kyrgyzstan’s ethnic Russian population left the country. These migration flows would affect reported mortality trends among Russians if those who left were healthier than those who stayed. To our knowledge, this explanation has not been raised for explaining patterns of ethnicity-specific mortality in central Asia. However, there exists a wide literature on the healthy migrant effect in the case of Hispanics in the United States (Abraido-Lanza et al. 1999; Franzini et al. 2001; Hummer et al. 2007; Markides and Eschbach 2005; Palloni and Morenoff 2001).
Cultural Effects
Cultural practices can have an impact on mortality through two main pathways. The first pathway involves health behaviors such as diet, smoking, and alcohol consumption. These health behaviors are closely related to cultural practices and have well-established consequences for health and mortality, especially smoking and alcohol. The second pathway involves social support and social integration, which are also related to culture to the extent that individuals’ ability to participate in social networks and derive social, emotional, and material support from these linkages is related to norms and beliefs about family relationships and obligations (Mendes de Leon and Glass 2004). Different cultural practices among ethnic groups could thus play a role in explaining observed mortality differences. (The cultural hypothesis has often been proposed for explaining the Hispanic mortality paradox, although it is not well supported by evidence; Palloni and Arias 2004.) Among the cultural characteristics that have been invoked for explaining the higher mortality of Russians, authors have mentioned the possibility that central Asians, for cultural or religious reasons, have lower levels of alcohol consumption than Russians (Andreev et al. 1992; Darsky and Andreev 1991). Here also, no conclusive evidence has been presented.
Although all three explanations are plausible, the literature offers no definite answer about their relative role in the paradoxical excess mortality of Russians in central Asia. In the remainder of this study, we take advantage of newly available data from Kyrgyzstan to contribute to this debate. These data, which we obtained directly from NSC, include unpublished, detailed tabulations of population, deaths, and migrations for the period 1959–1999. The data used in this analysis also include aggregate population counts from the 1999 census, and aggregate counts of deaths from vital registers for 1998–1999, which were derived for the purpose of this analysis from the individual-level databases located at NSC. The level of aggregation that we use is thus finer than that of unpublished tables routinely calculated by NSC. These data, which for the most part have never been analyzed, provide us with relevant information for examining the Russian mortality paradox in Kyrgyzstan.
Data Artifacts
It is not possible to estimate the completeness of deaths by ethnicity for past decades using classic intercensal methods because deaths and migrants by ethnicity are not available on an annual basis. We are also unable to estimate the completeness of deaths at ages 20–59 because migration at these ages is large relative to mortality, which makes it difficult to distinguish errors in death registration from errors in migration registration. However, the available data allow us to estimate the completeness of death registration at ages 65 and older, by urban/rural residence. Although these data refer to a different age range than the one we focus on, they give valuable information about patterns of registration completeness in the country. In fact, completeness at ages 65 and older may be interpreted as conservative estimates of completeness at ages 20–59 because underregistration is typically more severe at older ages than at adult ages in the former Soviet Union and elsewhere (Anderson and Silver 1986, 1990, 1994).
For each intercensal period (1959–1970–1970–1979–1979–1989–1989–1999), we estimate the number of intercensal deaths among cohorts aged 65 and older at the beginning of the period, using two successive censuses and the number of registered in-migrants and out-migrants during the intercensal period (i.e., population at the first census minus population at the second census plus intercensal in-migrants minus intercensal out-migrants). We then compare these estimated intercensal deaths with the corresponding registered deaths by calculating the ratio of registered versus estimated deaths. Privileging census information over registration information—an approach that has been often used in the former Soviet Union, for example, for assessing the completeness of birth registration (Coale et al. 1979; Jones and Grupp 1983)—this ratio can be interpreted as an estimate of death registration completeness at ages 65 and older. Results are shown in Table 3.
Table 3.
Estimates of death registration completeness for cohorts aged 65 and older at the beginning of each intercensal period, by sex and urban/rural residence, Kyrgyzstan, 1959–1999
| Intercensal Period | Males
|
Females
|
||||
|---|---|---|---|---|---|---|
| Urban Areas (%) | Rural Areas (%) | Total (%) | Urban Areas (%) | Rural Areas (%) | Total (%) | |
| 1959–1970 | 95.9 | 49.1 | 58.9 | 90.8 | 40.6 | 51.9 |
| 1970–1979 | 96.4 | 83.4 | 87.2 | 86.7 | 68.4 | 74.2 |
| 1979–1989 | 94.6 | 86.8 | 89.5 | 87.7 | 79.0 | 82.3 |
| 1989–1999 | 91.7 | 97.8 | 95.2 | 86.1 | 93.9 | 90.4 |
Source: Authors’ calculations based on national census and vital registration data.
The completeness estimates presented in Table 3 increase our confidence that the observed ethnic differences in mortality are real, especially during the later part of the 1959–1999 period, for the following reasons. First, completeness in rural areas, where the large majority of the Kyrgyz live, has dramatically improved over time and caught up with urban areas by the end of the Soviet period, yet the recorded excess mortality of Russians at the national level has not diminished. On the contrary, it is highest in 1999, at a time where we do not find evidence for lower completeness in rural areas. Second, the estimates in Table 3 show no evidence for a decline in completeness since the breakup of the Soviet Union, yet the recorded excess mortality of Russians increased substantially between 1989 and 1999. Third, completeness among males has been consistently higher than among females, yet the excess mortality of Russians is primarily found among males.
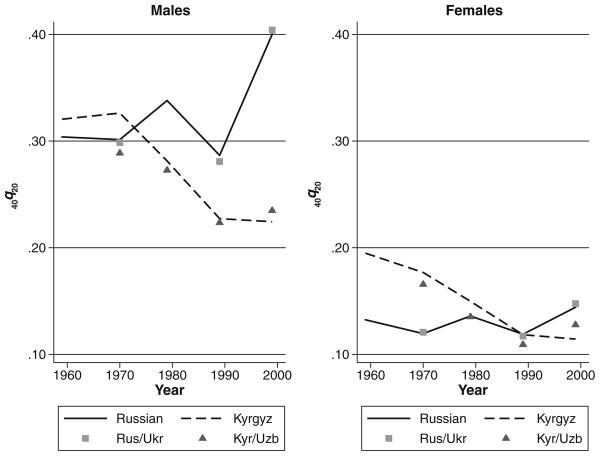
Another piece of evidence in support of the reality of the excess mortality of adult Russians in recent decades is presented in Fig. 2, which shows recorded estimates of 40q20 by sex and ethnicity in urban areas only. These estimates of urban mortality are informative because completeness in urban areas has been consistently high since 1959, as shown in Table 3. If the recorded excess mortality of Russians was produced by data artifacts, it would disappear (or be substantially diminished) in urban areas, where the data can be regarded with more confidence. Figure 2 shows that although this is the case during the earlier part of the period (1959–1970 for males and 1959 for females), the excess mortality of Russians persists in the urban data during the later part of the period (1979–1999 for males and 1999 for females). Also, the pattern of mortality divergence observed in 1989–1999 at the national level for both males and females remains strikingly pronounced in the urban data. This suggests that while underregistration in rural areas could explain the recorded excess mortality of Russians at the national level during the earlier part of the period (1959–1970 for males and 1959 for females), it fails to explain the existence of this excess mortality during the later part of the period (1979–1999 for males and 1999 for females), and also fails to explain the increase in Russian excess mortality between 1989 and 1999 for both males and females.
Fig. 2.
Probability of dying between ages 20 and 60 (40q20) by sex and ethnicity, Kyrgyzstan, 1959–1999, Urban areas. Rus/Ukr = Russians and Ukrainians combined; Kyr/Uzb = Kyrgyz and Uzbeks combined. Data are from authors’ calculations based on national census and vital registration data
Another possible source of error is the so-called numerator/denominator bias, which arises from inconsistent reporting of ethnicity in exposure (population) and death data, producing biased estimates of ethnicity-specific mortality rates. Because the numerators of mortality rates come from death certificates, where ethnicity is based on official passport information—whereas denominators come from census records, where ethnicity is self-reported—it is possible that an individual who declares a certain ethnicity in the census appears to have a different ethnicity on a death certificate. This problem can be particularly acute for individuals with mixed ancestry who are more likely to have complex ethnic identities. (Only one ethnicity can be reported on a death certificate or census record.) Although there is some degree of intermarriage among Slavic ethnic groups and among central Asian ethnic groups, ethnically mixed marriages that cross the central Asian versus Slavic line have been very rare in central Asia (Gorenburg 2006). Therefore, possible numerator/denominator inconsistencies are likely to be largely addressed after detailed ethnic groups are merged into broader central Asian versus Slavic groups. To address these potential numerator/denominator inconsistencies, we calculated mortality indicators for ethnic Russians and Ukrainians combined and for ethnic Kyrgyz and Uzbeks combined. Figures 1 and 2 show that this merging of ethnic groups does not alter the patterns described earlier.
Overall, results from this section suggest that although the Kyrgyz data are not free of errors, these errors fail to explain the existence of the Russian mortality paradox during the later part of the period (i.e., 1979–1999 for males and 1999 for females) and fail to explain the mortality divergence between Russians and Kyrgyz observed among males and females between 1989 and 1999.
Migration Effects
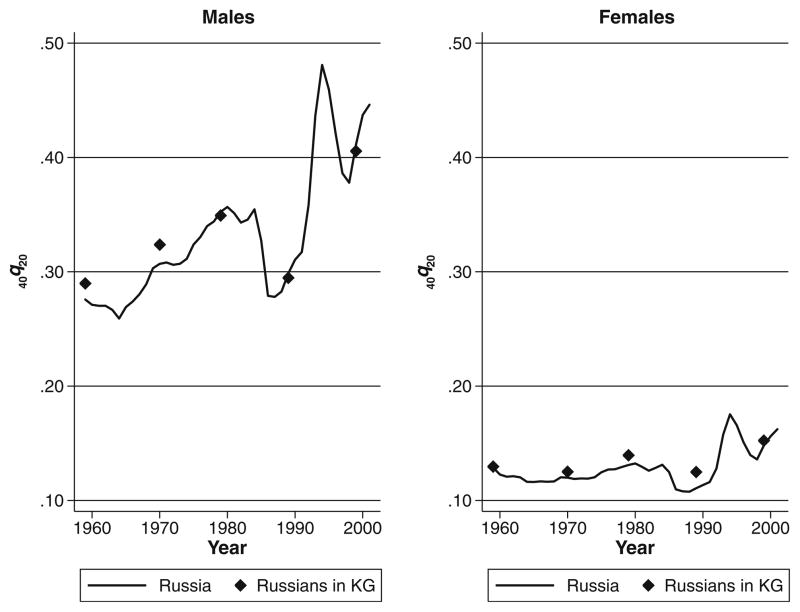
To evaluate the migration effect hypothesis, we compare levels of adult mortality among Russians living in Kyrgyzstan with those recorded in Russia. If migration of ethnic Russians from Russia to Kyrgyzstan was selective, we would expect the mortality levels of Russians in Kyrgyzstan to be different from the levels recorded in Russia. In particular, according to the healthy migrant hypothesis, we would expect mortality levels among Russians living in Kyrgyzstan to be somewhat lower than the levels recorded in Russia during the earlier part of the period, at the time when ethnic Russians were migrating to central Asia in large numbers. Similarly, if the Russians who left Kyrgyzstan en masse after 1991 were healthier than those who remained in Kyrgyzstan, we would expect this selective migration to have a detrimental impact on mortality trends among the Russians in Kyrgyzstan. In the context of increasing adult mortality in both Russia and Kyrgyzstan, we would expect migration effects to produce larger mortality increases among Russians living in Kyrgyzstan than in Russia, where mortality increases have been real and not explained in terms of selective migration (Leon et al. 1997).
Figure 3 shows levels of 40q20 by sex for Russians living in Kyrgyzstan (census years only) and Russia (annually). This figure shows that throughout the period, levels of adult mortality among Russians living in Kyrgyzstan have been strikingly similar to those recorded in Russia. The similarity holds for both males and females and suggests that selection may not be the main explanation for the observed mortality levels and trends among Russians in Kyrgyzstan. For the 1989–1999 period, in particular, it suggests that Russians, whether living in Russia or in Kyrgyzstan, are subject to comparable—and real—mortality increases.
Fig. 3.
Probability of dying between ages 20 and 60 (40q20) by sex, Russia (annually) and ethnic Russians in Kyrgyzstan (KG) (in census years), 1959–1999. Data for Russia are from the Human Mortality Database (www.mortality.org), and data for ethnic Russians in Kyrgyzstan (KG) are from authors’ calculations based on national census and vital registration data
Cultural Effects
We evaluate the “cultural effects” hypothesis indirectly, by examining causes of death among ethnic groups. The strategy is to examine whether the causes of death that explain the observed ethnic differences can be tied to the cultural practices of the corresponding ethnic groups.
Ideally, we would like to examine the causes of death that explain both the amount of ethnic difference in mortality and the change over time in this difference, especially between 1989 and 1999, when the difference increased substantially for both males and females. Unfortunately, cause-specific deaths by ethnicity were never tabulated by NSC. The only time period for which we are able to calculate cause-specific mortality rates by ethnicity is 1998–1999, thanks to the existence of a database containing electronic records of the original death certificates for these years. Combining these death registration data with the 1999 census data (for exposure), we are able to calculate mortality rates by age, sex, cause, and ethnicity for the two-year period centered at the 1999 census. We compare two ethnic groups: “Slavic,” which includes Russians, Ukrainians, and Belorussians; and “central Asian,” which includes the five titular central Asian ethnic groups (Kyrgyz, Uzbeks, Kazakhs, Tajiks, and Turkmen). (The existence of the microdata in 1998–1999 allows us to use here a slightly more inclusive—but not substantively different—merging of ethnic groups than the one presented in earlier figures.) For these ethnic groups, we compare age-standardized cause-specific mortality rates at ages 20–59. We use the WHO European standard for the age standardization. These mortality rates are based on about 2.2 million individual census records and 20,000 individual death certificates. Results are shown in Table 4 for males and Table 5 for females.
Table 4.
Age-standardized death rate (per 100,000) at ages 20–59 (40M20) for males, by ethnicity and cause of death, Kyrgyzstan, 1998–1999
| Cause of Death | Slavic (1) | Central Asian (2) | Difference (1) – (2) | % Difference | Ratio (1) / (2) |
|---|---|---|---|---|---|
| All Causes | 1,290.3 | 677.6 | 612.7 | 100.0 | 1.90 |
| Infectious and Parasitic Diseases | 101.0 | 43.9 | 57.1 | 9.3 | 2.30 |
| Neoplasms | 150.2 | 71.3 | 78.9 | 12.9 | 2.11 |
| Diseases of the Circulatory System | 374.4 | 253.4 | 121.0 | 19.7 | 1.48 |
| Diseases of the Respiratory System | 84.9 | 63.3 | 21.6 | 3.5 | 1.34 |
| Diseases of the Digestive System | 93.6 | 68.7 | 24.9 | 4.1 | 1.36 |
| External Causes | 403.6 | 118.7 | 284.9 | 46.5 | 3.40 |
| Other Causes | 82.8 | 58.3 | 24.5 | 4.0 | 1.42 |
| Detailed Infectious and Parasitic Diseases | |||||
| Tuberculosis | 94.8 | 38.3 | 56.5 | 9.2 | 2.48 |
| Other infectious and parasitic diseases | 6.2 | 5.6 | 0.6 | 0.1 | 1.11 |
| Detailed Neoplasms | |||||
| Upper aerodigestive tract cancer | 14.5 | 8.6 | 5.9 | 1.0 | 1.69 |
| Stomach cancer | 22.1 | 22.8 | −0.7 | −0.1 | 0.97 |
| Colorectal cancer | 12.3 | 2.4 | 9.9 | 1.6 | 5.13 |
| Other digestive cancer | 17.6 | 9.8 | 7.8 | 1.3 | 1.80 |
| Trachea, bronchus, and lung cancer | 37.9 | 12.0 | 25.9 | 4.2 | 3.16 |
| Breast cancer | 0.0 | 0.4 | −0.4 | −0.1 | 0.00 |
| Cancer of unspecified sites | 9.9 | 2.4 | 7.5 | 1.2 | 4.13 |
| Other neoplasms | 36.0 | 12.9 | 23.1 | 3.8 | 2.79 |
| Detailed Circulatory Diseases | |||||
| Myocardial infarction | 58.2 | 39.1 | 19.1 | 3.1 | 1.49 |
| Atherosclerotic heart disease | 102.3 | 41.9 | 60.4 | 9.9 | 2.44 |
| Other forms of acute and chronic ischemia | 51.6 | 21.7 | 29.9 | 4.9 | 2.38 |
| Other heart diseases, nonmyocardial | 36.8 | 12.8 | 24.0 | 3.9 | 2.88 |
| Cerebrovascular disease | 100.2 | 112.8 | −12.6 | −2.1 | 0.89 |
| Other circulatory diseases | 25.2 | 25.2 | 0.0 | 0.0 | 1.00 |
| Detailed External Causes | |||||
| Transport accidents | 36.8 | 20.4 | 16.4 | 2.7 | 1.80 |
| Accidental poisoning by alcohol | 67.9 | 3.5 | 64.4 | 10.5 | 19.40 |
| Other accidental poisoning | 34.8 | 4.9 | 29.9 | 4.9 | 7.10 |
| Other accidental causes | 39.1 | 22.1 | 17.0 | 2.8 | 1.77 |
| Suicides | 77.4 | 19.6 | 57.8 | 9.4 | 3.95 |
| Homicides | 45.4 | 11.5 | 33.9 | 5.5 | 3.95 |
| Injury of undetermined intent | 55.5 | 14.1 | 41.4 | 6.8 | 3.94 |
| Other injuries | 46.6 | 22.7 | 23.9 | 3.9 | 2.05 |
| Causes Directly Related to Alcohola | 86.1 | 6.1 | 80.0 | 13.1 | 14.11 |
Notes: “Central Asian” includes ethnic Kyrgyz, Uzbeks, Kazakhs, Tajiks, and Turkmens. “Slavic” includes ethnic Russians, Ukrainians, and Belorussians. Rates and percentages may not always add up to totals due to rounding.
Source: Authors’ calculations based on national census and vital registration data.
Alcohol poisoning, alcohol cirrhosis of the liver, alcohol psychosis, and chronic alcoholism.
Table 5.
Age-standardized death rate (per 100,000) at ages 20–59 (40M20) for females, by ethnicity and cause of death, Kyrgyzstan, 1998–1999
| Cause of Death | Slavic (1) | Central Asian (2) | Difference (1) – (2) | % Difference | Ratio (1) / (2) |
|---|---|---|---|---|---|
| All Causes | 414.4 | 350.4 | 64.0 | 100.0 | 1.18 |
| Infectious and Parasitic Diseases | 12.4 | 17.2 | −4.8 | −7.5 | 0.72 |
| Neoplasms | 107.6 | 53.1 | 54.5 | 85.2 | 2.03 |
| Diseases of the Circulatory System | 129.6 | 150.1 | −20.5 | −32.0 | 0.86 |
| Diseases of the Respiratory System | 17.8 | 27.9 | −10.1 | −15.8 | 0.64 |
| Diseases of the Digestive System | 30.6 | 34.8 | −4.2 | −6.6 | 0.88 |
| External Causes | 80.7 | 25.0 | 55.7 | 87.0 | 3.23 |
| Other Causes | 35.7 | 42.3 | −6.6 | −10.3 | 0.84 |
| Detailed Infectious and Parasitic Diseases | |||||
| Tuberculosis | 9.2 | 13.9 | −4.7 | −7.3 | 0.66 |
| Other infectious and parasitic diseases | 3.2 | 3.3 | −0.1 | −0.2 | 0.97 |
| Detailed Neoplasms | |||||
| Upper aerodigestive tract cancer | 0.9 | 3.3 | −2.4 | −3.8 | 0.27 |
| Stomach cancer | 12.0 | 12.4 | −0.4 | −0.6 | 0.97 |
| Colorectal cancer | 7.7 | 1.8 | 5.9 | 9.2 | 4.28 |
| Other digestive cancer | 9.8 | 6.9 | 2.9 | 4.5 | 1.42 |
| Trachea, bronchus, and lung cancer | 5.2 | 1.8 | 3.4 | 5.3 | 2.89 |
| Breast cancer | 23.6 | 7.6 | 16.0 | 25.0 | 3.11 |
| Female genital organ cancers | 24.3 | 9.4 | 14.9 | 23.3 | 2.59 |
| Cancer of unspecified sites | 7.0 | 2.0 | 5.0 | 7.8 | 3.50 |
| Other neoplasms | 17.3 | 8.1 | 9.2 | 14.4 | 2.14 |
| Detailed Circulatory Diseases | |||||
| Myocardial infarction | 9.2 | 7.4 | 1.8 | 2.8 | 1.24 |
| Atherosclerotic heart disease | 24.6 | 19.5 | 5.1 | 8.0 | 1.26 |
| Other forms of acute and chronic ischemia | 14.8 | 6.6 | 8.2 | 12.8 | 2.24 |
| Other heart diseases, nonmyocardial | 10.3 | 8.2 | 2.1 | 3.3 | 1.26 |
| Cerebrovascular disease | 57.7 | 81.4 | −23.7 | −37.0 | 0.71 |
| Other circulatory diseases | 13.1 | 27.0 | −13.9 | −21.7 | 0.49 |
| Detailed External Causes: | |||||
| Transport accidents | 8.5 | 5.5 | 3.0 | 4.7 | 1.55 |
| Accidental poisoning by alcohol | 16.0 | 0.6 | 15.4 | 24.1 | 26.67 |
| Other accidental poisoning | 10.6 | 2.0 | 8.6 | 13.4 | 5.30 |
| Other accidental causes | 7.5 | 3.2 | 4.3 | 6.7 | 2.34 |
| Suicides | 8.8 | 3.7 | 5.1 | 8.0 | 2.38 |
| Homicides | 13.1 | 2.6 | 10.5 | 16.4 | 5.04 |
| Injury of undetermined intent | 10.0 | 4.0 | 6.0 | 9.4 | 2.50 |
| Other injuries | 6.1 | 3.6 | 2.5 | 3.9 | 1.69 |
| Causes Directly Related to Alcohola | 21.6 | 0.8 | 20.8 | 32.5 | 27.00 |
Notes: “Central Asian” includes ethnic Kyrgyz, Uzbeks, Kazakhs, Tajiks, and Turkmens. “Slavic” includes ethnic Russians, Ukrainians, and Belorussians. Rates and percentages may not always sum to totals because of rounding.
Source: Authors’ calculations based on national census and vital registration data.
Alcohol poisoning, alcohol cirrhosis of the liver, alcohol psychosis, and chronic alcoholism.
For males, age-standardized mortality rates are higher among Slavs for all seven major causes shown in the top part of Table 4. However, the size of the difference varies substantially by cause. The biggest difference is for external causes, for which the age-standardized death rate is more than three times higher among Slavs. This represents an absolute difference of 284.9 deaths per 100,000—that is, almost one-half (46.5%) of the total difference in the age-standardized mortality rate between Slavs and central Asians in this age range. Other causes that explain a substantial portion of the difference are circulatory diseases (19.7%), neoplasms (12.9%), and infectious diseases (9.3%). However, these contributions are much lower than that of external causes, which clearly stand out as the largest contributor to the ethnic difference in adult mortality.
Because external causes play such an important role, we calculated the age-standardized mortality rate for the most important detailed causes within that broad category (bottom part of Table 4). It appears that for males, within the external causes category, accidental poisoning by alcohol is the cause with the largest absolute and relative ethnic difference. The age-standardized mortality rate for that detailed cause is more than 19 times larger among Slavs. The absolute difference in the rate for that cause alone represents 10.5% of the ethnic difference. Accidental poisoning by alcohol is the classic cause for coding deaths attributable to alcohol abuse in the former Soviet Union. Among the 187 elementary causes of death in the cause-of-death classification of Kyrgyzstan (which is similar to the one used in Russia at that time), this cause is the one with the largest ethnic difference. The other external cause that plays an important role is suicide, which alone explains 9.4% of the total difference.
There are other detailed causes, situated in other broad categories besides external causes, which play a role in the ethnic difference. Within the circulatory diseases category, heart diseases other than myocardial infarction—namely, atherosclerotic heart disease, “other forms of acute and chronic ischemia,” and “other heart diseases, nonmyocardial” contribute 9.9%, 4.9%, and 3.9%, respectively. Myocardial infarction plays a smaller role, explaining 3.1% of the difference. Mortality rates from cerebrovascular diseases are actually higher among central Asians and thus contribute negatively to the difference. A number of cancers contribute to the ethnic differences. Among them, the category for trachea, bronchus, and lung cancer stands out, contributing 4.2% of the total difference. Tuberculosis (TB) clearly dominates within the infectious diseases category. While rates of tuberculosis are high for both Slavs and central Asians, the rate is more than twice higher among Slavs, and this cause alone explains 9.2% of the ethnic difference.
The picture that emerges from this analysis of detailed causes is one in which the ethnic difference between Slavic and central Asian males is driven by (1) external causes (46.5%), especially alcohol poisoning and suicides; (2) nonmyocardial heart diseases (18.7%); and (3) tuberculosis (9.2%). These conditions explain 74.4% of the ethnic difference. Interestingly, external causes and nonmyocardial heart diseases were the main contributors of fluctuations in adult mortality rates in Russia in the 1990s (Zaridze et al. 2009b), and various studies have shown that in Russia, these conditions are strongly related to alcohol intake (Gavrilova et al. 2005; Leon et al. 2007; Pridemore 2002, 2004; Ramstedt 2009; Zaridze et al. 2009a, b). In a case-control study of adult deaths in three cities of Western Siberia, Zaridze et al. (2009a) found that causes that appear to be most strongly related to alcohol intake are accidents and violence (confirming results by Gavrilova et al. 2005), alcohol poisoning, and acute ischemic heart diseases other than myocardial infarction. On the basis of this study and an earlier study using autopsy data (Zaridze et al. 2009a, b), they concluded that many alcohol-related deaths are wrongly attributed to diseases of the circulatory system, especially to heart diseases other than myocardial infarction. In Kyrgyzstan, heart diseases other than myocardial infarction explain most of the ethnic difference from circulatory diseases (114.3 out of a difference of 121.0 per 100,000). As for TB, Zaridze et al. (2009a) also found this cause of death to be strongly related to alcohol intake in Russia. This may be explained in part by specific social mixing patterns associated with alcohol intake (Lönnroth et al. 2008), especially prison exposure (Bobrik et al. 2005). Indeed, there is a well-established link between alcohol and violent crime on one hand (Gavrilova et al. 2005; Pridemore 2002, 2004), and between prison exposure and TB transmission on the other hand, in Russia and other former Soviet republics (Bobrik et al. 2005; Coninx et al. 2000; Stern 1999).
In brief, the cause-of-death data presented in Table 4 strongly suggest that alcohol is a major determinant of the ethnic difference between Slavic and central Asian males in Kyrgyzstan. Not only is the difference particularly large for causes directly related to alcohol (a narrow definition that includes alcohol poisoning, alcohol cirrhosis, alcohol psychosis, and chronic alcoholism, and which represents 13.1% of the total difference, as shown at the bottom of Table 4), but it is disproportionally large for a number of causes that have been shown to be strongly related to alcohol intake in the study by Zaridze and his colleagues: namely, external causes, nonmyocardial heart diseases, and TB. These causes explain 74.4% of the ethnic difference. This percentage increases to 79.8% if we take into account all the causes defined in the Zaridze et al. study as “strongly alcohol-related causes” (Zaridze et al. 2009a:2211). The contribution of trachea, bronchus, and lung cancers (explaining 4.2% of the total ethnic difference) suggests that tobacco also plays some role, albeit in a much smaller proportion.
As mentioned earlier, females experience much lower levels of adult mortality than males in 1998–1999, and a much smaller ethnic difference. Examining broad causes of death in the top part of Table 5, we find that mortality is, in fact, lower among Slavic females than among central Asian females for most causes. The two exceptions are external causes and neoplasms. Mortality from external causes is more than three times higher among Slavic females, and the absolute difference of 55.7 per 100,000 represents 87.0% of the total ethnic difference of 64.0 per 100,000. Neoplasms also play an important role in the excess mortality of Slavic females, with an absolute difference of 54.5 per 100,000, or 85.2% of the total ethnic difference. Together, external causes and neoplasms add up to an excess mortality among Slavic females of 110.2 per 100,000, but then their lower mortality for all the other broad causes of death reduces the mortality difference for all causes combined to 64.0 per 100,000.
As in the case of males, mortality from external causes appear as the top contributor to the ethnic difference for females. Information on detailed external causes (bottom part of Table 5) shows that here also, accidental poisoning by alcohol is the external cause with the largest contribution. This cause alone represents 24.1% of the total ethnic difference in mortality. Homicides (16.4%) and “other accidental poisoning” (13.4%) also play an important role. The importance of external causes—and among them, accidental alcohol poisoning—suggests that alcohol is an important factor in the ethnic difference for females as well. In fact, 32.5% of the total difference is explained by causes directly related to alcohol, as shown at the bottom of Table 5.
The alcohol hypothesis for females is further supported by data on detailed circulatory causes. While mortality from circulatory diseases is on the whole lower among Slavic females, there is in fact excess mortality from heart diseases, especially for nonmyocardial heart diseases. The difference is particularly high for “other forms of acute and chronic ischemia,” a cause that may hide many deaths from excessive alcohol intake, as discussed earlier (Zaridze et al. 2009b). On the other hand, the difference is much lower for myocardial infarction, and it is in the other direction for cerebrovascular and other circulatory diseases. These circulatory causes have been less directly linked to alcohol intake than non-myocardial heart diseases.
Detailed information on neoplasms shows that for females, there are some other important factors to consider besides alcohol. Mortality rates are higher among Slavic females for breast cancer and female genital organ cancers, diseases that are not clearly related to alcohol consumption, although one study claims an elevated risk for breast cancer (Smith-Warner et al. 1998). This ethnic difference may be related in part to lower fertility levels among Slavic females.
Interestingly, mortality is lower among Slavic females for upper aerodigestive tract cancer and tuberculosis, two causes that were found to be related to alcohol intake in the Zaridze et al. study (2009a). Little can be learned from the upper aerodigestive tract cancer results because they are based on only three Slavic deaths and 27 central Asian deaths from that cause in 1998–1999. As for the lower rate of TB among Slavic females, this pattern may be explained by the fact that excessive alcohol consumption may be less associated with violent crime, and thus with prison exposure, for women than for men. Therefore, for women, Slavic versus central Asian mortality rates from TB may better reflect underlying patterns of socioeconomic differences, providing Slavic females with an advantage. (The impact of dimensions of socioeconomic status on mortality from infectious and other diseases will be discussed in the next section.)
The two major determinants of the excess mortality among Slavic females thus appear to be alcohol and cancers. It is difficult to determine which of these two main causes plays the most important role. However, given the importance of external causes and of nonmyocardial heart diseases, which together explain more of the difference than all neoplasms combined, it may be inferred that alcohol plays a more important role overall. If we take into account all the causes defined in the Zaridze et al. study as “strongly alcohol-related” (Zaridze et al. 2009a:2211), these causes explain 54.9 per 100,000, or 85.8% of the difference.
We conclude from this analysis that although various causes of death contribute to the excess mortality among Slavic males and females, alcohol emerges as a major determinant, especially for males. This empirical finding confirms Darsky and Andreev (1991) and Andreev et al.’s (1992) hypothesis that the lower levels of mortality observed among central Asian ethnic groups in the former Soviet Union are explained to a large extent by their lower levels of alcohol consumption.
Multivariate Analysis of Adult Mortality
The importance of personal behaviors, such as alcohol consumption, in explaining mortality differences between Slavs and central Asians supports the “cultural” hypothesis because, as we will discuss later, such behaviors seem related to cultural and religious practices among the different ethnic groups in Kyrgyzstan. However, Slavs and central Asians differ in many other dimensions, some of which are related to their mortality outcomes. For example, Slavs and central Asians have different patterns of urban/rural residence, with Slavs predominantly living in urban areas and central Asians predominantly living in rural areas. If, for example, alcoholism were a mostly urban phenomenon, different patterns of urban/rural residence among Slavs and central Asians would confound the ethnic mortality comparisons performed in the earlier section. Also, Slavs and central Asians have different patterns of educational attainment: Slavs, especially females, exhibit higher levels of educational attainment. The lower levels of mortality observed for most broad causes among Slavic females (including TB, as discussed earlier) may be explained in part by this educational advantage. Ethnic differences in mortality from neoplasms may be also related to residential and educational differences between Slavs and central Asians.
In this section, we take advantage of information on urban/rural residence and educational attainment, which is available on both census records and death certificates, to carry out finer comparisons of mortality by ethnicity. The purpose is not to draw a comprehensive explanatory model of the factors associated with mortality among ethnic groups. (Because death records cannot be linked to census records at the individual level, we can examine only a limited number of variables that exist in both sources.) Rather, the goal is to improve the comparisons of ethnic groups by taking account of these two variables that are strongly related to both ethnicity and mortality.
We conduct a multivariate analysis in which mortality by sex and cause is predicted as a function of age, ethnicity, residence, and education. We model mortality using negative binomial regression, instead of the more common Poisson regression, because the hypothesis that the mortality data are Poisson-distributed is rejected for mortality from all causes and external causes for males. We start with a simple model, Model 1, that includes only age and ethnicity as explanatory variables:
| (1) |
where Dij is the number of deaths in age group i and ethnic group j; Nij is the number of person-years of exposure at age i and ethnic group j; Xi is a dummy variable indicating membership in age group i; Xj is a dummy variable indicating membership in ethnic group j; εij is an error term whose exponential is gamma distributed; and βi and βj are coefficients indicating the estimated effect of the variables on mortality.
Models are estimated separately for deaths from all causes and deaths by major cause (seven categories). Death counts are for the period 1998–1999, and the exposure term is estimated using population counts at the 1999 census. We use eight 5-year age groups (from 20–24 to 55–59), and three ethnic categories (Slavic, central Asian, and other). Each model is estimated separately for males and females.
We then estimate a second model, in which we add urban/rural residence and education (with three categories: higher/incomplete higher, secondary/secondary special, and below secondary/unknown) as explanatory variables. We are particularly interested in comparing the effect of ethnicity in this model (Model 2) with the effect of ethnicity in Model 1, where mortality is predicted as a function of age and ethnicity only. This comparison is shown in Table 6, which presents risk ratios for Slavs, using central Asians as the reference category.
Table 6.
Slavic/central Asian risk ratio of mortality at ages 20–59, for all causes and by cause, Kyrgyzstan, 1998–1999
| Cause of Death | Males
|
Females
|
||
|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | |
| All Causes | 2.18*** | 1.94*** | 1.30*** | 1.31*** |
| Infectious and Parasitic Diseases | 2.27*** | 1.75*** | 0.70* | 0.77 |
| Neoplasms | 2.01*** | 2.06*** | 1.99*** | 1.95*** |
| Diseases of the Circulatory System | 1.75*** | 1.70*** | 1.03 | 1.07 |
| Diseases of the Respiratory System | 1.71*** | 1.56*** | 0.66* | 0.77 |
| Diseases of the Digestive System | 1.48*** | 1.40*** | 0.95 | 1.02 |
| External Causes | 3.12*** | 2.71*** | 2.74*** | 2.56*** |
| Other Causes | 1.56*** | 1.44*** | 0.84 | 0.92 |
Notes: Each cell in the table corresponds to a different model with different combinations of outcome and explanatory variables. Model 1 controls for age in addition to ethnicity; Model 2 controls for age, residence, and education in addition to ethnicity. See the text for details.
p ≤ .05;
p ≤ .01;
p ≤ .001
For males, results from Model 1 confirm the patterns discussed earlier. Excess mortality among Slavic males is particularly large for external causes (with a risk ratio of 3.12). Model 2 shows that the effect of ethnicity decreases after we control for residence and education. The decrease, however, is small. Risk ratios remain high and highly significant, especially for external causes. This means that the excess mortality observed among Slavic males is not merely the product of differences in patterns of urban/rural residence and education by ethnicity.
For females, Model 1 confirms the advantage Slavic females have for infectious diseases and respiratory diseases. However, this advantage disappears after we control for residence and education. This implies that the lower rates of infections and respiratory diseases among Slavic females are explained by their higher educational attainment and their urban residence. (Coefficients not shown in Table 6 indicate that higher education is associated with lower mortality from these two broad causes and that urban residence is related to lower mortality from respiratory diseases.) However, for neoplasms and external causes, and for all causes combined, where Slavic females have a disadvantage, the effect of ethnicity remains strong after we control for residence and education.
These results provide further evidence for the cultural hypothesis, although many important factors related to ethnicity, most notably income, are missing from Model 2. Nonetheless, ethnicity effects appear very robust, and it is unlikely that income would diminish these effects for causes of death where Slavs experience higher mortality because income, a variable typically associated with lower mortality, tends to be higher among Slavs, as discussed earlier.
Discussion
We find that excess mortality among adult Russians in Kyrgyzstan is not likely due to data artifacts or migration effects. Instead, we find that it is real and explained by important ethnic differences in cause-specific mortality. Although many causes of death contribute to the observed differences, we find that alcohol is a major determinant, especially for males. These differences are unexplained by education or residence.
We emphasize the role of culture because the personal behaviors that appear to generate a large part of the existing mortality differences in 1998–1999 seem to be closely tied to cultural practices. Patterns of alcohol consumption, in particular, are known to be closely related to culture (Heath 1995). The “culture of alcohol” among Russians (or, more generally, among Slavs) is a specific set of practices that involves binge drinking of hard liquors (vodka, in particular), and that is an inherent part of many social rituals, such as birthdays, weddings, and other celebrations (Cockerham 2000). This contrasts with central Asians, for whom alcohol consumption is a much less inherent part of social rituals and for whom the social stigma attached to drunkenness appears to be greater (Cockerham et al. 2004). The extent to which this is due to the direct influence of Islam and its prohibition of alcohol consumption is not clear. Indeed, the influence of Islam on everyday life in contemporary Kyrgyzstan is relatively small. The ethnic Kyrgyz, a historically nomadic people, converted to Islam relatively late (sometimes as late as the nineteenth century) and have never closely followed Islam’s prohibition of alcohol (Olcott 1995; Rose 2002). Observance of religious practices is more prevalent among ethnic Uzbeks, a historically sedentary people who converted to Islam at the time of the Arab conquest in the eighth century. But even for them, prohibition of alcohol consumption has not been strongly observed (Roy 1997), in part because of the official Soviet policy of atheism. (Abstinence has regained some popularity among Uzbeks since the reemergence of religious freedom in the late 1980s.) Kyrgyz and Uzbeks have also been influenced to some extent by Russians and their drinking habits. However, whether for religious or cultural reasons, the practice of drinking hard liquors is not as central a feature of socializing among ethnic Kyrgyz or ethnic Uzbeks as it is among Russians. Survey data on patterns of alcohol consumption confirm that in central Asia, Muslims are less likely to be frequent drinkers than are non-Muslims (Cockerham et al. 2004).
Implications for Understanding the Health Crisis in Post-Soviet States
A puzzling pattern of mortality trends in central Asian republics is that the mortality increases recorded in these republics after the breakup of the Soviet Union have not been as severe as in Russia. For example, in Kyrgyzstan, life expectancy at birth (for both sexes) declined by 3.3 years between 1990 and 1995 (from 68.8 to 65.5 years), while in Russia during the same period, it declined by 4.6 years (from 69.3 to 64.7 years). Moreover, the gap in life expectancy between Russia and Kyrgyzstan has increased in recent years, at the advantage of Kyrgyzstan. Similar patterns have been observed in the other central Asian republics. This is puzzling to many observers because the economic crisis has been more severe in central Asian republics. In 1990, the gross national income per capita in Russia was about 6.5 times greater than in Kyrgyzstan. In 2008, it was about 13 times greater (World Bank 2009). The “Russian mortality paradox,” which we observe when comparing ethnic Russians with ethnic Kyrgyz living in Kyrgyzstan, can be transposed at the national level: Russia, a much more developed country than Kyrgyzstan, exhibits lower life expectancy.
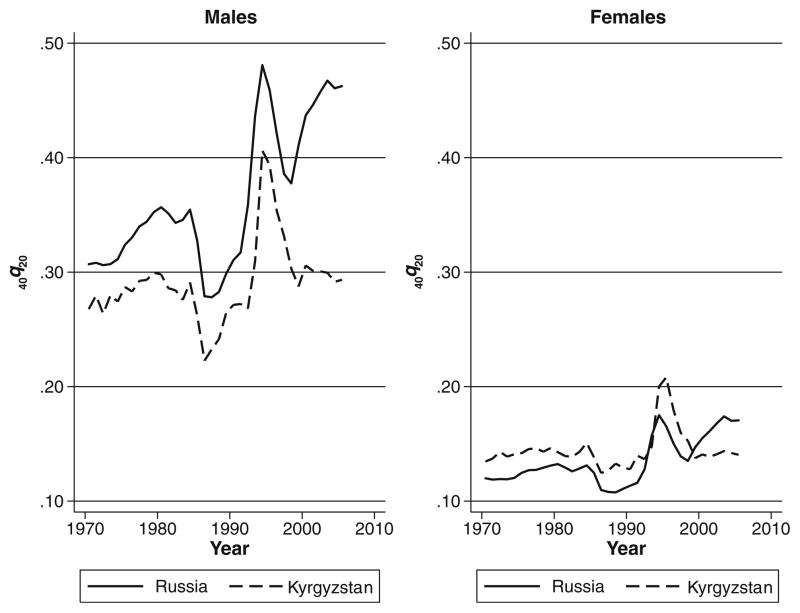
As in the case of ethnic differences, a deterioration of data quality problems in central Asian republics is often invoked as a possible explanation for this divergence (Becker et al. 1998). Indeed, a deterioration in the completeness of death registration in central Asia since 1991 would produce mortality trends that are more favorable than in reality. However, the divergence remains when looking specifically at mortality between ages 20 and 60: that is, ages at which we believe the quality of the mortality data has not deteriorated since 1991. (Note that the conclusion is different for infant and child ages. At these ages, there is evidence for data quality deterioration since 1991 (Guillot 2007; Guillot and Lim 2009).) Figure 4 shows trends in 40q20 in Russia and Kyrgyzstan. Except for the fact that this figure displays annual data and therefore shows the important mortality fluctuations of the 1980s and 1990s, patterns of adult mortality in Kyrgyzstan versus Russia are similar, both in terms of levels and trends, to the patterns of adult mortality among ethnic Kyrgyz versus ethnic Russians in Kyrgyzstan. In particular, the mortality divergence between Russia and Kyrgyzstan at adult ages is similar to the divergence that we established between ethnic Russians and ethnic Kyrgyz living in Kyrgyzstan. It is interesting to note also that the amount of fluctuation in adult mortality in the late 1980s and then in the 1990s, although large in both countries, was smaller in Kyrgyzstan.
Fig. 4.
Probability of dying between ages 20 and 60 (40q20) by sex, Kyrgyzstan and Russia, 1970–2005. Data for Russia are from the Human Mortality Database (www.mortality.org), and data for Kyrgyzstan are from authors’ calculations based on national population and vital registration information
Our analysis emphasizes the role of culture in explaining this divergence at the national level. The differential evolution of adult mortality among ethnic groups in Kyrgyzstan since 1989, and the causes of death responsible for the mortality differences in 1998–1999, illustrate that the health crisis in post-Soviet states is likely to be highly context, culture, or ethnicity specific. As a result, the republics that have fared worse economically may not necessarily be the ones with the largest mortality increases. Cultural characteristics are likely to play an important role in amplifying or buffering the impact of socioeconomic changes in the post-Soviet context.
A major cultural characteristic explaining the different evolution of mortality in post-Soviet states is likely to be the presence or not of a “culture of alcohol,” such as the one prevalent among Russians. Ethnic groups among whom this “culture of alcohol” is more prevalent and republics where these ethnic groups represent a greater proportion of the population have indeed experienced larger mortality increases than ethnic groups and republics for which this cultural characteristic is less prevalent (Brainerd 1998), regardless of the respective evolution of the material conditions of these populations. It is well established that alcohol is a major determinant of the mortality fluctuations in Russia (Brainerd and Cutler 2005; Cockerham 1999; McKee et al. 2001; Shkolnikov et al. 2001; Zaridze et al. 2009a, b). Alcohol, however, is often viewed as a proximate determinant of mortality, while economic factors (such as unemployment resulting from mass privatization) and social disruption are identified as the actual underlying forces that have induced the observed mortality increases (Cornia and Paniccia 1995; Leon and Shkolnikov 1998; Leon et al. 2007, 2009; Shapiro 1995; Shkolnikov et al. 1998; Stuckler et al. 2009). Indeed, fluctuations in mortality in Russia, for which alcohol has been identified as a major cause, appear to coincide with the economic and social upheavals of the 1990s (Zaridze et al. 2009a). This framework does not explain well why adult mortality has been lower and has not increased as much in a country like Kyrgyzstan, which underwent similar social and economic upheavals. In a different line of research, Cockerham (1999, 2000) and Cockerham et al. (2004, 2006) saw alcohol consumption in former Soviet republics as largely shaped by societal norms, rather than induced by psychological distress. The cultural dimension of alcohol intake does not appear well when examining mortality fluctuations in Russia alone because obviously one cannot explain rapid mortality fluctuations with a cultural factor that presumably does not vary quickly over time. The interethnic and interrepublic comparisons presented in this study suggest that mortality fluctuations in post-Soviet states may be viewed largely as the product of an interaction between socioeconomic upheavals and the existence of an underlying culture of alcohol.
Acknowledgments
This research was supported by grants from the National Institute of Child Health and Human Development (R03-HD38752 and R01-HD045531). The authors thank Zarylbek Kudabaev, former chairman of the National Statistical Committee of the Kyrgyz Republic, and Orozmat Abdykalykov, its current chairman, for giving us access to much of the data used in this article; and Liudmila Torgashova, Larissa Mimbaeva, and Elena Komandirova for supervising the data collection in Kyrgyzstan. Anonymous reviewers provided helpful comments on earlier versions of this article.
Contributor Information
Michel Guillot, Email: miguillo@sas.upenn.edu, Population Studies Center, University of Pennsylvania, 3718 Locust Walk, Philadelphia, PA 19104, USA.
Natalia Gavrilova, Center on Aging, NORC/University of Chicago, Chicago, IL, USA.
Tetyana Pudrovska, Population Research Center, University of Texas, Austin, TX, USA.
References
- Abraido-Lanza AF, Dohrenwend BP, Ng-Mak DS, Turner JB. The Latino mortality paradox: A test of the “salmon bias” and healthy migrant hypotheses. American Journal of Public Health. 1999;89:1543–1548. doi: 10.2105/ajph.89.10.1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ackland R, Falkingham J. A profile of poverty in Kygyzstan. In: Falkingham J, Klugman J, Marnie S, Micklewright J, editors. Household welfare in central Asia. Houndmills, Basingstoke [England]: Macmillan Press; New York: St. Martin’s Press; 1997. pp. 81–99. [Google Scholar]
- Anderson BA, Silver BD. Sex differentials in mortality in the Soviet Union: Regional differences in length of working life in comparative perspective. Population Studies. 1986;40:191–214. [Google Scholar]
- Anderson BA, Silver BD. Trends in mortality of the Soviet population. Soviet Economy. 1990;6:191–251. [PubMed] [Google Scholar]
- Anderson BA, Silver BD. Mortality trends in the working ages: Soviet regions in comparative perspective. In: Lutz W, Scherbov S, Volkov A, editors. Demographic trends and patterns in the Soviet Union before 1991. London, UK: Routledge; 1994. pp. 295–338. [Google Scholar]
- Anderson BA, Silver BD. Issues of data quality in assessing mortality trends and levels in the new independent states. In: Bobadilla JL, Costello CA, Mitchell F, editors. Premature death in the new independent state. Washington, DC: National Academy Press; 1997. pp. 120–155. [Google Scholar]
- Andreev EM, Dobrovolskaya VM, Shaburov KY. Etnicheskaya differentsiatsiya smertnosti [Ethnic mortality differentials] Sotsiologicheskie Issledovaniya. 1992;1992(7):43–49. [Google Scholar]
- Becker CM, Bibosunova DI, Holmes GE, Ibragimova MM. Maternal care vs. economic wealth and the health of newborns: Bishkek, Kyrgyz Republic and Kansas City, USA. World Development. 1998;11:2057–2072. [Google Scholar]
- Bobrik A, Danishevski K, Eroshina K, McKee M. Prison health in Russia: The larger picture. Journal of Public Health Policy. 2005;26:30–59. doi: 10.1057/palgrave.jphp.3200002. [DOI] [PubMed] [Google Scholar]
- Brainerd R. Market reform and mortality in transitions economics. World Development. 1998;26:2013–2027. [Google Scholar]
- Brainerd E, Cutler DM. Autopsy on an empire: Understanding mortality in Russia and the former Soviet Union. The Journal of Economic Perspectives. 2005;19:107–130. [Google Scholar]
- Coale AJ, Anderson BA, Härm E. Human fertility in Russia since the nineteenth century. Princeton, NJ: Princeton University Press; 1979. [Google Scholar]
- Cockerham WC. Health and social change in Russia and Eastern Europe. London, UK: Routledge; 1999. [Google Scholar]
- Cockerham WC. Health lifestyles in Russia. Social Science & Medicine. 2000;51:1313–1324. doi: 10.1016/s0277-9536(00)00094-0. [DOI] [PubMed] [Google Scholar]
- Cockerham WC, Hinote BP, Abbott P. Psychological distress, gender, and health lifestyles in Belarus, Kazakhstan, Russia, and Ukraine. Social Science & Medicine. 2006;63:2381–2394. doi: 10.1016/j.socscimed.2006.06.001. [DOI] [PubMed] [Google Scholar]
- Cockerham WC, Hinote BP, Abbott P, Haerpfer C. Health lifestyles in central Asia: The case of Kazakhstan and Kyrgyzstan. Social Science & Medicine. 2004;59:1409–1421. doi: 10.1016/j.socscimed.2004.01.023. [DOI] [PubMed] [Google Scholar]
- Coninx R, Maher D, Reyes H, Grzemska M. Tuberculosis in prisons in countries with high prevalence. British Medical Journal. 2000;320:440–442. doi: 10.1136/bmj.320.7232.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornia AG, Paniccia R. Innocenti Occasional Papers—Economic Policy Studies No. 49. Florence, Italy: UNICEF; 1995. The demographic impact of sudden impoverishment: Eastern Europe during the 1989–1994 transition. [Google Scholar]
- Darsky L, Andreev E. Vosproizvodstvo naseleniya otdel’nykh natsional’nostei v SSSR [Population growth among different nationalities in the USSR] Vestnik Statistiki. 1991;6:3–10. [PubMed] [Google Scholar]
- Dobrovolskaya VM. Etnicheskaya differentsiatsiya smertnosti [Ethnic differentials in mortality] In: Volkov AG, editor. Demograficheskie protsessy v SSSR [Demographic processes in the USSR] Moscow, Russia: Nauka; 1990. pp. 150–166. [Google Scholar]
- Franzini L, Ribble JC, Keddie AM. Understanding the Hispanic paradox. Ethnicity and Disease. 2001;11:496–518. [PubMed] [Google Scholar]
- Gavrilova NS, Gavrilov LA, Semyonova VG, Evdokushkina GN, Ivanova AE. Patterns of violent crime in Russia. In: Pridemore WA, editor. Ruling Russia: Law, crime, and justice in a changing society. Boulder, CO: Rowman & Littlefield Publishers, Inc; 2005. pp. 117–145. [Google Scholar]
- Gorenburg D. Rethinking interethnic marriage in the Soviet Union. Post-Soviet Affairs. 2006;22:145–165. [Google Scholar]
- Guillot M. Kachestvo Demograficheskikh Dannykh v Kyrgyzstane c 1958 g [The quality of demographic data in Kyrgyzstan since 1958] In: Kudabaev ZI, Guillot M, Denisenko M, editors. Naselenie Kyrgyzstana [The population of Kyrgyzstan] Bishkek, Kyrgyz Republic: Natsional’ny Statistichesky Komitet Kyrgyzkoy Respubliki; 2004. pp. 53–76. [Google Scholar]
- Guillot M. Mortality in Kyrgyzstan since 1959: Real patterns and data artifacts. Espace-Populations-Sociétés. 2007;1:113–126. [Google Scholar]
- Guillot M, Lim S. Infant mortality in Kyrgyzstan before and after the break-up of the Soviet Union. Paper presented at the annual meetings of the Population Association of America; Detroit, MI. 2009. May, [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heath DB, editor. International handbook on alcohol and culture. Westport, CT: Greenwood Press; 1995. [Google Scholar]
- Hummer RA, Powers DA, Pullum SG, Gossman GL, Frisbie WP. Paradox found (again): Infant mortality among the Mexican-origin population in the United States. Demography. 2007;44:441–457. doi: 10.1353/dem.2007.0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones E, Grupp FW. Infant mortality trends in the Soviet Union. Population and Development Review. 1983;9:213–246. [Google Scholar]
- Kahn M. Les Russes Dans les ex-Républiques Soviétiques. Le Courrier des Pays de l’Est. 1993;376:3–20. [Google Scholar]
- Leon DA, Chenet L, Shkolnikov VM, Zakharov S, Shapiro J, Rakhmanova G, …McKee M. Huge variation in Russian mortality rates 1984–94: Artefact, alcohol, or what? Lancet. 1997;350:383–388. doi: 10.1016/S0140-6736(97)03360-6. [DOI] [PubMed] [Google Scholar]
- Leon DA, Saburova L, Tomkins S, Andreev E, Kiryanov N, McKee M, Shkolnikov VM. Hazardous alcohol drinking and premature mortality in Russia: A population based case-control study. Lancet. 2007;369:2001–2009. doi: 10.1016/S0140-6736(07)60941-6. [DOI] [PubMed] [Google Scholar]
- Leon DA, Shkolnikov VM. Social stress and the Russian mortality crisis. Journal of the American Medical Association. 1998;11:790–791. doi: 10.1001/jama.279.10.790. [DOI] [PubMed] [Google Scholar]
- Leon DA, Shkolnikov VM, McKee M. Alcohol and Russian mortality: A continuing crisis. Addiction. 2009;104:1630–1636. doi: 10.1111/j.1360-0443.2009.02655.x. [DOI] [PubMed] [Google Scholar]
- Lönnroth K, Williams BG, Stadlin S, Jaramillo E, Dye C. Alcohol use as a risk factor for tuberculosis—A systematic review. BMC Public Health. 2008;8:289. doi: 10.1186/1471-2458-8-289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markides KS, Eschbach K. Aging, migration and mortality: Current status of research on the Hispanic paradox. Journals of Gerontology: Series B. 2005;60B(Special Issue II):68–75. doi: 10.1093/geronb/60.special_issue_2.s68. [DOI] [PubMed] [Google Scholar]
- McKee M, Shkolnikov VM, Leon DA. Alcohol is implicated in the fluctuations in cardiovascular disease in Russia since the 1980s. Annals of Epidemiology. 2001;11:1–6. doi: 10.1016/s1047-2797(00)00080-6. [DOI] [PubMed] [Google Scholar]
- Mendes de Leon CF, Glass TA. The role of social and personal resources in ethnic disparities in late life health. In: Anderson NB, Bulatao RA, Cohen B, editors. Critical perspectives on racial and ethnic differences in health in late life. Washington, DC: National Academies Press; 2004. pp. 353–405. [PubMed] [Google Scholar]
- Olcott MB. Islam and fundamentalism in independent central Asia. In: Ro’i Y, editor. Muslim Eurasia: Conflicting legacies. Portland, OR: F. Cass; 1995. pp. 21–40. [Google Scholar]
- Palloni A, Arias E. Paradox lost: Explaining the Hispanic adult mortality advantage. Demography. 2004;41:385–416. doi: 10.1353/dem.2004.0024. [DOI] [PubMed] [Google Scholar]
- Palloni A, Morenoff J. Interpreting the paradoxical in the “Hispanic Paradox”: Demographic and epidemiological approaches. In: Weinstein M, Hermalin A, Stoto M, editors. Population health and aging. New York: New York Academy of Sciences; 2001. pp. 140–174. [DOI] [PubMed] [Google Scholar]
- Poujol C. Minorites exogènes ou Russes de l’intérieur en Asie Centrale [Exogenous minorities or indigenous Russians in Central Asia] Revue d’Etudes Comparatives Est-Ouest. 1995;26(4):125–142. [Google Scholar]
- Pridemore WA. Vodka and violence: Alcohol consumption and homicide rates in Russia. American Journal of Public Health. 2002;92:1921–1930. doi: 10.2105/ajph.92.12.1921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pridemore WA. Weekend effects on binge drinking and homicide: The social connection between alcohol and violence in Russia. Addiction. 2004;99:1034–1041. doi: 10.1111/j.1360-0443.2004.00762.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramstedt M. Fluctuations in male ischaemic heart disease mortality in Russia 1959–1998: Assessing the importance of alcohol. Drug and Alcohol Review. 2009;28:390–395. doi: 10.1111/j.1465-3362.2009.00059.x. [DOI] [PubMed] [Google Scholar]
- Rose R. How Muslims view democracy: Evidence from central Asia. Journal of Democracy. 2002;13(4):102–111. [Google Scholar]
- Roy O. La nouvelle Asie centrale ou la fabrication des nations [The new central Asia or the making of nations] Paris, France: Editions du Seuil; 1997. [Google Scholar]
- Shapiro J. The Russian mortality crisis and its causes. In: Aslund A, editor. Russian economic reforms at risk. London, UK: Pinter; 1995. pp. 149–178. [Google Scholar]
- Shkolnikov VM, Cornia GA, Leon DA, Meslé F. Causes of the Russian mortality crisis. World Development. 1998;26:1995–2011. [Google Scholar]
- Shkolnikov VM, McKee M, Leon DA. Changes in life expectancy in Russia in the mid-1990s. Lancet. 2001;357:917–921. doi: 10.1016/S0140-6736(00)04212-4. [DOI] [PubMed] [Google Scholar]
- Sinelnikov AB. Dinamika urovnia smernosti v SSSR [The dynamics of the level of mortality in the USSR] In: Rybakovskii LL, editor. Naselenie SSSR za 70 let [The population of the USSR in the last 70 years] Moscow, Russia: Nauka; 1988. pp. 115–133. [Google Scholar]
- Smith-Warner SA, Spiegelman D, Yaun SS, van den Brandt PA, Folsom AR, Goldbohm RA, Hunter DJ. Alcohol and breast cancer in women: A pooled analysis of cohort studies. Journal of the American Medical Association. 1998;279:535–540. doi: 10.1001/jama.279.7.535. [DOI] [PubMed] [Google Scholar]
- Stern V, editor. Sentenced to die? The problem of TB in prisons in eastern Europe and central Asia. London, UK: Kings College; 1999. [Google Scholar]
- Stuckler D, King L, McKee M. Mass privatization and the post-communist mortality crisis: A cross-national analysis. Lancet. 2009;373:399–407. doi: 10.1016/S0140-6736(09)60005-2. [DOI] [PubMed] [Google Scholar]
- Vallin J, Meslé F. Trends in mortality and differential mortality. Strasbourg, France: Council of Europe Publishing; 2001. Trends in mortality in Europe since 1950: Age-, sex-, and cause-specific mortality; pp. 31–186. [Google Scholar]
- World Bank. Kyrgyz republic: Update on poverty in the Kyrgyz Republic (Report No. 19425-KG) Washington, DC: World Bank; 1999. [Google Scholar]
- World Bank. Kyrgyz Republic poverty assessment (Report No. 40864-KG) Washington, DC: World Bank; 2007. [Google Scholar]
- World Bank. World development indicators 2008. Washington, DC: World Bank; 2009. [Google Scholar]
- Zaridze D, Brennan P, Boreham J, Boroda A, Karpov R, Lazarev A, …Peto R. Alcohol and cause-specific mortality in Russia: A retrospective case-control study of 48,557 adult deaths. Lancet. 2009a;373:2201–2214. doi: 10.1016/S0140-6736(09)61034-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaridze D, Maximovitch D, Lazarev A, Igitov V, Boroda A, Boreham J, …Boffetta P. Alcohol poisoning is a main determinant of recent mortality trends in Russia: Evidence from a detailed analysis of mortality statistics and autopsies. International Journal of Epidemiology. 2009b;38:143–153. doi: 10.1093/ije/dyn160. [DOI] [PubMed] [Google Scholar]