Abstract
Objective
The purpose of this case report is to describe a patient with an L5/S1 posterior surgical fusion who presented to a chiropractic clinic with subsequent low back and leg pain and was treated with Cox decompression manipulation.
Clinical Features
A 55-year-old male postal clerk presented to a private chiropractic practice with complaints of pain and spasms in his low back radiating down the right buttock and leg. His pain was a 5 of 10, and Oswestry Disability Index score was 18%. The patient reported a previous surgical fusion at L5/S1 for a grade 2 spondylolytic spondylolisthesis. Radiographs revealed surgical hardware extending through the pedicles of L5 and S1, fusing the posterior arches.
Intervention and Outcome
Treatment consisted of ultrasound, electric stimulation, and Cox decompression manipulation (flexion distraction) to the low back. After 13 treatments, the patient had a complete resolution of his symptoms with a pain score of 0 of 10 and an Oswestry score of 2%. A 2-year follow-up revealed continued resolution of the patient's symptoms.
Conclusions
Cox chiropractic decompression manipulation may be an option for patients with back pain subsequent to spinal fusion. More research is needed to verify these results.
Key indexing terms: Spinal fusion; Lumbar vertebrae; Spondylolisthesis; Manipulation, spinal; Chiropractic
Introduction
In the past 20 to 30 years, lumbar fusion has been considered a standard surgical treatment of conditions such as spondylolisthesis and degenerative disk disease.1 However, there is some geographic discrepancy regarding the necessity of back surgery, with the rate of back surgery in the United States at least 40% higher than that in any other country and more than 5 times higher than the rates in England and Scotland.2 Even within the US borders, the South and Midwest regions have higher proportions of surgical fusions than other part of the United States,3 ranging in average costs per surgery from $24 405 in the Northeast US to $40 157 in the West.3
Given the high rates of spinal surgery in the United States and the associated costs, there still remains very little evidence in favor of surgical spinal fusion for back conditions.4,5 Of the 4 clinical trials that have attempted to compare surgical fusion with nonoperative care for chronic low back pain, only 1 study appeared to provide some evidence in favor of fusion, with the other studies failing to corroborate this finding.5 Furthermore, in the clinical trial that reported positive results with fusion, only 16% had excellent outcomes compared with 6% in the nonoperative group,6 demonstrating a small difference in outcomes that lacks clinical relevance.
To complicate the matter further, a recent prospective study reported that 59.4% of subjects who underwent thoracic and/or lumbar spine surgery experienced at least 1 complication, with 24.2% being major complications such as deep wound infection or death.7
There are serious issues surrounding spinal surgery for back pain, and the patients who are not helped by the surgical procedures may seek postsurgical conservative care. A 1994 study assessed the rate of patients with at least 1 spinal surgery who attended 1 of 12 chiropractic clinics in 6 different states.8 The postsurgical rate of chiropractic attendance was 3.75%, demonstrating the fact that postsurgical cases are not a rarity in the chiropractic office. The purpose of this case report is to describe a patient with an L5/S1 posterior surgical fusion who presented to a chiropractic clinic with subsequent low back and leg pain and was successfully treated with Cox decompression manipulation.
Case report
A 55-year-old male postal clerk presented to a private chiropractic office with acute, severe pain in his low back radiating down his right buttock, thigh, and leg. The pain began 2 days prior approximately 30 to 40 minutes after playing golf. He described the pain as constant and interfering with his work, daily routine, recreation, and walking. He rated his average pain in his back and right leg as a 5 on the visual analog pain scale of 0 (no pain) to 10 (worst pain imaginable), with the pain being more severe in the morning. His Oswestry Disability Index9,10 was scored at 18% disability (minimal) during the initial visit. He denied any lower extremity weakness, tingling, or numbness, or any changes in bowel or bladder control. The pain was worse with walking, most markedly when walking up or down an incline, and was described as a deep ache. He stated that over-the-counter anti-inflammatory medication helped reduce the severity of his pain. His medical history was significant for a spinal fusion at the L5/S1 level approximately 2 years prior. Before the lumbar fusion, he was treated by a different chiropractor on an as-needed basis. However, because of the unremitting nature of his pain and the severity of the grade 2 L5/S1 spondylolytic spondylolisthesis, the posterior fusion was performed with pedicle screws.
This patient was an otherwise healthy 55-year-old man measuring 5′11″ and weighing 164 lb. Visualization revealed a normal gait; however, his movements were guarded, and he was in obvious pain getting up and down from a seated position. He presented with a mild left lateral antalgia. Palpation revealed tenderness and hypertonicity of the lumbar spine erector muscles and gluteal muscles most markedly on the right. Lumbosacral ranges of motion included flexion at 35°, extension 15°, rotation 10° bilaterally, right lateral bending 10°, and left lateral bending 15°, all causing some increase in low back discomfort.
Moderate tenderness was noted at the L4/5 and L5/S1 levels, more markedly on the right. Straight leg raise was positive on the right at 40° and on the left at 50°, causing a significant increase in low back pain and moderate increase in right leg pain. Sensation to disposable pinwheel examination revealed mild hypoesthesia at the right L5 dermatome, otherwise normal bilaterally. The Achilles and patellar reflexes were found to be normal grade 2 bilaterally. Positive lumbar hyperextension causing pain was noted, as was the right Quadrant (Kemp) Test for an increase in lower back and leg pain. Lower extremity strength in all muscle groups was strong and was graded at a 5/5.
Lumbar spine radiographs included anterior-to-posterior (Fig 1), lateral neutral (Fig 2), lateral flexion (Fig 3), and lateral extension (Fig 4) projections revealing sacral, pelvic, and hip unleveling that was high on the left in the coronal plane. Sagittal plane alignment demonstrated an anterolisthesis of L5 on S1 of slightly less than 50%. Surgical fusion devices were noted at the L5/S1 level to stabilize the spondylolytic spondylolisthesis. The surgical hardware extended through the pedicles of L5 and S1 and attached to plates affixed to the posterior arches at these levels. There was no loss of vertebral body height. The sacroiliac joints and hips were normal, and soft tissue abnormalities were not apparent. It was noted that the surgical hardware was intact without any appearance of instability at that level.
Fig 1.

Anteroposterior view of lumbar spine showing pedicle screws and plates.
Fig 2.
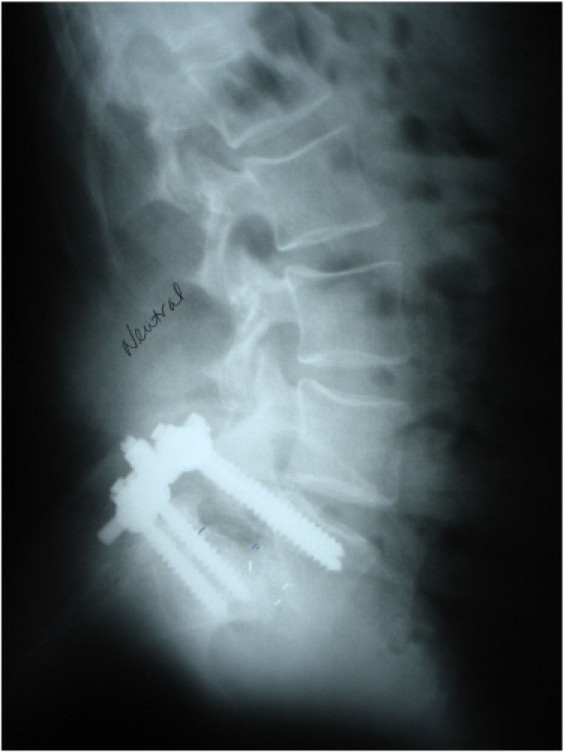
Neutral lateral view of lumbar spine demonstrating pedicle screws and plates.
Fig 3.

Lateral view of lumbar spine in flexion.
Fig 4.

Lateral view of lumbar spine in extension.
During the initial visit, physiotherapy modalities including ultrasound and attended electric stimulation were applied to the patient's low back. Cox decompression manipulation11 (Fig 5), also commonly known as flexion distraction, was instituted with the doctor contacting the spinous processes of the upper lumbar spine without additional distraction through utilization of ankle straps and included protocol 1 (3 sets of five 4-second pumps) while a small bolster was underneath the patient's waist. The patient was instructed to use a cold moist pack over the area for up to 15 minutes per waking hour and to return the next day. On his second visit the following day, acute care modalities were again performed, as was decompression manipulation to the lumbar spine without straps. On his third visit (day 3), the patient reported feeling approximately 50% better since his first treatment. Treatment was rendered; and this time, the ankle straps were applied to increase the total amount of decompressive force to the lumbar spine.
Fig 5.

Cox flexion distraction technique for the lumbar spine. (Color version of figure is available online.)
During the fifth visit (day 9), the patient was instructed to perform pelvic tilt and knee-to-chest exercises twice a day. The patient stated on his seventh visit (day 13) that prolonged standing at work caused some radiation of pain to the leg, but it was not as severe. On the eighth visit (day 16), the patient noted further progressive relief; and flexion distraction was performed using axial decompression manipulation with the ankle straps.
On his 10th visit (day 23), the patient reported feeling approximately 95% better with a full return to activities of daily living; and he was able to work without increased pain. This patient was treated a total of 13 times over a period of approximately 6 weeks, at which point he reported no pain, his objective findings were found to be normal, and his Oswestry Disability Index was graded as 2% disability. The patient was released from care and instructed to return if the low back or leg pain resumed.
The patient was contacted 2 years after his final treatment, at which point he reported that there were no further episodes of pain in the low back or leg and that he was very satisfied with the care he received.
Discussion
A spinal fusion alters the normal biomechanics of the spine, limiting motion at the fused levels. This loss of motion is compensated by an increase in motion at spinal levels above and below the fused site, resulting in a significant amount of additional force being placed on the adjacent facet joints12 and disks.1 The consequence of this additional force on those mobile segments is vertebral degeneration and is termed adjacent segment disease (ASD).1 This degeneration may result in instability and spondylolisthesis above the fused segment.13 Adjacent segment disease is one reason that positive results immediately following a posterior spinal fusion may diminish over time.
In a retrospective study of radiographic outcomes, adjacent segment disease was found in a significant number of patients who had lumbar or thoracolumbar fusion with pedicle screw instrumentation for degenerative disorders.1 The study included 188 patients at least 5 years after spinal fusion and determined both radiographic ASD and clinical ASD. Radiographic ASD occurred in 42.6% of the patients and was determined by radiographic evidence of degeneration including spondylolisthesis, segmental kyphosis, collapse of disk space, or worsening degeneration using the Weiner system of classification.14 Of the patients with radiographic ASD, 56% also had clinically significant ASD.1
The definition of clinical ASD, found in 30.3% of the patients in this study, included symptomatic spinal stenosis, intractable back pain, and subsequent sagittal or coronal imbalance.1 Although degeneration of the adjacent segment was found to occur both above and below the fused segment, it occurred most commonly cephalad to the fused segment (88.8%) and manifested primarily as spinal stenosis.1 New-onset mechanical back pain was found to occur more commonly when degeneration occurred caudal to the fused segment.1
A historical cohort study compared 725 nonsurgical low back pain cases with 725 cases of low back pain who subsequently underwent lumbar spinal fusion for diagnoses including disk herniation, disk degeneration, and/or radiculopathy.15 The authors determined that lumbar fusion cases were associated with a significant increase in disability, opiate use, prolonged work loss, and a poor return-to-work status. The surgical patients had a 36% complication rate and a 27% reoperation rate. A similar study that assessed 24 882 subjects who underwent surgical lumbar decompression or fusion found that the cumulative incidence of reoperation following fusion was 21.5%.16
One form of therapy that might be beneficial to postsurgical pain cases is Cox decompression manipulation. Decompression manipulation is considered a low-velocity, low-amplitude adjusting procedure and has been shown to create a decrease in intradiscal pressure, increase posterior disk height, and open the vertebral canal and intervertebral foramen by up to 28%.17 In a randomized clinical trial comparing decompression manipulation to physical therapy for chronic (nonsurgical) low back pain, patients with radiculopathy did significantly better with decompression treatment than with physical therapy.18 The statistically significant difference in treatment effects was maintained over a period of 1 year.19
Although Cox decompression manipulation has been documented to be effective for the treatment of chronic low back pain, the current case demonstrates that the technique along with physiotherapy modalities may also benefit postsurgical patients who have adjacent segment disease. When considering the complication rate of lumbar spinal fusion and the documented long-term sequela, Cox decompression manipulation may be a reasonable and viable option for the treatment of postsurgical pain patients.
Limitations
This study is not without limitations. First, these results are demonstrated in 1 single case and need to be verified in larger studies. And second, reduction of pain due to the natural history of the postsurgical condition cannot be ruled out.
Conclusion
Cox decompression manipulation may be an option for patients with back and leg pain subsequent to spinal fusion.
Funding sources and potential conflicts of interest
No funding sources or conflicts of interest were reported for this study.
References
- 1.Cheh G., Bridwell K.H., Lenke L.G., Buchowski J.M., Daubs M.D., Kim Y. Adjacent segment disease following lumbar/thoracolumbar fusion with pedicle screw instrumentation: a minimum 5-year follow-up. Spine. 2007;32(20):2253–2257. doi: 10.1097/BRS.0b013e31814b2d8e. [DOI] [PubMed] [Google Scholar]
- 2.Cherkin D.C., Deyo R.A., Loeser J.D., Bush T., Waddell G. An international comparison of back surgery rates. Spine. 1994;19(11):1201–1206. doi: 10.1097/00007632-199405310-00001. [DOI] [PubMed] [Google Scholar]
- 3.Cook C., Santos G.C., Lima R., Pietrobon R., Jacobs D.O., Richardson W. Geographic variation in lumbar fusion for degenerative disorders: 1990 to 2000. Spine J. 2007;7(5):552–557. doi: 10.1016/j.spinee.2006.09.010. [DOI] [PubMed] [Google Scholar]
- 4.Gibson J.A., Waddell G. Surgery for degenerative lumbar spondylosis. Cochrane Database Syst Rev. 2005;(Issue 4) doi: 10.1002/14651858.CD001352.pub3. Issue 4. Art. No.: CD001352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Don A.S., Carragee E. A brief overview of evidence-informed management of chronic low back pain with surgery. Spine J. 2008;8(1):258–265. doi: 10.1016/j.spinee.2007.10.027. [DOI] [PubMed] [Google Scholar]
- 6.Fritzell P., Hägg O., Wessberg P., Nordwall A., Swedish Lumbar Spine Study Group Lumbar fusion versus nonsurgical treatment for chronic low back pain: a multicenter randomized controlled trial from the Swedish Lumbar Spine Study Group. Spine. 2001;26(23):2521–2532. doi: 10.1097/00007632-200112010-00002. [DOI] [PubMed] [Google Scholar]
- 7.Campbell P.G., Malone J., Yadla S., Maltenfort M.G., Harrop J.S., Sharan A.D. Early complications related to approach in thoracic and lumbar spine surgery: a single center prospective study. World Neurosurg. 2010;73(4):395–401. doi: 10.1016/j.wneu.2010.01.024. [DOI] [PubMed] [Google Scholar]
- 8.Aspegren D.D., Burt A.L. A study of postspinal surgery cases in chiropractic offices. J Manipulative Physiol Ther. 1994;17(2):88–92. [PubMed] [Google Scholar]
- 9.Fairbank J.C.T., Pynsent P.B. The Oswestry Disability Index. Spine. 2000;25(22):2940–2953. doi: 10.1097/00007632-200011150-00017. [DOI] [PubMed] [Google Scholar]
- 10.Davidson M., Keating J. A comparison of five low back disability questionnaires: reliability and responsiveness. Physical Therapy. 2002;82:8–24. doi: 10.1093/ptj/82.1.8. [DOI] [PubMed] [Google Scholar]
- 11.Cox J.M. 6th ed. Lippincott Williams and Wilkins; Baltimore: 1999. Low back pain: mechanism, diagnosis, treatment. [Google Scholar]
- 12.Lee C.K., Langrana N.A. Lumbosacral spinal fusion. A biomechanical study. Spine. 1984;9(6):574–581. doi: 10.1097/00007632-198409000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Aota Y., Kumano K., Hirabayashi S. Postfusion instability at the adjacent segments after rigid pedicle screw fixation for degenerative lumbar spinal disorders. J Spinal Disord. 1995;8(6):464–473. [PubMed] [Google Scholar]
- 14.Weiner D.K., Distell B., Studenski S., Martinez S., Lomasney L., Bongiorni D. Does radiographic osteoarthritis correlate with flexibility of the lumbar spine? J Am Geriatr Soc. 1994;42:257–263. doi: 10.1111/j.1532-5415.1994.tb01748.x. [DOI] [PubMed] [Google Scholar]
- 15.Nguyen T.H., Randolph D.C., Talmage J., Succop P., Travis R. Long-term outcomes of lumbar fusion among workers' compensation subjects: an historical cohort study. Spine. 2011;36(4):320–331. doi: 10.1097/BRS.0b013e3181ccc220. [DOI] [PubMed] [Google Scholar]
- 16.Martin B.I., Mirza S.K., Comstock B.A., Gray D.T., Kreuter W., Deyo R.A. Reoperation rates following lumbar spine surgery and the influence of spinal fusion procedures. Spine. 2007;32(3):382–387. doi: 10.1097/01.brs.0000254104.55716.46. [DOI] [PubMed] [Google Scholar]
- 17.Cox J.M., Gudavalli M.R. Traction and distraction techniques. In: Haldeman S., Dagenais S., Budgell B., editors. Principles and practice of chiropractic. 3rd ed. McGraw-Hill; New York: 2005. pp. 821–840. [Google Scholar]
- 18.Gudavalli M.R., Cambron J.A., McGregor M., Jedlicka J., Keenum M., Ghanayem A.J. A randomized clinical trial and subgroup analysis to compare flexion-distraction with active exercise for chronic low back pain. Eur Spine J. 2006;15(7):1070–1082. doi: 10.1007/s00586-005-0021-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cambron J.A., Gudavalli M.R., McGregor M., Jedlicka J., Keenum M., Ghanayem A.J. Amount of health care and self-care following a randomized clinical trial comparing flexion-distraction with exercise program for chronic low back pain. Chiropr Osteopat. 2006;14:19. doi: 10.1186/1746-1340-14-19. [DOI] [PMC free article] [PubMed] [Google Scholar]


