Abstract
Objective
The purpose of this case study is to describe the effect of chiropractic care on a patient with chronic Bell's palsy.
Clinical Features
A 47-year-old woman with medically diagnosed Bell's palsy presented for chiropractic care. She had experienced right sinus pressure and congestion, lack of facial tone on the right, and intermittent tingling of the right side of her face.
Interventions and Outcomes
The patient received high-velocity, low-amplitude chiropractic manipulation (adjustments) to the cervical and thoracic spine, interferential muscle stimulation, and hydroculation on the trapezius muscles bilaterally. Reduction in symptoms occurred following the initial visit and continued over the next 9 weeks of care. After the course of a year of chiropractic care, the patient reached 90% improvement.
Conclusions
For this patient, chiropractic care reduced Bell's palsy symptoms.
Key indexing terms: Bell's palsy, Chiropractic
Introduction
Bell's palsy is a unilateral facial paralysis of sudden onset. Its cause is unknown but is believed to involve swelling of cranial nerve VII, or facial nerve, due to viral infection or immune disease. This swelling creates ischemia and compression of the nerve within the fallopian canal.1 Symptoms vary from mild weakness to total paralysis of one side of the face and can include, but is not limited to, drooping of the eyelid and corner of the mouth, dryness of the eye and/or mouth, and decreased sensation of taste.2 Bell's palsy is the most common cause of peripheral facial paralysis3,4 and accounts for more than 50% of all cases of facial paralysis.5 It affects approximately 40 000 Americans each year and afflicts men and women ages 15 to 60 years equally.2
The facial component of cranial nerve VII travels from its motor nucleus in the lower pons, past the olive and within the cerebellopontine angle. From there, it enters the internal acoustic meatus and travels through the facial canal in the petrous bone along with cranial nerve VIII and the labyrinthine artery. Here it is encased in a sheath of arachnoid-lined dura mater. After exiting the internal acoustic meatus, the facial nerve travels through the aqueductus fallopii in the temporal bone to its termination at the stylomastoid foramen. When it emerges from the stylomastoid foramen, the facial nerve travels forward to the ramus of the lower jaw where it divides into the temporofacial and cervicofacial branches.6,7
Many theories have been proposed and research projects performed to determine the etiology of Bell's palsy. The most widely accepted theory is that a viral infection causes the disorder. A Japanese research team suggests that Bell's palsy should be renamed herpetic facial paralysis after they found that only people with Bell's palsy have herpes simplex virus in the area around the geniculate ganglia of the human facial nerves.5 Another theory is based from the anatomical pathway the facial nerve travels and how it interacts with the structures along that pathway. For example, Blum6 reported that intracranial mechanical stress can affect cranial bones and meninges, which can lead to entrapment neuropathies. This is especially true of the facial nerve because of its relationship with the arachnoid and dura mater.
Although there is no standard course of treatment of Bell's palsy, chiropractic care has a potential role. The purpose of this case study is to describe the effect of chiropractic care of a patient with chronic Bell's palsy.
Case report
A 47-year-old woman presented to a chiropractic clinic in June 2009 with a complaint of sinus pressure and congestion on the right side due to Bell's palsy. The lateral canthus of her right eye and right corner of her mouth were noticeably drooping, and she reported an intermittent tingling sensation on the right side of her face. She stated that her sinus pressure and congestion were present every day and that they worsened with the onset of menses each month.
The patient's Bell's palsy started and was medically diagnosed in April 2004. At that time, she reported experiencing muscle spasms and lockjaw on the right side of her face. These symptoms caused her to experience foods and liquids falling out of the right side of her mouth when eating and drinking, as well as slurred speech. Her medical doctor prescribed a gabapentin (Neurontin, Pfizer, New York City, NY) and an eye lubricant, and recommended drinking cold water and using azithromycin (Z-Pak, Pfizer) if her condition worsened. In addition, a consultation with a neurologist was ordered. The neurologist stated that hers was a permanent condition and there was no treatment. According to the patient, the medical doctor agreed and concluded treatment. During the patient's chiropractic examination, cervical ranges of motion were within normal limits with a “pulling” sensation in the right trapezius in flexion and the left trapezius in right lateral flexion. Reflexes of the upper extremities were all +3 bilaterally. Muscle testing of the left upper extremity all elicited ratings of +4 except the deltoid, which was +3. Muscle testing of the right upper extremity elicited ratings of +2 except the biceps, triceps, and deltoid, which were +4. Palpation of the neck revealed fixation, swelling, and taut and tender fibers at the C1/2 levels on the right. Taut and tender fibers were also found at the C5-T2 levels on the right. The right trapezius and rhomboid were contracted.
A plain film radiographic study of her cervicothoracic spine was performed because of her history and physical examination findings. The anteroposterior view (Fig 1) displayed a levoscoliosis of 10° from C2 to C7. The lateral cervical view (Fig 2) showed a total loss of cervical lordotic curve and a 5° atlas angle to horizontal.
Fig 1.
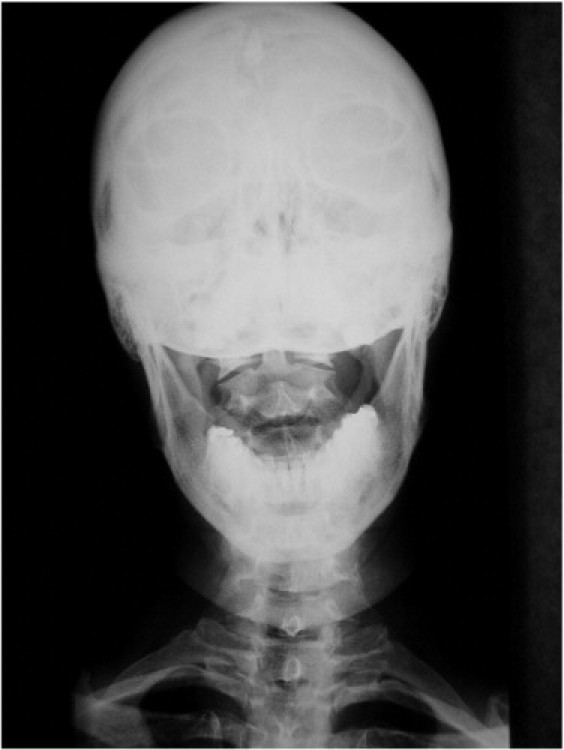
Anteroposterior radiograph of the patient showing a levoscoliosis of 10° from C2 to C7.
Fig 2.

Lateral cervical radiograph showing a total loss of cervical lordotic curve and a 5° atlas angle to horizontal.
The initial treatment plan consisted of chiropractic manipulation (CMT), interferential muscle stimulation, and hydroculation on the neck and trapezius bilaterally 3 times a week for 5 weeks followed by 1 time a week for 4 weeks. The CMT consisted of a high-velocity, low-amplitude technique while the patient lay supine of the C1 and C7 vertebrae and a high-velocity, low-amplitude technique while the patient lay prone (Diversified) of the T2 and T6 vertebrae.
Improvements in the patient's condition and overall health were observed after the first visit, and she reported to be sleeping more soundly. After her third visit, the patient reported that her sinuses were clearer, making breathing easier. In addition, the tightness of the right side of her face was reduced. When reviewing subjective findings on the sixth visit, she reported that her children had commented on her “smile going up more on the right.” The right corner of the patient's mouth was more even with the left side upon visual inspection. The patient continued to report decreased sinus pressure over the next 2 weeks. Significantly decreased sinus pressure was reported and significantly increased facial tone was visualized on her 17th visit.
After the patient's initial treatment plan concluded, a chiropractic reevaluation was performed. Palpation of the neck revealed reduced fixation at the C1/2 levels and that the swelling and taut and tender fibers at C1/2 on the right had subsided completely. The taut and tender fibers at the C5-T2 levels on the right had reduced, and the right trapezius and rhomboid muscles were no longer contracted.
The patient then began receiving chiropractic adjustments once a month. At 3 months, the patient's right eye was open approximately 50% more, and the right corner of her mouth was approximately 50% higher than at the start of care. The patient had sinus infections through the fifth and sixth months without Bell's palsy symptoms. Seven months after initiating care, the patient reported that she was no longer experiencing sinus infections and that her optometrist found her “vision was better” after a routine checkup. Upon physical examination, her right eye was more open and her smile was improved at 10 months after starting care.
During the next 4 months of care, the patient's improvement plateaued; and she experienced little change in her Bell's palsy symptoms. At 15 months, the patient reported less tension throughout her face and neck and visualized her “smile spreading more.” At 16 months after starting care, the corners of the patient's mouth were even; and her right eye was open twice as much as at the start of care. A plain film radiographic study of her cervicothoracic spine was performed. The anteroposterior view (Fig 3) displayed a 20% reduction in the C2-C7 levoscoliosis from 10° to 8°. The lateral cervical view (Fig 4) showed a 20% increase of atlas angle from 5° to 6°.
Fig 3.

Posttreatment anteroposterior radiograph showing a reduction in the C2-C7 levoscoliosis from 10° to 8°.
Fig 4.

Posttreatment lateral cervical radiograph showing an increase of atlas angle from 5° to 6°.
Discussion
Approximately 71% of patients with Bell's palsy will recover normal facial muscle function with treatment, 13% are left with slight weakness, and 16% experience moderate weakness resulting in major facial dysfunction.8
Medical treatment generally consists of antiviral and anti-inflammatory medications. Randomized clinical trials have shown acyclovir (antiviral) monotherapy to be inferior to prednisone (anti-inflammatory) monotherapy. Acyclovir and prednisone together are shown to be superior to prednisone alone.9 Surgical intervention has shown no positive effect. Transmastoid decompression should only be considered if a tumor is suspected.10
Chiropractic treatment of Bell's palsy has shown to be successful as reported in limited published case studies. Alcantara et al11 reported that a 49-year-old woman who had Bell's palsy for approximately 10 days presented for chiropractic care. This patient received 37 chiropractic adjustments over a 6-month period. The patient reported symptomatic relief in the cervical and facial regions after only 1 week. The patient noted that her facial pain was gone after 20 visits and that motor functions such as closing her right eye, smiling, raising her right eyebrow, and puffing her cheeks had returned. Shrode12 reported that 2 male teenagers presented separately with Bell's palsy, one with an onset of 2 days and the other 8 days. Both received high-voltage pulsed galvanic current to the muscles of the face and CMT to cervical spine fixations. The 2-day–onset patient received 16 treatments over a 6-week period with total remission at 6 weeks. The 8-day–onset patient received 9 treatments over a 3-week period with total remission at 3 weeks. Frach et al13 reported similar results in treating 2 patients with Bell's palsy. One was an 18-year-old woman of 10 days' duration with Bell's palsy, and the other was a 37-year-old man of 25 days duration' with Bell's palsy. The female patient's treatment consisted of mechanical force, manually assisted chiropractic technique and high-voltage galvanic therapy. She was released from care symptom-free after 5 treatments. The male patient's treatment consisted of mechanical force, manually assisted, high-voltage galvanic therapy and self-administered facial muscle exercises. This patient reported 60% to 70% improvement in his Bell's palsy symptoms after 9 treatments and discontinued care at that time. A patient having Bell's palsy for multiple years and regaining as much function as the subject of this case report has not been previously reported.
There are numerous theories as to why this patient's Bell's palsy symptoms responded favorably to chiropractic care. From an anatomical standpoint, the upper cervical adjustment could have changed tension from the arachnoid and dura mater, thus reducing a possible entrapment neuropathy.6 As cranial nerve VII exits the stylomastoid foramen, local entrapment may occur because of tension of the trapezius muscle that originates, in part, from the external occipital protuberance and the inner third of the superior curved line of the occipital bone.7 Tension of the sternocleidomastoid muscle, which inserts into the outer surface of the mastoid process and into the outer half of the superior line of the occipital bone, can also create local entrapment of the facial nerve.7 It is theorized that cervical manipulation may possibly help to reduce tension within these muscles by restoring proper biomechanical function and reducing nerve root compression.
There is a relationship between the facial nerve and the autonomic communicating branches in the upper cervical spine.4,12,14 As far back as 1910, DD Palmer reported how “misaligned” cervical vertebrae can potentially disrupt sympathetic nervous impulses to the facial nerve, causing facial paralysis.4,15
Limitations
As with any case study such as this, there are limitations.16,17 The most important limitation to consider is the uncontrollable environment in which patient care occurs.17,18 For example, a patient may not report taking a medication or supplement, may not follow at-home care recommendations, or may have an injury.17 The condition itself can cause limitations on patient results. This is especially true if the condition, like Bell's palsy, has the propensity for spontaneous remission.17,19 Response to the same treatment can vary greatly between patients with the same condition. This means that the information put forth in a case study cannot be used to come to a globalized conclusion.16,17,19,20
Other scenarios should also be considered. Bell's palsy, in most cases, is self-limiting and resolves without treatment.8 There is a possibility that this patient's case was resolving concurrently with the chiropractic care she received. Another scenario is that the patient experienced a placebo response to the chiropractic treatments. Finally, the author must depend on information retrieved from the patient treatment file. If detailed notes were not kept, a thorough case study cannot be accurately written. In addition, if the treating doctor and author are the same person, there is the possibility for personal bias to limit the interpretation of the notes.16,17
Because of the lack of literature, chiropractors should partner with neurologists on research projects and articles to compare different forms of Bell's palsy treatments. This partnership would increase the number of subjects, thus allowing for larger studies. In addition, more case studies of chiropractors helping patients reduce their Bell's palsy symptoms through chiropractic adjustments should be written. These reports will further support chiropractic care as a means of treating Bell's palsy.
Conclusion
For this patient, chiropractic care was shown to be effective in reducing the Bell's palsy symptoms, which this patient had experienced for 5 years.
Funding sources and potential conflicts of interest
No funding sources or conflicts of interest were reported for this study.
References
- 1.Taber's cyclopedic medical dictionary. 15th ed. F.A. Davis Company; Philadelphia: 1985. p. 190. Bell's palsy. [Google Scholar]
- 2.National Institute of Neurological Disorders and Stroke [Internet]. Bethesda, MD: National Institutes of Health; [updated 2010 Sep 27; cited 2010 Aug 1]. Bell's palsy fact sheet; [1 screen]. Available from: http://www.ninds.nih.gov/disorders/bells/detail_bells.htm.
- 3.Ruckenstein MJ. Evaluating facial paralysis, expensive diagnostic tests are often unnecessary. Postgrad Med 1998; 103:187-8, 191-2. [DOI] [PubMed]
- 4.Boneva D., Kessinger R. Bell's palsy and the upper cervical spine. Chiror Res J. 1999;6(2):47–56. [Google Scholar]
- 5.Schrim J., Mulkins P.S. Bell's palsy and herpes simplex virus. APMIS. 1997;105:815–823. doi: 10.1111/j.1699-0463.1997.tb05089.x. [DOI] [PubMed] [Google Scholar]
- 6.Blum C.L. Cranial therapeutic approach to cranial nerve entrapment. Part II: cranial nerve VII. J Chiropr. 1990;27(12):27–33. [Google Scholar]
- 7.Gray H. In: Gray's anatomy. 15th ed. Pick T.P., Howden R., editors. Barnes & Noble Books; New York: 1995. [Google Scholar]
- 8.Managing Bell's palsy. Drug Ther Bull. 2006;44(7):49–53. doi: 10.1136/dtb.2006.44749. [DOI] [PubMed] [Google Scholar]
- 9.Alberton D.L., Zed P.J. Bell's palsy: a review of treatment using antiviral agents. Ann Pharmacother. 2006;40:1838–1840. doi: 10.1345/aph.1H077. [DOI] [PubMed] [Google Scholar]
- 10.May M., Klein S.R., Taylor F.H. Indications for surgery for Bell's palsy. Am J Otolaryngol. 1984;5:503–512. [PubMed] [Google Scholar]
- 11.Alcantara J., Plaugher G., Van Wyngardern D. Chiropractic care of a patient with vertebral subluxation and Bell's palsy. J Manipulative Physiol Ther. 2003;26(4):253. doi: 10.1016/s0161-4754(02)54112-9. [DOI] [PubMed] [Google Scholar]
- 12.Shrode L.W. Treatment of facial muscles affected by Bell's palsy with high-voltage electrical muscle stimulation. J Manipulative Physiol Ther. 1993;16(5):347–352. [PubMed] [Google Scholar]
- 13.Frach J.P., Osterbauer P.J., Fuhr A.W. Treatment of Bell's palsy by mechanical force, manually assisted chiropractic adjusting and high-voltage electrotherapy. J Manipulative Physiol Ther. 1992;15(9):596–598. [PubMed] [Google Scholar]
- 14.Palmieri N.F. Idiopathic facial paralysis: mechanism, diagnosis, and conservative chiropractic management. Chiropr Tech. 1990;2:182–187. [Google Scholar]
- 15.Palmer D.D. Portland Publishing Company; Portland (OR): 1910. The chiropractic adjuster. [Google Scholar]
- 16.Martyn C. Case reports, case series, and systematic reviews. Q J Med. 2002;95:197–198. doi: 10.1093/qjmed/95.4.197. [DOI] [PubMed] [Google Scholar]
- 17.Green B.N., Johnson C.D. How to write a case report for publication. J Chiropr Med. 2006;5(2):72–82. doi: 10.1016/S0899-3467(07)60137-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grimes D.A., Schulz K.F. Descriptive studies: what they can and cannot do. Lancet. 2002;359:145–149. doi: 10.1016/S0140-6736(02)07373-7. [DOI] [PubMed] [Google Scholar]
- 19.Riddoch J. Evaluation of practice. Physiotherapy. 1991;77:439–444. [Google Scholar]
- 20.Doherty M. What value case reports? Ann Rheum Dis. 1994;53:1–2. doi: 10.1136/ard.53.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]


