Abstract
Objective
Methicillin-resistant Staphylococcus aureus (MRSA) is associated with difficult-to-treat infections and high levels of morbidity. Manual practitioners work in environments where MRSA is a common acquired infection. The purpose of this review is to provide a practical overview of MRSA as it applies to the manual therapy professions (eg, physical and occupational therapy, athletic training, chiropractic, osteopathy, massage, sports medicine) and to discuss how to identify and prevent MRSA infections in manual therapy work environments.
Methods
PubMed and CINAHL were searched from the beginning of their respective indexing years through June 2011 using the search terms MRSA, methicillin-resistant Staphylococcus aureus, and Staphylococcus aureus. Texts and authoritative Web sites were also reviewed. Pertinent articles from the authors' libraries were included if they were not already identified in the literature search. Articles were included if they were applicable to ambulatory health care environments in which manual therapists work or if the content of the article related to the clinical management of MRSA.
Results
Following information extraction, 95 citations were included in this review, to include 76 peer-reviewed journal articles, 16 government Web sites, and 3 textbooks. Information was organized into 10 clinically relevant categories for presentation. Information was organized into the following clinically relevant categories: microbiology, development of MRSA, risk factors for infection, clinical presentation, diagnostic tests, screening tests, reporting, treatment, prevention for patients and athletes, and prevention for health care workers.
Conclusion
Methicillin-resistant S aureus is a health risk in the community and to patients and athletes treated by manual therapists. Manual practitioners can play an essential role in recognizing MRSA infections and helping to control its transmission in the health care environment and the community. Essential methods for protecting patients and health care workers include being aware of presenting signs, patient education, and using appropriate hand and clinic hygiene.
Key indexing terms: Manual therapy, Methicillin-resistant Staphylococcus aureus, Public health
Introduction
Methicillin-resistant Staphylococcus aureus (MRSA) is a substantial public health problem worldwide, causing significant morbidity and mortality1 and elevated health care costs.2 There were an estimated 94 360 invasive MRSA infections in the United States in 2005, causing more than 18 000 deaths per year.1 Methicillin-resistant S aureus prevalence has increased over the last 10 years; MRSA-related hospital discharges have doubled over 10 years, with hospital discharges for MRSA skin and soft tissue infection tripling since 2004.3 Infections caused by MRSA are associated with longer hospital stays4, 5 and an increased financial burden on society, costing an estimated US $14.5 billion for all inpatient days in 2003.5 An example of the increased morbidity and mortality associated with MRSA can be seen when comparing the yearly infection rates and mortality rates in the United States for MRSA, AIDS, viral hepatitis, and tuberculosis. Methicillin-resistant S aureus is estimated to cause more infections than the other diseases combined (Fig 1A) and more deaths per year than AIDS (Fig 1B).
Fig 1.
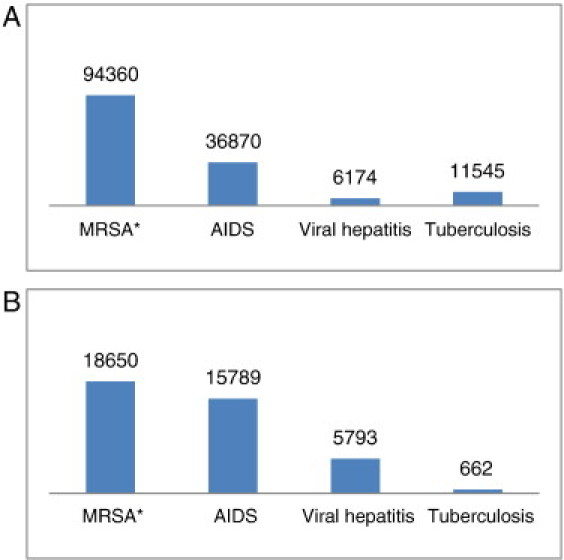
A, Infections per year in the United States. B, Deaths per year in the United States. *Because MRSA is currently not a nationally reportable disease, MRSA estimates of yearly infections and deaths are based on the study by Klevens et al1; and data for AIDS, viral hepatitis, and tuberculosis are from the CDC6 and Boucher and Corey.7 (The graphs created by the authors are in the public domain and thus free of any copyright restrictions.)
Methicillin-resistant S aureus is a common problem in health care facilities, sports facilities, clinics, and the community. The MRSA strains associated with hospitals are referred to as hospital-acquired MRSA (HA-MRSA) and are the most common cause of hospital-acquired infections.2, 5, 8, 9 Methicillin-resistant S aureus is the leading cause of skin and soft tissue infection in patients reporting to emergency departments for treatment,10 with a rising rate in primary care clinics11 and intensive care units.5 Invasive MRSA-related conditions most commonly reported include septic shock (56%), pneumonia (32%), endocarditis (19%), bacteremia (10%), and cellulitis (6%).1 Strains associated with the community are referred to as community-acquired MRSA (CA-MRSA) and are also present in people who serve as asymptomatic carriers.12
Methicillin-resistant S aureus is not restricted to any geographic area; it is a worldwide problem.5 Europe has a strong presence of MRSA, accounting for approximately 44% of nosocomial infections in the year 2008.13 Fortunately, this is improving because of surveillance programs and stringent outbreak control criteria.14 Hospital-acquired MRSA has a high prevalence in Australia,14 North Africa, the Middle East, and East Asia4 and has been reported in 25% or more of S aureus isolates in Bulgaria, Croatia, Cyprus, Greece, Israel, Italy, Malta, Portugal, Ireland, Romania, Spain, Turkey, and the UK.13 Community-acquired MRSA has a higher prevalence in the US,5 Canada,5 and Australia.13
The purpose of this narrative review is to provide apractical overview and framework for manual therapypractitioners to better understand MRSA and howto control its transmission in the ambulatory care work environment.
Methods
PubMed and CINAHL were searched from the beginning of their respective indexing years through June 2011. Search terms included MRSA, methicillin-resistant Staphylococcus aureus, and Staphylococcus aureus. Texts pertaining to infectious disease clinical management and epidemiology and the Web site of the Centers for Disease Control and Prevention (CDC) were also reviewed. Pertinent articles from the authors' libraries were included if they were not already identified in the literature search. For this review, articles were included if they were applicable to ambulatory health care environments in which manual therapists work or ifthe content of the article related to the clinical management of MRSA. Articles deemed not directly pertinent to the ambulatory care environment (eg, genetics, surgical methods) were not included.
Three authors (B.N.G., C.D.J., J.T.E.) performed the information abstraction from the source documents. Information from the source documents was organized into categories of chief concern for manual therapists. Primary attention was given to CA-MRSA epidemiology, information on MRSA carriage, skin and soft tissue infection recognition and response, musculoskeletal implications of MRSA infection and pharmacologic treatment, and clinical hygiene.
Results
More than 200 source documents were reviewed. Following information extraction, 95 citations were included in this review, to include 76 peer-reviewed journal articles, 16 government Web sites, and 3 textbooks. Information was organized into the following clinically relevant categories: microbiology, development of MRSA, risk factors for infection, clinical presentation, diagnostic tests, screening tests, reporting, treatment, prevention for patients and athletes, and prevention for health care workers.
Summary of findings
Few articles exist on the topic of MRSA as they are pertinent to practitioners of manual therapy. Research efforts have focused on the importance of treatment table and hand hygiene15, 16, 17, 18 and risk reduction in athletic environments,19, 20, 21 and one article22 has discussed the rising importance of MRSA for physical therapists. However, we did not find any articles that provided a clinically oriented practical overview of this topic for manual therapists and believe that this is the first such article. Considering the high prevalence of MRSA and relative paucity of literature for manual therapy practitioners that provides guidance on how to prevent and manage MRSA infections, the current article provides a concise and clinically relevant overview that fills a void in the literature.
Staphylococcus aureus is a common bacterium in humans and a potent pathogen possessing numerous virulence factors that enhance its opportunity to thrive.23 Some strains of S aureus have developed resistance to antibiotic medications, including methicillin and drugs in its class, giving such specific strains of S aureus the deserved name of MRSA. This drug resistance has developed rapidly and continues to evolve with each new medication developed to combat this infectious agent. Manual therapists who work directly with patients and athletes in the health care environment should be informed of this potentially harmful infection and take action to recognize and prevent it. The following discussion provides an overview of the microbiology, development, risk factors, clinical presentation, diagnostic tests, screening tests, reporting, treatment, and prevention measures for MRSA.
Microbiology
Staphylococcus aureus is a gram-positive, nonmotile, pus-producing coccus.23, 24 Microscopically, S aureus has the appearance of 0.5- to 1.5-µm balls that are clumped together, like grapes.23, 25 There are more than 200 strains of S aureus.2 Staphylococcus aureus possesses several virulence factors that, combined with its increasing antibiotic resistance, contribute to its success as an infective agent.8, 23
Development of MRSA
In 1929, Alexander Fleming discovered that a mold called Penicillium had the ability to secrete a substance that killed bacteria, including some staphylococci; and he called the filtrate of a broth of this culture penicillin.26 Within a year after the introduction of penicillin, isolates of S aureus had already become resistant to penicillin9; and S aureus went on to develop resistanceto other antibiotics.12, 27 In the 1950s, the first epidemics of nosocomial penicillin-resistant staphylococci were reported in Europe and North America, only a decade after the widespread prophylactic use of postoperative antibiotics became commonplace.28 By the 1960s, penicillin-resistant strains were already considered pandemic.12 Methicillin (also known internationally as meticillin) was introduced as an antibiotic against S aureus in 1959.29 By 1961, S aureus hadbegun developing resistance to methicillin,12, 29 quickly spread worldwide, and is now considered endemic to most hospitals as HA-MRSA.12 As time passed, S aureus not only evolved to become resistant to a host of antibiotics such as HA-MRSA but also transcended the confines of health care institutions to produce infection in healthy members of the community as CA-MRSA.9, 24, 30, 31, 32
The strains of S aureus that have developed resistance to common antibiotics are known collectively as methicillin-resistant S aureus, even though they may be resistant to other named antibiotics in the penicillin and cephalosporin categories.28, 30 Methicillin-resistant S aureus can live for months in hostile environments and is thereby transmitted from surfaces long after it is initially deposited.33, 34
Community-acquired MRSA–colonized individuals and their close contacts are more likely to develop skin and soft tissue infections.12 Among noninstitutionalized adults in the United States, there is an anterior nares MRSA carriage rate of 1.5%.35 Among certain adult populations, this rate can be much higher, such as 3% among US soldiers,36 7% among US undergraduate college students,37 and 23% among US college athletes.38 In long-term health care facilities, a large proportion of residents may be colonized with MRSA39; and as a consequence, asymptomatic MRSA carriers arepresent in treatment areas daily and represent a reservoir of MRSA that manual therapists must consider particularly as it pertains to infectious control practices.
The incidence of CA-MRSA has increased recently in people who are generally perceived as healthy (eg, athletes and soldiers).12, 36, 40, 41, 42 With CA-MRSA and HA-MRSA both being common, it has been noted thatthe strains may be present together, with community strains being introduced into hospitals43 and HA-MRSA being present in the community.11, 44, 45 The distinction between HA-MRSA and CA-MRSA is thus blurring,11 and co-colonization in the hospital is predicted to become the norm.46 In clinics where postoperative patients interact with nonoperative patients, there is an increased chance of the presence of both HA-MRSA and CA-MRSA, requiring clinicians to be vigilant for both forms and to use appropriate infection control efforts.
Methicillin-resistant S aureus' drug resistance continues to evolve. More than 50% of MRSA strains are resistant to drugs such as macrolides, lincosamides, fluoroquinolones, and aminoglycosides; and 30% are resistant to trimethoprim-sulfamethoxazole.8 Vancomycin was one of the few remaining medications to control difficult MRSA; however, vancomycin-resistant MRSA is now a reality.8 Methicillin-resistant Saureus is transmitted more easily in the community but has generally remained more susceptible to a broader range of antibiotics12; multidrug resistance in CA-MRSA, nevertheless, has been detected.47 Furthermore, as community and hospital strains intermingle44 and as patients and community members bring these strains into the hospital and vice versa, there is a growing concern that highly virulent community strains that affect healthy individuals will become less susceptible to antibiotics.41, 43
Risk factors for infection
The primary risk factor for MRSA infection in the inpatient setting is a compromised immune system. Those most at risk for infection are infants,2 the elderly,40, 48 the chronically ill,49 burn survivors,2 organ transplants recipients,2 cancer patients receiving chemotherapy agents,50 steroid users,50 diabetic patients,8 intravenous drug users, and those with AIDS.8 Additional risk factors for HA-MRSA infection include the length of stay in hospital, exposure to antibiotics,51 and exposure to people infected with MRSA.28
In the outpatient or community setting, risk factors for CA-MRSA infection include exposure to an individual with MRSA, usually skin-to-skin contact, and exposure to environments favorable to crowding49 or alack of cleanliness.12, 40, 52 Community-acquired MRSA is more common in competitive athletes,9, 40, 42 military personnel,9, 36, 40, 53 and prison inmates.9, 40, 54 In the community, MRSA tends to affect younger, healthier people12, 40, 48 such as college students.37, 55 Outbreaks have also been reported in children,9, 12, 56 the homeless,9, 40 men who have sex with men,47 some Native American groups,40 and injection drug users.57, 58 The CDC advocates the “5 Cs” (crowding, frequent skin-to-skin contact, compromised skin, contamination, lack of cleanliness) as important to MRSA transmission (Fig 2).52
Fig 2.

The 5 Cs related to CA-MRSA infection include crowding, frequent skin-to-skin contact, compromised skin (eg, cuts or abrasions), contaminated items and surfaces, and a lack of cleanliness.52 (This image created by the authors is in the public domain and thus free of any copyright restrictions.)
Community-acquired MRSA infections of the skin and soft tissues are becoming more common, and the incidence has been reported in association with various sports seasons. Reports of football teams with CA-MRSA have shown that increased exposure to training rooms and equipment is associated with increased cases of CA-MRSA among players59, 60, 61; and cosmetic body shaving among athletes has been associated with infection.42 For example, in a team of players that tested negative for anterior nares colonization at the beginning of a season, 5 members later were identified as having CA-MRSA.62 Another study showed that the number of nasal colonized student athletes varied across the season by intensity of activity.38 It is still not clear why some colonized individuals develop MRSA infection and others do not,58 although there is growing suspicion that colonization sites away from the nares (such as the genitalia, not tested in these studies) may play a more important role.63 In one natural history study, 38% of nares MRSA colonized soldiers went on to develop MRSA infection.36 In another study, over the course of a year, anterior nares colonization in athletes did not lead to infection outbreaks.38
Clinical presentation
As a ubiquitous bacterial pathogen, S aureus is responsible for a broad range of infections in nearly every body system. Staphylococcus aureus infections are pyogenic and known for their hallmark local tissue destruction and pain.23 Because of the prevalence of MRSA, it is expected that those infected with MRSA will present to clinic; hence, it is important for healthcare providers to identify potential MRSA cutaneous infections. Because MRSA infection may mimic other lesions, proper precautions and clinical suspicion are warranted.
In ambulatory health care and community settings, the majority of MRSA infections are cutaneous, involving cellulitis, an abscess, or both.40 Simple inspection and basic health history questions will provide much information in the identification of MRSA. Pain and pus production at the site of infection are characteristic of S aureus infections,64 and the infection is often accompanied by inflammation and swelling.12, 40, 58, 65, 66 Cutaneous MRSA lesions will frequently occur at the site of an abrasion or cut, even if the injury is mild.58, 66 For example, athletes with artificial turf abrasions or who have used cosmetic shaving have developed MRSA skin infections.42 Manual therapists should be vigilant for cutaneous staphylococcal lesions, such as cellulitis,40 abscesses, folliculitis,65, 67 furuncles,65, 67 carbuncles, erysipelas, and impetigo.58 Methicillin-resistant S aureus should be considered as a potential diagnosis for any pus-producing skin lesion. For cutaneous CA-MRSA, differential diagnoses may include spontaneous abscesses40 and lesions that appear to be spider bites.11, 53, 65 Examples of cutaneous MRSA lesions appear in Fig 3, Fig 4, Fig 5.
Fig 3.

A cutaneous abscess caused by MRSA. This image is in the public domain and thus free of any copyright restrictions. (The image is courtesy of Gregory Moran, MD, and available at http://www.cdc.gov/mrsa/mrsa_initiative/skin_infection/mrsa_photo_006.html.)
Fig 4.

This photograph depicts a cutaneous MRSA abscess located on the hip of a prison inmate, which had begun to spontaneously drain, releasing its purulent contents. This image is in the public domain and thus free of any copyright restrictions. (The image is courtesy of the CDC and available at http://www.cdc.gov/mrsa/mrsa_initiative/skin_infection/mrsa_photo_7826.html.)
Fig 5.

A cutaneous MRSA abscess located on a patient's back. This image is in the public domain and thus free of any copyright restrictions. (The image is courtesy of Gregory Moran, MD, and available at http://www.cdc.gov/mrsa/mrsa_initiative/skin_infection/mrsa_photo_010.html.)
The typical patient profile of a CA-MRSA skin infection is a young, healthy person with a pyogenic abscess surrounded by cellulitis.40 If a pyogenic lesion is found, practitioners should inquire about possible risk factors, including poor hygiene; close living conditions; sharing of personal linens or hygiene items, such as clothing, bedding, towels, or razors; the presence of a recent cut; abrasions or injuries in the area; a history of other soft tissue infections; or contact with aknown MRSA carrier.
Cutaneous skin infections can invade deeper tissue layers and become expansive.58 A minority of CA-MRSA infections are more severe and potentially invasive, including purpura fulminans, pyomyositis, myositis, necrotizing fasciitis, osteomyelitis, and necrotizing pneumonia.12, 58 In young children, scalded skin syndrome may be noted.50 Necrotizing fasciitis is suspected when a patient reports severe pain that appears to be out of proportion to the examination, a “wood like” feeling upon palpation of the area, or gas lucencies along fascial planes noted on radiographs.58
It is important to keep in mind that many people are asymptomatic carriers and may have no clinical symptoms of MRSA, and MRSA infections may not necessarily involve the skin or soft tissues. Further investigation may be needed to confirm if MRSA is present in individuals with suspected infections.
Diagnostic tests
The first step in confirming MRSA is to isolate Saureus from a culture of blood, tissue, or pus. If Saureus is not found in a culture, it is unlikely that theindividual has MRSA.12 The only time a culture would yield a false-negative result would be if the patient had recently received several days of antistaphylococcal medication in the days immediately preceding the culture.12 If S aureus is detected in a culture medium, then confirmatory testing can demonstrate if the organism is resistant to antibiotics.12, 68 Susceptibility tests do not discriminate between HA-MRSA and CA-MRSA strains; and clinically, it is often irrelevant to isolate CA-MRSA from HA-MRSA because the treatment is not governed by identification of the strain.44 Cultures are performed when infection fails torespond to treatment with incision and drainage or if first-line treatment of MRSA plus streptococcus continues to demonstrate resistant infection. Cultures may also be obtained when a cluster of infections is reported, when local infection is severe, or when there is systemic infection.31
Screening tests
Screening for MRSA occurs in some facilities, such as hospital inpatient settings, long-term care facilities, and nursing homes, with the intent of detecting MRSA carriers and using control measures to prevent the spread of MRSA.69 Manual therapy practitioners working in inpatient settings and those caring for patients in the postoperative setting may need to be aware of these practices. Historically, screening has included nasal swabbing to test for the presence of MRSA colonization in the anterior nares before admission.25, 70 Samples are incubated and cultured to identify S aureus colonies, and then susceptibility tests are performed to confirm the presence of MRSA. These tests typically take 16 to 48 hours to yield results and are not used in outpatient settings. Thus, there is no inexpensive, sensitive, specific, and rapid test that manual therapists can use to screen for MRSA.
If a patient is determined to be MRSA colonized, then he or she may be placed in contact isolation,25, 70 treated successfully before hospitalization,2 or placed in a room with another patient infected with the same organism.71, 72 Methicillin-resistant S aureus screening is a controversial topic, and it is beyond the scope of this article to present it in detail; however, it behooves the health care worker to know that such practices do exist and to become familiar with them if working in a facility that uses screening.
Reporting
Although national reporting is not currently required, reporting of individual MRSA cases is mandatory in some states. For example, since 2008, the state of California has required severe infections or any clusters or outbreaks of MRSA to be reported.73, 74 Because policies pertaining to the reporting of MRSA infections are ever-developing, providers should check with their state health department to determine if MRSA is considered reportable where they practice.75 If a practitioner recognizes a concentration of MRSA cases, such as in a sports team or at a summer camp, obligatory reporting to public health authorities is required.50 Hospitals are required to report MRSA infection rates within their hospital-acquired infection rates.76
Treatment
The treatment of MRSA is based upon the type of infection, the location, and the severity. When MRSA infection is suspected, clinical practice guidelines on the treatment of MRSA suggest immediate referral to initiate appropriate medical care.31, 58 The patient should avoid spreading the infection and not use wet compresses.58 For skin abscesses, medical care using incision and drainage is the treatment of choice.40 Daily cleansing of the skin with a disinfectant is often part of CA-MRSA dermatological care.25
If evidence of surrounding cellulitis is found, antibiotics may be added.31 Antibiotic choice should be guided by community susceptibilities but usually begins with trimethoprim-sulfamethoxazole or, for the sulfa allergic patient, doxycycline or minocycline. Additional coverage for methicillin-susceptible S aureus and streptococci is usually provided by cephalexin, dicloxacillin, or clindamycin.31 Methicillin-resistant S aureus infections that fail initial treatment may require multidrug therapy, such as the combination of vancomycin with one or more additional antibiotics.25, 77
Patients should be encouraged to take their full course of medication and contact their primary care provider immediately should adverse effects develop. Common adverse effects reported from antibiotic treatment include gastrointestinal distress, such as diarrhea, nausea, and abdominal pain78; rashes; itching; fevers or chills; jaundice; dyspnea; dysphagia; and headache.79, 80, 81, 82, 83 Manual therapists should be aware of the medications prescribed for MRSA that have adverse effects pertinent to the musculoskeletal system, such as joint aches,80, 82 joint stiffness or swelling,83 weakness,83 chest or back pain and tightness,79 and unusual bleeding or bruising.79, 84 Drugs in the fluoroquinolone class are infrequently used in the management of patients with MRSA, but may be used in multidrug therapy for osteomyelitis31 or osteoarticular infections31 or be prescribed unnecessarily.85 Fluoroquinolone use is associated with an increased prevalence oftendinopathy and joint lesions.86, 87, 88 Age greater than60 years, sex, use of corticosteroids, diabetes, and strength-training and aerobic-conditioning activities areassociated with higher rates of fluoroquinolone-induced tendinopathy.89 This tendinopathy may manifest in both the lower and upper extremities; range from minor discomfort to frank tendon rupture; or become symptomatic within hours of the initial dose, but typically a week after the start of therapy90; and may persist for months following cessation of medication therapy.78, 91 Awareness of medication use should influencemanual therapists' clinical decision making, such as when not to engage in strenuous activity or deep tissue mobilization.
Prevention for patients and athletes
For healthy individuals without signs and symptoms of infection, basic hygiene practices are the mainstay to prevent MRSA infections. Hands should be washed thoroughly with soap and warm water; washing can be replaced by alcohol-based hand rubs if the hands are not visibly soiled.92 To reduce the risk of infection, people should not share personal items (towels, razors, washcloths, dirty clothes, used athletic gear) and keep personal items (clothes, bedding, towels, work/study area) clean.52, 53
For patients with known infections, it is important to prevent spread to others. Persons participating in the changing of wound dressings should wash their hands.92 Wounds should be covered with a bandage until they are healed; and any wound containing pus should be covered with a clean, dry bandage to prevent the spread of infection. Bandages and tape used to cover wounds can be disposed of with regular garbage.92 If a person has a suspected MRSA skin infection, he or she should be discouraged from trying self-treatment by popping, draining, or lancing it and seek the advice of a health care provider.
Because many sports involve close personal contact, including the use of common equipment and shower areas, additional recommendations are available for athletes and athletic facilities. It is particularly important to disallow the participation of athletes with a cutaneous MRSA infection in close contact sports unless the wound can be completely covered or until full recovery is evident.19 Athletes should be discouraged from sharing clothing or protective gear, such as helmets and body armor,93 and from sharing bar soap.94 Wearing clean uniforms and changing clothes regularly reduce the risk for infection and should be encouraged.52, 53 Athletes with known cutaneous MRSA infections should not use common pools, including therapy whirlpools, unless the pool water is regularly changed after use.19 Shared athletic equipment, such as weight machines and benches, should be cleaned with disinfectant on all surfaces where skin touches the equipment; surfaces such as floors, mats, and doors should also be cleaned on a regular basis. The CDC offers a comprehensive list of suggestions for controlling MRSA in common settings and a list of appropriate disinfectants.20
Steps for the prevention of CA-MRSA should be made known to at-risk patient populations. The National Athletic Trainers' Association has produced a comprehensive position statement and an easy-to-use patient education document.21 The CDC Web site provides a number of client education tools and brochures available at http://www.cdc.gov/mrsa/prevent/index.html. Appendix A to this article offers a sample educational page for the layperson.
Prevention for health care workers
Standard precautions are recommended when treating those patients with infection or those who are susceptible to infection. Accordingly, health care providers should wear gloves when examining or treating body areas with a suspected cutaneous lesion; and proper hand washing following examination or treatment is required,2 including proper hand hygiene; gloving; wearing eye, mouth, and nose protection; gowning; cleaning equipment with disinfectant; and the appropriate cleaning of laundry.71
For interacting with patients without known infection, hand hygiene is critical in preventing MRSA transmission, including the proper use of alcohol-based hand sanitizers.2, 25, 33, 95 The practitioner should wash hands thoroughly with soap and warm water after working with each patient. Hand washing can be replaced by alcohol-based hand rubs if the hands are not visibly soiled.92 Health care workers should keep in mind that there are many asymptomatic MRSA carriers (potentially including the health care team), which further underscores the need for appropriate hand and clinic hygiene.
Simple hand hygiene can result in substantial reduction in infections. For example, a study in Canada reported a 51% reduction in the incidence of HA-MRSA per 1000 hospital admissions, saving substantial morbidity, mortality, and more than Can $858 000, after instituting an alcohol-based gel hand sanitizer program for patients and their contacts.95 More recently, US Veterans Affairs acute care hospitals reduced MRSA rates nationally after enforcing the use of standard precautions with emphasis on hand hygiene and infection control. After implementing the protocol, the rates of health care–associated MRSA infections decreased in these health care facilities by 45%.69
Items commonly used in the manual practitioner's office, such as examination or treatment tables, adjusting tables, physical therapy plinths and equipment, stethoscopes, blood pressure cuffs, and exercise mats, can easily become contaminated with MRSA, which may remain for an extended period if not cleaned properly.2, 16 Appropriate infection control measures, such as wiping treatment tables, exercise equipment, and mats with a disinfectant wipe or cleaning solutionafter every use, should be used.16 The CDC recommends that surfaces and floors be cleaned with disinfectants approved by the Environmental Protection Agency2 using List H on the Environmental Protection Agency's Web site of registered disinfectants (http://epa.gov/oppad001/chemregindex.htm).
Outpatient settings that provide access to people who are healthy or injured but noninfected (eg, athletes, soldiers) and at the same time provide treatment to postoperative patients may be at an increased risk of contamination from both HA-MRSA and CA-MRSA. Thus, facilities that serve combined populations should be extracautious and ensure implementation of appropriate clinic, patient, and provider hygiene.
Limitations
This is a narrative review of the literature and therefore did not implement quantitative methods to analyze the literature on clinical effectiveness or implementation of prevention programs. Not all detailed MRSA information is included in this report. Other authors have provided more in-depth studies and guidelines; readers are referred to these documents for more information.31, 58
Conclusion
Methicillin-resistant S aureus is commonly found in the population and may result in a harmful and potentially fatal infection. Identification of likely MRSA cutaneous lesions is straightforward and can lead to early treatment and perhaps even the prevention of systemic disease. Manual practitioners can use a variety of simple and routine infection control measures to prevent infections and the transmission of MRSA between patients, clinic staff members, and the community.
Funding sources and potential conflicts of interest
No funding sources were reported for this study. Bart Green is the Associate Editor for the National University of Health Sciences. Claire Johnson is the Editor-in-Chief for the National University of Health Sciences.
Footnotes
The views expressed in this article are those of the authors and do not reflect the official policy or position of the Department of the Navy, Department of Defense, Department of Veterans Affairs, or the United States Government.
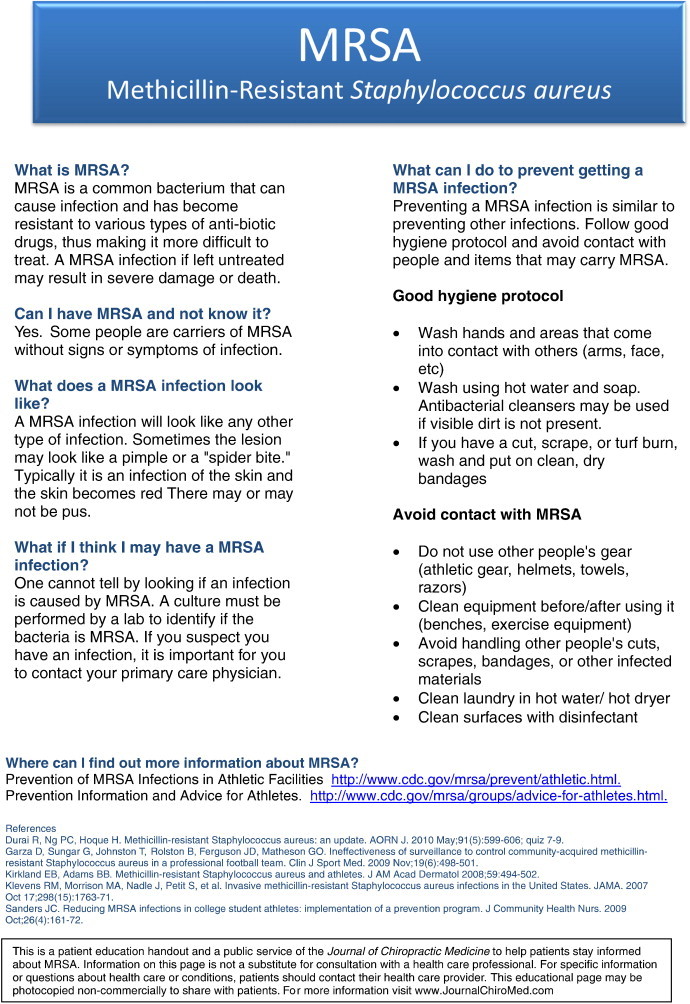
Appendix A. MRSA information sheet
References
- 1.Klevens R.M., Morrison M.A., Nadle J., Petit S., Gershman K., Ray S. Invasive methicillin-resistant Staphylococcus aureus infections in the United States. JAMA. 2007;298(15):1763–1771. doi: 10.1001/jama.298.15.1763. [DOI] [PubMed] [Google Scholar]
- 2.Durai R., Ng P.C., Hoque H. Methicillin-resistant Staphylococcus aureus: an update. AORN J. 2010;91(5):599–606. doi: 10.1016/j.aorn.2009.11.065. [quiz 7-9] [DOI] [PubMed] [Google Scholar]
- 3.Mera R.M., Suaya J.A., Amrine-Madsen H., Hogea C.S., Miller L.A., Lu E.P. Increasing role of Staphylococcus aureus and community-acquired methicillin-resistant Staphylococcus aureus infections in the United States: a 10-year trend of replacement and expansion. Microb Drug Resist. 2011;17(2):321–328. doi: 10.1089/mdr.2010.0193. [DOI] [PubMed] [Google Scholar]
- 4.Ippolito G., Leone S., Lauria F.N., Nicastri E., Wenzel R.P. Methicillin-resistant Staphylococcus aureus: the superbug. Int J Infect Dis. 2010;14(Suppl 4):S7–S11. doi: 10.1016/j.ijid.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 5.Carroll K.C. Rapid diagnostics for methicillin-resistant Staphylococcus aureus: current status. Mol Diagn Ther. 2008;12(1):15–24. doi: 10.1007/BF03256265. [DOI] [PubMed] [Google Scholar]
- 6.Summary of notifiable diseases: United States, 2009. MMWR Morb Mortal Wkly Rep. 2011;58(53):1–100. [PubMed] [Google Scholar]
- 7.Boucher H.W., Corey G.R. Epidemiology of methicillin-resistant Staphylococcus aureus. Clin Infect Dis. 2008;46(Suppl 5):S344–S349. doi: 10.1086/533590. [DOI] [PubMed] [Google Scholar]
- 8.Archer G.L. Staphylococcus aureus: a well-armed pathogen. Clin Infect Dis. 1998;26(5):1179–1181. doi: 10.1086/520289. [DOI] [PubMed] [Google Scholar]
- 9.Deresinski S. Methicillin-resistant Staphylococcus aureus: an evolutionary, epidemiologic, and therapeutic odyssey. Clin Infect Dis. 2005;40(4):562–573. doi: 10.1086/427701. [DOI] [PubMed] [Google Scholar]
- 10.Moran G.J., Krishnadasan A., Gorwitz R.J., Fosheim G.E., McDougal L.K., Carey R.B. Methicillin-resistant S. aureus infections among patients in the emergency department. N Engl J Med. 2006;355(7):666–674. doi: 10.1056/NEJMoa055356. [DOI] [PubMed] [Google Scholar]
- 11.Parchman M.L., Munoz A. Risk factors for methicillin-resistant Staphylococcus aureus skin and soft tissue infections presenting in primary care: a South Texas Ambulatory Research Network (STARNet) study. J Am Board Fam Med. 2009;22(4):375–379. doi: 10.3122/jabfm.2009.04.090003. [DOI] [PubMed] [Google Scholar]
- 12.Deleo F.R., Otto M., Kreiswirth B.N., Chambers H.F. Community-associated meticillin-resistant Staphylococcus aureus. Lancet. 2010;375(9725):1557–1568. doi: 10.1016/S0140-6736(09)61999-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kock R., Becker K., Cookson B., van Gemert-Pijnen J.E., Harbarth S., Kluytmans J. Methicillin-resistant Staphylococcus aureus (MRSA): burden of disease and control challenges in Europe. Euro Surveill. 2010;15(41):19688. doi: 10.2807/ese.15.41.19688-en. [DOI] [PubMed] [Google Scholar]
- 14.Humphreys H. National guidelines for the control and prevention of methicillin-resistant Staphylococcus aureus—what do they tell us? Clin Microbiol Infect. 2007;13(9):846–853. doi: 10.1111/j.1469-0691.2007.01766.x. [DOI] [PubMed] [Google Scholar]
- 15.Evans M.W., Jr., Ramcharan M., Ndetan H., Floyd R., Globe G., Pfefer M. Hand hygiene and treatment table sanitizing in chiropractic teaching institutions: results of an education intervention to increase compliance. J Manipulative Physiol Ther. 2009;32(6):469–476. doi: 10.1016/j.jmpt.2009.06.007. [DOI] [PubMed] [Google Scholar]
- 16.Evans M.W., Jr., Ramcharan M., Floyd R., Globe G., Ndetan H., Williams R. A proposed protocol for hand and table sanitizing in chiropractic clinics and education institutions. J Chiropr Med. 2009;8(1):38–47. doi: 10.1016/j.jcm.2008.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bifero A.E., Prakash J., Bergin J. The role of chiropractic adjusting tables as reservoirs for microbial diseases. Am J Infect Control. 2006;34(3):155–157. doi: 10.1016/j.ajic.2005.12.007. [DOI] [PubMed] [Google Scholar]
- 18.Burnham K., Peterson D., Vavrek D., Haas M. The impact of microbial surveys on disinfection protocols in a chiropractic college environment. J Manipulative Physiol Ther. 2009;32(6):463–468. doi: 10.1016/j.jmpt.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention . Centers for Disease Control; Atlanta: 2010. Prevention of MRSA infections in athletic facilities.http://www.cdc.gov/mrsa/prevent/athletic.html [cited 2011 July 14, 2011]; Available from: [Google Scholar]
- 20.Centers for Disease Control and Prevention . Centers for Disease Control and Prevention; Atlanta: 2010. Cleaning & disinfecting athletic facilities for MRSA.http://www.cdc.gov/mrsa/environment/athleticFacilities.html [cited 2011 July 15, 2011]; Available from: [Google Scholar]
- 21.Zinder S.M., Basler R.S., Foley J., Scarlata C., Vasily D.B. National athletic trainers' association position statement: skin diseases. JAthl Train. 2010;45(4):411–428. doi: 10.4085/1062-6050-45.4.411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Levenhagen K.M. Community-acquired methicillin-resistant Staphylococcus aureus: an emerging concern for physical therapists: discussion. Physiother Res Int. 2008;13(1):9–17. doi: 10.1002/pri.392. [DOI] [PubMed] [Google Scholar]
- 23.Cotran R.S., Kumar V., Collins T. 6th ed. W.B. Saunders Company; Philadelphia: 1999. Robbins pathologic basis of disease. [Google Scholar]
- 24.Deurenberg R.H., Stobberingh E.E. The evolution of Staphylococcus aureus. Infect Genet Evol. 2008;8(6):747–763. doi: 10.1016/j.meegid.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 25.Dissemond J. Methicillin resistant Staphylococcus aureus (MRSA): diagnostic, clinical relevance and therapy. J Dtsch Dermatol Ges. 2009;7(6):544–551. doi: 10.1111/j.1610-0387.2009.07015.x. [quiz 52-3] [DOI] [PubMed] [Google Scholar]
- 26.Fleming A. On the antibacterial action of cultures of a Penicillium with special reference to their use in the isolation of B. influenzae. Br J Exp Pathol. 1929;10:226–236. [Google Scholar]
- 27.Schentag J.J., Hyatt J.M., Carr J.R., Paladino J.A., Birmingham M.C., Zimmer G.S. Genesis of methicillin-resistant Staphylococcus aureus (MRSA), how treatment of MRSA infections has selected for vancomycin-resistant Enterococcus faecium, and the importance of antibiotic management and infection control. Clin Infect Dis. 1998;26(5):1204–1214. doi: 10.1086/520287. [DOI] [PubMed] [Google Scholar]
- 28.Nelson K.E., Williams C.M. 2nd ed. Jones and Bartlett Publishers; Sudbury, MA: 2007. Infectious disease epidemiology : theory and practice. [Google Scholar]
- 29.Enright M.C., Robinson D.A., Randle G., Feil E.J., Grundmann H., Spratt B.G. The evolutionary history of methicillin-resistant Staphylococcus aureus (MRSA) Proc Natl Acad Sci U S A. 2002;99(11):7687–7692. doi: 10.1073/pnas.122108599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chambers H.F. The changing epidemiology of Staphylococcus aureus? Emerg Infect Dis. 2001;7(2):178–182. doi: 10.3201/eid0702.010204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu C., Bayer A., Cosgrove S.E., Daum R.S., Fridkin S.K., Gorwitz R.J. Clinical practice guidelines by the infectious diseases society of america for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin Infect Dis. 2011;52(3):e18–e55. doi: 10.1093/cid/ciq146. [DOI] [PubMed] [Google Scholar]
- 32.Charlebois E.D., Perdreau-Remington F., Kreiswirth B., Bangsberg D.R., Ciccarone D., Diep B.A. Origins of community strains of methicillin-resistant Staphylococcus aureus. Clin Infect Dis. 2004;39(1):47–54. doi: 10.1086/421090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Humphreys H., Grundmann H., Skov R., Lucet J.C., Cauda R. Prevention and control of methicillin-resistant Staphylococcus aureus. Clin Microbiol Infect. 2009;15(2):120–124. doi: 10.1111/j.1469-0691.2009.02699.x. [DOI] [PubMed] [Google Scholar]
- 34.Smith T.C., Moritz E.D., Leedom Larson K.R., Ferguson D.D. The environment as a factor in methicillin-resistant Staphylococcus aureus transmission. Rev Environ Health. 2010;25(2):121–134. doi: 10.1515/reveh.2010.25.2.121. [DOI] [PubMed] [Google Scholar]
- 35.Gorwitz R.J., Kruszon-Moran D., McAllister S.K., McQuillan G., McDougal L.K., Fosheim G.E. Changes in the prevalence of nasal colonization with Staphylococcus aureus in the United States, 2001-2004. J Infect Dis. 2008;197(9):1226–1234. doi: 10.1086/533494. [DOI] [PubMed] [Google Scholar]
- 36.Ellis M.W., Hospenthal D.R., Dooley D.P., Gray P.J., Murray C.K. Natural history of community-acquired methicillin-resistant Staphylococcus aureus colonization and infection in soldiers. Clin Infect Dis. 2004;39(7):971–979. doi: 10.1086/423965. [DOI] [PubMed] [Google Scholar]
- 37.Rohde R.E., Denham R., Brannon A. Methicillin resistant Staphylococcus aureus: carriage rates and characterization of students in a Texas university. Clin Lab Sci. 2009;22(3):176–184. [PubMed] [Google Scholar]
- 38.Creech C.B., Saye E., McKenna B.D., Johnson B.G., Jimenez N., Talbot T.R. One-year surveillance of methicillin-resistant Staphylococcus aureus nasal colonization and skin and soft tissue infections in collegiate athletes. Arch Pediatr Adolesc Med. 2010;164(7):615–620. doi: 10.1001/archpediatrics.2010.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.O'Fallon E., Schreiber R., Kandel R., D'Agata E.M. Multidrug-resistant gram-negative bacteria at a long-term care facility: assessment of residents, healthcare workers, and inanimate surfaces. Infect Control Hosp Epidemiol. 2009;30(12):1172–1179. doi: 10.1086/648453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Elston D.M. Community-acquired methicillin-resistant Staphylococcus aureus. J Am Acad Dermatol. 2007;56(1):1–16. doi: 10.1016/j.jaad.2006.04.018. [quiz 7-20] [DOI] [PubMed] [Google Scholar]
- 41.Li M., Diep B.A., Villaruz A.E., Braughton K.R., Jiang X., DeLeo F.R. Evolution of virulence in epidemic community-associated methicillin-resistant Staphylococcus aureus. Proc Natl Acad Sci U S A. 2009;106(14):5883–5888. doi: 10.1073/pnas.0900743106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Begier E.M., Frenette K., Barrett N.L., Mshar P., Petit S., Boxrud D.J. A high-morbidity outbreak of methicillin-resistant Staphylococcus aureus among players on a college football team, facilitated by cosmetic body shaving and turf burns. Clin Infect Dis. 2004;39(10):1446–1453. doi: 10.1086/425313. [DOI] [PubMed] [Google Scholar]
- 43.Carleton H.A., Diep B.A., Charlebois E.D., Sensabaugh G.F., Perdreau-Remington F. Community-adapted methicillin-resistant Staphylococcus aureus (MRSA): population dynamics of an expanding community reservoir of MRSA. J Infect Dis. 2004;190(10):1730–1738. doi: 10.1086/425019. [DOI] [PubMed] [Google Scholar]
- 44.McCarthy N.L., Sullivan P.S., Gaynes R., Rimland D. Health care-associated and community-associated methicillin-resistant Staphylococcus aureus infections: a comparison of definitions. Am J Infect Control. 2010;38(8):600–606. doi: 10.1016/j.ajic.2010.01.006. [DOI] [PubMed] [Google Scholar]
- 45.Klevens R.M., Morrison M.A., Fridkin S.K., Reingold A., Petit S., Gershman K. Community-associated methicillin-resistant Staphylococcus aureus and healthcare risk factors. Emerg Infect Dis. 2006;12(12):1991–1993. doi: 10.3201/eid1212.060505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.D'Agata E.M., Webb G.F., Pressley J. Rapid emergence of co-colonization with community-acquired and hospital-acquired methicillin-resistant Staphylococcus aureus strains in the hospital setting. Math Model Nat Phenom. 2010;5(3):76–83. doi: 10.1051/mmnp/20105306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Diep B.A., Chambers H.F., Graber C.J., Szumowski J.D., Miller L.G., Han L.L. Emergence of multidrug-resistant, community-associated, methicillin-resistant Staphylococcus aureus clone USA300 in men who have sex with men. Ann Intern Med. 2008;148(4):249–257. doi: 10.7326/0003-4819-148-4-200802190-00204. [DOI] [PubMed] [Google Scholar]
- 48.Matouskova I., Janout V. Current knowledge of methicillin-resistant Staphylococcus aureus and community-associated methicillin-resistant Staphylococcus aureus. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2008;152(2):191–202. doi: 10.5507/bp.2008.030. [DOI] [PubMed] [Google Scholar]
- 49.Herman R.A., Kee V.R., Moores K.G., Ross M.B. Etiology and treatment of community-associated methicillin-resistant Staphylococcus aureus. Am J Health Syst Pharm. 2008;65(3):219–225. doi: 10.2146/ajhp060637. [DOI] [PubMed] [Google Scholar]
- 50.Heymann D.L., American Public Health Association . 19th ed. American Public Health Association; Washington, DC: 2008. Control of communicable diseases manual. [Google Scholar]
- 51.Tacconelli E., De Angelis G., Cataldo M.A., Pozzi E., Cauda R. Does antibiotic exposure increase the risk of methicillin-resistant Staphylococcus aureus (MRSA) isolation? A systematic review and meta-analysis. J Antimicrob Chemother. 2008;61(1):26–38. doi: 10.1093/jac/dkm416. [DOI] [PubMed] [Google Scholar]
- 52.Workplace safety and health topics: MRSA and the workplace. Centers for Disease Control and Prevention; Atlanta: 2010. http://www.cdc.gov/niosh/topics/mrsa/ Retrieved November 22, 2010, from. [Google Scholar]
- 53.Roberts S.S., Kazragis R.J. Methicillin-resistant Staphylococcus aureus infections in U.S. service members deployed to Iraq. Mil Med. 2009;174(4):408–411. doi: 10.7205/milmed-d-02-8408. [DOI] [PubMed] [Google Scholar]
- 54.Maree C.L., Eells S.J., Tan J., Bancroft E.A., Malek M., Harawa N.T. Risk factors for infection and colonization with community-associated methicillin-resistant Staphylococcus aureusin the Los Angeles County jail: a case-control study. Clin Infect Dis. 2010;51(11):1248–1257. doi: 10.1086/657067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Morita J.E., Fujioka R.S., Tice A.D., Berestecky J., Sato D., Seifried S.E. Survey of methicillin-resistant Staphylococcus aureus (MRSA) carriage in healthy college students, Hawai'i. Hawaii Med J. 2007;66(8):213–215. [PubMed] [Google Scholar]
- 56.Fritz S.A., Garbutt J., Elward A., Shannon W., Storch G.A. Prevalence of and risk factors for community-acquired methicillin-resistant and methicillin-sensitive Staphylococcus aureus colonization in children seen in a practice-based research network. Pediatrics. 2008;121(6):1090–1098. doi: 10.1542/peds.2007-2104. [DOI] [PubMed] [Google Scholar]
- 57.Nourbakhsh A., Papafragkou S., Dever L.L., Capo J., Tan V. Stratification of the risk factors of community-acquired methicillin-resistant Staphylococcus aureus hand infection. JHand Surg Am. 2010;35(7):1135–1141. doi: 10.1016/j.jhsa.2010.03.039. [DOI] [PubMed] [Google Scholar]
- 58.Stevens D.L., Bisno A.L., Chambers H.F., Everett E.D., Dellinger P., Goldstein E.J. Practice guidelines for the diagnosis and management of skin and soft-tissue infections. Clin Infect Dis. 2005;41(10):1373–1406. doi: 10.1086/497143. [DOI] [PubMed] [Google Scholar]
- 59.Kazakova S.V., Hageman J.C., Matava M., Srinivasan A., Phelan L., Garfinkel B. A clone of methicillin-resistant Staphylococcus aureus among professional football players. N Engl J Med. 2005;352(5):468–475. doi: 10.1056/NEJMoa042859. [DOI] [PubMed] [Google Scholar]
- 60.Romano R., Lu D., Holtom P. Outbreak of community-acquired methicillin-resistant Staphylococcus aureus skin infections among a collegiate football team. J Athl Train. 2006;41(2):141–145. [PMC free article] [PubMed] [Google Scholar]
- 61.Sanders J.C. Reducing MRSA infections in college student athletes: implementation of a prevention program. J Community Health Nurs. 2009;26(4):161–172. doi: 10.1080/07370010903259162. [DOI] [PubMed] [Google Scholar]
- 62.Garza D., Sungar G., Johnston T., Rolston B., Ferguson J.D., Matheson G.O. Ineffectiveness of surveillance to control community-acquired methicillin-resistant Staphylococcus aureus in a professional football team. Clin J Sport Med. 2009;19(6):498–501. doi: 10.1097/JSM.0b013e3181bd09e0. [DOI] [PubMed] [Google Scholar]
- 63.Yang E.S., Tan J., Eells S., Rieg G., Tagudar G., Miller L.G. Body site colonization in patients with community-associated methicillin-resistant Staphylococcus aureus and other types of S. aureus skin infections. Clin Microbiol Infect. 2010;16(5):425–431. doi: 10.1111/j.1469-0691.2009.02836.x. [DOI] [PubMed] [Google Scholar]
- 64.Tang Y.W., Stratton C.W. Staphylococcus aureus: an old pathogen with new weapons. Clin Lab Med. 2010;30(1):179–208. doi: 10.1016/j.cll.2010.01.005. [DOI] [PubMed] [Google Scholar]
- 65.Patel M. Community-associated meticillin-resistant Staphylococcus aureus infections: epidemiology, recognition and management. Drugs. 2009;69(6):693–716. doi: 10.2165/00003495-200969060-00004. [DOI] [PubMed] [Google Scholar]
- 66.Centers for Disease Control and Prevention . Centers for Disease Control and Prevention; Atlanta: 2010. Symptoms of MRSA.http://www.cdc.gov/mrsa/symptoms/index.html Available from: [Google Scholar]
- 67.Morrison-Rodriguez S.M., Pacha L.A., Patrick J.E., Jordan N.N. Community-associated methicillin-resistant Staphylococcus aureus infections at an Army training installation. Epidemiol Infect. 2010;138(5):721–729. doi: 10.1017/S0950268810000142. [DOI] [PubMed] [Google Scholar]
- 68.Sturenburg E. Rapid detection of methicillin-resistant Staphylococcus aureus directly from clinical samples: methods, effectiveness and cost considerations. Ger Med Sci. 2009;7:1–9. doi: 10.3205/000065. [Doc06] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Jain R., Kralovic S.M., Evans M.E., Ambrose M., Simbartl L.A., Obrosky D.S. Veterans Affairs initiative to prevent methicillin-resistant Staphylococcus aureus infections. N Engl J Med. 2011;364(15):1419–1430. doi: 10.1056/NEJMoa1007474. [DOI] [PubMed] [Google Scholar]
- 70.Cooper B.S., Medley G.F., Stone S.P., Kibbler C.C., Cookson B.D., Roberts J.A. Methicillin-resistant Staphylococcus aureus in hospitals and the community: stealth dynamics and control catastrophes. Proc Natl Acad Sci U S A. 2004;101(27):10223–10228. doi: 10.1073/pnas.0401324101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Centers for Disease Control and Prevention . Centers for Disease Control; Atlanta: 2010. Precautions to prevent the spread of MRSA in healthcare settings.http://www.cdc.gov/mrsa/prevent/healthcare/precautions.html#standard [cited 2011 July 17, 2011]; Available from: [Google Scholar]
- 72.Siegel J.D., Rhinehart E., Jackson M., Chiarello L. Management of multidrug-resistant organisms in health care settings, 2006. Am J Infect Control. 2007;35(10 Suppl 2):S165–S193. doi: 10.1016/j.ajic.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 73.California Department of Public Health . The Department; Sacramento: 2008. California Department of Public Health announces state will require mandatory reporting of severe MRSA cases.http://www.cdph.ca.gov/Pages/PH08-06.aspx Available from: [Google Scholar]
- 74.California Department of Public Health . California Department of Public Health; Sacramento: 2010. Technical report: healthcare-associated bloodstream infections in California hospitals, January 2009 through March 2010.http://www.cdph.ca.gov/programs/hai/Documents/HAIReportSB-1058BSI-FINAL.pdf Available from: [Google Scholar]
- 75.Centers for Disease Control and Prevention . Centers for Disease Control and Prevention; Atlanta: 2010. Diagnosis and testing of MRSA infections.http://www.cdc.gov/mrsa/diagnosis/index.html [cited 2011 July 16]; Available from: [Google Scholar]
- 76.Halpin H.A., Milstein A., Shortell S.M., Vanneman M., Rosenberg J. Mandatory public reporting of hospital-acquired infection rates: a report from California. Health Aff (Millwood) 2011;30(4):723–729. doi: 10.1377/hlthaff.2009.0990. [DOI] [PubMed] [Google Scholar]
- 77.Deresinski S. Vancomycin in combination with other antibiotics for the treatment of serious methicillin-resistant Staphylococcus aureus infections. Clin Infect Dis. 2009;49(7):1072–1079. doi: 10.1086/605572. [DOI] [PubMed] [Google Scholar]
- 78.Owens R.C., Jr., Ambrose P.G. Antimicrobial safety: focus on fluoroquinolones. Clin Infect Dis. 2005;41(Suppl 2):S144–S157. doi: 10.1086/428055. [DOI] [PubMed] [Google Scholar]
- 79.National Institutes of Health . National Library of Medicine; Bethesda: 2008. Medline Plus—vancomycin.http://www.nlm.nih.gov/medlineplus/druginfo/meds/a604038.html#side-effects Available from: [Google Scholar]
- 80.National Institutes of Health . National Library of Medicine; Bethesda: 2008. Medline Plus—trimethoprim.http://www.nlm.nih.gov/medlineplus/druginfo/meds/a684025.html Available from: [Google Scholar]
- 81.National Institutes of Health . National Library of Medicine; Bethesda: 2008. Medline Plus—doxycycline.http://www.nlm.nih.gov/medlineplus/druginfo/meds/a682063.html Available from: [Google Scholar]
- 82.National Institutes of Health . National Library of Medicine; Bethesda: 2008. Medline Plus—clindamycin.http://www.nlm.nih.gov/medlineplus/druginfo/meds/a682399.html Available from: [Google Scholar]
- 83.National Institutes of Health . National Library of Medicine; Bethesda: 2008. Medline Plus—minocycline.http://www.nlm.nih.gov/medlineplus/druginfo/meds/a682101.html#side-effects Available from: [Google Scholar]
- 84.National Institutes of Health . National Library of Medicine; Bethesda: 2008. Medline Plus—linezolid.http://www.nlm.nih.gov/medlineplus/druginfo/meds/a602004.html#side-effects Available from: [Google Scholar]
- 85.Werner N.L., Hecker M.T., Sethi A.K., Donskey C.J. Unnecessary use of fluoroquinolone antibiotics in hospitalized patients. BMC Infect Dis. 2011;11(1):187. doi: 10.1186/1471-2334-11-187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Belavic J.M. Fluoroquinolone-induced tendinopathy. Nurse Prac. 2009;34(1):17–18. doi: 10.1097/01.NPR.0000343751.83969.1b. [DOI] [PubMed] [Google Scholar]
- 87.Noel G.J., Bradley J.S., Kauffman R.E., Duffy C.M., Gerbino P.G., Arguedas A. Comparative safety profile of levofloxacin in 2523 children with a focus on four specific musculoskeletal disorders. Pediatr Infect Dis J. 2007;26(10):879–891. doi: 10.1097/INF.0b013e3180cbd382. [DOI] [PubMed] [Google Scholar]
- 88.Hall M.M., Finnoff J.T., Smith J. Musculoskeletal complications of fluoroquinolones: guidelines and precautions for usage in the athletic population. PM R. 2011;3(2):132–142. doi: 10.1016/j.pmrj.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 89.Childs S.G. Pathogenesis of tendon rupture secondary to fluoroquinolone therapy. Orthop Nurs. 2007;26(3):175–182. doi: 10.1097/01.NOR.0000276969.09808.2c. [quiz 83-4] [DOI] [PubMed] [Google Scholar]
- 90.Khaliq Y., Zhanel G.G. Fluoroquinolone-associated tendinopathy: a critical review of the literature. Clin Infect Dis. 2003;36(11):1404–1410. doi: 10.1086/375078. [DOI] [PubMed] [Google Scholar]
- 91.Gold L., Igra H. Levofloxacin-induced tendon rupture: a case report and review of the literature. J Am Board Fam Med/Am Board Fam Pract. 2003;16(5):458–460. doi: 10.3122/jabfm.16.5.458. [DOI] [PubMed] [Google Scholar]
- 92.Centers for Disease Control and Prevention . Centers for Disease Control and Prevention; Atlanta: 2010. Personal prevention of MRSA skin infections.http://www.cdc.gov/mrsa/prevent/personal.html [cited 2011 July 15, 2011]; Available from: [Google Scholar]
- 93.Methicillin-resistant Staphylococcus aureus infections among competitive sports participants—Colorado, Indiana, Pennsylvania, and Los Angeles County, 2000-2003. MMWR Morb Mortal Wkly Rep. 2003;52(33):793–795. [PubMed] [Google Scholar]
- 94.Centers for Disease Control and Prevention . Centers for Disease Control; Atlanta: 2010. Prevention information and advice for athletes.http://www.cdc.gov/mrsa/groups/advice-for-athletes.html [cited 2011 July 16, 2011]; Available from: [Google Scholar]
- 95.Gagne D., Bedard G., Maziade P.J. Systematic patients' hand disinfection: impact on meticillin-resistant Staphylococcus aureus infection rates in a community hospital. J Hosp Infect. 2010;75(4):269–272. doi: 10.1016/j.jhin.2010.02.028. [DOI] [PubMed] [Google Scholar]


